Laser Therapy in Heavily Treated Oncological Patients Improves Vaginal Health Parameters
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
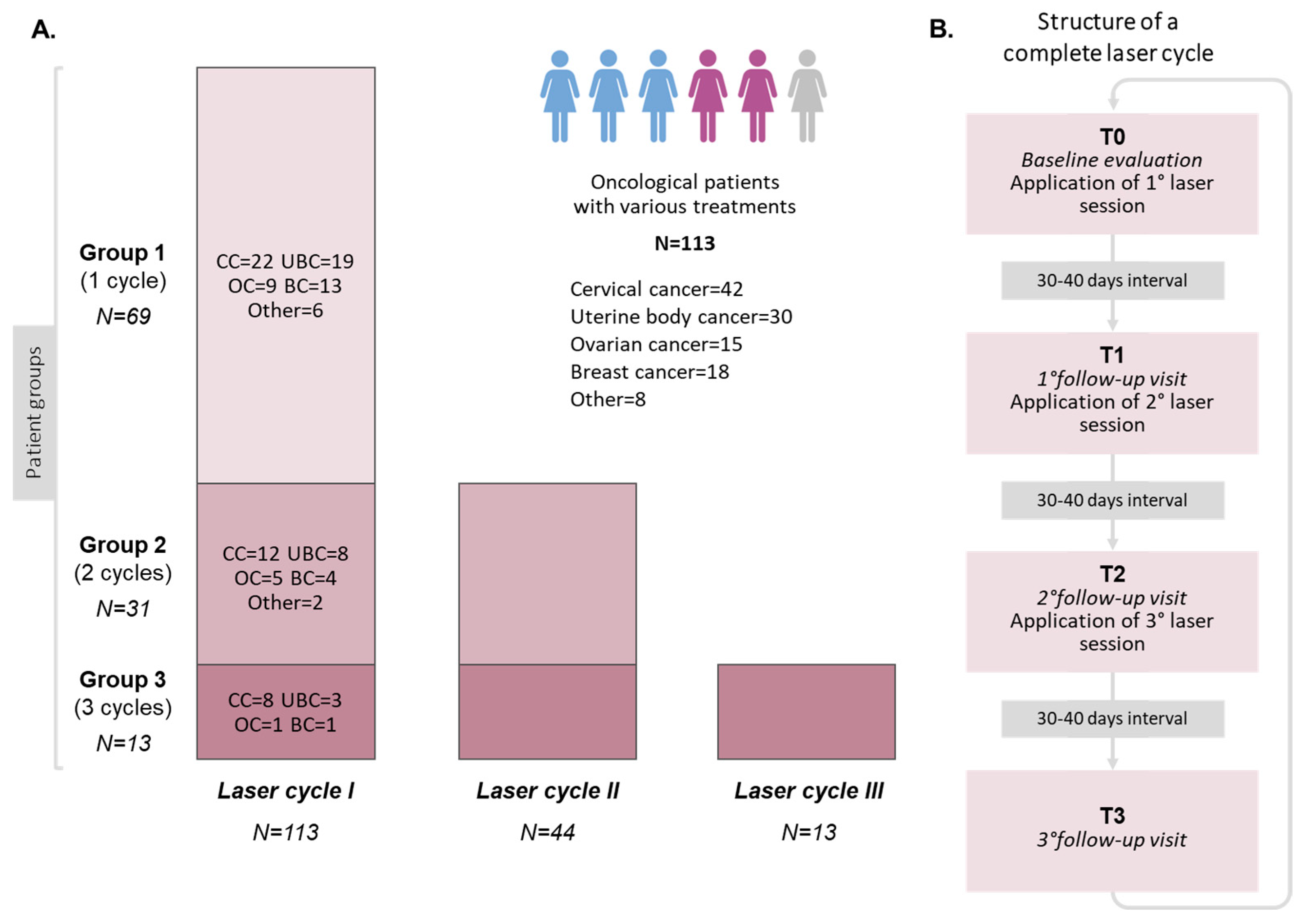
2.1. Study Design
2.2. Laser Procedure
2.3. Assessment of Vaginal Physical Parameters and Sexual Function Questionnaire
2.4. Population
2.5. Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Laser Treatment
3.3. Laser Procedure Tolerability
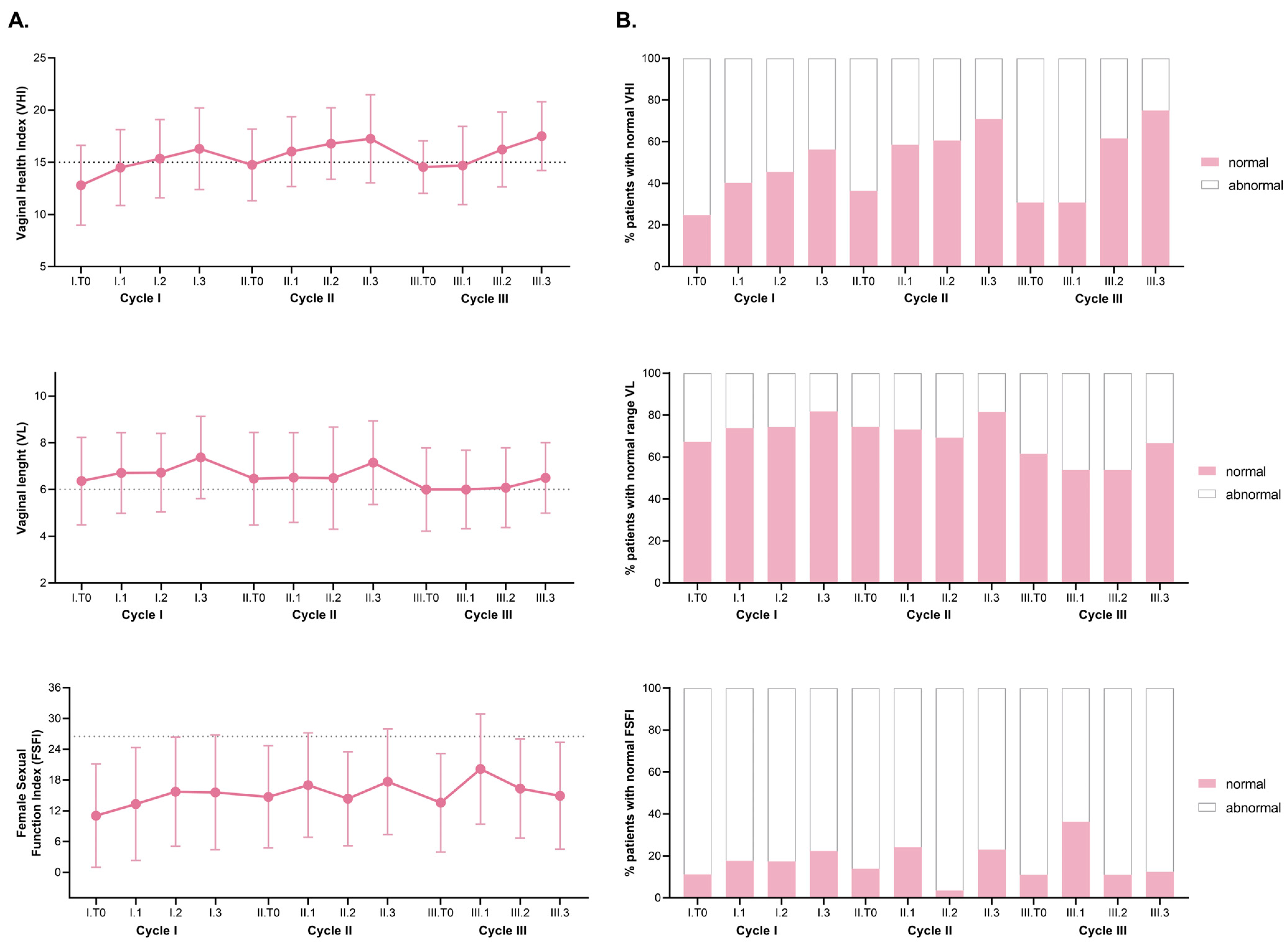
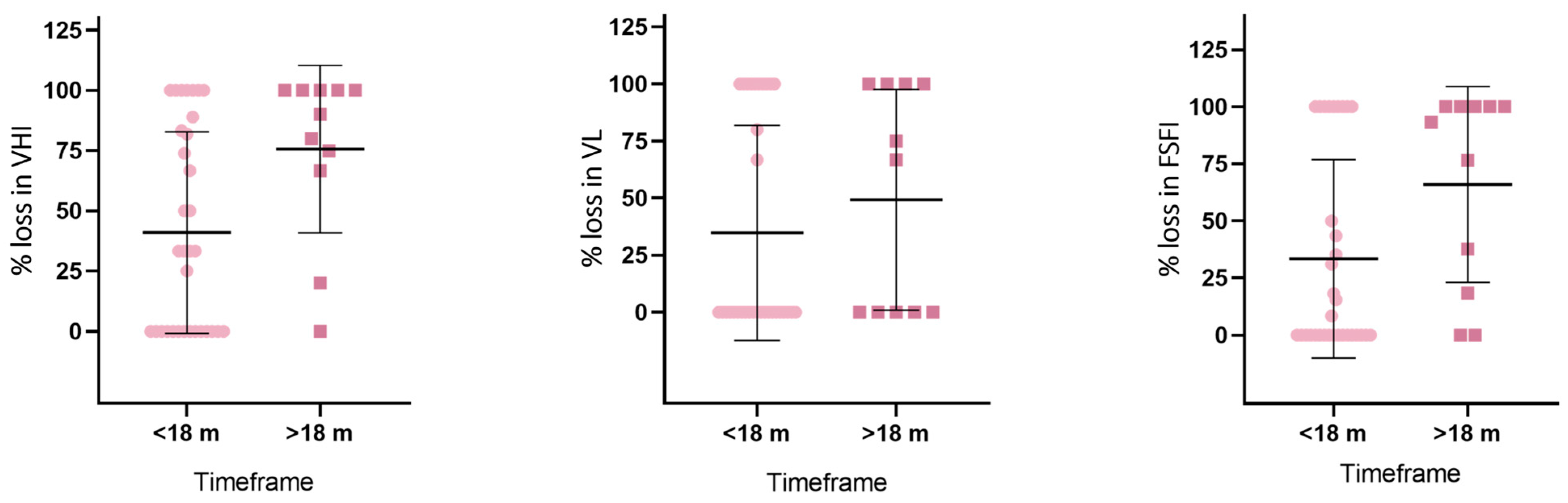
3.4. Vaginal Health Parameters and FSFI Score
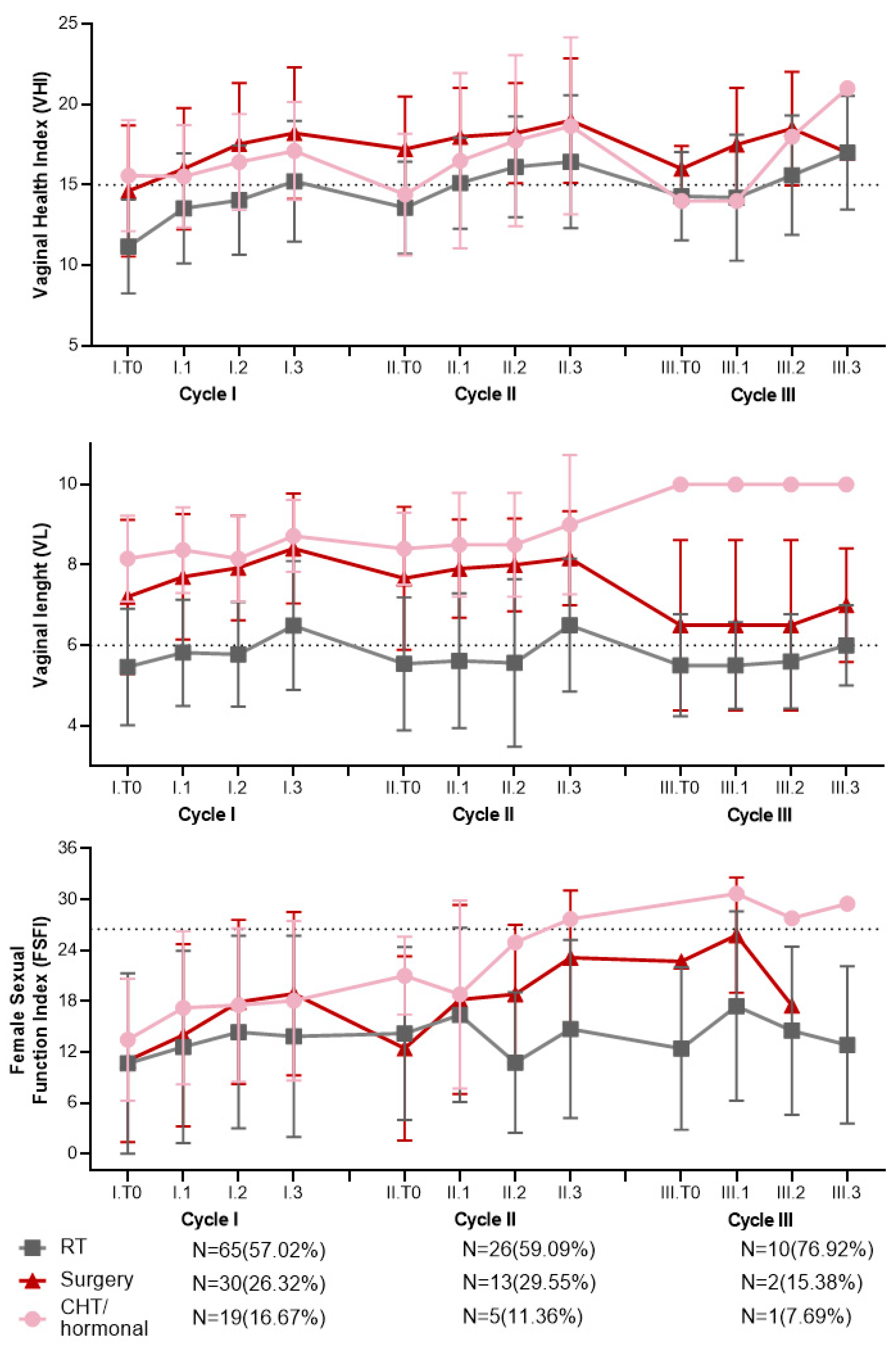
3.5. Evolution of Vaginal and Sexual Parameters Based on the Different Oncological Treatments
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fanfani, F.; Vizza, E.; Landoni, F.; de Iaco, P.; Ferrandina, G.; Corrado, G.; Gallotta, V.; Gambacorta, M.A.; Fagotti, A.; Monterossi, G.; et al. Radical Hysterectomy after Chemoradiation in FIGO Stage III Cervical Cancer Patients versus Chemoradiation and Brachytherapy: Complications and 3-Years Survival. Eur. J. Surg. Oncol. 2016, 42, 1519–1525. [Google Scholar] [CrossRef]
- Galuppi, A.; Perrone, A.M.; Macchia, M.L.; Santini, D.; Medoro, S.; Maccarini, L.R.; Strada, I.; Pozzati, F.; Rossi, M.; Iaco, P.D. Local α-Tocopherol for Acute and Short-Term Vaginal Toxicity Prevention in Patients Treated with Radiotherapy for Gynecologic Tumors. Int. J. Gynecol. Cancer 2011, 21, 1708–1711. [Google Scholar] [CrossRef]
- White, I.D.; Sangha, A.; Lucas, G.; Wiseman, T. Assessment of Sexual Difficulties Associated with Multi-Modal Treatment for Cervical or Endometrial Cancer: A Systematic Review of Measurement Instruments. Gynecol. Oncol. 2016, 143, 664–673. [Google Scholar] [CrossRef]
