Systemic Treatment in Intermediate Stage (Barcelona Clinic Liver Cancer-B) Hepatocellular Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Tyrosine Kinase Inhibitors (TKIs)
2.1. Sorafenib
2.2. Regorafenib
2.3. Lenvatinib
2.4. Cabozantinib
2.5. Immune Checkpoint Inhibitors (ICIs)
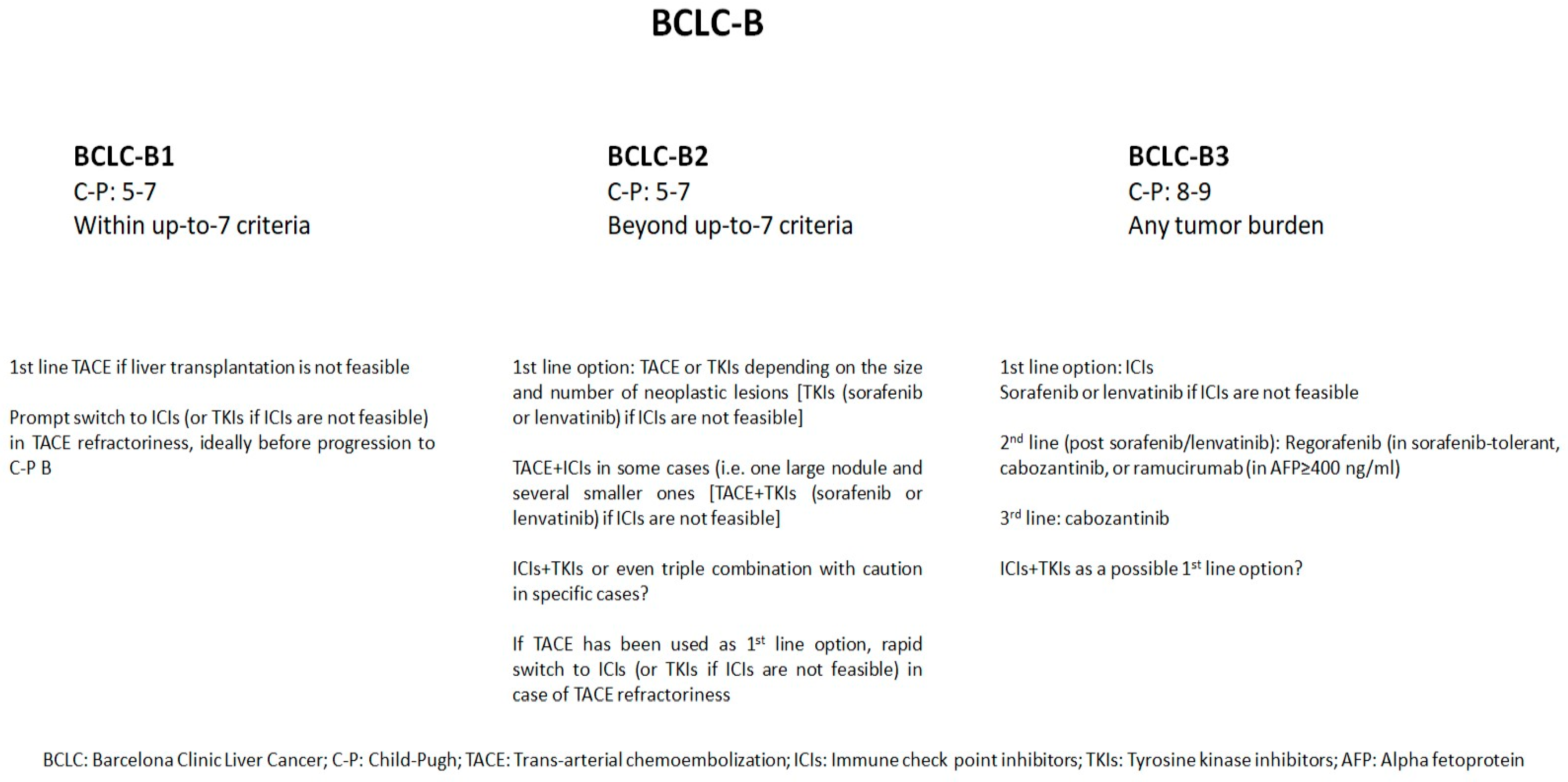
3. Discussion
4. Conclusions
Funding
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020, GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Asafo-Agyei, K.O.; Samant, H. Hepatocellular Carcinoma; StatPearls Publishing: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Simonetti, R.G.; Cammà, C.; Fiorello, F.; Politi, F.; D’Amico, G.; Pagliaro, L. Hepatocellular carcinoma. A worldwide problem and the major risk factors. Dig. Dis. Sci. 1991, 36, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Luo, P.; Wu, S.; Yu, Y.; Ming, X.; Li, S.; Zuo, X.; Tu, J. Current Status and Perspective Biomarkers in AFP Negative HCC: Towards Screening for and Diagnosing Hepatocellular Carcinoma at an Earlier Stage. Pathol. Oncol. Res. 2020, 26, 599–603. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Kulik, L.M.; Finn, R.S.; Sirlin, C.B.; Abecassis, M.M.; Roberts, L.R.; Zhu, A.X.; Murad, M.H.; Marrero, J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018, 67, 358–380. [Google Scholar] [CrossRef]
- Omata, M.; Cheng, A.L.; Kokudo, N.; Kudo, M.; Lee, J.M.; Jia, J.; Tateishi, R.; Han, K.-Y.; Chawla, Y.K.; Shiina, S.; et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: A 2017 update. Hepatol. Int. 2017, 11, 317–370. [Google Scholar] [CrossRef]
- Llovet, J.M.; Brú, C.; Bruix, J. Prognosis of hepatocellular carcinoma: The BCLC staging classification. Semin. Liver Dis. 1999, 19, 329–338. [Google Scholar] [CrossRef]
- Hasegawa, K.; Kokudo, N.; Makuuchi, M.; Izumi, N.; Ichida, T.; Kudo, M.; Ku, Y.; Sakamoto, M.; Nakashima, O.; Matsui, O.; et al. Comparison of resection and ablation for hepatocellular carcinoma: A cohort study based on a Japanese nationwide survey. J. Hepatol. 2013, 58, 724–729, Correction in J. Hepatol. 2013, 59, 641. [Google Scholar] [CrossRef]
- Dong, S.C.; Bai, D.S.; Wang, F.A.; Jin, S.-J.; Zhang, C.; Zhou, B.-H.; Jiang, G.-Q. Radiofrequency ablation is an inferior option to liver resection for solitary hepatocellular carcinoma ≤ 5 cm without cirrhosis: A population-based study with stratification by tumor size. Hepatobiliary Pancreat. Dis. Int. 2023, 22, 605–614. [Google Scholar] [CrossRef]
- Yang, W.; Yan, K.; Goldberg, S.N.; Lee, J.-C.; Wu, W.; Zhang, Z.-Y.; Wang, S.; Chen, M.-H. Ten-year survival of hepatocellular carcinoma patients undergoing radiofrequency ablation as a first-line treatment. World J. Gastroenterol. 2016, 22, 2993–3005. [Google Scholar] [CrossRef]
- Chen, H.Y.; Lu, S.N.; Hung, C.H.; Wang, J.-H.; Chen, C.-H.; Yen, Y.-H.; Kuo, Y.-H.; Kee, K.-M. Predicting outcomes for recurrent hepatocellular carcinoma within Milan criteria after complete radiofrequency ablation. PLoS ONE 2020, 15, e0242113. [Google Scholar] [CrossRef] [PubMed]
- Sherman, M. Recurrence of hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 2045–2047. [Google Scholar] [CrossRef] [PubMed]
