Molecular Characterization and Xenotransplantation of Pancreatic Cancer Using Endoscopic Ultrasound-Guided Fine Needle Aspiration (EUS-FNA)
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Sample Size Calculation
2.3. EUS-FNA
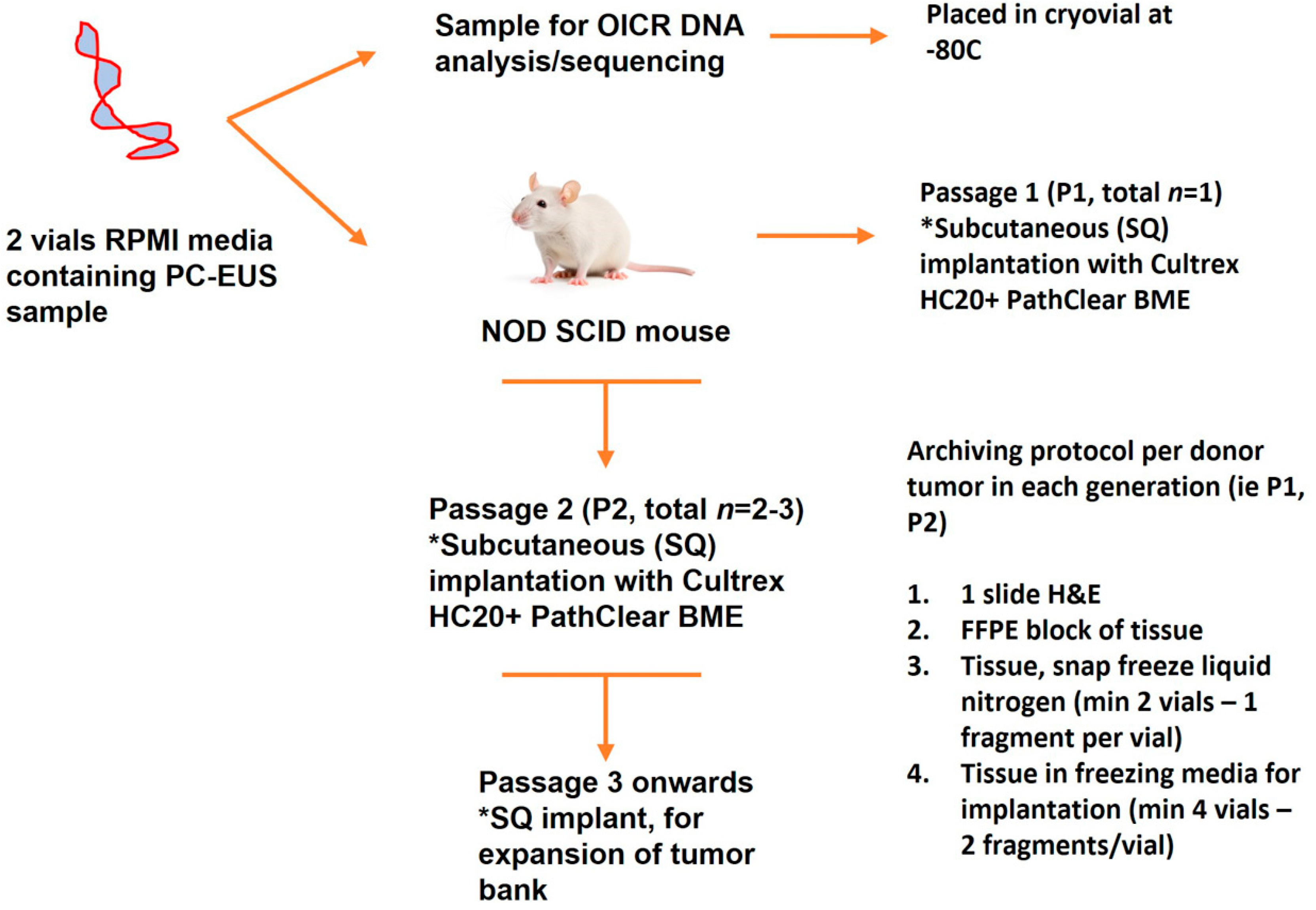
2.4. Xenotransplantation
2.5. Sample Purity
