Predictive Factors of Complete Response to Transarterial Chemoembolization in Intermediate Stage Hepatocellular Carcinoma beyond Up-To-7 Criteria
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
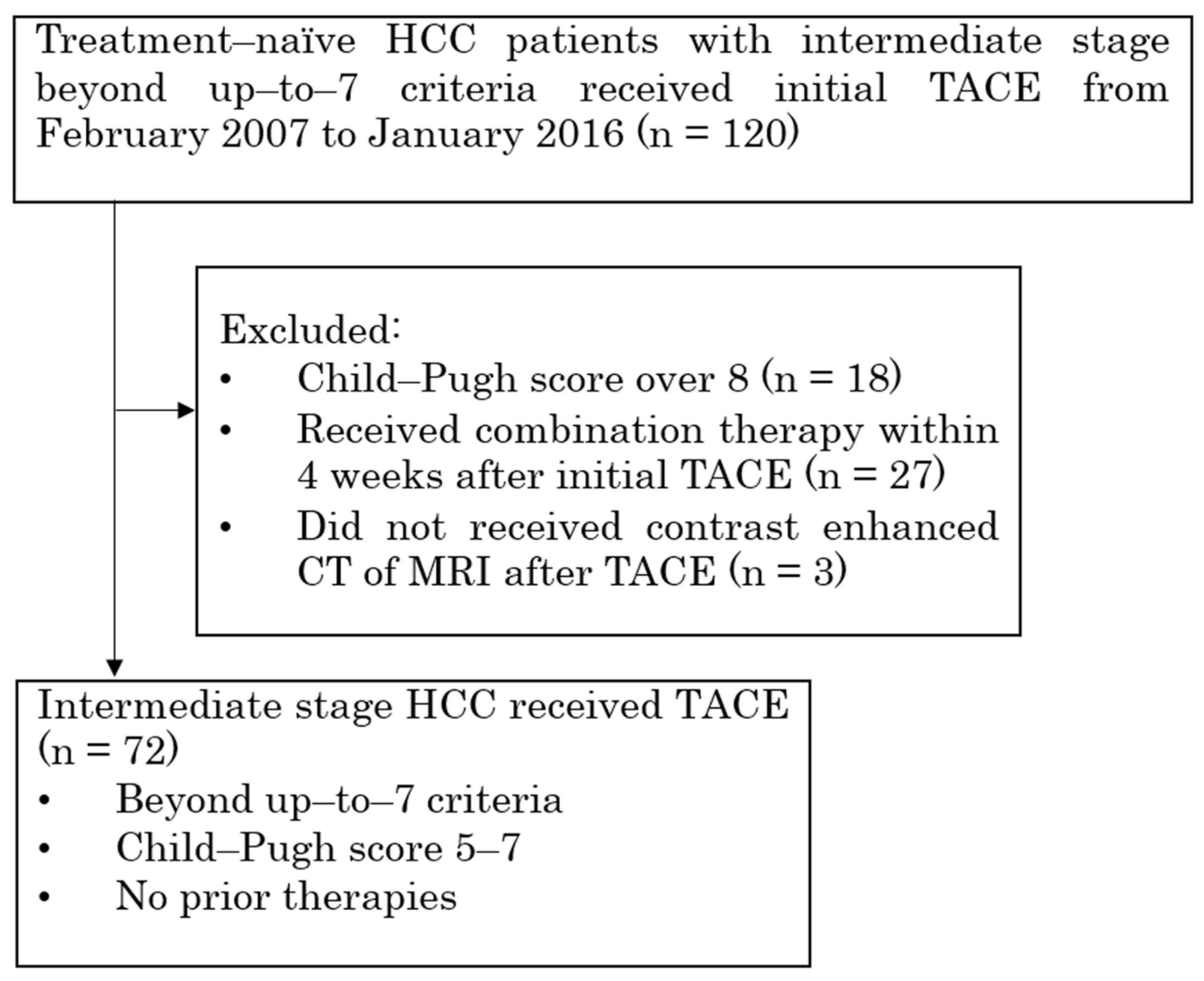
2.1. Patient Data Collection and Eligibility Criteria
2.2. TACE Procedure
2.3. Follow-Up and Evaluations
2.4. Definition
2.5. Statistical Analysis
3. Results
3.1. Patients
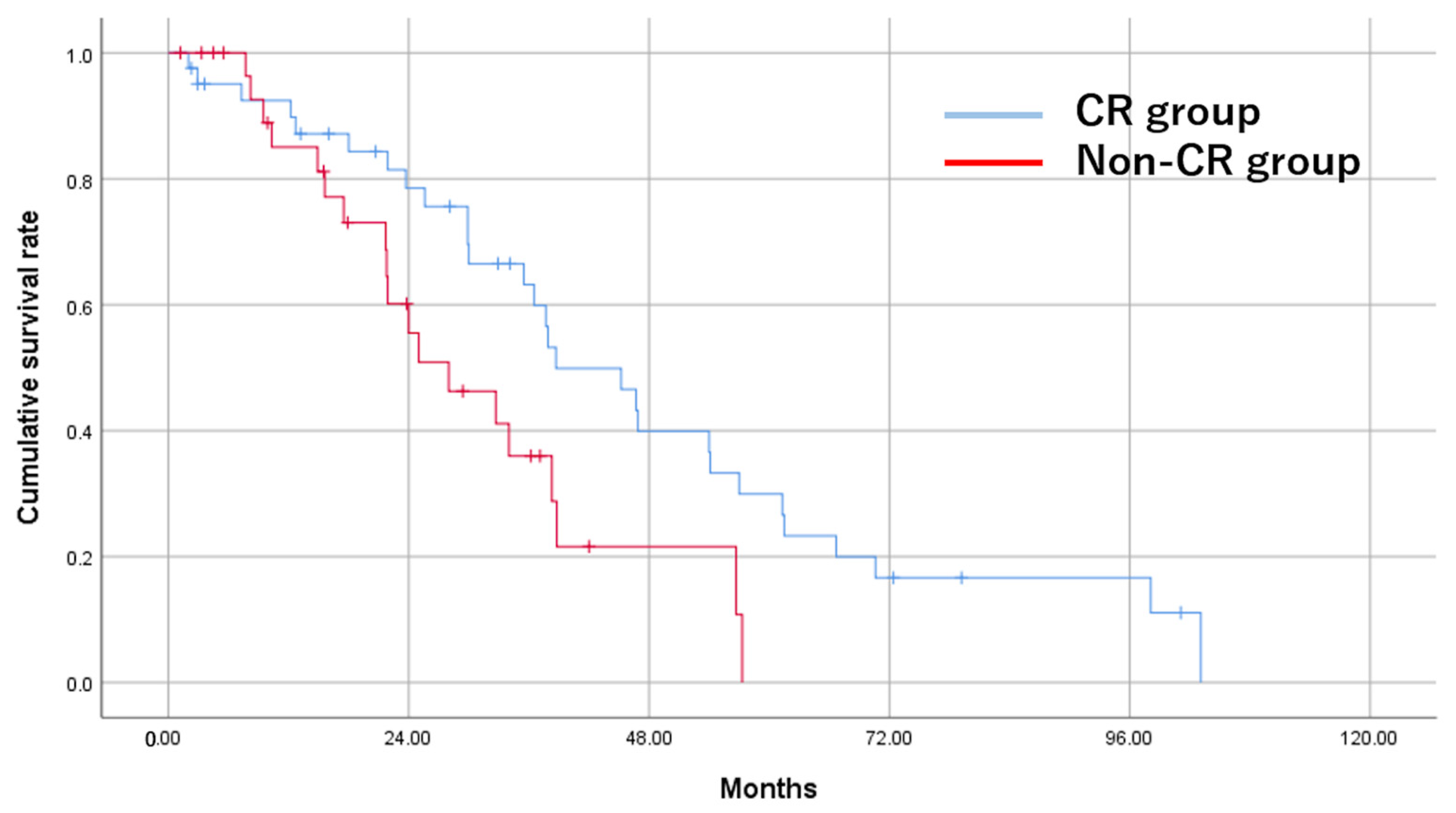
3.2. Tumor Response
3.3. Rate of Liver Function Deterioration
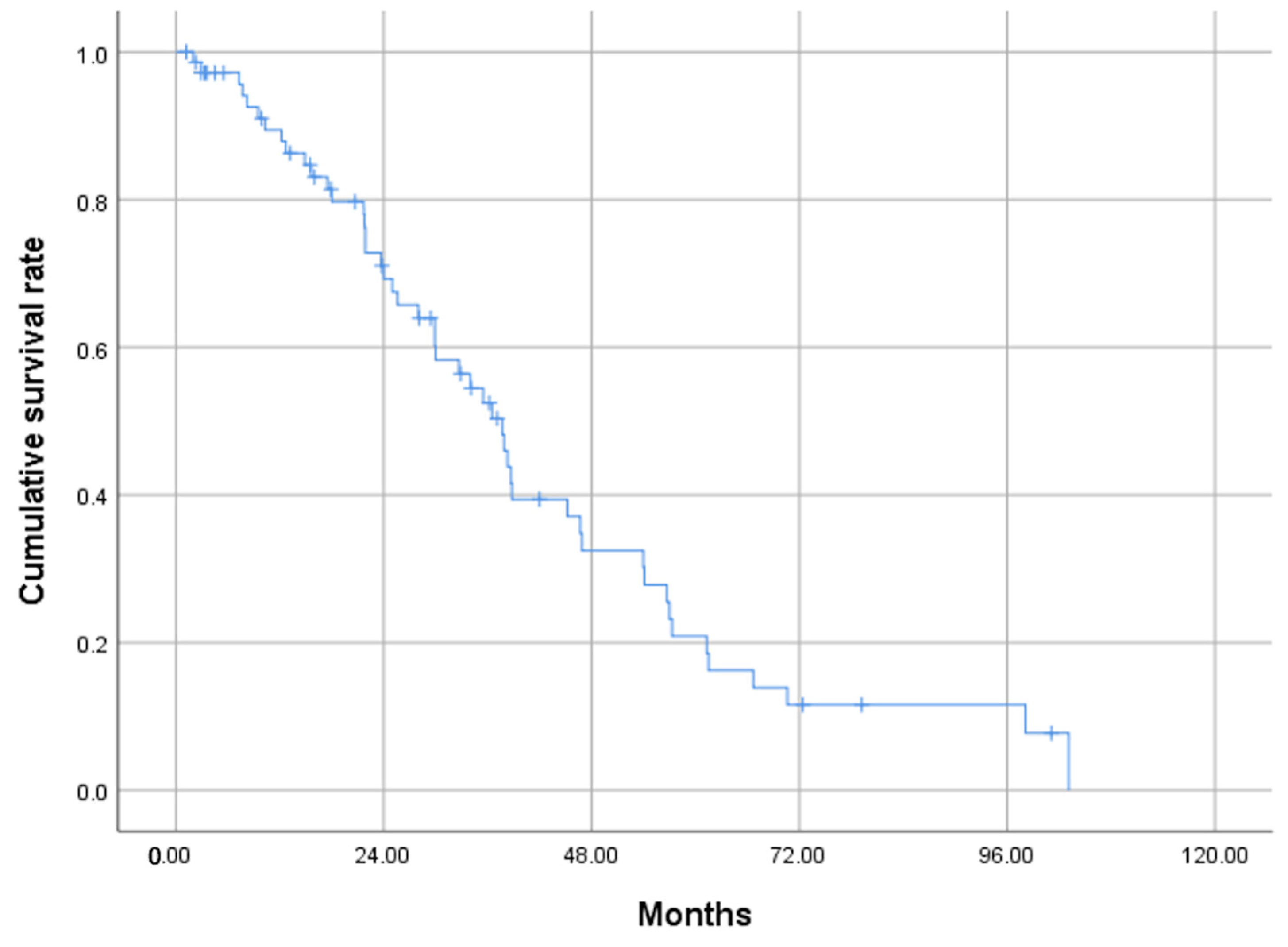
3.4. OS Rates
3.5. Univariate and Multivariate Analyses
3.6. Analyses of Additional Treatments after TACE
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Forner, A.; Reig, M.E.; de Lope, C.R.; Bruix, J. Current strategy for staging and treatment: The BCLC update and future prospects. Semin. Liver Dis. 2010, 30, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Han, K.H.; Ye, S.L.; Zhou, J.; Huang, Y.H.; Lin, S.M.; Wang, C.K.; Ikeda, M.; Chan, S.L.; Choo, S.P.; et al. A Changing Paradigm for the Treatment of Intermediate-Stage Hepatocellular Carcinoma: Asia-Pacific Primary Liver Cancer Expert Consensus Statements. Liver Cancer 2020, 9, 245–260. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Shim, J.H.; Lee, H.C.; Sung, K.B.; Ko, H.K.; Ko, G.Y.; Gwon, D.I.; Kim, J.W.; Lim, Y.S.; Park, S.H. New intermediate-stage subclassification for patients with hepatocellular carcinoma treated with transarterial chemoembolization. Liver Int. 2017, 37, 1861–1868. [Google Scholar] [CrossRef] [PubMed]
- Hung, Y.W.; Lee, I.C.; Chi, C.T.; Lee, R.C.; Liu, C.A.; Chiu, N.C.; Hwang, H.E.; Chao, Y.; Hou, M.C.; Huang, Y.H. Redefining Tumor Burden in Patients with Intermediate-Stage Hepatocellular Carcinoma: The Seven-Eleven Criteria. Liver Cancer 2021, 10, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Shimose, S.; Iwamoto, H.; Tanaka, M.; Niizeki, T.; Shirono, T.; Noda, Y.; Kamachi, N.; Okamura, S.; Nakano, M.; Suga, H.; et al. Alternating Lenvatinib and Trans-Arterial Therapy Prolongs Overall Survival in Patients with Inter-Mediate Stage HepatoCellular Carcinoma: A Propensity Score Matching Study. Cancers 2021, 13, 160. