Optimizing Hearing Outcomes in Nasopharyngeal Cancer Survivors in the Era of Modern Radiotherapy and Systemic Therapy
Abstract
Simple Summary
Abstract
1. Introduction
2. Incidence of SNHL after IMRT for NPC
3. Radiation Dose–Toxicity Relationship of SNHL
4. Prevention Strategy
4.1. De-Escalating Radiotherapy
4.2. Individualizing Cochlea Dose Constraints
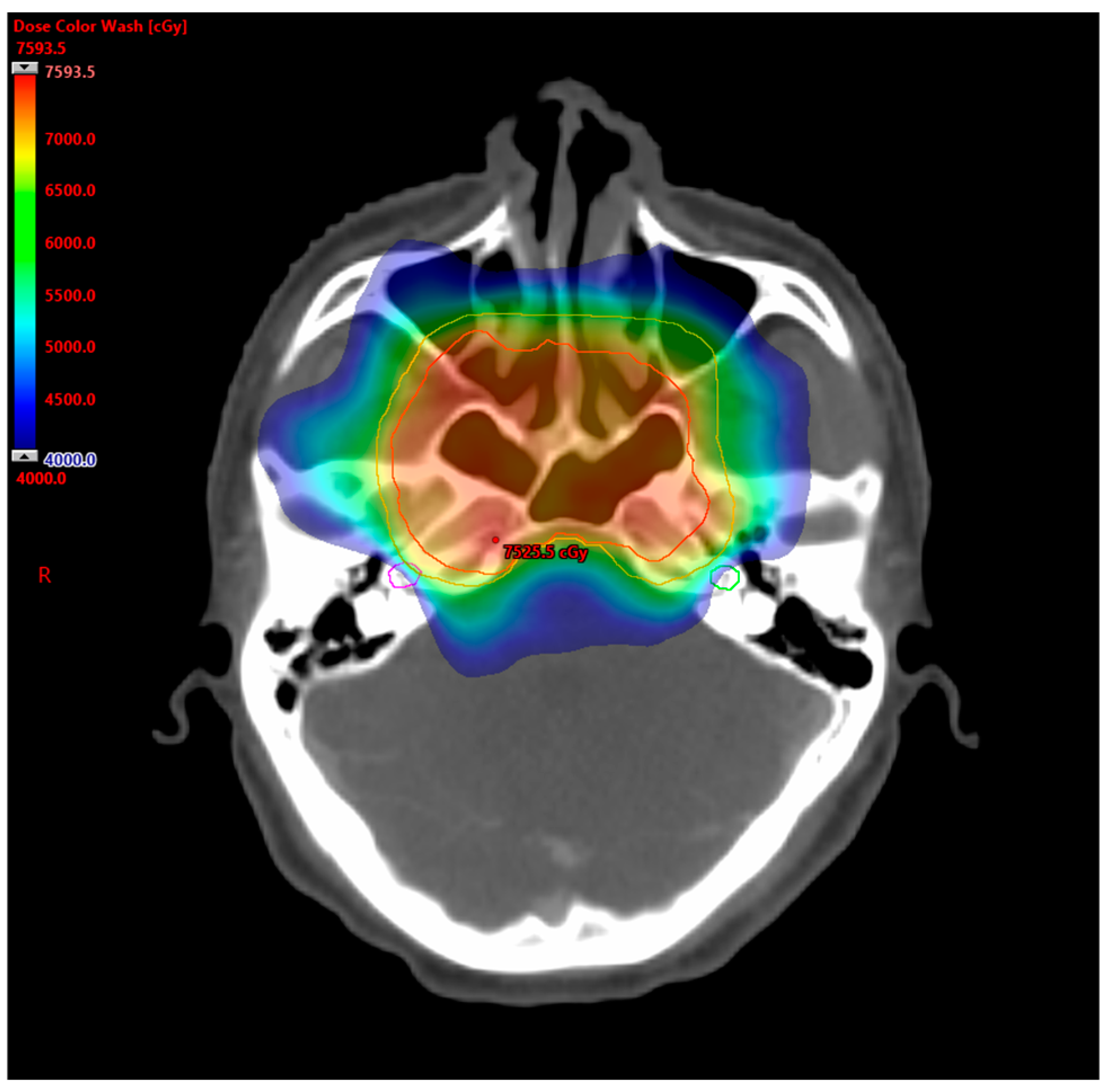
4.3. Selection of Radiotherapy Techniques
4.4. De-Escalating Systemic Therapy
5. Management
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Peng, G.; Wang, T.; Yang, K.Y.; Zhang, S.; Zhang, T.; Li, Q.; Han, J.; Wu, G. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother. Oncol. 2012, 104, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Hou, X.; Bao, X.; Hou, W.; Jiang, X.; Ma, L.; Jiang, X.; Dong, L. Mechanism and Protection of Radiotherapy Induced Sensorineural Hearing Loss for Head and Neck Cancer. Biomed. Res. Int. 2021, 2021, 3548706. [Google Scholar] [CrossRef] [PubMed]
- Low, W.K.; Tan, M.G.; Chua, A.W.; Sun, L.; Wang, D.Y. 12th Yahya Cohen Memorial Lecture: The cellular and molecular basis of radiation-induced sensori-neural hearing loss. Ann. Acad. Med. Singap. 2009, 38, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.J.T.; Vlajkovic, S.M. Molecular Characteristics of Cisplatin-Induced Ototoxicity and Therapeutic Interventions. Int. J. Mol. Sci. 2023, 24, 16545. [Google Scholar] [CrossRef] [PubMed]
- Chattaraj, A.; Syed, M.P.; Low, C.A.; Owonikoko, T.K. Cisplatin-Induced Ototoxicity: A Concise Review of the Burden, Prevention, and Interception Strategies. JCO Oncol. Pract. 2023, 19, 278–283. [Google Scholar] [CrossRef]
- Oh, Y.T.; Kim, C.H.; Choi, J.H.; Kang, S.H.; Chun, M. Sensory neural hearing loss after concurrent cisplatin and radiation therapy for nasopharyngeal carcinoma. Radiother. Oncol. 2004, 72, 79–82. [Google Scholar] [CrossRef]
- Ho, W.K.; Wei, W.I.; Kwong, D.L.; Sham, J.S.; Tai, P.T.; Yuen, A.P.; Au, D.K. Long-term sensorineural hearing deficit following radiotherapy in patients suffering from nasopharyngeal carcinoma: A prospective study. Head. Neck 1999, 21, 547–553. [Google Scholar] [CrossRef]
- Kwong, D.L.; Wei, W.I.; Sham, J.S.; Ho, W.K.; Yuen, P.W.; Chua, D.T.; Au, D.K.; Wu, P.M.; Choy, D.T. Sensorineural hearing loss in patients treated for nasopharyngeal carcinoma: A prospective study of the effect of radiation and cisplatin treatment. Int. J. Radiat. Oncol. Biol. Phys. 1996, 36, 281–289. [Google Scholar] [CrossRef]
- Moretti, J.A. Sensori-neural hearing loss following radiotherapy to the nasopharynx. Laryngoscope 1976, 86, 598–602. [Google Scholar] [CrossRef]
- Hsin, C.H.; Chen, T.H.; Young, Y.H.; Liu, W.S. Comparison of otologic complications between intensity-modulated and two-dimensional radiotherapies in nasopharyngeal carcinoma patients. Otolaryngol. Head. Neck Surg. 2010, 143, 662–668. [Google Scholar] [CrossRef]
- Petsuksiri, J.; Sermsree, A.; Thephamongkhol, K.; Keskool, P.; Thongyai, K.; Chansilpa, Y.; Pattaranutaporn, P. Sensorineural hearing loss after concurrent chemoradiotherapy in nasopharyngeal cancer patients. Radiat. Oncol. 2011, 6, 19. [Google Scholar] [CrossRef] [PubMed]
- Leung, S.W.; Lee, T.F. Treatment of nasopharyngeal carcinoma by tomotherapy: Five-year experience. Radiat. Oncol. 2013, 8, 107. [Google Scholar] [CrossRef]
- Lee, A.W.; Ng, W.T.; Chan, L.L.; Hung, W.M.; Chan, C.C.; Sze, H.C.; Chan, O.S.; Chang, A.T.; Yeung, R.M. Evolution of treatment for nasopharyngeal cancer--success and setback in the intensity-modulated radiotherapy era. Radiother. Oncol. 2014, 110, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Ou, X.; Zhou, X.; Shi, Q.; Xing, X.; Yang, Y.; Xu, T.; Shen, C.; Wang, X.; He, X.; Kong, L.; et al. Treatment outcomes and late toxicities of 869 patients with nasopharyngeal carcinoma treated with definitive intensity modulated radiation therapy: New insight into the value of total dose of cisplatin and radiation boost. Oncotarget 2015, 6, 38381–38397. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chen, Y.Y.; Tai, A.; Chen, X.L.; Huang, S.M.; Yang, C.; Bao, Y.; Li, N.W.; Deng, X.W.; Zhao, C.; et al. Sensorineural Hearing Loss after Combined Intensity Modulated Radiation Therapy and Cisplatin-Based Chemotherapy for Nasopharyngeal Carcinoma. Transl. Oncol. 2015, 8, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Han, F.; Xiao, W.; Xiang, Y.; Lu, L.; Deng, X.; Cui, N.; Zhao, C. Analysis of late toxicity in nasopharyngeal carcinoma patients treated with intensity modulated radiation therapy. Radiat. Oncol. 2015, 10, 17. [Google Scholar] [CrossRef]
