Artificial Intelligence and Panendoscopy—Automatic Detection of Clinically Relevant Lesions in Multibrand Device-Assisted Enteroscopy
Abstract
Simple Summary
Abstract
1. Introduction
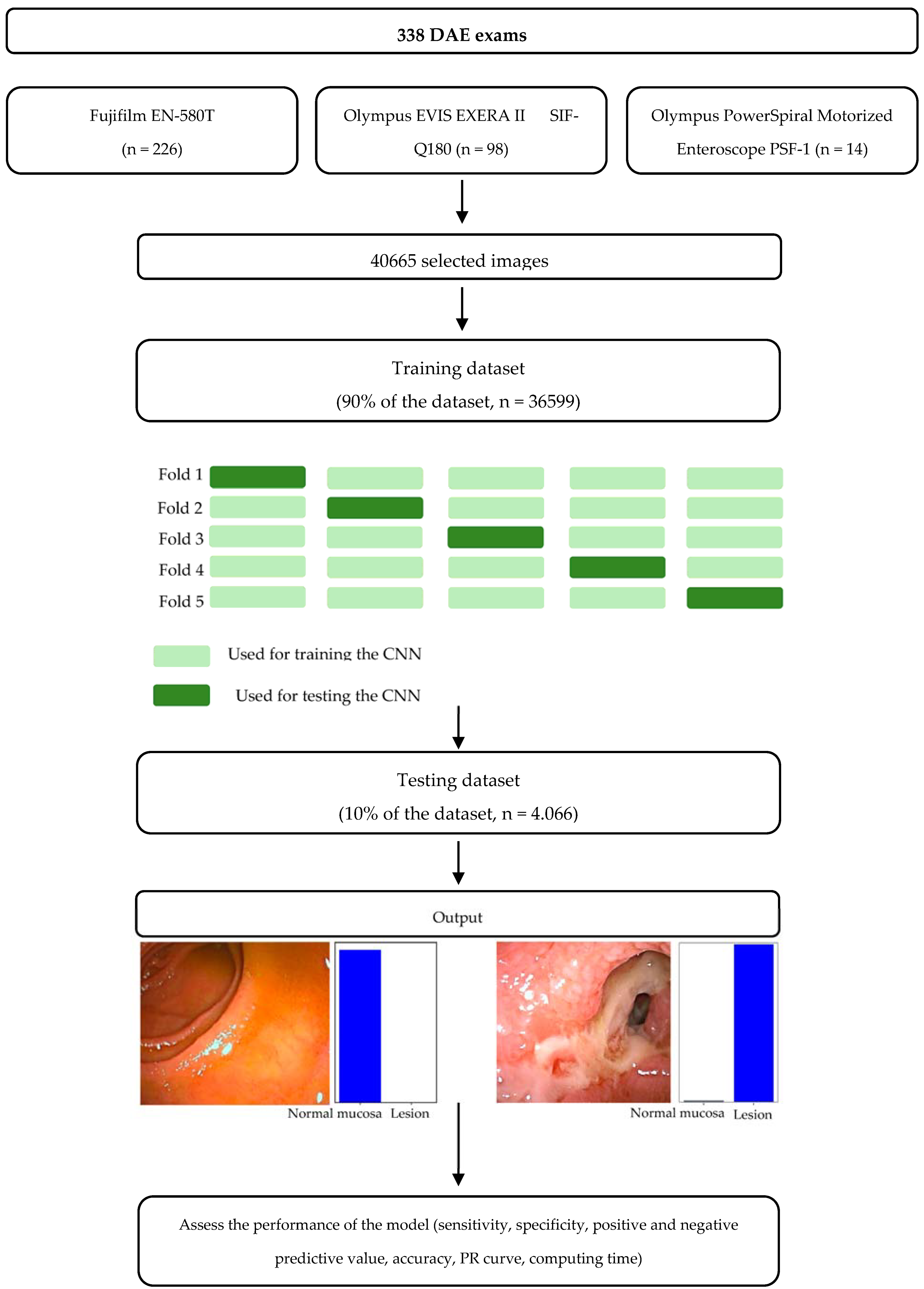
2. Materials and Methods
2.1. Study Design
2.2. Lesion Classification
2.3. CNN Development
2.4. Performance Measures and Statistical Analysis
3. Results
3.1. Construction of the Network
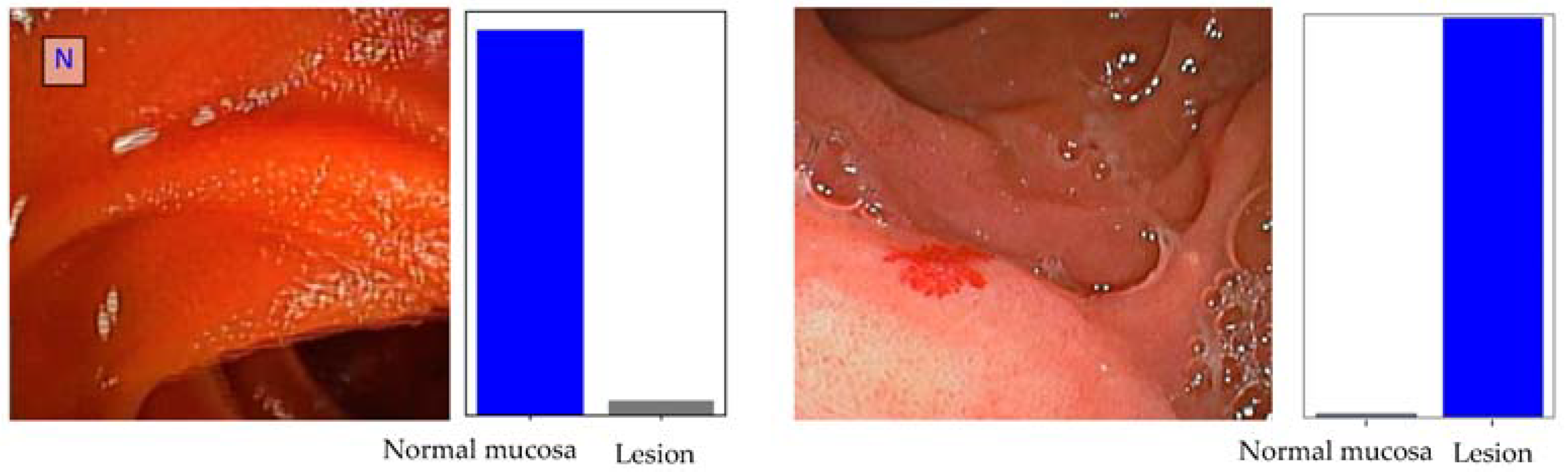
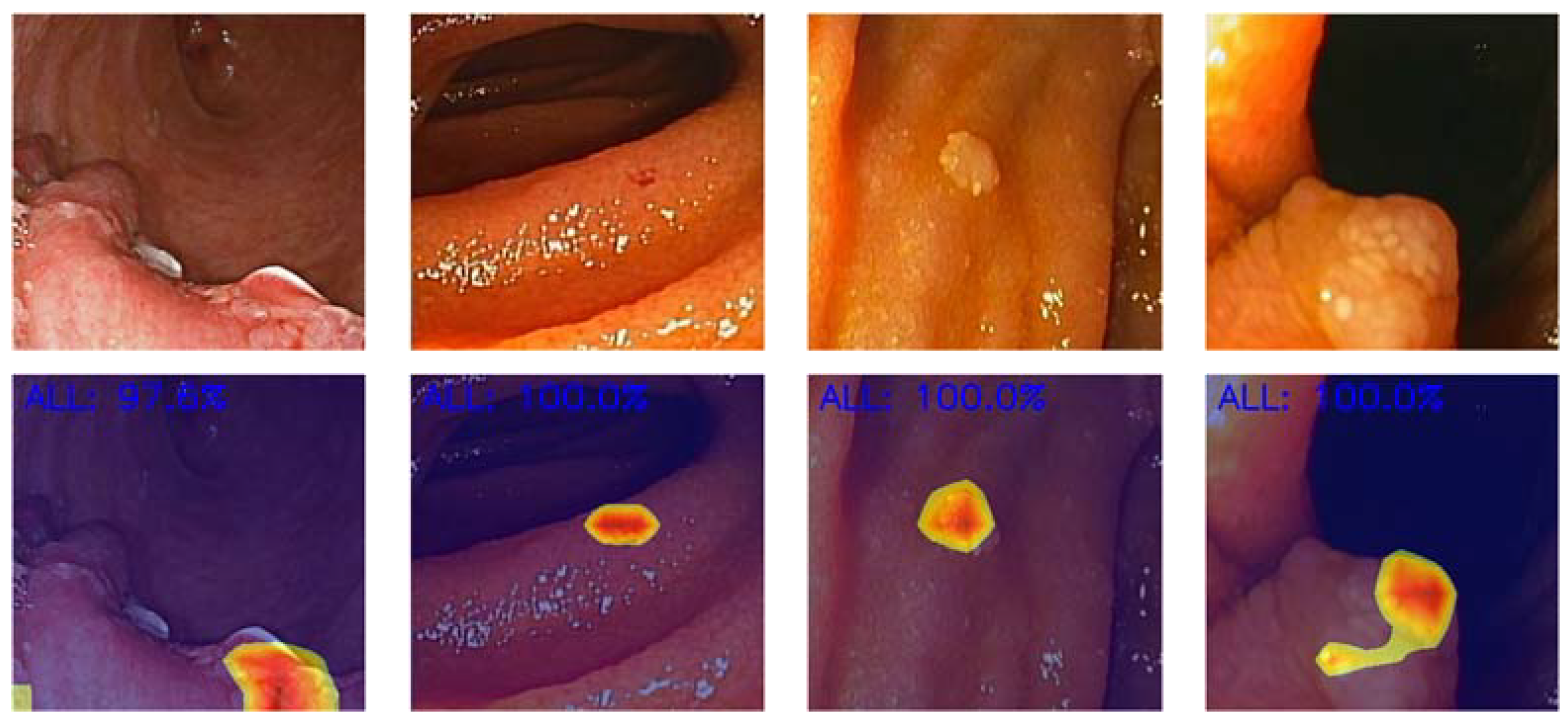
3.2. Global Performance of the Network
3.3. Convolutional Neural Network Computational Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pennazio, M.; Rondonotti, E.; Despott, E.J.; Dray, X.; Keuchel, M.; Moreels, T.; Sanders, D.S.; Spada, C.; Carretero, C.; Cortegoso Valdivia, P.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2022. Endoscopy 2023, 55, 58–95. [Google Scholar] [CrossRef]
- Beyna, T.; Arvanitakis, M.; Schneider, M.; Gerges, C.; Hoellerich, J.; Deviere, J.; Neuhaus, H. Total motorized spiral enteroscopy: First prospective clinical feasibility trial. Gastrointest. Endosc. 2021, 93, 1362–1370. [Google Scholar] [CrossRef]
- Rondonotti, E.; Spada, C.; Adler, S.; May, A.; Despott, E.J.; Koulaouzidis, A.; Panter, S.; Domagk, D.; Fernandez-Urien, I.; Rahmi, G.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy 2018, 50, 423–446. [Google Scholar] [CrossRef]
- Goenka, M.K.; Majumder, S.; Kumar, S.; Sethy, P.K.; Goenka, U. Single center experience of capsule endoscopy in patients with obscure gastrointestinal bleeding. World J. Gastroenterol. 2011, 17, 774–778. [Google Scholar] [CrossRef]
- Bettenworth, D.; Bokemeyer, A.; Kou, L.; Lopez, R.; Bena, J.F.; El Ouali, S.; Mao, R.; Kurada, S.; Bhatt, A.; Beyna, T.; et al. Systematic review with meta-analysis: Efficacy of balloon-assisted enteroscopy for dilation of small bowel Crohn’s disease strictures. Aliment. Pharmacol. Ther. 2020, 52, 1104–1116. [Google Scholar] [CrossRef]