- Solimando, A.G.; Susca, N.; Argentiero, A.; Brunetti, O.; Leone, P.; De Re, V.; Fasano, R.; Krebs, M.; Petracci, E.; Azzali, I.; et al. Second-line treatments for Advanced Hepatocellular Carcinoma: A Systematic Review and Bayesian Network Meta-analysis. Clin. Exp. Med. 2022, 22, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Lang, L. FDA approves sorafenib for patients with inoperable liver cancer. Gastroenterology 2008, 134, 379. [Google Scholar] [CrossRef] [PubMed]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V.; et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 389, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.W.; Han, G.; Jassem, J.; et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomized phase 3 non-inferiority trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Meyer, T.; Cheng, A.L.; El-Khoueiry, A.B.; Rimassa, L.; Ryoo, B.Y.; Cicin, I.; Merle, P.; Chen, Y.; Park, J.W.; et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N. Engl. J. Med. 2018, 379, 54–63. [Google Scholar] [CrossRef]
- Yau, T.; Park, J.W.; Finn, R.S.; Cheng, A.-L.; Mathurin, P.; Edeline, J.; Kudo, M.; Harding, J.J.; Merle, P.; Rosmorduc, O.; et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): A randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2022, 23, 77–90. [Google Scholar] [CrossRef]
- Finn, R.S.; Ryoo, B.Y.; Merle, P.; Kudo, M.; Bouattour, M.; Lim, H.-Y.; Breder, V.; Edeline, J.; Chao, Y.; Ogasawara, S.; et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240, a randomized, double-blind, phase III trial. J. Clin. Oncol. 2020, 38, 193–202. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef]
- Cheng, A.L.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Lim, H.-Y.; Kudo, M.; Breder, V.; Merle, P.; et al. Updated efficacy and safety data from IMbrave150, atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J. Hepatol. 2022, 76, 862–873. [Google Scholar] [CrossRef] [PubMed]
- Abou-Alfa, G.K.; Lau, G.; Kudo, M.; Chan, S.L.; Kelley, R.K.; Furuse, J.; Sukeepaisarnjaroen, W.; Kang, Y.-K.; Dao, T.V.; De Toni, E.N.; et al. Tremelimumab plus durvalumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. Evid. 2022, 1, EVIDoa2100070. [Google Scholar] [CrossRef]
- Singal, A.G.; Kudo, M.; Bruix, J. Breakthroughs in Hepatocellular Carcinoma Therapies. Clin. Gastroenterol. Hepatol. 2023, 21, 2135–2149. [Google Scholar] [CrossRef] [PubMed]
- Peck-Radosavljevic, M.; Kudo, M.; Raoul, J.-L.; Lee, H.C.; Decaens, T.; Heo, J.; Lin, S.-M.; Shan, H.; Yang, Y.; Bayh, I.; et al. Outcomes of patients (PATIENTS) with hepatocellular carcinoma (HCC) treated with transarterial chemoembolization (TACE): Global OPTIMIS final analysis. J. Clin. Oncol. 2018, 36, 4018. [Google Scholar] [CrossRef]
- Kudo, M. Regorafenib as Second-Line Systemic Therapy May Change the Treatment Strategy and Management Paradigm for Hepatocellular Carcinoma. Liver Cancer 2016, 5, 235–244. [Google Scholar] [PubMed]
- Arizumi, T.; Ueshima, K.; Iwanishi, M.; Minami, T.; Chishina, H.; Kono, M.; Takita, M.; Kitai, S.; Inoue, T.; Yada, N.; et al. Validation of a modified substaging system (Kinki criteria) for patients with intermediate-stage hepatocellular carcinoma. Oncology 2015, 89 (Suppl. S2), 47–52. [Google Scholar] [CrossRef] [PubMed]
- Pottier, C.; Fresnais, M.; Gilon, M.; Jérusalem, G.; Longuespée, R.; Sounni, N.E. Tyrosine Kinase Inhibitors in Cancer: Breakthrough and Challenges of Targeted Therapy. Cancers 2020, 12, 731. [Google Scholar] [CrossRef]
- Huang, L.; Jiang, S.; Shi, Y. Tyrosine kinase inhibitors for solid tumors in the past 20 years (2001–2020). J. Hematol. Oncol. 2020, 13, 143. [Google Scholar] [CrossRef]
- Sudhesh Dev, S.; Zainal Abidin, S.A.; Farghadani, R.; Othman, I.; Naidu, R. Receptor Tyrosine Kinases and Their Signaling Pathways as Therapeutic Targets of Curcumin in Cancer. Front. Pharmacol. 2021, 12, 772510. [Google Scholar] [CrossRef]
- Mirshafiey, A.; Ghalamfarsa, G.; Asghari, B.; Azizi, G. Receptor Tyrosine Kinase and Tyrosine Kinase Inhibitors: New Hope for Success in Multiple Sclerosis Therapy. Innov. Clin. Neurosci. 2014, 11, 23–36. [Google Scholar]