- Huang, T.L.; Chien, C.Y.; Tsai, W.L.; Liao, K.C.; Chou, S.Y.; Lin, H.C.; Dean Luo, S.; Lee, T.F.; Lee, C.H.; Fang, F.M. Long-term late toxicities and quality of life for survivors of nasopharyngeal carcinoma treated with intensity-modulated radiotherapy versus non-intensity-modulated radiotherapy. Head Neck 2016, 38 (Suppl. S1), E1026–E1032. [Google Scholar] [CrossRef]
- Qiu, W.Z.; Peng, X.S.; Xia, H.Q.; Huang, P.Y.; Guo, X.; Cao, K.J. A retrospective study comparing the outcomes and toxicities of intensity-modulated radiotherapy versus two-dimensional conventional radiotherapy for the treatment of children and adolescent nasopharyngeal carcinoma. J. Cancer Res. Clin. Oncol. 2017, 143, 1563–1572. [Google Scholar] [CrossRef]
- Chan, S.L.; Ng, L.S.; Goh, X.; Siow, C.H.; Goh, H.L.; Goh, B.C.; Cheo, T.; Loh, K.S.; Brunham, L.R. Time course and clinical characterization of cisplatin-induced ototoxicity after treatment for nasopharyngeal carcinoma in a South East Asian population. Head Neck 2018, 40, 1425–1433. [Google Scholar] [CrossRef]
- Zhu, W.; Chen, F.; Li, J.; Wang, W.; Zhang, H.; Yang, G.; Zou, L.; Zhu, Y.; Yuan, W.; Ding, H.; et al. Dosimetric parameters associated with conductive or sensorineural hearing loss 5 years after intensity-modulated radiation therapy in nasopharyngeal carcinoma. Acta Otolaryngol. 2019, 139, 263–268. [Google Scholar] [CrossRef]
- Inada, M.; Nishimura, Y.; Ishikura, S.; Ishikawa, K.; Murakami, N.; Kodaira, T.; Ito, Y.; Tsuchiya, K.; Murakami, Y.; Saito, J.; et al. Organs-at-risk dose constraints in head and neck intensity-modulated radiation therapy using a dataset from a multi-institutional clinical trial (JCOG1015A1). Radiat. Oncol. 2022, 17, 133. [Google Scholar] [CrossRef] [PubMed]
- Yip, P.L.; Mok, K.C.J.; Ho, H.S.; Lee, W.Y.V.; Wong, A.C.L.; Lau, C.T.; Wong, F.C.S.; Yeung, K.W.; Lee, S.F. Sensorineural Hearing Loss in Nasopharyngeal Carcinoma Survivors in the Modern Treatment Era—The Early and Late Effects of Radiation and Cisplatin. Clin. Oncol. (R. Coll. Radiol.) 2022, 34, e160–e167. [Google Scholar] [CrossRef] [PubMed]
- Doi, H.; Ri, A.; Inada, M.; Tatsuno, S.; Uehara, T.; Matsuura, T.; Ishikawa, K.; Nakamatsu, K.; Hosono, M.; Nishimura, Y. Clinical course of longer than five years after definitive radiotherapy for nasopharyngeal carcinoma. Int. J. Clin. Oncol. 2023, 28, 1607–1615. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Li, J.; Li, K.; Hu, J.; Li, Q.; Huang, C.; Wang, G.; Liu, N.; Tang, L. Evaluation and analysis of risk factors of hearing impairment for nasopharyngeal carcinoma treated using intensity-modulated radiotherapy. Radiother. Oncol. 2024, 190, 109985. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute (US). Common Terminology Criteria for Adverse Events (CTCAE), 4th ed.; U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute: Bethesda, MD, USA, 2009. [Google Scholar]
- LENT SOMA scales for all anatomic sites. Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 1049–1091. [CrossRef]
- Cox, J.D.; Stetz, J.; Pajak, T.F. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 1341–1346. [Google Scholar] [CrossRef]
- Newman, C.W.; Weinstein, B.E.; Jacobson, G.P.; Hug, G.A. Test-retest reliability of the hearing handicap inventory for adults. Ear Hear. 1991, 12, 355–357. [Google Scholar] [CrossRef]
- Bass, J.K.; Wang, F.; Thaxton, M.E.; Warren, S.E.; Srivastava, D.K.; Hudson, M.M.; Ness, K.K.; Brinkman, T.M. Association of hearing loss with patient-reported functional outcomes in adult survivors of childhood cancer. J. Natl. Cancer Inst. 2024, 116, 596–605. [Google Scholar] [CrossRef]
- Lau, S.K.; Wei, W.I.; Sham, J.S.; Choy, D.T.; Hui, Y. Early changes of auditory brain stem evoked response after radiotherapy for nasopharyngeal carcinoma--a prospective study. J. Laryngol. Otol. 1992, 106, 887–892. [Google Scholar] [CrossRef]
- Chen, Y.P.; Ismaila, N.; Chua, M.L.K.; Colevas, A.D.; Haddad, R.; Huang, S.H.; Wee, J.T.S.; Whitley, A.C.; Yi, J.L.; Yom, S.S.; et al. Chemotherapy in Combination With Radiotherapy for Definitive-Intent Treatment of Stage II-IVA Nasopharyngeal Carcinoma: CSCO and ASCO Guideline. J. Clin. Oncol. 2021, 39, 840–859. [Google Scholar] [CrossRef]
- Bossi, P.; Chan, A.T.; Licitra, L.; Trama, A.; Orlandi, E.; Hui, E.P.; Halamkova, J.; Mattheis, S.; Baujat, B.; Hardillo, J.; et al. Nasopharyngeal carcinoma: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up(dagger). Ann. Oncol. 2021, 32, 452–465. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Yu, X.L.; Luo, W.; Lee, A.W.; Wee, J.T.; Lee, N.; Zhou, G.Q.; Tang, L.L.; Tao, C.J.; Guo, R.; et al. Recommendation for a contouring method and atlas of organs at risk in nasopharyngeal carcinoma patients receiving intensity-modulated radiotherapy. Radiother. Oncol. 2014, 110, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.C.; Jackson, A.; Budnick, A.S.; Pfister, D.G.; Kraus, D.H.; Hunt, M.A.; Stambuk, H.; Levegrun, S.; Wolden, S.L. Sensorineural hearing loss in combined modality treatment of nasopharyngeal carcinoma. Cancer 2006, 106, 820–829. [Google Scholar] [CrossRef]