- Rondonotti, E.; Koulaouzidis, A.; Yung, D.E.; Reddy, S.N.; Georgiou, J.; Pennazio, M. Neoplastic Diseases of the Small Bowel. Gastrointest. Endosc. Clin. N. Am. 2017, 27, 93–112. [Google Scholar] [CrossRef]
- Sakamoto, H.; Yamamoto, H.; Hayashi, Y.; Yano, T.; Miyata, T.; Nishimura, N.; Shinhata, H.; Sato, H.; Sunada, K.; Sugano, K. Nonsurgical management of small-bowel polyps in Peutz-Jeghers syndrome with extensive polypectomy by using double-balloon endoscopy. Gastrointest. Endosc. 2011, 74, 328–333. [Google Scholar] [CrossRef]
- Teshima, C.W.; Kuipers, E.J.; van Zanten, S.V.; Mensink, P.B. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: An updated meta-analysis. J. Gastroenterol. Hepatol. 2011, 26, 796–801. [Google Scholar] [CrossRef]
- Despott, E.J.; Murino, A.; Nakamura, M.; Bourikas, L.; Fraser, C. A prospective randomised study comparing double-balloon colonoscopy and conventional colonoscopy in pre-defined technically difficult cases. Dig. Liver Dis. 2017, 49, 507–513. [Google Scholar] [CrossRef]
- Nehme, F.; Goyal, H.; Perisetti, A.; Tharian, B.; Sharma, N.; Tham, T.C.; Chhabra, R. The Evolution of Device-Assisted Enteroscopy: From Sonde Enteroscopy to Motorized Spiral Enteroscopy. Front. Med. 2021, 8, 792668. [Google Scholar] [CrossRef]
- Yamashita, R.; Nishio, M.; Do, R.K.G.; Togashi, K. Convolutional neural networks: An overview and application in radiology. Insights Imaging 2018, 9, 611–629. [Google Scholar] [CrossRef]
- Khurshid, S.; Friedman, S.; Reeder, C.; Di Achille, P.; Diamant, N.; Singh, P.; Harrington, L.X.; Wang, X.; Al-Alusi, M.A.; Sarma, G.; et al. ECG-Based Deep Learning and Clinical Risk Factors to Predict Atrial Fibrillation. Circulation 2022, 145, 122–133. [Google Scholar] [CrossRef]
- Sanyal, P.; Dey, P. Using a deep learning neural network for the identification of malignant cells in effusion cytology material. Cytopathology 2023, 34, 466–471. [Google Scholar] [CrossRef]
- Khan, R.A.; Fu, M.; Brent, B.; Luo, Y.; Wu, F.X. A multi-modal deep neural network for multi-class liver cancer diagnosis. Neural Netw. 2023, 165, 553–561. [Google Scholar] [CrossRef]