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.-F.; de Oliveira, A.C.; Santoro, A.; Raoul, J.-L.; Forner, A.; et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Marrero, J.A.; Kudo, M.; Venook, A.P.; Ye, S.-L.; Bronowicki, J.-P.; Chen, X.-P.; Dagher, L.; Furuse, J.; Geschwind, J.-F.H.; de Guevara, L.L.; et al. Observational registry of sorafenib use in clinical practice across Child-Pugh subgroups: The GIDEON study. J. Hepatol. 2016, 65, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- McNamara, M.G.; Slagter, A.E.; Nuttall, C.; Frizziero, M.; Pihlak, R.; Lamarca, A.; Tariq, N.; Valle, J.W.; Hubner, R.A.; Knox, J.J.; et al. Sorafenib as first-line therapy in patients with advanced Child-Pugh B hepatocellular carcinoma-a meta-analysis. Eur. J. Cancer 2018, 105, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ogasawara, S.; Chiba, T.; Ooka, Y.; Kanogawa, N.; Motoyama, T.; Suzuki, E.; Tawada, A.; Kanai, F.; Yoshikawa, M.; Yokosuka, O. Efficacy of sorafenib in intermediate-stage hepatocellular carcinoma patients refractory to transarterial chemoembolization. Oncology 2014, 87, 330–341. [Google Scholar] [CrossRef] [PubMed]
- Arizumi, T.; Ueshima, K.; Minami, T.; Kono, M.; Chishina, H.; Takita, M.; Kitai, S.; Inoue, T.; Yada, N.; Hagiwara, S.; et al. Effectiveness of sorafenib in patients with transcatheter arterial chemoembolization (TACE) refractory and intermediate-stage hepatocellular carcinoma. Liver Cancer 2015, 4, 253–262. [Google Scholar] [CrossRef]
- Ren, B.; Wang, W.; Shen, J.; Li, W.; Ni, C.; Zhu, X. Transarterial Chemoembolization (TACE) Combined with Sorafenib versus TACE Alone for Unresectable Hepatocellular Carcinoma: A Propensity Score Matching Study. J. Cancer 2019, 10, 1189–1196. [Google Scholar] [CrossRef]
- Meyer, T.; Fox, R.; Ma, Y.T.; Ross, P.J.; James, M.W.; Sturgess, R.; Stubbs, C.; Stocken, D.D.; Wall, L.; Watkinson, A.; et al. Sorafenib in combination with transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma (TACE 2): A randomised placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol. Hepatol. 2017, 2, 565–575. [Google Scholar] [CrossRef]
- Kudo, M.; Ueshima, K.; Ikeda, M.; Torimura, T.; Tanabe, N.; Aikata, H.; Izumi, N.; Yamasaki, T.; Nojiri, S.; Hino, K.; et al. Final Results of TACTICS: A Randomized, Prospective Trial Comparing Transarterial Chemoembolization Plus Sorafenib to Transarterial Chemoembolization Alone in Patients with Unresectable Hepatocellular Carcinoma. Liver Cancer 2022, 11, 354–367. [Google Scholar] [CrossRef]
- Merle, P.; Lim, H.Y.; Finn, R.S.; Ikeda, M.; Kudo, M.; Frenette, C.T.; Masi, G.; Kim, Y.J.; Gerolami, R.; Kurosaki, M.; et al. Sequential treatment with sorafenib followed by regorafenib in patients with unresectable hepatocellular carcinoma (HCC): Interim analysis of the observational REFINE study. J. Clin. Oncol. 2020, 38 (Suppl. S15), e16680. [Google Scholar] [CrossRef]
- Adhoute, X.; De Matharel, M.; Mineur, L.; Pénaranda, G.; Ouizeman, D.; Toullec, C.; Tran, A.; Castellani, P.; Rollet, A.; Oules, V.; et al. Second-line therapy for advanced hepatocellular carcinoma with regorafenib or cabozantinib: Multicenter French clinical experience in real-life after matching. World J. Gastrointest. Oncol. 2022, 14, 1510–1527. [Google Scholar] [CrossRef]
- Lee, I.-C.; Chao, Y.; Lee, P.-C.; Chen, S.-C.; Chi, C.-T.; Wu, C.-J.; Wu, K.-C.; Hou, M.-C.; Huang, Y.-H. Determinants of Survival and Post-Progression Outcomes by Sorafenib–Regorafenib Sequencing for Unresectable Hepatocellular Carcinoma. Cancers 2022, 14, 2014. [Google Scholar] [CrossRef] [PubMed]