- Bober, S.L.; Kingsberg, S.A.; Faubion, S.S. Sexual Function after Cancer: Paying the Price of Survivorship. Climacteric 2019, 22, 558–564. [Google Scholar] [CrossRef]
- North American Menopause Society. Management of Symptomatic Vulvovaginal Atrophy: 2013 Position Statement of The North American Menopause Society. Menopause 2013, 20, 888–902; quiz 903–904. [Google Scholar] [CrossRef]
- Hofsjö, A.; Bohm-Starke, N.; Bergmark, K.; Masironi, B.; Sahlin, L. Sex Steroid Hormone Receptor Expression in the Vaginal Wall in Cervical Cancer Survivors after Radiotherapy. Acta Oncol. 2019, 58, 1107–1115. [Google Scholar] [CrossRef]
- Kovacevic, N.; Cilensek, I.; Merlo, S.; Segedin, B. Modern Approach to the Management of Genitourinary Syndrome in Women with Gynecological Malignancies. Radiol. Oncol. 2023, 57, 292–298. [Google Scholar] [CrossRef]
- Gunter, J. Genitourinary Syndrome of Menopause and the False Promise of Vaginal Laser Therapy. JAMA Netw. Open 2023, 6, e2255706. [Google Scholar] [CrossRef]
- Kesic, V.; Carcopino, X.; Preti, M.; Vieira-Baptista, P.; Bevilacqua, F.; Bornstein, J.; Chargari, C.; Cruickshank, M.; Erzeneoglu, E.; Gallio, N.; et al. The European Society of Gynaecological Oncology (ESGO), the International Society for the Study of Vulvovaginal Disease (ISSVD), the European College for the Study of Vulval Disease (ECSVD), and the European Federation for Colposcopy (EFC) Consensus Statement on the Management of Vaginal Intraepithelial Neoplasia. J. Low. Genit. Tract Dis. 2023, 27, 131. [Google Scholar] [CrossRef]
- Zipper, R.; Lamvu, G. Vaginal Laser Therapy for Gynecologic Conditions: Re-Examining the Controversy and Where Do We Go from Here. J. Comp. Eff. Res. 2022, 11, 843–851. [Google Scholar] [CrossRef]