- Mascarenhas, M.; Ribeiro, T.; Afonso, J.; Ferreira, J.P.S.; Cardoso, H.; Andrade, P.; Parente, M.P.L.; Jorge, R.N.; Mascarenhas Saraiva, M.; Macedo, G. Deep learning and colon capsule endoscopy: Automatic detection of blood and colonic mucosal lesions using a convolutional neural network. Endosc. Int. Open 2022, 10, E171–E177. [Google Scholar] [CrossRef]
- Chu, Y.; Huang, F.; Gao, M.; Zou, D.W.; Zhong, J.; Wu, W.; Wang, Q.; Shen, X.N.; Gong, T.T.; Li, Y.Y.; et al. Convolutional neural network-based segmentation network applied to image recognition of angiodysplasias lesion under capsule endoscopy. World J. Gastroenterol. 2023, 29, 879–889. [Google Scholar] [CrossRef]
- Soffer, S.; Klang, E.; Shimon, O.; Nachmias, N.; Eliakim, R.; Ben-Horin, S.; Kopylov, U.; Barash, Y. Deep learning for wireless capsule endoscopy: A systematic review and meta-analysis. Gastrointest. Endosc. 2020, 92, 831–839. [Google Scholar] [CrossRef]
- Mascarenhas Saraiva, M.; Ribeiro, T.; Afonso, J.; Andrade, P.; Cardoso, P.; Ferreira, J.; Cardoso, H.; Macedo, G. Deep Learning and Device-Assisted Enteroscopy: Automatic Detection of Gastrointestinal Angioectasia. Medicina 2021, 57, 1378. [Google Scholar] [CrossRef]
- Martins, M.; Mascarenhas, M.; Afonso, J.; Ribeiro, T.; Cardoso, P.; Mendes, F.; Cardoso, H.; Andrade, P.; Ferreira, J.; Macedo, G. Deep-Learning and Device-Assisted Enteroscopy: Automatic Panendoscopic Detection of Ulcers and Erosions. Medicina 2023, 59, 172. [Google Scholar] [CrossRef]
- Cardoso, P.; Saraiva, M.M.; Afonso, J.; Ribeiro, T.; Andrade, P.; Ferreira, J.; Cardoso, H.; Macedo, G. Artificial Intelligence and Device-Assisted Enteroscopy: Automatic Detection of Enteric Protruding Lesions Using a Convolutional Neural Network. Clin. Transl. Gastroenterol. 2022, 13, e00514. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine Learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Hawkins, D.M.; Basak, S.C.; Mills, D. Assessing model fit by cross-validation. J. Chem. Inf. Comput. Sci. 2003, 43, 579–586. [Google Scholar] [CrossRef]