- Sonbol, M.B.; Riaz, I.B.; Naqvi, S.Y.A.; Almquist, D.R.; Mina, S.; Almasri, J.; Shah, S.; Almader-Douglas, D.; Junior, P.L.S.U.; Mahipal, A.; et al. Systemic Therapy and Sequencing Options in Advanced Hepatocellular Carcinoma: A Systemic Review and Network Meta-analysis. JAMA Oncol. 2020, 6, e204930. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Cao, G.; Sun, B.; Wang, J.; Yan, D.; Xu, H.; Shi, O.; Liu, Z.; Zhi, W.; Xu, L.; et al. Regorafenib combined with transarterial chemoembolization for unresectable hepatocellular carcinoma: A real-world study. BMC Gastroenterol. 2021, 21, 393. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Ueshima, K.; Chan, S.; Minami, T.; Chishina, H.; Aoki, T.; Takita, M.; Hagiwara, S.; Minami, Y.; Ida, H.; et al. Lenvatinib as an Initial Treatment in Patients with Intermediate-Stage Hepatocellular Carcinoma Beyond Up-To-Seven Criteria and Child-Pugh A Liver Function: A Proof-Of-Concept Study. Cancers 2019, 11, 1084. [Google Scholar] [CrossRef] [PubMed]
- Biolato, M.; Gallusi, G.; Lavarone, M.; Cabibbo, G.; Racco, S.; De Santis, A.; Della Corte, C.; Maida, M.; Attili, A.F.; Sangiovanni, A.; et al. Prognostic ability of BCLC-B subclassifcation in patients with hepatocellular carcinoma undergoing transarterial chemoembolization. Ann. Hepatol. 2018, 17, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Ha, Y.; Shim, J.H.; Kim, S.O.; Lim, Y.-S.; Lee, H.C. Clinical appraisal of the recently proposed Barcelona Clinic Liver Cancer stage B subclassification by survival analysis. J. Gastroenterol. Hepatol. 2014, 29, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Weinmann, A.; Koch, S.; Sprinzl, M.; Kloeckner, R.; Schulze-Bergkamen, H.; Düber, C.; Lang, H.; Otto, G.; Wörns, M.A.; Galle, P.R. Survival analysis of proposed BCLC-B subgroups in hepatocellular carcinoma patients. Liver Int. 2015, 35, 591–600. [Google Scholar] [CrossRef]
- Wang, J.H.; Kee, K.M.; Lin, C.Y.; Hung, C.-H.; Chen, C.-H.; Lee, C.-M.; Lu, S.-N. Validation and modifcation of a proposed substaging system for patients with intermediate hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2015, 30, 358–363. [Google Scholar] [CrossRef]
- Kim, J.H.; Shim, J.H.; Lee, H.C.; Sung, K.-B.; Ko, H.-K.; Ko, G.-Y.; Gwon, D., II; Kim, J.W.; Lim, Y.-S.; Park, S.H. New intermediate stage subclassification for patients with hepatocellular carcinoma treated with trans arterial chemoembolization. Liver Int. 2017, 37, 1861–1868. [Google Scholar] [CrossRef]
- Giannini, E.G.; Moscatelli, A.; Pellegatta, G.; Vitale, A.; Farinati, F.; Ciccarese, F.; Piscaglia, F.; Rapaccini, G.L.; Di Marco, M.; Caturelli, E.; et al. Application of the intermediate-stage subclassification to patients with untreated hepatocellular carcinoma. Am. J. Gastroenterol. 2016, 111, 70–77. [Google Scholar] [CrossRef]
- Kobayashi, S.; Fukushima, T.; Ueno, M.; Moriya, S.; Chuma, M.; Numata, K.; Tsuruya, K.; Hirose, S.; Kagawa, T.; Hattori, N.; et al. A prospective observational cohort study of lenvatinib as initial treatment in patients with BCLC-defined stage B hepatocellular carcinoma. BMC Cancer 2022, 22, 517. [Google Scholar] [CrossRef] [PubMed]
- Patwala, K.; Prince, D.-S.; Celermajer, Y.; Alam, W.; Paul, E.; Strasser, S.I.; McCaughan, G.W.; Gow, P.; Sood, S.; Murphy, E.; et al. Lenvatinib for the treatment of hepatocellular carcinoma-a real-world multicenter Australian cohort study. Hepatol. Int. 2022, 16, 1170–1178. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Kumada, T.; Tada, T.; Tani, J.; Kariyama, K.; Fukunishi, S.; Atsukawa, M.; Hirooka, M.; Tsuji, K.; Ishikawa, T.; et al. Efficacy of lenvatinib for unresectable hepatocellular carcinoma based on background liver disease etiology: Multi-center retrospective study. Sci. Rep. 2021, 11, 16663. [Google Scholar] [CrossRef] [PubMed]