- Perino, A.; Calligaro, A.; Forlani, F.; Tiberio, C.; Cucinella, G.; Svelato, A.; Saitta, S.; Calagna, G. Vulvo-Vaginal Atrophy: A New Treatment Modality Using Thermo-Ablative Fractional CO2 Laser. Maturitas 2015, 80, 296–301. [Google Scholar] [CrossRef]
- Cruz, V.L.; Steiner, M.L.; Pompei, L.M.; Strufaldi, R.; Fonseca, F.L.A.; Santiago, L.H.S.; Wajsfeld, T.; Fernandes, C.E. Randomized, Double-Blind, Placebo-Controlled Clinical Trial for Evaluating the Efficacy of Fractional CO2 Laser Compared with Topical Estriol in the Treatment of Vaginal Atrophy in Postmenopausal Women. Menopause 2018, 25, 21–28. [Google Scholar] [CrossRef]
- Preti, M.; Vieira-Baptista, P.; Digesu, G.A.; Bretschneider, C.E.; Damaser, M.; Demirkesen, O.; Heller, D.S.; Mangir, N.; Marchitelli, C.; Mourad, S.; et al. The Clinical Role of LASER for Vulvar and Vaginal Treatments in Gynecology and Female Urology: An ICS/ISSVD Best Practice Consensus Document. Neurourol. Urodyn. 2019, 38, 1009–1023. [Google Scholar] [CrossRef]
- Alvisi, S.; Lami, A.; Baldassarre, M.; Lenzi, J.; Mancini, I.; Seracchioli, R.; Meriggiola, M.C. Short-Term Efficacy and Safety of Non-Ablative Laser Treatment Alone or with Estriol or Moisturizers in Postmenopausal Women with Vulvovaginal Atrophy. J. Sex Med. 2022, 19, 761–770. [Google Scholar] [CrossRef]
- Col, N.F.; Kim, J.A.; Chlebowski, R.T. Menopausal Hormone Therapy after Breast Cancer: A Meta-Analysis and Critical Appraisal of the Evidence. Breast Cancer Res. 2005, 7, R535–R540. [Google Scholar] [CrossRef]
- Angioli, R.; Stefano, S.; Filippini, M.; Pieralli, A.; Montera, R.; Plotti, F.; Gatti, A.; Bartolone, M.; Luvero, D. Effectiveness of CO2 Laser on Urogenital Syndrome in Women with a Previous Gynecological Neoplasia: A Multicentric Study. Int. J. Gynecol. Cancer 2020, 30, 590–595. [Google Scholar] [CrossRef]