- Chan, S.H.; Ng, W.T.; Kam, K.L.; Lee, M.C.; Choi, C.W.; Yau, T.K.; Lee, A.W.; Chow, S.K. Sensorineural hearing loss after treatment of nasopharyngeal carcinoma: A longitudinal analysis. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Zhou, T.; Zhu, J.; Zhang, Y.; Sun, M.; Ding, X.; Wang, D.; Li, H.; Li, B. Long-term outcome of sensorineural hearing loss in nasopharyngeal carcinoma patients: Comparison between treatment with radiotherapy alone and chemoradiotherapy. Cell Biochem. Biophys. 2014, 69, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Peuker, L.; Rolf, D.; Oertel, M.; Peuker, A.; Scobioala, S.; Hering, D.; Rudack, C.; Haverkamp, U.; Eich, H.T. Definition of an Normal Tissue Complication Probability Model for the Inner Ear in Definitive Radiochemotherapy of Nasopharynx Carcinoma. Cancers 2022, 14, 3422. [Google Scholar] [CrossRef]
- Bhandare, N.; Jackson, A.; Eisbruch, A.; Pan, C.C.; Flickinger, J.C.; Antonelli, P.; Mendenhall, W.M. Radiation therapy and hearing loss. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, S50–S57. [Google Scholar] [CrossRef]
- Lee, A.W.; Ng, W.T.; Pan, J.J.; Chiang, C.L.; Poh, S.S.; Choi, H.C.; Ahn, Y.C.; AlHussain, H.; Corry, J.; Grau, C.; et al. International Guideline on Dose Prioritization and Acceptance Criteria in Radiation Therapy Planning for Nasopharyngeal Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, 567–580. [Google Scholar] [CrossRef]
- Lee, N.; Harris, J.; Garden, A.S.; Straube, W.; Glisson, B.; Xia, P.; Bosch, W.; Morrison, W.H.; Quivey, J.; Thorstad, W.; et al. Intensity-modulated radiation therapy with or without chemotherapy for nasopharyngeal carcinoma: Radiation therapy oncology group phase II trial 0225. J. Clin. Oncol. 2009, 27, 3684–3690. [Google Scholar] [CrossRef]
- Au, K.H.; Ngan, R.K.C.; Ng, A.W.Y.; Poon, D.M.C.; Ng, W.T.; Yuen, K.T.; Lee, V.H.F.; Tung, S.Y.; Chan, A.T.C.; Sze, H.C.K.; et al. Treatment outcomes of nasopharyngeal carcinoma in modern era after intensity modulated radiotherapy (IMRT) in Hong Kong: A report of 3328 patients (HKNPCSG 1301 study). Oral Oncol. 2018, 77, 16–21. [Google Scholar] [CrossRef]
- Lee, A.W.; Ng, W.T.; Pan, J.J.; Poh, S.S.; Ahn, Y.C.; AlHussain, H.; Corry, J.; Grau, C.; Gregoire, V.; Harrington, K.J.; et al. International guideline for the delineation of the clinical target volumes (CTV) for nasopharyngeal carcinoma. Radiother. Oncol. 2018, 126, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Xie, D.H.; Wu, Z.; Li, W.Z.; Cheng, W.Q.; Tao, Y.L.; Wang, L.; Lv, S.W.; Lin, F.F.; Cui, N.J.; Zhao, C.; et al. Individualized clinical target volume delineation and efficacy analysis in unilateral nasopharyngeal carcinoma treated with intensity-modulated radiotherapy (IMRT): 10-year summary. J. Cancer Res. Clin. Oncol. 2022, 148, 1931–1942. [Google Scholar] [CrossRef] [PubMed]
- Xiang, L.; Rong, J.F.; Xin, C.; Li, X.Y.; Zheng, Y.; Ren, P.R.; Lin, S.; Wen, Q.L.; He, L.J.; Zhang, J.W.; et al. Reducing Target Volumes of Intensity Modulated Radiation Therapy After Induction Chemotherapy in Locoregionally Advanced Nasopharyngeal Carcinoma: Long-Term Results of a Prospective, Multicenter, Randomized Trial. Int. J. Radiat. Oncol. Biol. Phys. 2023, 117, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Huang, N.; Yip, P.L.; Wang, J.; Huang, R.; Sun, Z.; Kang, D.; He, Q.; Deng, X.; Zhao, C.; et al. The individualized delineation of clinical target volume for primary nasopharyngeal carcinoma based on invasion risk of substructures: A prospective, real-world study with a large population. Radiother. Oncol. 2024, 194, 110154. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.J.; Jin, Y.N.; Lin, Y.J.; Zhang, W.J.; Marks, T.; Ryan, I.; Zhang, H.Y.; Xia, L.P. The feasibility of reduced-dose radiotherapy in childhood nasopharyngeal carcinoma with favorable response to neoadjuvant chemotherapy. Radiother. Oncol. 2023, 178, 109414. [Google Scholar] [CrossRef]
- Luo, D.H.; Li, X.Y.; Guo, S.S.; Guo, W.P.; Liu, L.T.; Mo, H.Y.; Guo, L.; Lv, X.F.; Liu, L.Z.; Li, J.B.; et al. Paclitaxel liposome, cisplatin and 5-fluorouracil-based induction chemotherapy followed by de-escalated intensity-modulated radiotherapy with concurrent cisplatin in stage IVA-IVB childhood nasopharyngeal carcinoma in endemic area: A phase II, single-arm trial. Lancet Reg. Health West. Pac. 2023, 40, 100895. [Google Scholar] [CrossRef]