- Ando, Y.; Kawaoka, T.; Amioka, K.; Naruto, K.; Ogawa, Y.; Yoshikawa, Y.; Kikukawa, C.; Kosaka, Y.; Uchikawa, S.; Morio, K.; et al. Efficacy and Safety of Lenvatinib-Transcatheter Arterial Chemoembolization Sequential Therapy for Patients with Intermediate-Stage Hepatocellular Carcinoma. Oncology 2021, 99, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Fu, Z.; Li, X.; Zhong, J.; Chen, X.; Cao, K.; Ding, N.; Liu, L.; Zhang, X.; Zhai, J.; Qu, Z. Lenvatinib in combination with transarterial chemoembolization for treatment of unresectable hepatocellular carcinoma (uHCC): A retrospective controlled study. Hepatol. Int. 2021, 15, 663–675. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.; Gelfond, J.; Arora, S.P. Second-line treatment with nivolumab, cabozantinib, regorafenib, or best supportive care in patients with advanced hepatocellular carcinoma: Analysis at a Hispanic-majority NCI-designated cancer center. J. Gastrointest. Oncol. 2021, 12, 2943–2951. [Google Scholar] [CrossRef]
- Finkelmeiera, F.; Scheinerd, B.; Leyhf, C.; Best, J.; Fründt, T.W.; Czauderna, C.; Beutel, A.; Bettinger, D.; Weiß, J.; Meischl, T.; et al. Cabozantinib in Advanced Hepatocellular Carcinoma: Efficacy and Safety Data from an International Multicenter Real-Life Cohort. Liver Cancer 2021, 10, 360–369. [Google Scholar] [CrossRef]
- Kuzuya, T.; Kawabe, N.; Ariga, M.; Ohno, E.; Funasaka, K.; Nagasaka, M.; Nakagawa, Y.; Miyahara, R.; Shibata, T.; Takahara, T.; et al. Clinical Outcomes of Cabozantinib in Patients Previously Treated with Atezolizumab/Bevacizumab for Advanced Hepatocellular Carcinoma—Importance of Good Liver Function and Good Performance Status. Cancers 2023, 15, 2952. [Google Scholar] [CrossRef]
- Kelley, R.K.; Rimassa, L.; Cheng, A.-L.; Kaseb, A.; Qin, S.; Zhu, A.X.; Chan, S.L.; Melkadze, T.; Sukeepaisarnjaroen, W.; Breder, V.; et al. Cabozantinib plus atezolizumab versus sorafenib for advanced hepatocellular carcinoma (COSMIC-312): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2022, 23, 995–1008. [Google Scholar] [CrossRef]
- Singal, A.G.; Llovet, J.M.; Yarchoan, M.; Mehta, N.; Heimbach, J.K.; Dawson, L.A.; Jou, J.H.; Kulik, L.M.; Agopian, V.G.; Marrero, J.A.; et al. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology 2023, 78, 1922–1965. [Google Scholar] [CrossRef]
- Hiraoka, A.; Kumada, T.; Tada, T.; Hirooka, M.; Kariyama, K.; Tani, J.; Atsukawa, M.; Takaguchi, K.; Itobayashi, E.; Fukunishi, S.; et al. Atezolizumab plus bevacizumab treatment for unresectable hepatocellular carcinoma: Early clinical experience. Cancer Rep. 2022, 5, e1464. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Kumada, T.; Tada, T.; Hirooka, M.; Kariyama, K.; Tani, J.; Atsukawa, M.; Takaguchi, K.; Itobayashi, E.; Fukunishi, S.; et al. Does first-line treatment have prognostic impact for unresectable HCC?—Atezolizumab plus bevacizumab versus Lenvatinib. Cancer Med. 2023, 12, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Deng, H.; Sun, Y.; Zhang, Y.; Lu, Y.; Xu, G.; Huang, X. Efficacy and Safety of Regorafenib Plus Immune Checkpoint Inhibitors with or without TACE as a Second-Line Treatment for Advanced Hepatocellular Carcinoma: A Propensity Score Matching Analysis. J. Hepatocell. Carcinoma. 2023, 10, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wang, P.; Shang, L.; Zhang, Z.; Tian, Y.; Chen, X.; Ma, Y.; Shao, H. TACE plus tyrosine kinase inhibitors and immune checkpoint inhibitors versus TACE plus tyrosine kinase inhibitors for the treatment of patients with hepatocellular carcinoma: A meta-analysis and trial sequential analysis. Hepatol. Int. 2023. Online ahead of print. [Google Scholar] [CrossRef]