- Tougui, I.; Jilbab, A.; Mhamdi, J.E. Impact of the Choice of Cross-Validation Techniques on the Results of Machine Learning-Based Diagnostic Applications. Healthc. Inform. Res. 2021, 27, 189–199. [Google Scholar] [CrossRef]
- Movahedi, F.; Padman, R.; Antaki, J.F. Limitations of receiver operating characteristic curve on imbalanced data: Assist device mortality risk scores. J. Thorac. Cardiovasc. Surg. 2023, 165, 1433–1442.e1432. [Google Scholar] [CrossRef]
- Halligan, S.; Altman, D.G.; Mallett, S. Disadvantages of using the area under the receiver operating characteristic curve to assess imaging tests: A discussion and proposal for an alternative approach. Eur. Radiol. 2015, 25, 932–939. [Google Scholar] [CrossRef]
- Saito, T.; Rehmsmeier, M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE 2015, 10, e0118432. [Google Scholar] [CrossRef]
- Belle, V.; Papantonis, I. Principles and Practice of Explainable Machine Learning. Front. Big Data 2021, 4, 688969. [Google Scholar] [CrossRef]
- Linardatos, P.; Papastefanopoulos, V.; Kotsiantis, S. Explainable AI: A Review of Machine Learning Interpretability Methods. Entropy 2020, 23, 18. [Google Scholar] [CrossRef]
- Mascarenhas, M.; Afonso, J.; Ribeiro, T.; Andrade, P.; Cardoso, H.; Macedo, G. The Promise of Artificial Intelligence in Digestive Healthcare and the Bioethics Challenges It Presents. Medicina 2023, 59, 790. [Google Scholar] [CrossRef]
- Watson, D.S.; Krutzinna, J.; Bruce, I.N.; Griffiths, C.E.; McInnes, I.B.; Barnes, M.R.; Floridi, L. Clinical applications of machine learning algorithms: Beyond the black box. BMJ 2019, 364, l886. [Google Scholar] [CrossRef]
- Taddeo, M.; Floridi, L. How AI can be a force for good. Science 2018, 361, 751–752. [Google Scholar] [CrossRef]