- Guo, S.S.; Yang, J.H.; Sun, X.S.; Liu, L.Z.; Yang, Z.C.; Liu, L.T.; Liu, S.L.; Li, X.Y.; Lv, X.F.; Luo, D.H.; et al. Reduced-dose radiotherapy for Epstein-Barr virus DNA selected staged III nasopharyngeal carcinoma: A single-arm, phase 2 trial. Eur. J. Cancer 2023, 194, 113336. [Google Scholar] [CrossRef]
- Zhang, C.; Liu, L.X.; Li, W.Z.; Liang, W.; Chen, Z.H.; Huang, X.H.; Qi, J.; Chen, X.H.; Liang, J.G.; Cao, X.L. Cochlea sparing with a stratified scheme of dose limitation employed in intensity-modulated radiotherapy for nasopharyngeal carcinoma: A dosimetry study. Med. Dosim. 2019, 44, 226–232. [Google Scholar] [CrossRef]
- Gao, J.; Qian, T.L.; Tao, C.Z.; Zhang, Y.H.; Zhou, Y.; Yang, J.; He, J.; Wang, R.; Zhou, P.J. SmartArc-based volumetric modulated arc therapy can improve the middle ear, vestibule and cochlea sparing for locoregionally advanced nasopharyngeal carcinoma: A dosimetric comparison with step-and-shoot intensity-modulated radiotherapy. Br. J. Radiol. 2015, 88, 20150052. [Google Scholar] [CrossRef]
- He, L.; Xiao, J.; Wei, Z.; He, Y.; Wang, J.; Guan, H.; Mu, X.; Peng, X. Toxicity and dosimetric analysis of nasopharyngeal carcinoma patients undergoing radiotherapy with IMRT or VMAT: A regional center’s experience. Oral Oncol. 2020, 109, 104978. [Google Scholar] [CrossRef]
- Lamaj, E.; Vu, E.; van Timmeren, J.E.; Leonardi, C.; Marc, L.; Pytko, I.; Guckenberger, M.; Balermpas, P. Cochlea sparing optimized radiotherapy for nasopharyngeal carcinoma. Radiat. Oncol. 2021, 16, 64. [Google Scholar] [CrossRef] [PubMed]
- Nanda, S.; Parida, S.; Ahirwar, M.K. A Dosimetric Comparison of Volumetric-modulated Arc Therapy and IMRT for Cochlea-sparing Radiation Therapy in Locally Advanced Nasopharyngeal Cancer. J. Med. Phys. 2023, 48, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Jiri, K.; Vladimir, V.; Michal, A.; Matej, N.; Silvia, S.; Pavel, V.; Katerina, D.; Jana, P.; Barbora, O.; Eliska, R.; et al. Proton pencil-beam scanning radiotherapy in the treatment of nasopharyngeal cancer: Dosimetric parameters and 2-year results. Eur. Arch. Otorhinolaryngol. 2021, 278, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Williams, V.M.; Parvathaneni, U.; Laramore, G.E.; Aljabab, S.; Wong, T.P.; Liao, J.J. Intensity-Modulated Proton Therapy for Nasopharynx Cancer: 2-year Outcomes from a Single Institution. Int. J. Part. Ther. 2021, 8, 28–40. [Google Scholar] [CrossRef]
- Anderson, J.L.; Schreibmann, E.; Bates, J.E.; Rudra, S.; Hall, B.; Neunuebel, A.; Remick, J.S.; Stokes, W.A.; McDonald, M.W. Photon vs. Proton Radiotherapy in the Definitive Treatment of Nasopharyngeal Cancer: Single Institution Experience. Int. J. Radiat. Oncol. Biol. Phys. 2023, 117, e562. [Google Scholar] [CrossRef]
- Tang, L.L.; Guo, R.; Zhang, N.; Deng, B.; Chen, L.; Cheng, Z.B.; Huang, J.; Hu, W.H.; Huang, S.H.; Luo, W.J.; et al. Effect of Radiotherapy Alone vs Radiotherapy With Concurrent Chemoradiotherapy on Survival Without Disease Relapse in Patients With Low-risk Nasopharyngeal Carcinoma: A Randomized Clinical Trial. JAMA 2022, 328, 728–736. [Google Scholar] [CrossRef]
- Li, X.Y.; Luo, D.H.; Guo, L.; Mo, H.Y.; Sun, R.; Guo, S.S.; Liu, L.T.; Yang, Z.C.; Yang, J.H.; Qiu, F.; et al. Deintensified Chemoradiotherapy for Pretreatment Epstein-Barr Virus DNA-Selected Low-Risk Locoregionally Advanced Nasopharyngeal Carcinoma: A Phase II Randomized Noninferiority Trial. J. Clin. Oncol. 2022, 40, 1163–1173. [Google Scholar] [CrossRef]
- Tang, L.Q.; Chen, D.P.; Guo, L.; Mo, H.Y.; Huang, Y.; Guo, S.S.; Qi, B.; Tang, Q.N.; Wang, P.; Li, X.Y.; et al. Concurrent chemoradiotherapy with nedaplatin versus cisplatin in stage II-IVB nasopharyngeal carcinoma: An open-label, non-inferiority, randomised phase 3 trial. Lancet Oncol. 2018, 19, 461–473. [Google Scholar] [CrossRef]
- Lv, T.; Wang, Y.; Ou, D.; Liu, P.; Qin, S.; Liu, L.; Lou, P.; Wang, X. IMRT combined with S-1 concurrent chemoradiotherapy in locally advanced nasopharyngeal carcinoma: A prospective phase II study. Investig. New Drugs 2019, 37, 352–359. [Google Scholar] [CrossRef]
- Wu, Z.; Qi, B.; Lin, F.F.; Zhang, L.; He, Q.; Li, F.P.; Wang, H.; Han, Y.Q.; Yin, W.J. Characteristics of local extension based on tumor distribution in nasopharyngeal carcinoma and proposed clinical target volume delineation. Radiother. Oncol. 2023, 183, 109595. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, L.; Hu, G.Q.; Zhang, N.; Zhu, X.D.; Yang, K.Y.; Jin, F.; Shi, M.; Chen, Y.P.; Hu, W.H.; et al. Final Overall Survival Analysis of Gemcitabine and Cisplatin Induction Chemotherapy in Nasopharyngeal Carcinoma: A Multicenter, Randomized Phase III Trial. J. Clin. Oncol. 2022, 40, 2420–2425. [Google Scholar] [CrossRef] [PubMed]