- Ahn, J.C.; Lee, Y.T.; Agopian, V.G.; Zhu, Y.; You, S.; Tseng, H.R.; Yang, J.D. Hepatocellular carcinoma surveillance: Current practice and future directions. Hepatoma. Res. 2022, 8, 10. [Google Scholar] [CrossRef]
- Kudo, M.; Arizumi, T.; Ueshima, K.; Sakurai, T.; Kitano, M.; Nishida, N. Subclassification of BCLC B Stage Hepatocellular Carcinoma and Treatment Strategies: Proposal of Modified Bolondi’s Subclassification (Kinki Criteria). Dig. Dis. 2015, 33, 751–758. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Chan, S.L.; Kudo, M.; Lau, G.; Kelley, R.K.; Furuse, J.; Sukeepaisarnjaroen, W.; Kang, Y.-K.; Dao, T.V.; De Toni, E.N.; et al. Phase 3 randomized, open-label, multicenter study of tremelimumab and durvalumab as first-line therapy in patients with unresectable hepatocellular carcinoma: HIMALAYA. J. Clin. Oncol. 2022, 40, 379. [Google Scholar] [CrossRef]
| Tyrosine Kinase Inhibitors | |||
|---|---|---|---|
| Sorafenib | |||
| Authors/Year/Ref No. | Study | Description | Results |
| Llovet J.M. et al. (2008) [32] | RCT | Sorafenib vs. placebo C-P A, PS 0–1 BCLC-C (80% in each group) | Sorafenib superior to placebo Median OS: 10.7 vs. 7.9 months; HR: 0.69; 95% CI: 0.55–0.87, p < 0.001. TTP: 5.5 vs. 2.8 months; HR: 0.58; 95% CI: 0.45–0.74, p < 0.001. AE: 80% vs. 50%. |
| Marrero J.A. et al. (2016) [33] | Observational | Sorafenib in C-P A vs. sorafenib in C-P B | Better OS in C-P A OS: 13.6 vs. 5.2 months. No significant differences in the type and severity of AE. |
| McNamara M.G. et al. (2018) [34] | Meta-analysis | 30 studies, 8678 C-P A/B patients in the sorafenib group as a first-line systemic treatment for advanced HCC | Better OS in C-P A Treatment discontinuation rates without HCC progression and treatment-related deaths without significant difference between C-P A and C-P B. OS: 4.6 months in C-P B vs. 8.8 in C-P A, p < 0.0001. |
| Ogasawara S. et al. (2014) [35] | Retrospective | 122 patients refractory to TACE 20 converted to SOR vs. 36 continued with TACE | Better results after switching to sorafenib TTP: 22.3 vs. 7.7 months (p = 0.001). OS: 25.4 vs. 11.5 months (p = 0.003). |
| Arizumi T. et al. (2015) [36] | Retrospective | 56 patients non-responders to TACE 32 switched to SOR vs. 24 continued with TACE | Better results after switching to sorafenib OS: 24.7 vs. 13.6 months (p = 0.002). |
| Ren B. et al. (2019) [37] | Retrospective | SOR+TACE vs. TACE | SOR/TACE superior to TACE in the entire population as well as in BCLC-B in particular OS: 29 ± 7.2 vs. 14.9 ± 1.1 months; p = 0.008). In the propensity matching cohort (61 patients in SOR/TACE vs. 122 patients in TACE → median OS: 29 ± 7.2 vs. 14.9 ± 1.5 months (HR 0.684, 95% CI: 0.470–0.997; p = 0.018). Exclusively in BCLC-B → median OS: 33 ± 9.8 vs. 25.3 ± 6.7 months (HR 0.620, 95% CI: 0.345–1.114; p = 0.041). |
| Meyer T. et al. (2017) [38] | RCT | SOR/TACE (n = 157) vs. TACE (n = 156) | No difference between SOR/TACE and TACE alone PFS: 238 vs. 235 days (HR 0.99; 95% CI: 0.77–1.27, p = 0.94). |
| Kudo M. et al. (2022) [39] | RCT | SOR/TACE vs. TACE BCLC-B: n = 44/80 (55%) in the first group and n = 34/76 (45%) in the second | SOR/TACE superior to TACE Median OS: 36.2 vs. 30.8 months (HR 0.861; 95% CI: 0.607–1.223; p = 0.40). The SOR/TACE offered a clinically meaningful prolongation of OS (ΔOS 5.4 months). PFS: 22.8 vs. 13.5 months (HR 0.661; 95% CI: 0.466–0.938; p = 0.02). |
| Regorafenib | |||
| Bruix J. et al. (2017) [16] | RCT | REG vs. placebo | REG superior to placebo OS: 10.6 vs. 7.8 months (HR: 0.63, p < 0.0001). PFS: 3.1 vs. 1.5 months. TTP: 3.2 vs. 1.5 months (HR: 0.44; 95% CI: 0.36–0.55, p < 0.001). AE: in 100% of regorafenib recipients and 93% of placebo recipients. No sub-analysis merely in BCLC-B. |