- Santen, R.J.; Stuenkel, C.A.; Davis, S.R.; Pinkerton, J.V.; Gompel, A.; Lumsden, M.A. Managing Menopausal Symptoms and Associated Clinical Issues in Breast Cancer Survivors. J. Clin. Endocrinol. Metab. 2017, 102, 3647–3661. [Google Scholar] [CrossRef]
- Athanasiou, S.; Pitsouni, E.; Douskos, A.; Salvatore, S.; Loutradis, D.; Grigoriadis, T. Intravaginal Energy-Based Devices and Sexual Health of Female Cancer Survivors: A Systematic Review and Meta-Analysis. Lasers Med. Sci. 2020, 35, 1–11. [Google Scholar] [CrossRef]
- D’Oria, O.; Giannini, A.; Buzzaccarini, G.; Tinelli, A.; Corrado, G.; Frega, A.; Vizza, E.; Caserta, D. Fractional CO2 Laser for Vulvo-Vaginal Atrophy in Gynecologic Cancer Patients: A Valid Therapeutic Choice? A Systematic Review. Eur. J. Obs. Gynecol. Reprod. Biol. 2022, 277, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Pieralli, A.; Fallani, M.G.; Becorpi, A.; Bianchi, C.; Corioni, S.; Longinotti, M.; Tredici, Z.; Guaschino, S. Fractional CO2 Laser for Vulvovaginal Atrophy (VVA) Dyspareunia Relief in Breast Cancer Survivors. Arch. Gynecol. Obs. 2016, 294, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Quick, A.M.; Zvinovski, F.; Hudson, C.; Hundley, A.; Evans, C.; Suresh, A.; Stephens, J.A.; Arthur, E.; Ramaswamy, B.; Reinbolt, R.E.; et al. Fractional CO2 Laser Therapy for Genitourinary Syndrome of Menopause for Breast Cancer Survivors. Support Care Cancer 2020, 28, 3669–3677. [Google Scholar] [CrossRef]
- Gambacciani, M.; Levancini, M. Vaginal Erbium Laser as Second-Generation Thermotherapy for the Genitourinary Syndrome of Menopause: A Pilot Study in Breast Cancer Survivors. Menopause 2017, 24, 316–319. [Google Scholar] [CrossRef] [PubMed]