- Lee, F.K.; Yip, C.W.; Cheung, F.C.; Leung, A.K.; Chau, R.M.; Ngan, R.K. Dosimetric difference amongst 3 techniques: TomoTherapy, sliding-window intensity-modulated radiotherapy (IMRT), and RapidArc radiotherapy in the treatment of late-stage nasopharyngeal carcinoma (NPC). Med. Dosim. 2014, 39, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.L.; Chen, Y.P.; Chen, C.B.; Chen, M.Y.; Chen, N.Y.; Chen, X.Z.; Du, X.J.; Fang, W.F.; Feng, M.; Gao, J.; et al. The Chinese Society of Clinical Oncology (CSCO) clinical guidelines for the diagnosis and treatment of nasopharyngeal carcinoma. Cancer Commun. 2021, 41, 1195–1227. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Head and Neck Cancers (Version 4.2024). Available online: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf (accessed on 20 May 2024).
- Chen, Q.Y.; Wen, Y.F.; Guo, L.; Liu, H.; Huang, P.Y.; Mo, H.Y.; Li, N.W.; Xiang, Y.Q.; Luo, D.H.; Qiu, F.; et al. Concurrent chemoradiotherapy vs radiotherapy alone in stage II nasopharyngeal carcinoma: Phase III randomized trial. J. Natl. Cancer Inst. 2011, 103, 1761–1770. [Google Scholar] [CrossRef] [PubMed]
- Su, S.F.; Han, F.; Zhao, C.; Chen, C.Y.; Xiao, W.W.; Li, J.X.; Lu, T.X. Long-term outcomes of early-stage nasopharyngeal carcinoma patients treated with intensity-modulated radiotherapy alone. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Zhang, Y.; Li, W.F.; Liu, X.; Guo, R.; Sun, Y.; Lin, A.H.; Chen, L.; Ma, J. Efficacy of Concurrent Chemotherapy for Intermediate Risk NPC in the Intensity-Modulated Radiotherapy Era: A Propensity-Matched Analysis. Sci. Rep. 2015, 5, 17378. [Google Scholar] [CrossRef]
- Huang, X.; Chen, X.; Zhao, C.; Wang, J.; Wang, K.; Wang, L.; Miao, J.; Cao, C.; Jin, T.; Zhang, Y.; et al. Adding Concurrent Chemotherapy to Intensity-Modulated Radiotherapy Does Not Improve Treatment Outcomes for Stage II Nasopharyngeal Carcinoma: A Phase 2 Multicenter Clinical Trial. Front. Oncol. 2020, 10, 1314. [Google Scholar] [CrossRef]
- Al-Sarraf, M.; LeBlanc, M.; Giri, P.G.; Fu, K.K.; Cooper, J.; Vuong, T.; Forastiere, A.A.; Adams, G.; Sakr, W.A.; Schuller, D.E.; et al. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: Phase III randomized Intergroup study 0099. J. Clin. Oncol. 1998, 16, 1310–1317. [Google Scholar] [CrossRef]
- Teft, W.A.; Winquist, E.; Nichols, A.C.; Kuruvilla, S.; Richter, S.; Parker, C.; Francis, P.; Trinnear, M.; Lukovic, J.; Bukhari, N.; et al. Predictors of cisplatin-induced ototoxicity and survival in chemoradiation treated head and neck cancer patients. Oral Oncol. 2019, 89, 72–78. [Google Scholar] [CrossRef]
- Xia, W.X.; Lv, X.; Liang, H.; Liu, G.Y.; Sun, R.; Zeng, Q.; Li, S.W.; Mo, H.Y.; Han, F.; Luo, D.H.; et al. A Randomized Controlled Trial Comparing Two Different Schedules for Cisplatin Treatment in Patients with Locoregionally Advanced Nasopharyngeal Cancer. Clin. Cancer Res. 2021, 27, 4186–4194. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Y.; Yang, K.Y.; Zhang, N.; Jin, F.; Zou, G.R.; Zhu, X.D.; Xie, F.Y.; Liang, X.Y.; Li, W.F.; et al. Induction-concurrent chemoradiotherapy with or without sintilimab in patients with locoregionally advanced nasopharyngeal carcinoma in China (CONTINUUM): A multicentre, open-label, parallel-group, randomised, controlled, phase 3 trial. Lancet 2024, 403, 2720–2731. [Google Scholar] [CrossRef] [PubMed]
- Ishak, E.M.; Gallitto, M.; Golub, J.S.; Sisti, M.B.; Wang, T.J.C. Radiation-Induced Sensorineural Hearing Loss and Potential Management. Pract. Radiat. Oncol. 2024, 14, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Deep, N.L.; Dowling, E.M.; Jethanamest, D.; Carlson, M.L. Cochlear Implantation: An Overview. J. Neurol. Surg. B Skull Base 2019, 80, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Li, J.J.; Guo, Y.K.; Tang, Q.L.; Li, S.S.; Zhang, X.L.; Wu, P.A.; Yang, X.M. Prospective study of sensorineural hearing loss following radiotherapy for nasopharyngeal carcinoma. J. Laryngol. Otol. 2010, 124, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.W.; Yeung, K.N.; Luk, B.P.; Leung, K.K.; Sung, J.K.; Tong, M.C. Cochlear implantation in postirradiated ears: A case-control comparative study. Laryngoscope Investig. Otolaryngol. 2020, 5, 1163–1167. [Google Scholar] [CrossRef]
- Lee, C.Y.; Lin, W.C.; Lin, C.C.; Hsu, C.J.; Wu, H.P. Management Options for Patients With Nasopharyngeal Carcinoma Undergoing Cochlear Implantation. Ear Nose Throat J. 2020, 145561320947274. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, X.; Huang, H.; Ge, R.; Liu, X.; Huang, D.; Huang, Y.; Mo, Y.; Lin, X.; Liu, T.; et al. Long-Term Outcomes of Cochlear Implantation in Irradiated Ears of Nasopharyngeal Carcinoma Patients. Laryngoscope 2021, 131, 649–655. [Google Scholar] [CrossRef]