| Merle P. et al. (2020) [40] | Observational | 500 patients with HCC of whom 482 patients had been previously treated with SOR Subsequent switch to REG | Better results in an early switch from Sorafenib to Regorafenib Evaluation considering liver function at the time of the switch (C-P A vs. C-P B and ALBI-1 vs. ALBI-2 vs. ALBI-3). Median OS: 16 months in C-P A versus 8 months in C-P B. Median OS: 19.6 months in ALBI-1, 10.5 months in ALBI-2, 3.1 months in ALBI-3. |
| Han Y. et al. (2021) [44] | Retrospective | REG+TACE after failure to SOR | Median OS: 14.3 months. Median PFS: 9.1 months. Median TTP: 9.1 months. The BCLC stage was not found to correlate with OS, PFS, and TTP in Cox regression analysis. |
| Lee I.-C. et al. (2022) [42] | Retrospective | 108 patients BCLC B/C: 18.5%/81.5% ALBI 1/2/3: 40.7%/58.3%/0.9% C-P A/B: 84.3%/15.7% REG after SOR | Better results in early switch from sorafenib to regorafenib Evaluation considering BCLC stage and liver function at the time of the switch (ALBI-1 vs. ALBI-2 vs. ALBI-3). No significant difference in PFS between BCLC-B and BCLC-C. Better OS in lower ALBI: 2–3/1 → HR 2.758, 95% CI: 1.458–5.216, p = 0.002. Better post-progression survival in lower ALBI: 2/1 → HR 4.499, 95% CI: 1.541–13.137, p = 0.006 and 3/1 → HR 26.926, 95% CI: 6.638–109.227, p < 0.001. |
| Lenvatinib | |||
| Kudo M et al. (2019) [45] | Prospective | 176 patients Lenvatinib vs. TACE in BCLC-B, C-P A No prior TACE/systemic treatment 30 patients in the lenvatinib group vs. 60 patients in the TACE group | Lenvatinib superior to TACE Change in ALBI score during treatment: −2.61 to −2.61 in lenvatinib patients (p = 0.254) and from −2.66 to −2.09 in TACE patients (p < 0.01). ORR: 73.3% vs. 33.3%; p < 0.001. Median PFS: 16 vs. 3 months; p < 0.001. OS: 37.9 vs. 21.3 months; HR: 0.48, p < 0.01. |
| Kobayashi S. et al. (2022) [52] | Prospective | Lenvatinib vs. TACE (historical controls) in BCLC-B2, C-P: 5–6 31 patients | Lenvatinib potentially superior to TACE Historical controls of TACE: OS and 1-year survival rates for substage B2 patients: 15.6–26.9 months and 59.2–75.5%, respectively. With lenvatinib: Median OS: 17.0 months. 1-year survival rate: 71.0%. 2-year survival rate: 32.3%. Median PFS: 10.4 months. 1-year PFS rate: 42%. ORR: 22.6% and DCR: 90.3%. |
| Patwala K. et al. (2022) [53] | Retrospective | 155 patients (BCLC stage C (69.7%) and BCLC stage B (27.7%); C-P A/B/C: 78.8%/19.7%/1.5%) Efficacy of lenvatinib | Better results in C-P A and BCLC-B stage Median OS in the entire population: 7.7 months. Median PFS in the entire population: 5.3 months. OS: C-P B/C vs. C-P A: 5.6 vs. 12.5 months; p < 0.01. In multivariate analysis: BCLC stage HR: 2.50, 95% CI: 1.40–4.45, p < 0.01. A higher baseline C-P score was an independent predictor of PFS (HR: 1.24, 95% CI: 1.01–1.52, p = 0.04). |
| Hiraoka A. et al. (2021) [54] | Retrospective | To determine whether the cause of liver cirrhosis (NAFLD vs. non-NAFLD) had any additional impact on OS and PFS of HCC patients treated with lenvatinib | Cox regression analysis: elevated ALT (≥30 U/L) (HR 1.247, p = 0.029), modified ALBI grade 2b (HR 1.236, p = 0.047), elevated AFP (≥400 ng/mL) (HR 1.294, p = 0.014), and NAFLD (HR 0.763, p = 0.036) were significant prognostic factors of PFS. Higher AFP (≥400 ng/mL) (HR 1.402, p = 0.009), BCLC-C stage (HR 1.297, p = 0.035), later introduction of lenvatinib (HR 0.737, p = 0.014), and modified ALBI grade 2b (HR 1.875, p < 0.001) were independently associated with OS. |