2.6. Histologic Characterization and Immunohistochemistry of Xenograft Samples
2.7. Genetic Analysis
2.8. Virus, Tumor Core Infection and Plaque Assays
3. Results
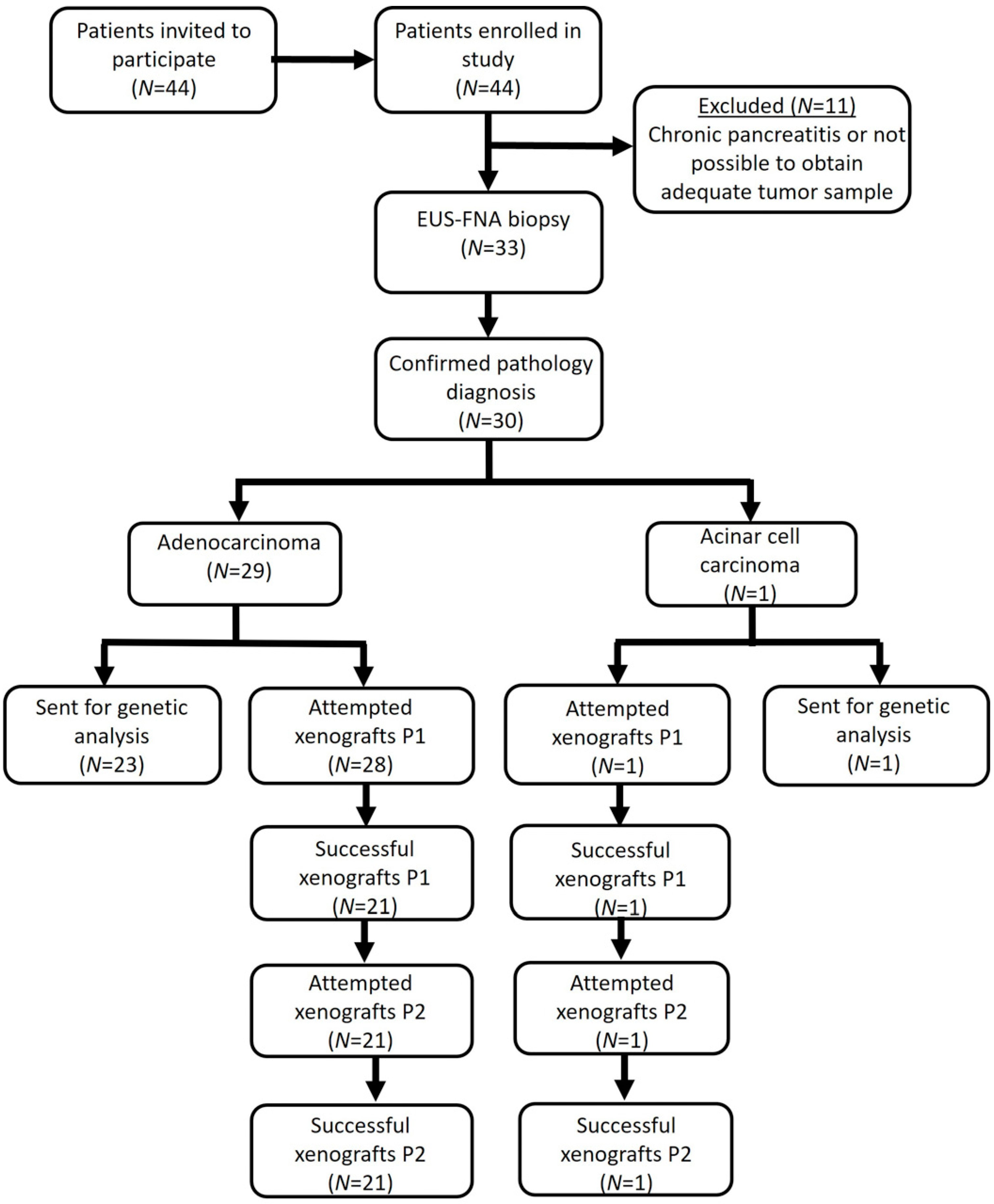
3.1. Patient Characteristics
3.2. EUS-FNA
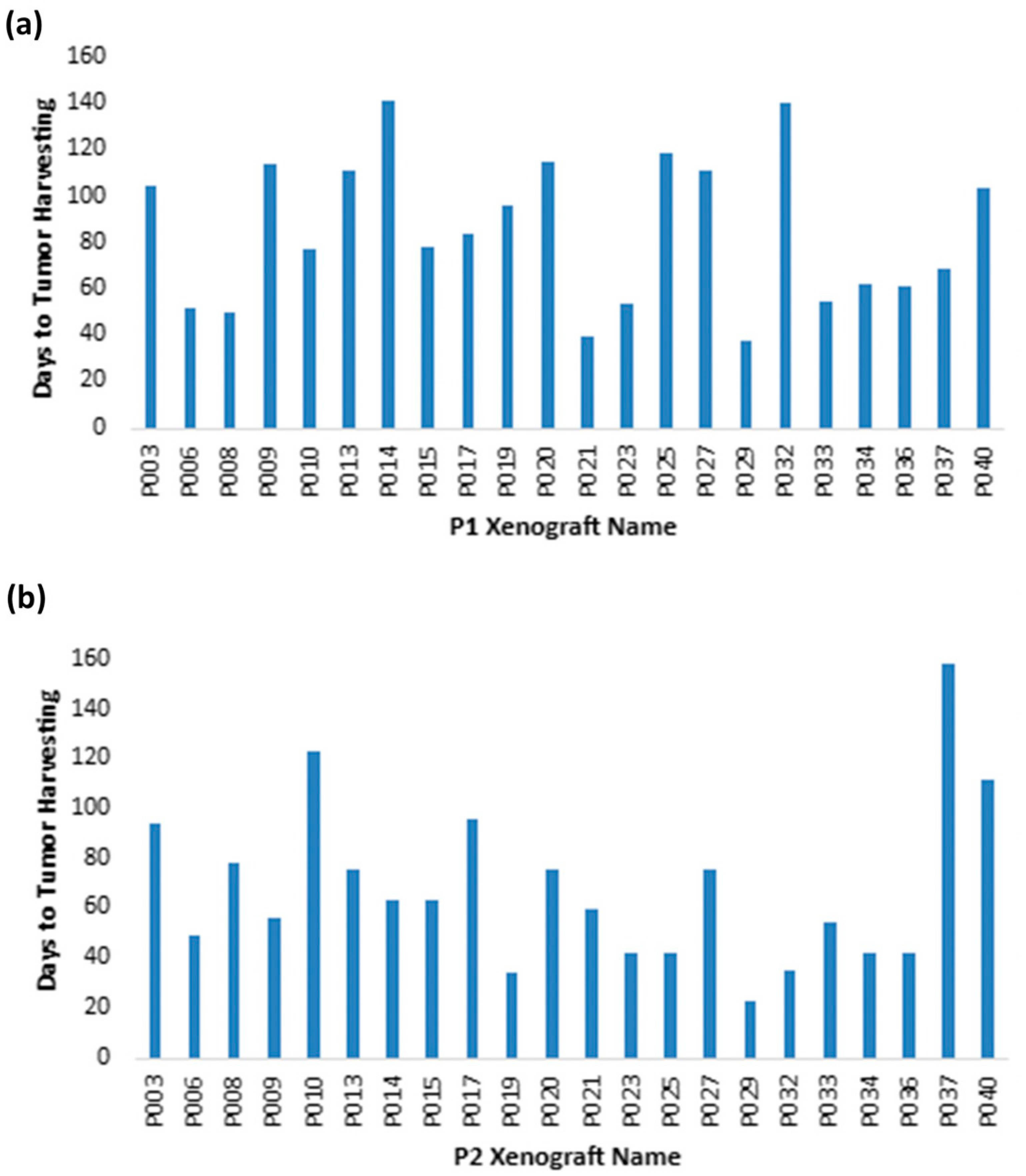
3.3. Generation of a Pancreatic Tumor Graft Biobank