- Alahmadi, A.; Abdelsamad, Y.; Al-Zuraiqi, B.; Alghamdi, S.; Hagr, A.; Saleh, E. Cochlear Implantation in Radiation-Induced Hearing Loss: A Systematic Review. Otol. Neurotol. 2023, 44, 767–774. [Google Scholar] [CrossRef]
- Soo, G.; Tong, M.C.; Tsang, W.S.; Wong, T.K.; To, K.F.; Leung, S.F.; van Hasselt, C.A. The BAHA hearing system for hearing-impaired postirradiated nasopharyngeal cancer patients: A new indication. Otol. Neurotol. 2009, 30, 496–501. [Google Scholar] [CrossRef]
- Staecker, H.; Jokovic, G.; Karpishchenko, S.; Kienle-Gogolok, A.; Krzyzaniak, A.; Lin, C.D.; Navratil, P.; Tzvetkov, V.; Wright, N.; Meyer, T. Efficacy and Safety of AM-111 in the Treatment of Acute Unilateral Sudden Deafness-A Double-blind, Randomized, Placebo-controlled Phase 3 Study. Otol. Neurotol. 2019, 40, 584–594. [Google Scholar] [CrossRef]
- Tan, P.X.; Du, S.S.; Ren, C.; Yao, Q.W.; Yuan, Y.W. Radiation-induced Cochlea hair cell death: Mechanisms and protection. Asian Pac. J. Cancer Prev. 2013, 14, 5631–5635. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhao, Y.; Zhou, X.; Tan, L.; Ou, Z.; Yu, Y.; Wang, Y. Methylprednisolone use during radiotherapy extenuates hearing loss in patients with nasopharyngeal carcinoma. Laryngoscope 2016, 126, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Khalaily, L.; Avraham, K.B. Insights into the regulation of hearing regeneration. Front. Audiol. Otol. 2024, 2, 1404617. [Google Scholar] [CrossRef]
| Study | Study Design | n | Median Age (Years) | Median FU (Months) | Cisplatin Use | Cisplatin Dose | Definition of SNHL | Incidence |
|---|---|---|---|---|---|---|---|---|
| Hsin et al., 2010 [10] | Prospective cohort | 26 a | Mean 43 | 36 | 88.5% | Concurrent 30 mg/m2 weekly | Increase in BCT ≥20 dB at 4 kHz | 46% |
| Petsuksiri et al., 2011 [11] | Retrospective cohort | 27 a | 47.5 b | 27.5 b | 97% b | Concurrent 100 mg/m2 Q3w Adjuvant 80 mg/m2 with 5FU Q3w | Increase in BCT of ≥15 dB at 4 kHz | 37% c |
| Leung et al., 2013 [12] | Prospective cohort | 72 | 46.5 | 41 | 62.5% | NR | As per RTOG | 3% (G3) |
| Lee et al., 2014 [13] | Retrospective cohort | 444 a | Mean 52 | 81.6 b | 87% | NR | CTCAE ≥G3 | 17.2% |
| Ou et al., 2015 [14] | Retrospective cohort | 869 | Mean, 49 | 54.3 | 84.8% | Induction or adjuvant 75 mg/m2 with docetaxel and/or 5FU and/or gemcitabine Q3w for 2–3 (induction) or Q4w for 2–3 cycles (adjuvant) Concurrent 80 mg/m2 Q3w or 40 mg/m2 weekly | CTCAE | 13.0% (any grade) 1.7% (≥G3) |
| Wang et al., 2015 [15] | Retrospective cohort | 51 | 42 | 60 | 100% | Induction 80 mg/m2 with 5FU Q3w for 2–3 cycles Concurrent 80 mg/m2 Q3w or 40 mg/m2 weekly Adjuvant 80 mg/m2 with 5FU Q3w for 3–4 cycles | Increase in threshold ≥15 dB | At 0.5–2 kHz: 12.7% At 4 kHz: 42.2% c |
| Zheng et al., 2015 [16] | Prospective cohort | 208 | 42 | 78 | 38.9% | NR | As per LENT/SOMA | 47.1% (G1) 19.7% (G2) 0.96% (G3) |
| Huang et al., 2016 [17] | Cross-sectional study | 100 a | 46.2 | ≥60 | 73% | NR | CTCAE ≥G2 | 26.0% |
| Qiu et al., 2017 [18] | Retrospective cohort | 102 a | Range, 7–20 b | 52 b | 97.1% | Induction with 5FU Q3w for 1–3 cycles Concurrent 30 mg/m2 weekly or 80–100 mg/m2 Q3w | CTCAE ≥G2 | 22.5% |
| Chan et al., 2018 [19] | Prospective and retrospective cohort | 142 | 56.8 (RT) 49.6 (CRT) 52.5 (iCRT) | 14.7 (RT) 15.2 (CRT) 17.8 (iCRT) | 78.2% | Induction 75 mg/m2 Q3w for 3 cycles Concurrent 40 mg/m2 weekly | CTCAE ≥G2 | 27.5% |
| Zhu et al., 2019 [20] | Retrospective cohort | 70 | 44 | 69 | NR | 70 mg/m2 with 5FU Q3w | Increase in hearing threshold ≥15 dB | At 0.5–2 kHz: 7.69% At 4 kHz: 35.9% c |
| Inada et al., 2022 [21] | Prospective cohort | 74 | 55 | 50 | 100% | Concurrent 80 mg/m2 Q3w | CTCAE ≥G2 | 5-year incidence 26% |
| Yip et al., 2022 [22] | Retrospective cohort | 81 | 53.5 (RT) 48.9 (CRT) 49.1 (iCRT) | 38 | 64.0% | Induction 100 mg/m2 Q3w for 3 cycles Concurrent 100 mg/m2 Q3w or 40 mg/m2 weekly | Increase in BCT ≥15 dB within 12 months after completion of RT (early) and at least 2 years after completion of RT (late) | At 4 kHz, Early: 19.9% Late: 32.2% |
| Doi et al., 2023 [23] | Retrospective cohort | 43 | 55 | 119 | 100% | Concurrent 80 mg/m2 for 2–3 cycles Adjuvant 70 mg/m2 with 5FU for 2–3 cycles | CTCAE ≥G2 | 7% |
| Chen et al., 2024 [24] | Retrospective cohort | 588 | 27 | 103.4 | 84.8% | Concurrent weekly or Q3w regimen Median 160 mg/m2 | The Hearing Handicap Inventory for Adult-Screening version (HHIA-S) | Hearing impairment: 39.5% Severe hearing impairment: 29.7% |
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | |