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, H.; Oikawa, T.; Ninomiya, M.; Fujita, M.; Abe, K.; Okumoto, K.; Katsumi, T.; Sato, W.; Igarashi, G.; Iino, C.; et al. Objective Response by mRECIST to Initial Lenvatinib Therapy Is an Independent Factor Contributing to Deep Response in Hepatocellular Carcinoma Treated with Lenvatinib-Transcatheter Arterial Chemoembolization Sequential Therapy. Liver Cancer 2022, 11, 383–396. [Google Scholar] [CrossRef]
- Kudo, M.; Ueshima, K.; Ikeda, M.; Torimura, T.; Tanabe, N.; Aikata, H.; Izumi, N.; Yamasaki, T.; Nojiri, S.; Hino, K.; et al. Randomised, multicentre prospective trial of transarterial chemoembolisation (TACE) plus sorafenib as compared with TACE alone in patients with hepatocellular carcinoma: TACTICS trial. Gut 2020, 69, 1492–1501. [Google Scholar] [CrossRef]
- Ando, Y.; Kawaoka, T.; Amioka, K.; Naruto, K.; Ogawa, Y.; Yoshikawa, Y.; Kikukawa, C.; Kosaka, Y.; Uchikawa, S.; Morio, K.; et al. Efficacy and Safety of Lenvatinib-Transcatheter Arterial Chemoembolization Sequential Therapy for Patients with Intermediate-Stage Hepatocellular Carcinoma. Oncology 2021, 99, 507–517. [Google Scholar] [CrossRef]
- Kim, B.K.; Kim, S.U.; Kim, K.A.; Chung, Y.E.; Kim, M.J.; Park, M.S.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Kim, M.D.; et al. Complete response at first chemoembolization is still the most robust predictor for favorable outcome in hepatocellular carcinoma. J. Hepatol. 2015, 62, 1304–1310. [Google Scholar] [CrossRef]
- Park, C.; Chu, H.H.; Kim, J.H.; Kim, S.Y.; Alrashidi, I.; Gwon, D.I.; Yoon, H.K.; Kim, N. Clinical Significance of the Initial and Best Responses after Chemoembolization in the Treatment of Intermediate-Stage Hepatocellular Carcinoma with Preserved Liver Function. J. Vasc. Interv. Radiol. 2020, 31, 1998–2006.e1991. [Google Scholar] [CrossRef]