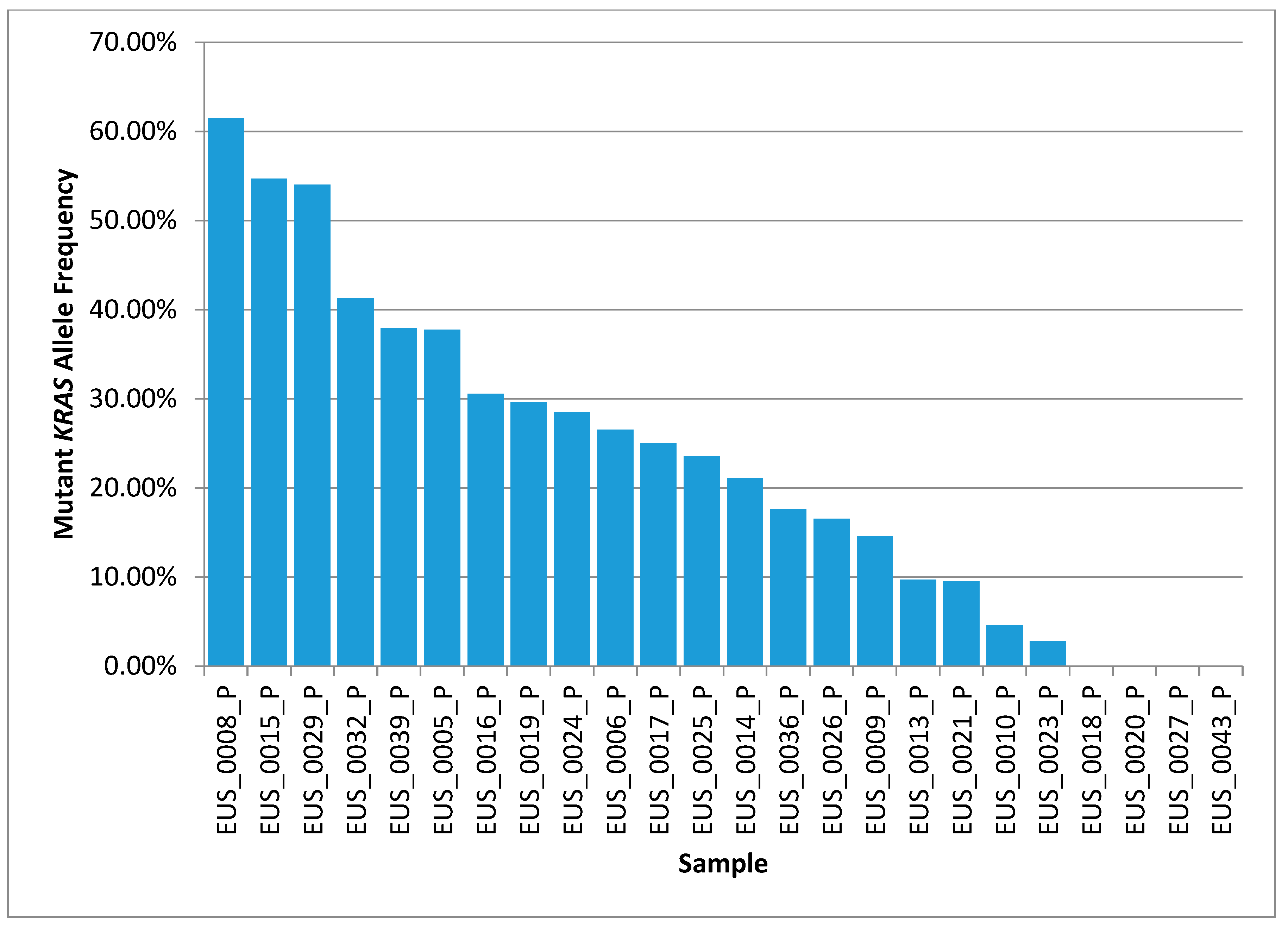
3.4. Genetic Sequencing Feasibility
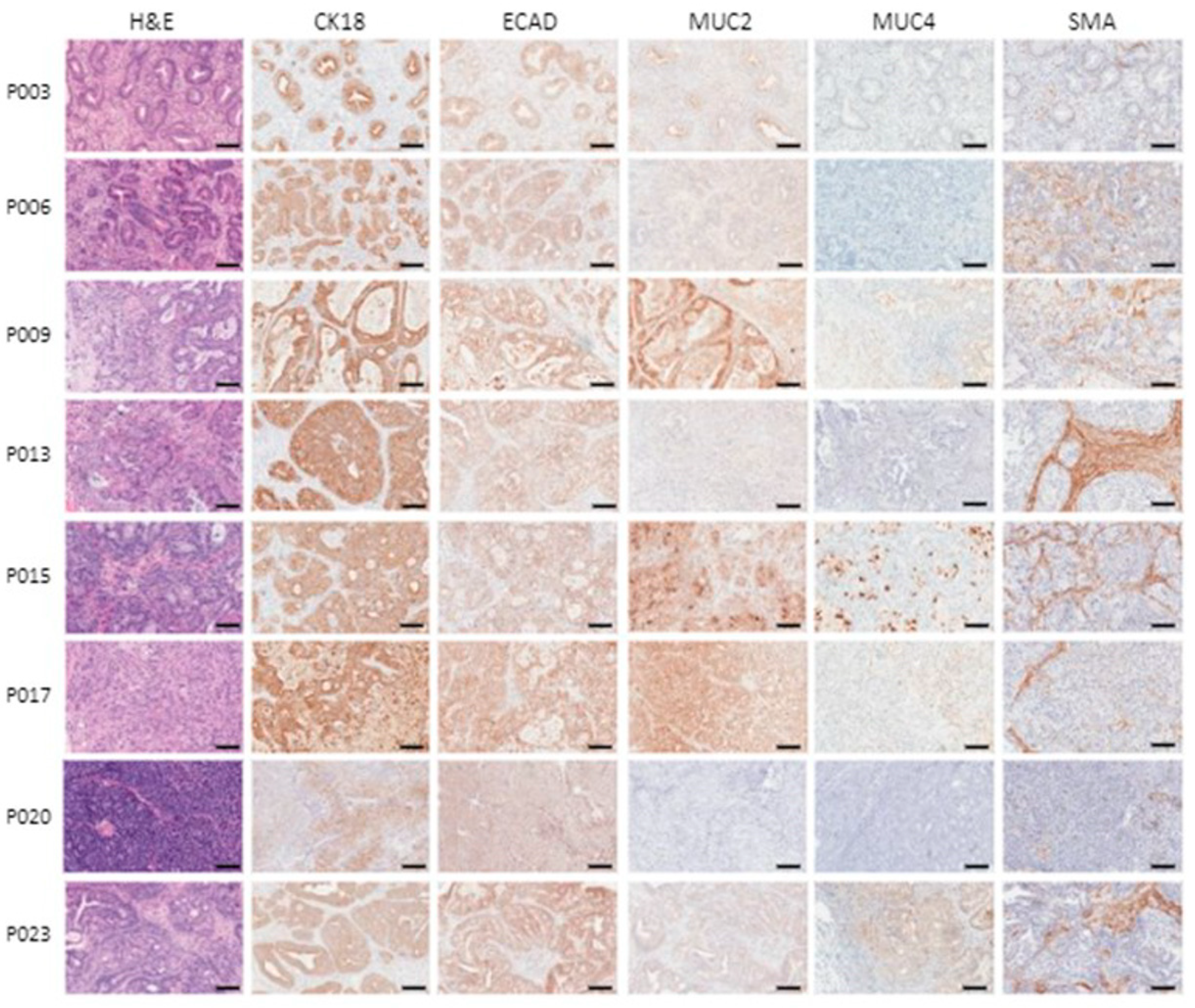
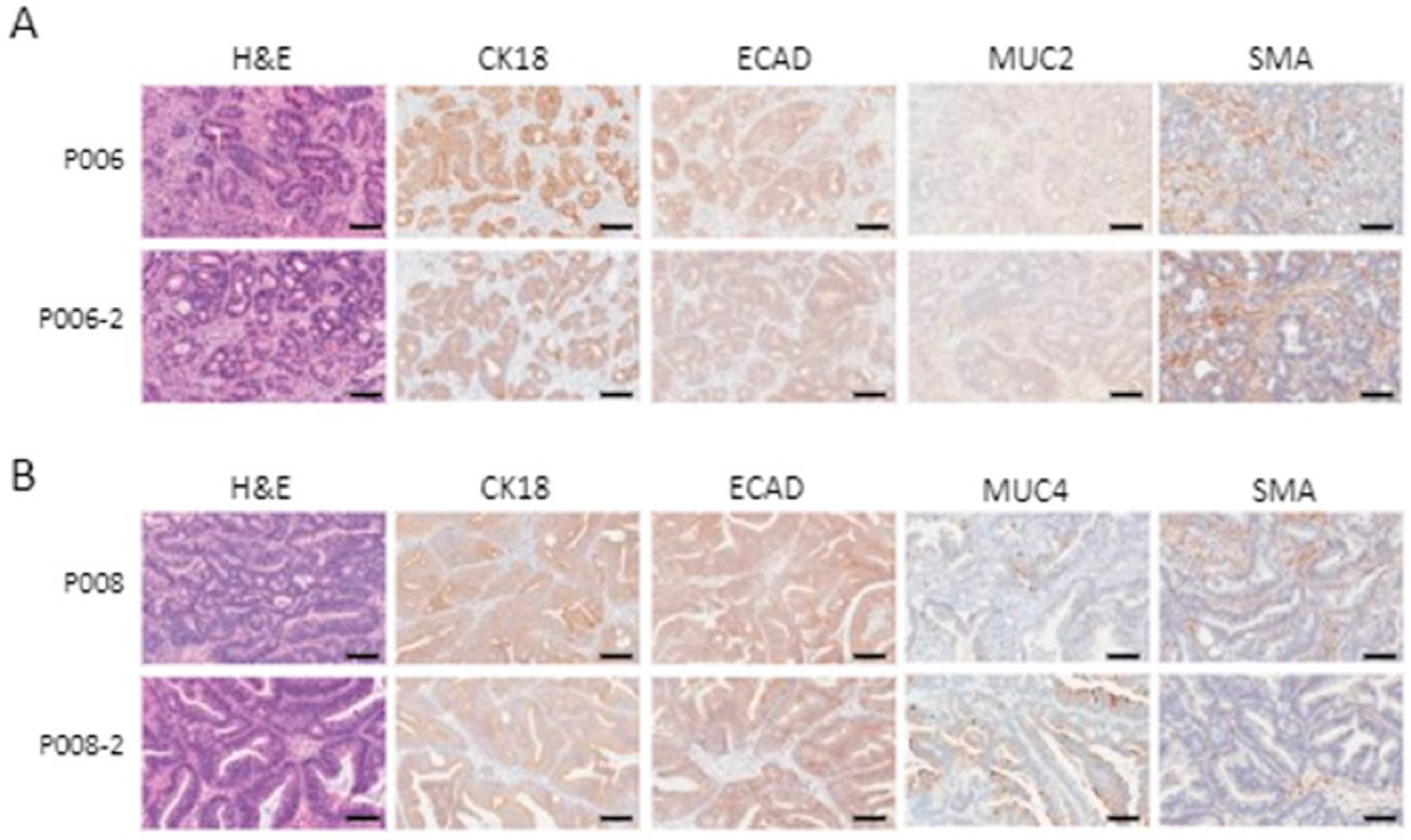
3.5. Patient-Derived Xenografts Express Pancreatic Cancer Markers and Retain Their Histological Characteristics after Passaging