|---|---|---|---|---|
| CTCAE v4.0/v5.0 a [25] Enrolled in a monitoring program (1, 2, 3, 4, 6, and 8 kHz audiogram) | Threshold shift of 15–25 dB averaged at 2 contiguous test frequencies in at least one ear | Threshold shift of >25 dB averaged at 2 contiguous test frequencies in at least one ear | Threshold shift of >25 dB averaged at 3 contiguous test frequencies in at least one ear; therapeutic intervention indicated | Profound bilateral hearing loss (>80 dB at 2 kHz and above) |
| CTCAE v4.0/v5.0 [25] Not enrolled in monitoring program | Subjective change in hearing in the absence of documented hearing loss | Hearing loss but hearing aid or intervention not indicated; limiting instrumental ADL | Hearing loss with hearing aid or intervention indicated; limiting self-care ADL | Non-serviceable hearing |
| LENT/SOMA [26] | <10 dB loss in one or more frequencies; minor loss, no change in daily activities | 10–15 dB loss in one or more frequencies; frequent difficulties with faint speech | >15–20 dB loss in one or more frequencies; frequent difficult with loud speech; hearing aid required | >20 dB loss in one or more frequencies; complete deafness |
| RTOG/EORTC Toxicity Criteria [27] | Mild | Moderate | Severe | Life-threatening or disabling |
| Study | n | RT Technique | Proposed Parameter | Proposed Dosimetric Constraint | Adjusted for Cisplatin? | Adjusted for T Staging? | Median FU (Months) | Incidence of SNHL Per Ear (Low Risk Group vs. High Risk Group with Reference to the Proposed Dosimetric Cut-Off Point) |
|---|---|---|---|---|---|---|---|---|
| Chen et al., 2006 [34] | 22 | IMRT 68% 3DCRT 32% | Dmean cochlea | ≤48 Gy | No | No | 29 | 24% vs. 61% at 4 kHz |
| Chan et al., 2009 [35] | 87 | IMRT 69% 3DCRT 31% | Dmean cochlea | <47 Gy | Yes | No | 24 | 14% vs. 31% |
| Petsuksiri et al., 2011 [11] | 68 | IMRT 40% 2DRT 60% | Dmean IAC | ≤50 Gy | Yes | No | 27.5 | 25.81% vs. 52.17% |
| Wei et al., 2014 [36] | 72 | IMRT 100% | Dmean cochlea | <46 Gy | No | No | 60 | NR |
| Wang et al., 2015 [15] | 51 | IMRT 100% | D0.1ml cochlea | <39.8 Gy | Yes | Yes | 60 | 4.3% vs. 20.0% |
| Zhu et al., 2019 [20] | 70 | IMRT 100% | Dmax IAC | <42.13 Gy | No | Yes | 69 | 19.4% vs. 41.9% |
| Dmean IAC | <32.72 Gy | 21.6% vs. 42.5% | ||||||
| Yip et al., 2022 [22] | 81 | IMRT 100% | Dmean cochlea | <40 Gy | Yes | No | 38 | 0% vs. 29.4% Every 10 Gy increase in Dmean cochlea leads to 5 dB increase in BCT at 4 kHz |
| Dmean inner ear | NR | Every 10 Gy increase in Dmean inner ear leads to 6 dB increase in BCT at 4 kHz | ||||||
| Inada et al., 2022 [21] | 74 | IMRT 100% | Dmean ipsilateral inner ear | <44 Gy | No | No | 50 | 18% vs. 42% |
| Peuker et al., 2022 [37] | 46 | IMRT 97.8% 3DCRT 2.2% | Dmean inner ear | <44Gy | No | No | 31.2 | 25% vs. NR a |
| Dmax inner ear | <58 Gy | 25% vs. NR a | ||||||
| Chen et al., 2024 [24] | 588 | IMRT 100% | HI: | Yes | No | 103.4 | NR | |
| V45 inner ear | <50% | |||||||
| V50 IAC | <40% | |||||||
| Severe HI: | ||||||||
| Dmin IAC | <44 Gy | |||||||
| V60 IAC | <40% |
| Prevention Strategy | Study | Strategy Details | n | Median FU (Months) | Auditory Outcomes |
|---|---|---|---|---|---|
| De-escalating radiotherapy | |||||
| Reducing treatment volume | Xie et al., 2022 [43] | CTV delineated by geometric expansion of gross tumor for unilateral NPC (defined as tumor confined to one side of NP and did not cross the midline by endoscopy and MRI) without including the whole nasopharyngeal mucosa | 95 | 84 | Low incidence of hearing impairment on tumor-contralateral side (1.1%) |
| Xiang et al., 2023 [44] | GTV contoured according to post-induction chemotherapy tumor extent, with pre-induction chemotherapy tumor extent included in the high-risk prophylactic volume | 233 | 98.4 | Lower incidence of any grade hearing loss compared to control (52.2% vs. 69.1%) | |
| Wang et al., 2024 [45] | Divide the neighboring structures of nasopharynx into 4 levels; CTV delineated by geometric expansion of gross tumor plus the inclusion of neighboring structures according to the extent of primary tumor | 1004 | 66.6 | RTOG G1 hearing impairment 24.1%, G2 2.1%, G3 0.2% | |
| Reducing radiation dose | Yao et al., 2023 [46] | Lower radiation dose to GTV (60–65.9 Gy) for patients with stage III–IVA (AJCC 8th edition) NPC who achieved tumor response after induction chemotherapy | 132 | 75.2 | Lower incidence of CTCAE G3–4 hearing loss compared to control (5.9% vs. 10.6%) |
| Luo et al., 2023 [47] | Lower radiation dose to GTV (60 Gy) for patients with stage IVA–IVB (AJCC 7th edition) NPC who achieved tumor response after induction chemotherapy; those with SD or PD received the standard dose (70 Gy) | 44 | 38.2 | CTCAE G1–2 hearing impairment 14%, G3–4 0% | |