- Perrone, A.M.; Tesei, M.; Ferioli, M.; De Terlizzi, F.; Della Gatta, A.N.; Boussedra, S.; Dondi, G.; Galuppi, A.; Morganti, A.G.; De Iaco, P. Results of a Phase I-II Study on Laser Therapy for Vaginal Side Effects after Radiotherapy for Cancer of Uterine Cervix or Endometrium. Cancers 2020, 12, 1639. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.S.; Lukacz, E.S.; Menefee, S.A.; Luber, K.M.; Albo, M.E.; Nager, C.W. Determinants of Vaginal Length. Am. J. Obs. Gynecol. 2006, 195, 1846–1850. [Google Scholar] [CrossRef]
- Bachmann, G. Urogenital Ageing: An Old Problem Newly Recognized. Maturitas 1995, 22, S1–S5. [Google Scholar] [CrossRef]
- Heller, G.Z.; Manuguerra, M.; Chow, R. How to Analyze the Visual Analogue Scale: Myths, Truths and Clinical Relevance. Scand. J. Pain 2016, 13, 67–75. [Google Scholar] [CrossRef]
- Rosen, R.; Brown, C.; Heiman, J.; Leiblum, S.; Meston, C.; Shabsigh, R.; Ferguson, D.; D’Agostino, R. The Female Sexual Function Index (FSFI): A Multidimensional Self-Report Instrument for the Assessment of Female Sexual Function. J. Sex Marital. Ther. 2000, 26, 191–208. [Google Scholar] [CrossRef]
- R Core Team. European Environment Agency. 2020. Available online: https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006 (accessed on 31 August 2022).
- Bakdash, J.Z.; Marusich, L.R. Repeated Measures Correlation. Front. Psychol. 2017, 8, 456. [Google Scholar] [CrossRef]
- Bulus, M. pwrss: Statistical Power and Sample Size Calculation Tools. R Package Version 0.3.1. 2023. Available online: https://CRAN.R-project.org/package=pwrss (accessed on 31 August 2022).