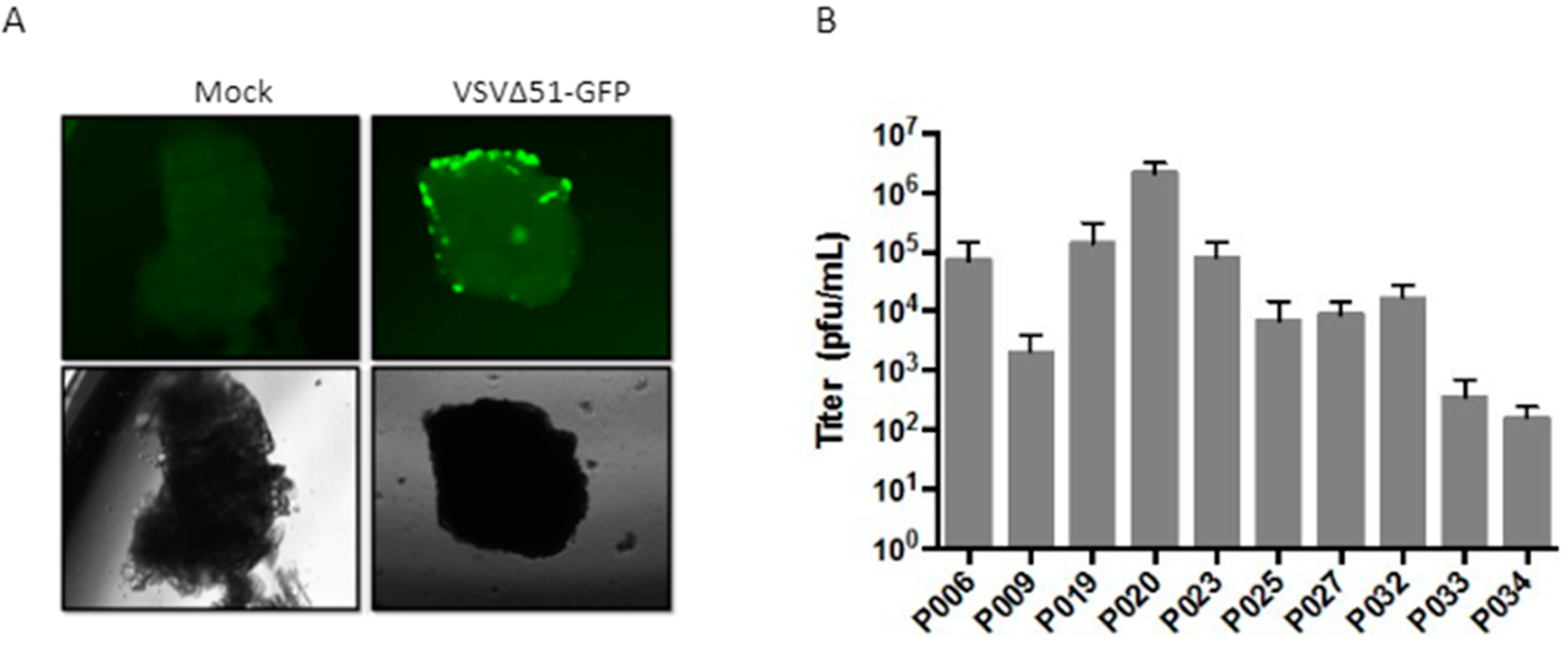
3.6. Patient-Derived Xenograft Models Can Be Used to Evaluate Oncolytic Virotherapy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute. Cancer Stat Facts: Pancreatic Cancer. Available online: https://seer.cancer.gov/statfacts/html/common.html (accessed on 29 December 2021).