- Saito, N.; Tanaka, T.; Nishiohuku, H.; Sato, T.; Masada, T.; Matsumoto, T.; Anai, H.; Sakaguchi, H.; Sueyoshi, S.; Marugami, N.; et al. Transarterial-chemoembolization remains an effective therapy for intermediate-stage hepatocellular carcinoma with preserved liver function. Hepatol. Res. 2020, 50, 1176–1185. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Ueshima, K.; Chan, S.; Minami, T.; Chishina, H.; Aoki, T.; Takita, M.; Hagiwara, S.; Minami, Y.; Ida, H.; et al. Lenvatinib as an Initial Treatment in Patients with Intermediate-Stage Hepatocellular Carcinoma Beyond Up-to-Seven Criteria and Child-Pugh A Liver Function: A Proof-of-Concept Study. Cancers 2019, 11, 1084. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.S.; Tang, B.; Yuan, J.; Lu, S.X.; Li, M.; Chen, R.X.; Zhang, L.; Ren, Z.G.; Yin, X. A new substage classification strategy for Barcelona Clinic Liver Cancer stage B patients with hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2019, 34, 1984–1991. [Google Scholar] [CrossRef] [PubMed]
- Famularo, S.; Di Sandro, S.; Giani, A.; Bernasconi, D.P.; Lauterio, A.; Ciulli, C.; Rampoldi, A.G.; Corso, R.; De Carlis, R.; Romano, F.; et al. Treatment of hepatocellular carcinoma beyond the Milan criteria. A weighted comparative study of surgical resection versus chemoembolization. HPB 2020, 22, 1349–1358. [Google Scholar] [CrossRef] [PubMed]
- Amioka, K.; Kawaoka, T.; Kinami, T.; Yamasaki, S.; Kosaka, M.; Johira, Y.; Yano, S.; Naruto, K.; Ando, Y.; Fujii, Y.; et al. Analysis of Lenvatinib’s Efficacy against Intermediate-Stage Unresectable Hepatocellular Carcinoma. Cancers 2022, 14, 5066. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Finn, R.S.; Galle, P.R.; Zhu, A.X.; Ducreux, M.; Cheng, A.L.; Ikeda, M.; Tsuchiya, K.; Aoki, K.; Jia, J.; et al. IMbrave150: Efficacy and Safety of Atezolizumab plus Bevacizumab versus Sorafenib in Patients with Barcelona Clinic Liver Cancer Stage B Unresectable Hepatocellular Carcinoma: An Exploratory Analysis of the Phase III Study. Liver Cancer 2022, 1–13. [Google Scholar] [CrossRef]