- He, J.; Baxter, S.L.; Xu, J.; Xu, J.; Zhou, X.; Zhang, K. The practical implementation of artificial intelligence technologies in medicine. Nat. Med. 2019, 25, 30–36. [Google Scholar] [CrossRef]
- Wilkinson, M.D.; Dumontier, M.; Aalbersberg, I.J.; Appleton, G.; Axton, M.; Baak, A.; Blomberg, N.; Boiten, J.W.; da Silva Santos, L.B.; Bourne, P.E.; et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci. Data 2016, 3, 160018. [Google Scholar] [CrossRef]
- Zhang, J.; Ashrafian, H.; Delaney, B.; Darzi, A. Impact of primary to secondary care data sharing on care quality in NHS England hospitals. NPJ Digit. Med. 2023, 6, 144. [Google Scholar] [CrossRef]
- Rajamani, S.; Chakoian, H.; Bieringer, A.; Lintelmann, A.; Sanders, J.; Ostadkar, R.; Saupe, A.; Grilli, G.; White, K.; Solarz, S.; et al. Development and implementation of an interoperability tool across state public health agency’s disease surveillance and immunization information systems. JAMIA Open 2023, 6, ooad055. [Google Scholar] [CrossRef]
- Benhamou, P.Y.; Adenis, A.; Lablanche, S.; Franc, S.; Amadou, C.; Penfornis, A.; Kariyawasam, D.; Beltrand, J.; Charpentier, G. First Generation of a Modular Interoperable Closed-Loop System for Automated Insulin Delivery in Patients With Type 1 Diabetes: Lessons From Trials and Real-Life Data. J. Diabetes Sci. Technol. 2023, 17, 1433–1439. [Google Scholar] [CrossRef]
- Lavin, A.; Gilligan-Lee, C.M.; Visnjic, A.; Ganju, S.; Newman, D.; Ganguly, S.; Lange, D.; Baydin, A.G.; Sharma, A.; Gibson, A.; et al. Technology readiness levels for machine learning systems. Nat. Commun. 2022, 13, 6039. [Google Scholar] [CrossRef]
- Afonso, J.; Saraiva, M.M.; Ferreira, J.P.S.; Cardoso, H.; Ribeiro, T.; Andrade, P.; Parente, M.; Jorge, R.N.; Macedo, G. Automated detection of ulcers and erosions in capsule endoscopy images using a convolutional neural network. Med. Biol. Eng. Comput. 2022, 60, 719–725. [Google Scholar] [CrossRef]