- Citterio, C.; Baccini, M.; Orlandi, E.; Di Nunzio, C.; Cavanna, L. Second-line chemotherapy for the treatment of metastatic pancreatic cancer after first-line gemcitabine-based chemotherapy: A network meta-analysis. Oncotarget 2018, 9, 29801–29809. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Berry, W.; Lundy, J.; Croagh, D.; Jenkins, B.J. Reviewing the Utility of EUS FNA to Advance Precision Medicine in Pancreatic Cancer. Cancers 2018, 10, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Romanelli, A.; Clark, A.; Assayag, F.; Chateau-Joubert, S.; Poupon, M.F.; Servely, J.L.; Fontaine, J.J.; Liu, X.; Spooner, E.; Goodstal, S.; et al. Inhibiting aurora kinases reduces tumor growth and suppresses tumor recurrence after chemotherapy in patient-derived triple-negative breast cancer xenografts. Mol. Cancer Ther. 2012, 11, 2693–2703. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, M.; Amant, F.; Biankin, A.V.; Budinská, E.; Byrne, A.T.; Caldas, C.; Clarke, R.B.; de Jong, S.; Jonkers, J.; Mælandsmo, G.M.; et al. Patient-derived xenograft models: An emerging platform for translational cancer research. Cancer Discov. 2014, 4, 998–1013. [Google Scholar] [CrossRef] [PubMed]
- Laheru, D.; Shah, P.; Rajeshkumar, N.V.; McAllister, F.; Taylor, G.; Goldsweig, H.; Le, D.T.; Donehower, R.; Jimeno, A.; Linden, S.; et al. Integrated preclinical and clinical development of S-trans, trans-Farnesylthiosalicylic Acid (FTS, Salirasib) in pancreatic cancer. Investig. New Drugs 2012, 30, 2391–2399. [Google Scholar] [CrossRef] [PubMed]
- Guenot, D.; Guérin, E.; Aguillon-Romain, S.; Pencreach, E.; Schneider, A.; Neuville, A.; Chenard, M.P.; Duluc, I.; Du Manoir, S.; Brigand, C.; et al. Primary tumor genetic alterations and intra-tumoral heterogeneity are maintained in xenografts of human colon cancers showing chromosome instability. J. Pathol. 2006, 208, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Krumbach, R.; Schüler, J.; Hofmann, M.; Giesemann, T.; Fiebig, H.H.; Beckers, T. Primary resistance to cetuximab in a panel of patient-derived tumor xenograft models: Activation of MET as one mechanism for drug resistance. Eur. J. Cancer 2011, 47, 1231–1243. [Google Scholar] [CrossRef] [PubMed]
- Meijer, T.G.; Naipal, K.A.; Jager, A.; van Gent, D.C. Ex. vivo tumor culture systems for functional drug testing and therapy response prediction. Future Sci. OA 2017, 3, FSO190. [Google Scholar] [CrossRef]
- Kandel, P.; Wallace, M.B. Advanced EUS Guided Tissue Acquisition Methods for Pancreatic Cancer. Cancers 2018, 10, 54. [Google Scholar] [CrossRef]
- Campbell, P.J.; Yachida, S.; Mudie, L.J.; Stephens, P.J.; Pleasance, E.D.; Stebbings, L.; Morsberger, L.A.; Latimer, C.; McLaren, S.; Lin, M.L.; et al. The patterns and dynamics of genomic instability in metastatic pancreatic cancer. Nature 2010, 467, 1109–1113. [Google Scholar] [CrossRef] [PubMed]
- Voss, M.; Hammel, P.; Molas, G.; Palazzo, L.; Dancour, A.; O’Toole, D.; Terris, B.; Degott, C.; Bernades, P.; Ruszniewski, P. Value of endoscopic ultrasound guided fine needle aspiration biopsy in the diagnosis of solid pancreatic masses. Gut 2000, 46, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Bayan, C.Y.; Lopez, A.T.; Gartrell, R.D.; Komatsubara, K.M.; Bogardus, M.; Rao, N.; Chen, C.; Hart, T.D.; Enzler, T.; Rizk, E.M.; et al. The Role of Oncolytic Viruses in the Treatment of Melanoma. Curr. Oncol. Rep. 2018, 20, 80. [Google Scholar] [CrossRef] [PubMed]
- Bang, J.Y.; Magee, S.H.; Ramesh, J.; Trevino, J.M.; Varadarajulu, S. Randomized trial comparing fanning with standard technique for endoscopic ultrasound-guided fine-needle aspiration of solid pancreatic mass lesions. Endoscopy 2013, 45, 445–450. [Google Scholar] [CrossRef]
- Weng, Y.R.; Cui, Y.; Fang, J.Y. Biological functions of cytokeratin 18 in cancer. Mol. Cancer Res. 2012, 10, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Wells, A.; Yates, C.; Shepard, C.R. E-cadherin as an indicator of mesenchymal to epithelial reverting transitions during the metastatic seeding of disseminated carcinomas. Clin. Exp. Metastasis 2008, 25, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Guilford, P. E-cadherin downregulation in cancer: Fuel on the fire? Mol. Med. Today 1999, 5, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Jonckheere, N.; Skrypek, N.; Van Seuningen, I. Mucins and pancreatic cancer. Cancers 2010, 2, 1794–1812. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaur, S.; Kumar, S.; Momi, N.; Sasson, A.R.; Batra, S.K. Mucins in pancreatic cancer and its microenvironment. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 607–620. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, K.; Li, M.; Hakonarson, H. ANNOVAR: Functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010, 38, e164. [Google Scholar] [CrossRef]
- Adzhubei, I.A.; Schmidt, S.; Peshkin, L.; Ramensky, V.E.; Gerasimova, A.; Bork, P.; Kondrashov, A.S.; Sunyaev, S.R. A method and server for predicting damaging missense mutations. Nat. Methods 2010, 7, 248–249. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ng, P.C.; Henikoff, S. Predicting deleterious amino acid substitutions. Genome Res. 2001, 11, 863–874. [Google Scholar] [CrossRef] [PubMed]