- Wiegel, M.; Meston, C.; Rosen, R. The Female Sexual Function Index (FSFI): Cross-Validation and Development of Clinical Cutoff Scores. J. Sex. Marital. Ther. 2005, 31, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Marci, R.; Mallozzi, M.; Di Benedetto, L.; Schimberni, M.; Mossa, S.; Soave, I.; Palomba, S.; Caserta, D. Radiations and Female Fertility. Reprod Biol. Endocrinol. 2018, 16, 112. [Google Scholar] [CrossRef] [PubMed]
- Macchia, G.; Cilla, S.; Deodato, F.; Ianiro, A.; Legge, F.; Marucci, M.; Cammelli, S.; Perrone, A.M.; De Iaco, P.; Gambacorta, M.A.; et al. Simultaneous Integrated Boost Volumetric Modulated Arc Therapy in the Postoperative Treatment of High-Risk to Intermediate-Risk Endometrial Cancer: Results of ADA II Phase 1-2 Trial. Int. J. Radiat. Oncol. Biol. Phys. 2016, 96, 606–613. [Google Scholar] [CrossRef]
- Dabaghi, S.; Zandi, M.; Ilkhani, M. Sexual Satisfaction in Patients with Mayer-Rokitansky-Küster-Hauser Syndrome after Surgical and Non-Surgical Techniques: A Systematic Review. Int. Urogynecol. J. 2019, 30, 353–362. [Google Scholar] [CrossRef]
- Brand, A.H.; Bull, C.A.; Cakir, B. Vaginal Stenosis in Patients Treated with Radiotherapy for Carcinoma of the Cervix. Int. J. Gynecol. Cancer 2006, 16, 288–293. [Google Scholar] [CrossRef]
- Faubion, S.S.; Rullo, J.E. Sexual Dysfunction in Women: A Practical Approach. Am. Fam. Physician 2015, 92, 281–288. [Google Scholar]
- Goldstein, I. Current Management Strategies of the Postmenopausal Patient with Sexual Health Problems. J. Sex Med. 2007, 4 (Suppl. S3), 235–253. [Google Scholar] [CrossRef]
- Hsieh, C.-C.; Chen, C.-A.; Hsiao, F.-H.; Shun, S.-C. The Correlations of Sexual Activity, Sleep Problems, Emotional Distress, Attachment Styles with Quality of Life: Comparison between Gynaecological Cancer Survivors and Noncancer Women. J. Clin. Nurs. 2014, 23, 985–994. [Google Scholar] [CrossRef]
- Liu, M.; Juravic, M.; Mazza, G.; Krychman, M.L. Vaginal Dilators: Issues and Answers. Sex Med. Rev. 2021, 9, 212–220. [Google Scholar] [CrossRef]
- Miles, T.; Johnson, N. Vaginal Dilator Therapy for Women Receiving Pelvic Radiotherapy. Cochrane Database Syst. Rev. 2014, 2014, CD007291. [Google Scholar] [CrossRef]
- Martins, J.; Vaz, A.F.; Grion, R.C.; Costa-Paiva, L.; Baccaro, L.F. Topical Estrogen, Testosterone, and Vaginal Dilator in the Prevention of Vaginal Stenosis after Radiotherapy in Women with Cervical Cancer: A Randomized Clinical Trial. BMC Cancer 2021, 21, 682. [Google Scholar] [CrossRef]
- Taha, O.T.; Al-Okda, N.; Hamdy, M.A. Vaginal length and sexual function after vertical versus horizontal closure of the vaginal cuff after abdominal hysterectomy: A randomised clinical trial. J. Obstet. Gynaecol. 2021, 42, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
| Patients Group. N(%)/Mean ± SD | ||||||
|---|---|---|---|---|---|---|
| Variable | Total N = 113 | 1 Cycle N = 69(61.1%) | 2 Cycles N = 31(27.4%) | 3 Cycles N = 13(11.5%) | p-Value | |
| Age at oncological diagnosis | 46.6 ± 8.5 | 48 ± 9 | 45.47 ± 6.85 | 44.57 ± 8.11 | 0.5 | |
| Age at first laser | 50.5 ± 8.3 | 51.54 ± 8.97 | 50.06 ± 6.67 | 45.69 ± 6.99 | 0.06 | |
| Age group | ≤45 | 35(31) | 18(26.1) | 9(29) | 8(61.5) | 0.04 |
| >45 | 78(69) | 51(73.9) | 22(71) | 5(38.5) | ||