- Ueshima, K.; Ishikawa, T.; Saeki, I.; Morimoto, N.; Aikata, H.; Tanabe, N.; Inaba, Y.; Wada, Y.; Kondo, Y.; Tsuda, M.; et al. Transcatheter arterial chemoembolization therapy in combination strategy with lenvatinib in patients with unresectable hepatocellular carcinoma (TACTICS-L) in Japan: Final analysis. J. Clin. Oncol. 2022, 40, 417. [Google Scholar] [CrossRef]
- Reis, S.P.; Sutphin, P.D.; Singal, A.G.; Grzybowski, R.; Fisher, S.; Ball, C.; Xi, Y.; Grewal, S.; Kalva, S.P. Tumor Enhancement and Heterogeneity Are Associated with Treatment Response to Drug-Eluting Bead Chemoembolization for Hepatocellular Carcinoma. J. Comput. Assist. Tomogr. 2017, 41, 289–293. [Google Scholar] [CrossRef]
- Minamiguchi, K.; Nishiofuku, H.; Saito, N.; Sato, T.; Taiji, R.; Matsumoto, T.; Maeda, S.; Chanoki, Y.; Tachiiri, T.; Kunichika, H.; et al. Quantitative Analysis of Signal Heterogeneity in the Hepatobiliary Phase of Pretreatment Gadoxetic Acid-Enhanced MRI as a Prognostic Imaging Biomarker in Transarterial Chemoembolization for Intermediate-Stage Hepatocellular Carcinoma. Cancers 2023, 15, 1238. [Google Scholar] [CrossRef]
- Aoki, T.; Nishida, N.; Ueshima, K.; Morita, M.; Chishina, H.; Takita, M.; Hagiwara, S.; Ida, H.; Minami, Y.; Yamada, A.; et al. Higher Enhancement Intrahepatic Nodules on the Hepatobiliary Phase of Gd-EOB-DTPA-Enhanced MRI as a Poor Responsive Marker of Anti-PD-1/PD-L1 Monotherapy for Unresectable Hepatocellular Carcinoma. Liver Cancer 2021, 10, 615–628. [Google Scholar] [CrossRef]