- Xi, T.; Jones, I.M.; Mohrenweiser, H.W. Many amino acid substitution variants identified in DNA repair genes during human population screenings are predicted to impact protein function. Genomics 2004, 83, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Stojdl, D.F.; Lichty, B.D.; tenOever, B.R.; Paterson, J.M.; Power, A.T.; Knowles, S.; Marius, R.; Reynard, J.; Poliquin, L.; Atkins, H.; et al. VSV strains with defects in their ability to shutdown innate immunity are potent systemic anti-cancer agents. Cancer Cell 2003, 4, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Diallo, J.S.; Roy, D.; Abdelbary, H.; De Silva, N.; Bell, J.C. Ex vivo infection of live tissue with oncolytic viruses. J. Vis. Exp. 2011, 52, 2854. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ilkow, C.S.; Marguerie, M.; Batenchuk, C.; Mayer, J.; Ben Neriah, D.; Cousineau, S.; Falls, T.; Jennings, V.A.; Boileau, M.; Bellamy, D.; et al. Reciprocal cellular cross-talk within the tumor microenvironment promotes oncolytic virus activity. Nat. Med. 2015, 21, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Berry, W.; Algar, E.; Kumar, B.; Desmond, C.; Swan, M.; Jenkins, B.J.; Croagh, D. Endoscopic ultrasound-guided fine-needle aspirate-derived preclinical pancreatic cancer models reveal panitumumab sensitivity in KRAS wild-type tumors. Int. J. Cancer 2017, 140, 2331–2343. [Google Scholar] [CrossRef] [PubMed]
- Allaway, R.J.; Fischer, D.A.; de Abreu, F.B.; Gardner, T.B.; Gordon, S.R.; Barth, R.J.; Colacchio, T.A.; Wood, M.; Kacsoh, B.Z.; Bouley, S.J.; et al. Genomic characterization of patient-derived xenograft models established from fine needle aspirate biopsies of a primary pancreatic ductal adenocarcinoma and from patient-matched metastatic sites. Oncotarget 2016, 7, 17087–17102. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, J.K.; Choi, J.H.; Lee, K.H.; Kim, K.M.; Shin, J.U.; Lee, J.K.; Lee, K.T.; Jang, K.T. A prospective, comparative trial to optimize sampling techniques in EUS-guided FNA of solid pancreatic masses. Gastrointest. Endosc. 2013, 77, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Liu, E.; Sun, S. Rapid on-site evaluation (ROSE) with EUS-FNA: The ROSE looks beautiful. Endosc. Ultrasound 2019, 8, 283–287. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Facciorusso, A.; Mohan, B.P.; Crinò, S.F.; Ofosu, A.; Ramai, D.; Lisotti, A.; Chandan, S.; Fusaroli, P. Contrast-enhanced harmonic endoscopic ultrasound-guided fine-needle aspiration versus standard fine-needle aspiration in pancreatic masses: A meta-analysis. Expert. Rev. Gastroenterol. Hepatol. 2021, 15, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Haeberle, L.; Esposito, I. Pathology of pancreatic cancer. Transl. Gastroenterol. Hepatol. 2019, 4, 50. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, K.H.; Kim, E.Y.; Cho, J.; Kang, D.; Bang, S.; Kim, H.K.; Kim, G.H.; Choi, H.J.; Han, J.H.; Jeon, S.W.; et al. Risk factors associated with adverse events during endoscopic ultrasound-guided tissue sampling. PLoS ONE 2017, 12, e0189347. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hermans, E.; Van der Merwe, S.W.; Depreeuw, J.; Dekervel, J.; Radaelli, E.; Roskams, T.; van Pelt Jos, J.; Topal, B.; Verslype, C.; Prenen, H.; et al. Successful application of endoscopic ultrasound-guided fine needle biopsy to establish pancreatic patient-derived tumor xenografts: A pilot study. Endoscopy 2016, 48, 1016–1022. [Google Scholar] [CrossRef] [PubMed]
- Nakaoka, K.; Ohno, E.; Kawabe, N.; Kuzuya, T.; Funasaka, K.; Nakagawa, Y.; Nagasaka, M.; Ishikawa, T.; Watanabe, A.; Tochio, T.; et al. Current Status of the Diagnosis of Early-Stage Pancreatic Ductal Adenocarcinoma. Diagnostics 2023, 13, 215. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Park, J.K.; Lee, K.H. Present and Future of Endoscopic Ultrasound-Guided Tissue Acquisition in Solid Pancreatic Tumors. Clin. Endosc. 2019, 52, 541–548. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dahiya, D.S.; Shah, Y.R.; Ali, H.; Chandan, S.; Gangwani, M.K.; Canakis, A.; Ramai, D.; Hayat, U.; Pinnam, B.S.M.; Iqbal, A.; et al. Basic Principles and Role of Endoscopic Ultrasound in Diagnosis and Differentiation of Pancreatic Cancer from Other Pancreatic Lesions: A Comprehensive Review of Endoscopic Ultrasound for Pancreatic Cancer. J. Clin. Med. 2024, 13, 2599. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, J.; Zhao, S.; Chen, Y.; Jia, R.; Zhang, X. Endoscopic ultrasound guided fine needle aspiration versus endoscopic ultrasound guided fine needle biopsy in sampling pancreatic masses: A meta-analysis. Medicine 2017, 96, e7452. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Z.; Liu, W.; Xu, X.; Li, P. A Meta-Analysis Comparing Endoscopic Ultrasound-guided Fine-needle Aspiration With Endoscopic Ultrasound-guided Fine-needle Biopsy. J. Clin. Gastroenterol. 2022, 56, 668–678. [Google Scholar] [CrossRef] [PubMed]
- Vanbiervliet, G.; Napoléon, B.; Saint Paul, M.C.; Sakarovitch, C.; Wangermez, M.; Bichard, P.; Subtil, C.; Koch, S.; Grandval, P.; Gincul, R.; et al. Core needle versus standard needle for endoscopic ultrasound-guided biopsy of solid pancreatic masses: A randomized crossover study. Endoscopy 2014, 46, 1063–1070. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Tang, A.L.; Zhang, L.; Liu, X.W.; Li, J.B.; Wang, F.; Shen, S.R.; Wang, X.Y. Evaluation of 22G fine-needle aspiration (FNA) versus fine-needle biopsy (FNB) for endoscopic ultrasound-guided sampling of pancreatic lesions: A prospective comparison study. Surg. Endosc. 2018, 32, 3533–3539, Erratum in Surg Endosc. 2018, 32, 4706. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gan, Q.; Roy-Chowdhuri, S.; Duose, D.Y.; Stewart, J.M.; Coronel, E.; Bhutani, M.S.; Lee, J.H.; Weston, B.; Ge, P.S.; Ross, W.A.; et al. Adequacy evaluation and use of pancreatic adenocarcinoma specimens for next-generation sequencing acquired by endoscopic ultrasound-guided FNA and FNB. Cancer Cytopathol. 2022, 130, 275–283. [Google Scholar] [CrossRef] [PubMed]