| Ando Y. et al. (2021) [55] | Prospective | 88 BCLC-B subjects previously controlled by taking lenvatinib Two groups: 30 patients continued with lenvatinib plus TACE 58 patients remained on lenvatinib BCLC stage B (100%); beyond up-to-seven criteria (68.4% vs. 63.16%); ALBI grade 2 (31.58% vs. 31.58%) | Lenvatinib/TACE potentially superior to lenvatinib ORR: 63.2% vs. 63.2%. Multivariate analysis: addition of TACE (HR: 0.264, 95% CI: 0.087–0.802, p = 0.019) and C-P score 5 (HR: 0.223, 95% CI: 0.070–0.704, p = 0.011) were independent predictors of PFS. Median PFS: 11.6 vs. 10.1 months CR: 15.8% vs. 10.5%. |
| Fu Z. et al. (2021) [56] | Retrospective | LEN/TACE vs. TACE | Lenvatinib/TACE superior to TACE 1-year OS: 88.4% vs. 79.2%. 2-year OS: 79.8% vs. 49.2%. 1-year PFS: 78.4% vs. 64.7 (p < 0.001). 2-year PFS rate: 45.5% vs. 38.0% (p < 0.001). ORR: 68.3% vs. 31.7% (p < 0.001). In BCLC-B patients: ORR: 69.7% vs. 38.5%, p = 0.016. PFS: HR: 0.149; 95% CI: 0.059–0.379, p < 0.001. OS: HR: 0.28; 95% CI: 0.092–0.853, p = 0.07. |
| Immune Checkpoint Inhibitors (ICIs) | |||
|---|---|---|---|
| Authors/Year/Ref No. | Study | Description | Results |
| Hiraoka A. et al. (2022) [62] | Prospective | 171 HCC patients treated with atezolizumab plus bevacizumab. A number of patients had BCLC-B HCCs (n = 68, 40%) | ORR in 6 weeks of 10.6%. DCR in 6 weeks of 79.6%. The study did not provide comparative data regarding ORR and DCR between BCLC-B and BCLC-C patients. |
| Hiraoka A. et al. (2023) [63] | Prospective | Atezolizumab/bevacizumab vs. lenvatinib (BCLC-B/C) | Atezolizumab/bevacizumab potentially superior to lenvatinib No significant differences in response rates of the two groups by using the m-RECIST criteria. PFS and OS were comparable between the two groups. After adjusting with inverse probability weighting, the Atez/Bev group showed better PFS (0.5-/1-/1.5-years: 56.6%/31.6%/non-estimable vs. 48.6%/20.4%/11.2%, p < 0.0001) and OS (0.5-/1-/1.5-years: 89.6%/67.2%/58.1% vs. 77.8%/66.2%/52.7%, p = 0.002). |
| Yang X. et al. (2023) [64] | Retrospective | Regorafenib plus ICIs and TACE (R+ICIs+TACE) vs. regorafenib plus ICIs (R+ICIs), as second-line treatment for patients with HCC | R/ICIs/TACE superior to R/TACE After propensity score matching: ORR: 34.8% vs. 4.3%, p = 0.009. PFS: 5.8 vs. 2.6 months, p = 0.014. Cox regression model: BCLC stage was not found to correlate with PFS or OS. |
| Liu et al. (2023) [65] | Meta-analysis | 5 studies, 425 patients TACE plus TKIs plus ICIs vs. TACE plus TKIs | ICIs/TKIs/TACE superior to TKIs/TACE Triple treatment → ORR (RR 1.53, 95% CI: 1.27–1.85, p < 0.01), PFS→ mean difference: 4.51 months, p < 0.01 OS→ mean difference: 5.75 months, p < 0.01. Fixed-effects models: OS among C-P A patients, considering treatment options: TACE/TKIs/ICIs vs. TACE/TKIs: 22.6 vs. 15.1 months, p = 0.05. OS among C-P B subjects: TACE/TKIs/ICIs and TACE/TKIs: 12.9 vs. 6.5 months, p < 0.01. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karagiannakis, D.S. Systemic Treatment in Intermediate Stage (Barcelona Clinic Liver Cancer-B) Hepatocellular Carcinoma. Cancers 2024, 16, 51. https://doi.org/10.3390/cancers16010051
Karagiannakis DS. Systemic Treatment in Intermediate Stage (Barcelona Clinic Liver Cancer-B) Hepatocellular Carcinoma. Cancers. 2024; 16(1):51. https://doi.org/10.3390/cancers16010051
Chicago/Turabian StyleKaragiannakis, Dimitrios S. 2024. "Systemic Treatment in Intermediate Stage (Barcelona Clinic Liver Cancer-B) Hepatocellular Carcinoma" Cancers 16, no. 1: 51. https://doi.org/10.3390/cancers16010051
APA StyleKaragiannakis, D. S. (2024). Systemic Treatment in Intermediate Stage (Barcelona Clinic Liver Cancer-B) Hepatocellular Carcinoma. Cancers, 16(1), 51. https://doi.org/10.3390/cancers16010051