| Age at menopause | 45.2 ± 6.3 | 45.48 ± 6.62 | 45.62 ± 5.39 | 43.43 ± 5.79 | 0.38 | |
| Early menopause < 45 years | No | 58(52.3) | 40(59) | 15(54.8) | 3(23.1) | 0.07 |
| Yes | 53(47.7) | 29(41) | 14(45.2) | 10(76.9) | ||
| N/A | 2 | |||||
| Premature menopause < 40 years | No | 94(84.7) | 59(85.5) | 27(93.5) | 8(61.5) | 0.03 |
| Yes | 17(15.3) | 10(14.5) | 2(6.5) | 5(38.5) | ||
| N/A | 2 | |||||
| BMI (kg/m2) | 23.49 ± 4.4 | 23.71 ± 4.9 | 23.63 ± 3.42 | 21.97 ± 4.43 | 0.42 | |
| BMI category | Normal | 100(89.3) | 58(84.1) | 30(96.7) | 12(92.3) | 0.22 |
| Overweight | 12(10.7) | 10(15.9) | 1(3.3) | 1(7.7) | ||
| Parity | Nulliparous | 43(39.1) | 24(36.4) | 14(45.2) | 5(38.5) | 0.42 |
| Parous | 55(50) | 32(48.5) | 15(48.4) | 8(61.5) | ||
| Cesarean section | 12(10.9) | 10(15.1) | 2(6.5) | - | ||
| N/A | 3 | |||||
| Tumor type at diagnosis | Cervix | 42(37.2) | 22(31.9) | 12(38.7) | 8(61.5) | 0.84 |
| Uterus | 30(26.5) | 19(27.6) | 8(25.8) | 3(23.1) | ||
| Rectal | 5(4.4) | 4(5.8) | 1(3.2) | - | ||
| Ovarian | 15(13.3) | 9(13) | 5(16.1) | 1(7.7) | ||
| Breast | 18(15.9) | 13(18.8) | 4(13) | 1(7.7) | ||
| Other | 3(2.7) | 2(2.9) | 1(3.2) | - | ||
| Stage | I + II | 86(76.1) | 52(75.4) | 27(87.1) | 12(92.3) | 0.11 |
| III + IV | 25(23.9) | 20(24.6) | 3(12.9) | 2(7.7) | ||
| N/A | 2 | |||||
| Radiotherapy and/or Brachytherapy | 65(57.6) | 39(56.5) | 16(51.6) | 10(76.9) | 0.36 | |
| Hysterectomy and Bilateral adnexectomy | 30(26.6) | 16(23.2) | 11(35.5) | 2(15.4) | ||
| Chemotherapy and anti-hormonal therapy | 19(16.8) | 14(20.3) | 4(12.9) | 1(7.7) | ||
| Cycle Number | Laser Application | Number of Patients with VHI > 15 N/Total(%) | Number of Patients with VL ≥ 6 cm N/Total(%) | Number of Patients with FSFI > 26.55 N/Total(%) |
|---|---|---|---|---|
| I | T0 Before Treatment Initiation | 28/113(24.78) | 76/113(67.26) | 10/89(11.24) |
| T1 | 45/112(40.18) | 82/111(73.87) | 15/85(17.65) | |
| T2 | 50/110(45.46) | 81/109(74.31) | 15/86(17.44) | |
| T3 | 54/96(56.25) | 85/104(81.73) | 17/76(22.37) | |
| II | T0 Before Cycle II | 16/44(36.37) | 32/43(74.42) | 5/36(13.89) |
| T1 | 24/41(58.54) | 30/41(73.17) | 7/29(24.14) | |
| T2 | 23/38(60.53) | 27/39(69.23) | 1/28(3.57) | |
| T3 | 17/24(70.83) | 22/27(81.48) | 3/13(23.08) | |
| III | T0 Before Cycle III | 4/13(30.77) | 8/13(61.54) | 1/9(11.11) |
| T1 | 4/13(30.77) | 7/13(53.85) | 4/11(36.36) | |
| T2 | 8/13(61.54) | 7/13(53.85) | 1/9(11.11) | |
| T3 | 6/8(75) | 8/12(66.67) | 1/8(12.5) |
| Radiotherapy-Based Treatments (Radiotherapy, Brachytherapy) | |||||||
|---|---|---|---|---|---|---|---|
| VHI (Points) | LV (cm) | FSFI (Points) | |||||
| Cycle Number | Laser Session | Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value |
| I N = 65 | T0 | 11.2 ± 2.92 | <0.001 | 5.46 ± 1.45 | <0.001 | 10.7 ± 10.6 | 0.05 |
| T1 | 13.5 ± 3.43 | 5.82 ± 1.32 | 12.6 ± 11.3 | ||||
| T2 | 14 ± 3.4 | 5.78 ± 1.3 | 14.4 ± 11.4 | ||||
| T3 | 15.2 ± 3.75 | 6.49 ± 1.6 | 13.9 ± 11.9 | ||||
| II N = 26 | T0 | 13.6 ± 2.86 | 0.02 | 5.54 ± 1.66 | <0.001 | 14.2 ± 10.2 | 0.62 |
| T1 | 15.1 ± 2.83 | 5.62 ± 1.68 | 16.8 ± 10.6 | ||||
| T2 | 16.1 ± 3.14 | 5.56 ± 2.08 | 10.8 ± 8.3 | ||||
| T3 | 16.4 ± 4.13 | 6.5 ± 1.65 | 14.7 ± 10.5 | ||||
| III N = 10 | T0 | 14.3 ± 2.75 | <0.001 | 5.5 ± 1.27 | 0.01 | 12.4 ± 9.59 | 0.88 |