- DeRose, Y.S.; Gligorich, K.M.; Wang, G.; Georgelas, A.; Bowman, P.; Courdy, S.J.; Welm, A.L.; Welm, B.E. Patient-derived models of human breast cancer: Protocols for in vitro and in vivo applications in tumor biology and translational medicine. Curr. Protoc. Pharmacol. 2013, 60, 14.23.1–14.23.43. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leong, T.L.; Marini, K.D.; Rossello, F.J.; Jayasekara, S.N.; Russell, P.A.; Prodanovic, Z.; Kumar, B.; Ganju, V.; Alamgeer, M.; Irving, L.B.; et al. Genomic characterisation of small cell lung cancer patient-derived xenografts generated from endobronchial ultrasound-guided transbronchial needle aspiration specimens. PLoS ONE 2014, 9, e106862. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Peng, S.; Creighton, C.J.; Zhang, Y.; Sen, B.; Mazumdar, T.; Myers, J.N.; Lai, S.Y.; Woolfson, A.; Lorenzi, M.V.; Bell, D.; et al. Tumor grafts derived from patients with head and neck squamous carcinoma authentically maintain the molecular and histologic characteristics of human cancers. J. Transl. Med. 2013, 11, 198, Erratum in J. Transl. Med. 2014, 12, 67. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Felsenstein, M.; Hruban, R.H.; Wood, L.D. New Developments in the Molecular Mechanisms of Pancreatic Tumorigenesis. Adv. Anat. Pathol. 2018, 25, 131–142. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zaman, A.; Wu, W.; Bivona, T.G. Targeting Oncogenic BRAF: Past, Present, and Future. Cancers 2019, 11, 1197. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Waters, A.M.; Der, C.J. KRAS: The Critical Driver and Therapeutic Target for Pancreatic Cancer. Cold Spring Harb. Perspect. Med. 2018, 8, a031435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Duffy, M.J.; Synnott, N.C.; O’Grady, S.; Crown, J. Targeting p53 for the treatment of cancer. Semin. Cancer Biol. 2022, 79, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Fiorini, C.; Cordani, M.; Padroni, C.; Blandino, G.; Di Agostino, S.; Donadelli, M. Mutant p53 stimulates chemoresistance of pancreatic adenocarcinoma cells to gemcitabine. Biochim. Biophys. Acta 2015, 1853, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Sinn, M.; Sinn, B.V.; Treue, D.; Keilholz, U.; Damm, F.; Schmuck, R.; Lohneis, P.; Klauschen, F.; Striefler, J.K.; Bahra, M.; et al. TP53 Mutations Predict Sensitivity to Adjuvant Gemcitabine in Patients with Pancreatic Ductal Adenocarcinoma: Next-Generation Sequencing Results from the CONKO-001. Trial. Clin. Cancer Res. 2020, 26, 3732–3739. [Google Scholar] [CrossRef] [PubMed]
- Abraham, S.C.; Wu, T.T.; Hruban, R.H.; Lee, J.H.; Yeo, C.J.; Conlon, K.; Brennan, M.; Cameron, J.L.; Klimstra, D.S. Genetic and immunohistochemical analysis of pancreatic acinar cell carcinoma: Frequent allelic loss on chromosome 11p and alterations in the APC/beta-catenin pathway. Am. J. Pathol. 2002, 160, 953–962. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Hader, A.; Al-Rohil, R.N.; Han, H.; Von Hoff, D. Pancreatic acinar cell carcinoma: A review on molecular profiling of patient tumors. World J. Gastroenterol. 2017, 23, 7945–7951. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reale, A.; Vitiello, A.; Conciatori, V.; Parolin, C.; Calistri, A.; Palù, G. Perspectives on immunotherapy via oncolytic viruses. Infect. Agent. Cancer 2019, 14, 5. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hammerich, L.; Binder, A.; Brody, J.D. In situ vaccination: Cancer immunotherapy both personalized and off-the-shelf. Mol. Oncol. 2015, 9, 1966–1981. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Achard, C.; Surendran, A.; Wedge, M.E.; Ungerechts, G.; Bell, J.; Ilkow, C.S. Lighting a Fire in the Tumor Microenvironment Using Oncolytic Immunotherapy. EBioMedicine 2018, 31, 17–24. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maleki Vareki, S. High and low mutational burden tumors versus immunologically hot and cold tumors and response to immune checkpoint inhibitors. J. Immunother. Cancer. 2018, 6, 157. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Variables | Value | % |
|---|---|---|
| Demographics | ||
| Gender | M—19 | 63.3 |
| F—11 | 36.7 | |
| Average Age | M: 65.1 | NA |
| F: 75.5 | NA | |
| Symptoms | ||
| Weight Loss | Y—25 | 83 |
| N—5 | 17 | |
| Jaundice | Y—9 | 30 |
| N—21 | 70 | |
| Abdominal Pain | Y—23 | 77 |
| N—7 | 23 | |
| Health History | ||
| Previous Cancer Diagnosis | Y—4 | 13 |
| N—26 | 87 | |
| Familial Pancreatic Cancer History | Y—3 | 10 |
| N—27 | 90 | |
| If Yes: Associated degree | First Degree—1 | 33.3 |
| Second Degree—2 | 66.6 | |
| Third Degree—0 | 0 | |
| Acute Pancreatitis | Y—1 | 3 |
| N—29 | 97 | |
| Diabetic | Y—7 | 23 |
| N—23 | 77 | |
| Lifestyle Factors | ||
| Smoking History | Y—6 | 20 |
| N—24 | 80 | |
| Alcohol Consumption | Y—14 | 47 |
| N—16 | 53 | |
| Disease Risk Category | ||
| Low Risk | 11 | 37 |
| Increased Risk | 4 | 13 |
| High Risk | 0 | 0 |
| No Risk | 15 | 50 |
| Disease Characteristics | ||
| Stage | Locally advanced—27 | 90 |
| Metastatic—3 | 10 | |
| Tumor Type | Adenocarcinoma—29 | 96.7 |
| Acinar cell carcinoma—1 | 3.3 | |
| Tumor Characteristics | Well differentiated—18 | 60 |
| Moderately differentiated—10 | 33.3 | |
| Poorly differentiated—2 | 6.7 | |
| Outcomes | ||
| Adverse events | None—30 | 100 |
| Concerns—0 | 0 | |
| Clinical Outcome | Surgery—2 | 6.6 |
| Chemotherapy—19 | 63.3 | |
| Radiation—0 | 0 | |
| No therapy—10 | 33.3 | |
| Chromosome | Position | Ref | Alt | Prediction | Gene | Consequence | Times Called | PolyPhen-2 | SIFT | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| chr3 | 10188328 | C | T | Likely Somatic | VHL | intronic | 1 | Not found | N/A | Not found | N/A |
| chr3 | 178952085 | A | G | Likely Somatic | PIK3CA | nonsynonymous SNV * | 1 | Not found | N/A | 0.136 | Borderline |
| chr3 | 37083758 | G | C | Potentially Somatic | MLH1 | splicing | 1 | Not found | N/A | Not found | N/A |
| chr3 | 37090070 | G | T | Likely Somatic | MLH1 | synonymous SNV | 3 | Not found | N/A | 1 | Tolerant |
| chr3 | 37092176 | C | T | Potentially Somatic | MLH1 | UTR3 | 1 | Not found | N/A | Not found | N/A |
| chr4 | 1805639 | A | G | Potentially Somatic | FGFR3 | intronic | 1 | Not found | N/A | Not found | N/A |
| chr4 | 55161348 | T | A | Potentially Somatic | PDGFRA | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr4 | 55593481 | A | G | Likely Somatic | KIT | synonymous SNV | 1 | Not found | N/A | 1 | Tolerant |