- Ribeiro, T.; Mascarenhas Saraiva, M.J.; Afonso, J.; Cardoso, P.; Mendes, F.; Martins, M.; Andrade, A.P.; Cardoso, H.; Mascarenhas Saraiva, M.; Ferreira, J.; et al. Design of a Convolutional Neural Network as a Deep Learning Tool for the Automatic Classification of Small-Bowel Cleansing in Capsule Endoscopy. Medicina 2023, 59, 810. [Google Scholar] [CrossRef]
- Cherubini, A.; Dinh, N.N. A Review of the Technology, Training, and Assessment Methods for the First Real-Time AI-Enhanced Medical Device for Endoscopy. Bioengineering 2023, 10, 404. [Google Scholar] [CrossRef]
- Singh, P.; Singla, V.; Bopanna, S.; Shawl, M.R.; Garg, P.; Agrawal, J.; Arya, A.; Mittal, V.; Bhargava, R.; Madan, K. Safety and efficacy of the novel motorized power spiral enteroscopy: A single-center experience. DEN Open 2023, 3, e148. [Google Scholar] [CrossRef] [PubMed]
- Rondonotti, E.; Pennazio, M. Colon capsule for panendoscopy: A narrow window of opportunity. Endosc. Int. Open 2021, 9, E1860–E1862. [Google Scholar] [CrossRef] [PubMed]
- Vuik, F.E.R.; Moen, S.; Spaander, M.C.W. Colon capsule endoscopy as panendoscopy: Using current knowledge to enhance possibilities. Endosc. Int. Open 2022, 10, E584. [Google Scholar] [CrossRef] [PubMed]
- Majtner, T.; Brodersen, J.B.; Herp, J.; Kjeldsen, J.; Halling, M.L.; Jensen, M.D. A deep learning framework for autonomous detection and classification of Crohn’s disease lesions in the small bowel and colon with capsule endoscopy. Endosc. Int. Open 2021, 9, E1361–E1370. [Google Scholar] [CrossRef]
- Gilabert, P.; Vitria, J.; Laiz, P.; Malagelada, C.; Watson, A.; Wenzek, H.; Segui, S. Artificial intelligence to improve polyp detection and screening time in colon capsule endoscopy. Front. Med. 2022, 9, 1000726. [Google Scholar] [CrossRef]
| Experts Classification | |||
|---|---|---|---|
| Normal Mucosa | Clinically Relevant Lesions | ||
| CNN Classification | Normal mucosa | 3168 (0.97) | 96 (0.03) |
| Clinically relevant lesions | 34 (0.04) | 769 (0.96) | |
| Sn | Sp | PPV | NPV | Acc | |
|---|---|---|---|---|---|
| Fold 1 | 0.87 | 0.95 | 0.81 | 0.96 | 0.93 |