- Hiraoka, A.; Kumada, T.; Kudo, M.; Hirooka, M.; Koizumi, Y.; Hiasa, Y.; Tajiri, K.; Toyoda, H.; Tada, T.; Ochi, H.; et al. Hepatic Function during Repeated TACE Procedures and Prognosis after Introducing Sorafenib in Patients with Unresectable Hepatocellular Carcinoma: Multicenter Analysis. Dig. Dis. 2017, 35, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Peck-Radosavljevic, M.; Raoul, J.-L.; Lee, H.C.; Kudo, M.; Nakajima, K.; Cheng, A.-L. OPTIMIS: An international observational study to assess the use of sorafenib after transarterial chemoembolization (TACE) in patients with hepatocellular carcinoma (HCC). J. Clin. Oncol. 2014, 32, TPS4155. [Google Scholar] [CrossRef]
- Miyayama, S.; Yamashiro, M.; Sugimori, N.; Ikeda, R.; Okimura, K.; Sakuragawa, N. Outcomes of Patients with Hepatocellular Carcinoma Treated with Conventional Transarterial Chemoembolization Using Guidance Software. J. Vasc. Interv. Radiol. 2019, 30, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Deschamps, F.; Solomon, S.B.; Thornton, R.H.; Rao, P.; Hakime, A.; Kuoch, V.; de Baere, T. Computed analysis of three-dimensional cone-beam computed tomography angiography for determination of tumor-feeding vessels during chemoembolization of liver tumor: A pilot study. Cardiovasc. Intervent. Radiol. 2010, 33, 1235–1242. [Google Scholar] [CrossRef]
| Characteristics | Value | % |
|---|---|---|
| Age | ||
| <75 years | 39 | 54.2 |
| ≥75 years | 33 | 45.8 |
| Gender | ||
| Male | 59 | 81.9 |
| Female | 13 | 18.1 |
| Virus | ||
| B, C | 46 | 63.9 |
| nonB nonC | 26 | 36.1 |
| Child-Pugh score | ||
| 5, 6 | 65 | 90.3 |
| 7 | 7 | 9.7 |
| mALBI grade | ||
| 1, 2a | 49 | 68.1 |
| 2b | 23 | 31.9 |
| AFP (ng/mL) | ||
| <200 | 59 | 81.9 |
| ≥200 | 13 | 18.1 |
| Tumor diameter(cm) | ||
| <6 | 51 | 70.8 |
| ≥6 | 21 | 29.2 |
| Tumor count | ||
| <7 | 47 | 65.2 |
| ≥7 | 25 | 34.8 |
| Up-to-11 criteria | ||
| in | 41 | 56.9 |
| out | 31 | 43.1 |
| MTA after refractory to TACE | ||
| No | 56 | 77.8 |
| Yes | 16 | 22.2 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Risk Factors | p | HR (95% CI) | p | HR (95% CI) |