| Guo et al., 2023 [48] | Lower radiation dose to GTV (60 Gy) for patients with stage III (AJCC 8th edition) NPC who had pre-treatment plasma EBV DNA <4000 copies/mL and achieved tumor response and undetectable plasma EBV DNA after induction chemotherapy; a 6 Gy boost to residual tumors at the end of treatment | 215 | 43.9 | RTOG G1–2 hearing impairment 14.7% vs. 41.4%, G3 hearing impairment 0% vs. 1% | |
| Individualizing cochlea dose constraints | |||||
| Zhang et al., 2019 [49] | Based on T-stage, a cochlea-sparing plan was designed by individualizing dose constraints, and/or upgrading cochlea protection weight, and/or changing radiation beams angles | 19 | N/A | Significantly lower ipsilateral cochlear Dmean (46.2 Gy vs. 50.6 Gy) and contralateral cochlear Dmean (43.9 Gy vs. 49.9 Gy) compared to standard plans | |
| Radiotherapy techniques | |||||
| Volumetric-modulated arc therapy | Gao et al., 2015 [50] | VMAT plan with the SmartArc planning algorithm in stage III or IV NPC | 20 | N/A | Significantly lower cochlear Dmean (42.7–43.8 Gy) than the control IMRT plan (47.6–47.8 Gy) |
| He et al., 2020 [51] | VMAT plan in stage I–IVB NPC | 627 | ≥12 | Significantly lower cochlear Dmean in T3–4 tumor (45.08 Gy vs. 46.31 Gy) and lower ototoxicity (G1–2 16.4% vs. 25.1%, G3–4 0.9% vs. 3.1%) than the control IMRT plan | |
| Lamaj et al., 2021 [52] | VMAT with jaw tracking to ensure the cochlea would remain outside the treatment field whenever possible, or as as close to the cochlea as possible if very close to the PTV | 20 | N/A | Significantly lower cochlear Dmean (14.97–18.47 Gy vs. 24.09–26.05 Gy) than the control plan | |
| Nanda et al., 2023 [53] | VMAT plan in stage III or IV NPC | 14 | N/A | Significantly lower cochlear Dmean (38.05–38.26 Gy vs. 42.13–43.16 Gy) than the control IMRT plan | |
| Proton therapy | Jiri et al., 2021 [54] | Three-field pencil-beam scanning IMPT with adaptive re-planning | 40 | 24 | RTOG G2 ototoxicity 7%, G3 or above 0% |
| Williams et al., 2021 [55] | Two- to five-field pencil-beam scanning IMPT | 26 | 25 | CTCAE G1 hearing impairment 27%, G2 4%, ≥G3 0% | |
| Anderson et al., 2023 [56] | Pencil-beam scanning proton therapy | 32 | 30 | Significantly lower cochlear Dmean at the less spared side (33.2 Gy vs. 41.8 Gy) and better spared side (25.5 Gy vs. 31.5 Gy) than the control IMRT/VMAT plan | |
| De-escalating systemic therapy | |||||
| Omission of concurrent cisplatin | Tang et al., 2022 [57] | Omit concurrent cisplatin in low-risk NPC, defined as stage II or T3N0M0 (AJCC 7th edition) without adverse features (all lymph nodes <3 cm, no level IV/VB involvement, no ECE, plasma EBV DNA level <4000 copies/mL) | 341 | 46 | RTOG G1–2 hearing impairment 40% vs. 47%, G3–4 1% vs. 1% compared to control group |
| Alternative cisplatin schedule | Li et al., 2022 [58] | Reduce cumulative cisplatin dose by using 2 cycles of concurrent cisplatin (100 mg/m2 every 3 weeks) instead of 3 cycles, in low-risk locally advanced NPC as defined by stages III to IVB (AJCC 7th edition) and plasma EBV DNA <4000 copies/mL | 332 | 37.7 | Lower rates of RTOG hearing impairment of any grade, 22.9% vs. 35.2%, and G3–4 hearing impairment, 0.6% vs. 3.6% |
| Alternative concurrent agent other than cisplatin | Tang et al., 2018 [59] | Use of nedaplatin as the concurrent agent with IMRT | 402 | 48 | Lower rates of RTOG hearing impairment of any grade, 14% vs. 23%, and G3, 2% vs. 6% |
| Lv et al., 2019 [60] | Use of oral S-1 as the concurrent agent with IMRT in locally advanced NPC | 131 | 24.5 | RTOG G1 hearing impairment 2.3%, G2 or above 0% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, J.C.S.; Ma, B.B.Y.; Chow, J.C.H. Optimizing Hearing Outcomes in Nasopharyngeal Cancer Survivors in the Era of Modern Radiotherapy and Systemic Therapy. Cancers 2024, 16, 3237. https://doi.org/10.3390/cancers16183237
Ho JCS, Ma BBY, Chow JCH. Optimizing Hearing Outcomes in Nasopharyngeal Cancer Survivors in the Era of Modern Radiotherapy and Systemic Therapy. Cancers. 2024; 16(18):3237. https://doi.org/10.3390/cancers16183237
Chicago/Turabian StyleHo, Jason C. S., Brigette B. Y. Ma, and James C. H. Chow. 2024. "Optimizing Hearing Outcomes in Nasopharyngeal Cancer Survivors in the Era of Modern Radiotherapy and Systemic Therapy" Cancers 16, no. 18: 3237. https://doi.org/10.3390/cancers16183237
APA StyleHo, J. C. S., Ma, B. B. Y., & Chow, J. C. H. (2024). Optimizing Hearing Outcomes in Nasopharyngeal Cancer Survivors in the Era of Modern Radiotherapy and Systemic Therapy. Cancers, 16(18), 3237. https://doi.org/10.3390/cancers16183237