| Fold 2 | 0.87 | 0.97 | 0.90 | 0.96 | 0.95 |
| Fold 3 | 0.89 | 0.99 | 0.97 | 0.97 | 0.97 |
| Fold 4 | 0.91 | 0.99 | 0.97 | 0.98 | 0.97 |
| Fold 5 | 0.90 | 0.99 | 0.98 | 0.97 | 0.97 |
| Training dataset mean N = 38,599 | 0.887 (0.880–0.895) | 0.980 (0.978–0.981) | 0.926 (0.920–0.931) | 0.970 (0.968–0.972) | 0.960 (0.958–0.962) |
| Testing dataset N = 4068 | 0.889 (0.866–0.909) | 0.989 (0.985–0.993) | 0.958 (0.942–0.969) | 0.971 (0.965–0.976) | 0.968 (0.962–0.973) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendes, F.; Mascarenhas, M.; Ribeiro, T.; Afonso, J.; Cardoso, P.; Martins, M.; Cardoso, H.; Andrade, P.; Ferreira, J.P.S.; Mascarenhas Saraiva, M.; et al. Artificial Intelligence and Panendoscopy—Automatic Detection of Clinically Relevant Lesions in Multibrand Device-Assisted Enteroscopy. Cancers 2024, 16, 208. https://doi.org/10.3390/cancers16010208
Mendes F, Mascarenhas M, Ribeiro T, Afonso J, Cardoso P, Martins M, Cardoso H, Andrade P, Ferreira JPS, Mascarenhas Saraiva M, et al. Artificial Intelligence and Panendoscopy—Automatic Detection of Clinically Relevant Lesions in Multibrand Device-Assisted Enteroscopy. Cancers. 2024; 16(1):208. https://doi.org/10.3390/cancers16010208
Chicago/Turabian StyleMendes, Francisco, Miguel Mascarenhas, Tiago Ribeiro, João Afonso, Pedro Cardoso, Miguel Martins, Hélder Cardoso, Patrícia Andrade, João P. S. Ferreira, Miguel Mascarenhas Saraiva, and et al. 2024. "Artificial Intelligence and Panendoscopy—Automatic Detection of Clinically Relevant Lesions in Multibrand Device-Assisted Enteroscopy" Cancers 16, no. 1: 208. https://doi.org/10.3390/cancers16010208
APA StyleMendes, F., Mascarenhas, M., Ribeiro, T., Afonso, J., Cardoso, P., Martins, M., Cardoso, H., Andrade, P., Ferreira, J. P. S., Mascarenhas Saraiva, M., & Macedo, G. (2024). Artificial Intelligence and Panendoscopy—Automatic Detection of Clinically Relevant Lesions in Multibrand Device-Assisted Enteroscopy. Cancers, 16(1), 208. https://doi.org/10.3390/cancers16010208