| Age < 75 years | 0.564 | 0.758 (0.296–1.942) | ||
| Virus infection | 0.737 | 0.844 (0.315–2.265) | ||
| Child-Pugh score A | 0.423 | 0.497 (0.090–2.749) | ||
| mALBI grade 1, 2a | 0.097 | 0.412 (0.145–1.172) | 0.198 | 0.481 (0.158–1.466) |
| AFP < 200 ng/ml | 0.043 | 3.784 (1.041–13.755) | 0.121 | 3.022 (0.748–12.211) |
| Within up-to-11 criteria | 0.008 | 0.261 (0.097–0.701) | 0.042 | 0.341 (0.121–0.960) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, N.; Nishiofuku, H.; Sato, T.; Maeda, S.; Minamiguchi, K.; Taiji, R.; Matsumoto, T.; Chanoki, Y.; Tachiiri, T.; Kunichika, H.; et al. Predictive Factors of Complete Response to Transarterial Chemoembolization in Intermediate Stage Hepatocellular Carcinoma beyond Up-To-7 Criteria. Cancers 2023, 15, 2609. https://doi.org/10.3390/cancers15092609
Saito N, Nishiofuku H, Sato T, Maeda S, Minamiguchi K, Taiji R, Matsumoto T, Chanoki Y, Tachiiri T, Kunichika H, et al. Predictive Factors of Complete Response to Transarterial Chemoembolization in Intermediate Stage Hepatocellular Carcinoma beyond Up-To-7 Criteria. Cancers. 2023; 15(9):2609. https://doi.org/10.3390/cancers15092609
Chicago/Turabian StyleSaito, Natsuhiko, Hideyuki Nishiofuku, Takeshi Sato, Shinsaku Maeda, Kiyoyuki Minamiguchi, Ryosuke Taiji, Takeshi Matsumoto, Yuto Chanoki, Tetsuya Tachiiri, Hideki Kunichika, and et al. 2023. "Predictive Factors of Complete Response to Transarterial Chemoembolization in Intermediate Stage Hepatocellular Carcinoma beyond Up-To-7 Criteria" Cancers 15, no. 9: 2609. https://doi.org/10.3390/cancers15092609
APA StyleSaito, N., Nishiofuku, H., Sato, T., Maeda, S., Minamiguchi, K., Taiji, R., Matsumoto, T., Chanoki, Y., Tachiiri, T., Kunichika, H., Marugami, N., & Tanaka, T. (2023). Predictive Factors of Complete Response to Transarterial Chemoembolization in Intermediate Stage Hepatocellular Carcinoma beyond Up-To-7 Criteria. Cancers, 15(9), 2609. https://doi.org/10.3390/cancers15092609