| T1 | 14.2 ± 3.91 | 5.5 ± 1.08 | 17.4 ± 11.2 | ||||
| T2 | 15.6 ± 3.72 | 5.6 ± 1.17 | 14 ± 10.8 | ||||
| T3 | 17 ± 3.52 | 6 ± 1 | 12.8 ± 9.27 | ||||
| Surgery | |||||||
| VHI (Points) | LV (cm) | FSFI (Points) | |||||
| Cycle Number | Laser Session | Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value |
| I N = 29 | T0 | 16 ± 3.78 | <0.001 | 7.21 ± 1.92 | <0.001 | 11 ± 9.63 | 0.01 |
| T1 | 14.6 ± 4.07 | 7.7 ± 1.56 | 14 ± 10.8 | ||||
| T2 | 17.5 ± 3.8 | 7.93 ± 1.3 | 17.9 ± 9.67 | ||||
| T3 | 18.2 ± 4.09 | 8.41 ± 1.37 | 18.9 ± 9.64 | ||||
| II N = 13 | T0 | 17.2 ± 3.27 | 0.84 | 7.67 ± 1.78 | 0.89 | 12.4 ± 10.9 | 0.12 |
| T1 | 18 ± 3.03 | 7.91 ± 1.22 | 18.2 ± 11.1 | ||||
| T2 | 18.2 ± 3.11 | 8 ± 1.16 | 18.8 ± 8.21 | ||||
| T3 | 19 ± 3.87 | 8.17 ± 1.17 | 23.1 ± 7.93 | ||||
| III N = 2 | T0 | 16 ± 1.41 | n/a | 6.5 ± 2.12 | n/a | 19.8 ± 4.03 | n/a |
| T1 | 17.5 ± 3.54 | 6.5 ± 2.12 | 25.8 ± 6.79 | ||||
| T2 | 18.5 ± 3.54 | 6.5 ± 2.12 | 22.8 ± 7.42 | ||||
| T3 | 20 ± 4.24 | 7 ± 1.41 | 24.5 ± 10.6 | ||||
| Chemotherapy and/or Hormonal Therapy | |||||||
| VHI (Points) | LV (cm) | FSFI (Points) | |||||
| Cycle Number | Laser Session | Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value |
| I N = 19 | T0 | 15.6 ± 3.45 | 0.08 | 8.16 ± 1.07 | 0.16 | 13.5 ± 7.17 | 0.47 |
| T1 | 15.5 ± 3.19 | 8.37 ± 1.06 | 17.2 ± 9.01 | ||||
| T2 | 16.4 ± 2.99 | 8.16 ± 1.07 | 17.6 ± 9.05 | ||||
| T3 | 17.1 ± 3.05 | 8.72 ± 0.89 | 18.1 ± 9.41 | ||||
| II N = 5 | T0 | 14.4 ± 3.78 | 0.05 | 8.4 ± 0.894 | 0.28 | 21 ± 4.59 | 0.67 |
| T1 | 16.5 ± 5.45 | 8.5 ± 1.29 | 18.4 ± 9.09 | ||||
| T2 | 17.8 ± 5.32 | 8.5 ± 1.29 | 19.6 ± 11.3 | ||||
| T3 | 18.7 ± 5.51 | 9 ± 1.73 | 24.1 ± 6.21 | ||||
| III N = 1 | T0 | 14 | n/a | 10 | n/a | 27 | n/a |
| T1 | 14 | 10 | 30.7 | ||||
| T2 | 18 | 10 | 27.8 | ||||
| T3 | 21 | 10 | 29.5 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Stanislao, M.; Coada, C.A.; De Terlizzi, F.; Di Costanzo, S.; Fiuzzi, E.; Mezzapesa, F.; Dondi, G.; Paoli, D.; Damiani, G.R.; Raspagliesi, F.; et al. Laser Therapy in Heavily Treated Oncological Patients Improves Vaginal Health Parameters. Cancers 2024, 16, 2722. https://doi.org/10.3390/cancers16152722
Di Stanislao M, Coada CA, De Terlizzi F, Di Costanzo S, Fiuzzi E, Mezzapesa F, Dondi G, Paoli D, Damiani GR, Raspagliesi F, et al. Laser Therapy in Heavily Treated Oncological Patients Improves Vaginal Health Parameters. Cancers. 2024; 16(15):2722. https://doi.org/10.3390/cancers16152722
Chicago/Turabian StyleDi Stanislao, Marco, Camelia Alexandra Coada, Francesca De Terlizzi, Stella Di Costanzo, Enrico Fiuzzi, Francesco Mezzapesa, Giulia Dondi, Damiano Paoli, Gianluca Raffaello Damiani, Francesco Raspagliesi, and et al. 2024. "Laser Therapy in Heavily Treated Oncological Patients Improves Vaginal Health Parameters" Cancers 16, no. 15: 2722. https://doi.org/10.3390/cancers16152722
APA StyleDi Stanislao, M., Coada, C. A., De Terlizzi, F., Di Costanzo, S., Fiuzzi, E., Mezzapesa, F., Dondi, G., Paoli, D., Damiani, G. R., Raspagliesi, F., Bogani, G., Ditto, A., Morganti, A. G., De Iaco, P., & Perrone, A. M. (2024). Laser Therapy in Heavily Treated Oncological Patients Improves Vaginal Health Parameters. Cancers, 16(15), 2722. https://doi.org/10.3390/cancers16152722