| chr5 | 112174456 | A | T | Potentially Somatic | APC | synonymous SNV | 2 | Not found | N/A | 1 | Tolerant |
| chr5 | 112175240 | G | C | Likely Somatic | APC | nonsynonymous SNV | 1 | 0.001 | Benign | 0.11 | Borderline |
| chr7 | 116339642 | G | T | Likely Somatic | MET | nonsynonymous SNV | 1 | Not found | N/A | 0.16 | Borderline |
| chr7 | 116411990 | C | T | Likely Somatic | MET | nonsynonymous SNV | 1 | 0.999 | Probably damaging | 0.03 | Intolerant |
| chr7 | 140453136 | A | C | Likely Somatic | BRAF | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr7 | 140453136 | A | T | Likely Somatic | BRAF | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr7 | 140453137 | C | T | Likely Somatic | BRAF | nonsynonymous SNV | 1 | Not found | N/A | 0.02 | Intolerant |
| chr7 | 140481393 | T | C | Likely Somatic | BRAF | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr7 | 55268949 | A | G | Potentially Somatic | EGFR | synonymous SNV | 1 | Not found | N/A | 1 | Tolerant |
| chr8 | 42174380 | G | A | Potentially Somatic | IKBKB | synonymous SNV | 1 | Not found | N/A | 1 | Tolerant |
| chr9 | 139397728 | C | T | Potentially Somatic | NOTCH1 | synonymous SNV | 1 | Not found | N/A | 0.563 | Tolerant |
| chr10 | 43597827 | C | A | Potentially Somatic | RET | synonymous SNV | 1 | Not found | N/A | 1 | Tolerant |
| chr10 | 89690764 | A | G | Likely Somatic | PTEN | intronic | 1 | Not found | N/A | Not found | N/A |
| chr12 | 25380275 | T | G | Likely Somatic | KRAS | nonsynonymous SNV | 1 | 0.142 | Benign | 0.002 | Intolerant |
| chr12 | 25398284 | C | A | Likely Somatic | KRAS | nonsynonymous SNV | 8 | Not found | N/A | Not found | N/A |
| chr12 | 25398284 | C | T | Likely Somatic | KRAS | nonsynonymous SNV | 4 | Not found | N/A | Not found | N/A |
| chr12 | 25398285 | C | A | Likely Somatic | KRAS | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr12 | 25398285 | C | G | Likely Somatic | KRAS | nonsynonymous SNV | 5 | Not found | N/A | Not found | N/A |
| chr13 | 32912008 | G | A | Potentially Somatic | BRCA2 | synonymous SNV | 1 | Not found | N/A | 1 | Tolerant |
| chr17 | 12028657 | G | A | Likely Somatic | MAP2K4 | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7577093 | C | G | Likely Somatic | TP53 | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7577120 | C | T | Likely Somatic | TP53 | nonsynonymous SNV | 1 | 0.985 | Probably damaging | Not found | N/A |
| chr17 | 7577124 | C | T | Likely Somatic | TP53 | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7577127 | C | A | Likely Somatic | TP53 | stopgain SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7577130 | A | G | Likely Somatic | TP53 | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7577548 | C | T | Likely Somatic | TP53 | nonsynonymous SNV | 2 | 1 | Probably damaging | Not found | N/A |
| chr17 | 7578190 | T | C | Likely Somatic | TP53 | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7578217 | G | A | Likely Somatic | TP53 | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7578263 | G | A | Likely Somatic | TP53 | stopgain SNV | 1 | Not found | N/A | Not found | N/A |
| chr17 | 7578406 | C | T | Likely Somatic | TP53 | nonsynonymous SNV | 1 | 0.881 | Possibly damaging | Not found | N/A |
| chr18 | 48575202 | C | G | Potentially Somatic | SMAD4 | nonsynonymous SNV | 1 | Not found | N/A | Not found | N/A |
| chr21 | 36259324 | A | G | Likely Somatic | RUNX1 | nonsynonymous SNV | 2 | Not found | N/A | >0.4 | Tolerant |
| chr22 | 30067871 | G | A | Potentially Somatic | NF2 | synonymous SNV | 1 | Not found | N/A | >0.3 | Tolerant |
| chr22 | 30077428 | A | G | Potentially Somatic | NF2 | synonymous SNV | 1 | Not found | N/A | Not found | N/A |
| Type of Variant | Gene | Chromosome | Position | Reference | Variant | Consequence | PolyPhen-2 | SIFT | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Somatic | KRAS | chr12 | 25398284 | C | A | Nonsynonymous single-nucleotide variation | Not found | N/A | Not found | N/A |
| Somatic | KRAS | chr12 | 25398284 | C | T | Nonsynonymous single-nucleotide variation | Not found | N/A | Not found | N/A |
| Somatic | KRAS | chr12 | 25398285 | C | G | Nonsynonymous single-nucleotide variation | Not found | N/A | Not found | N/A |
| Somatic | TP53 | chr17 | 7578406 | C | T | Nonsynonymous single-nucleotide variation | 0.881 | Possibly damaging | Not found | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonova, L.; Paramanthan, P.; Falls, T.; Wedge, M.-E.; Mayer, J.; Sekhon, H.S.; McPherson, J.; Denroche, R.E.; Gallinger, S.; Bell, J.C.; et al. Molecular Characterization and Xenotransplantation of Pancreatic Cancer Using Endoscopic Ultrasound-Guided Fine Needle Aspiration (EUS-FNA). Cancers 2024, 16, 2721. https://doi.org/10.3390/cancers16152721
Antonova L, Paramanthan P, Falls T, Wedge M-E, Mayer J, Sekhon HS, McPherson J, Denroche RE, Gallinger S, Bell JC, et al. Molecular Characterization and Xenotransplantation of Pancreatic Cancer Using Endoscopic Ultrasound-Guided Fine Needle Aspiration (EUS-FNA). Cancers. 2024; 16(15):2721. https://doi.org/10.3390/cancers16152721
Chicago/Turabian StyleAntonova, Lilia, Piriya Paramanthan, Theresa Falls, Marie-Eve Wedge, Justin Mayer, Harman S. Sekhon, John McPherson, Robert E. Denroche, Steven Gallinger, John Cameron Bell, and et al. 2024. "Molecular Characterization and Xenotransplantation of Pancreatic Cancer Using Endoscopic Ultrasound-Guided Fine Needle Aspiration (EUS-FNA)" Cancers 16, no. 15: 2721. https://doi.org/10.3390/cancers16152721
APA StyleAntonova, L., Paramanthan, P., Falls, T., Wedge, M.-E., Mayer, J., Sekhon, H. S., McPherson, J., Denroche, R. E., Gallinger, S., Bell, J. C., Ilkow, C. S., & Chatterjee, A. (2024). Molecular Characterization and Xenotransplantation of Pancreatic Cancer Using Endoscopic Ultrasound-Guided Fine Needle Aspiration (EUS-FNA). Cancers, 16(15), 2721. https://doi.org/10.3390/cancers16152721






