Rising Incidence of Non-Cardia Gastric Cancer among Young Women in the United States, 2000–2018: A Time-Trend Analysis Using the USCS Database
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Databases and Exclusion Criteria
2.2. Statistical Analysis
3. Results
3.1. Discovery Phase: SEER Database 2000–2018
3.1.1. Overall Rates and Trends
3.1.2. Sex-Specific Trends by Age Groups
3.2. External Validation Phase: SEER-Independent NPCR Database 2001–2018
3.2.1. Overall Rates and Trends
3.2.2. Sex-Specific Trends by Age Groups
3.3. Evaluation of Risk Factors among Young Adults
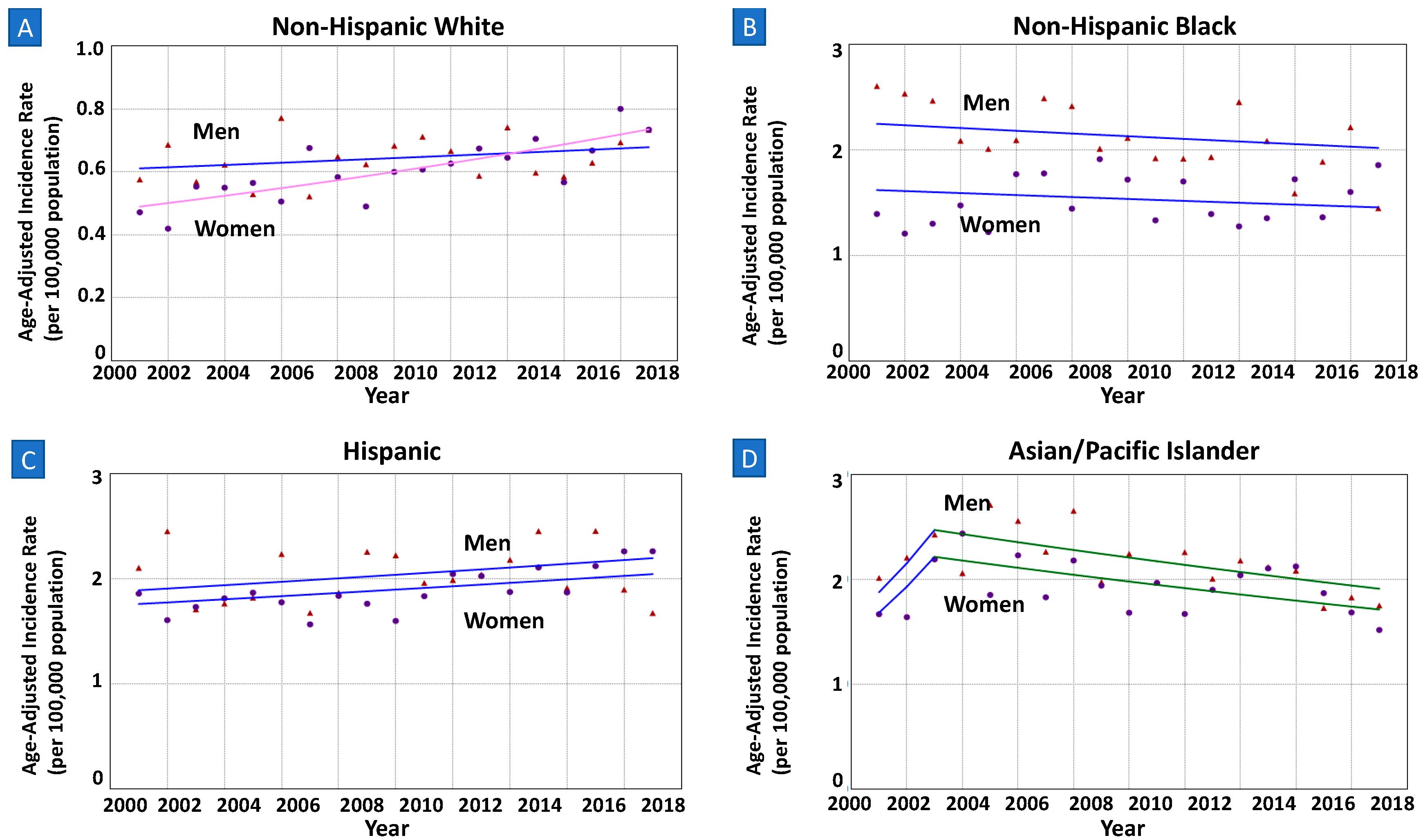
3.3.1. Sex-Specific Trends by Race/Ethnicity
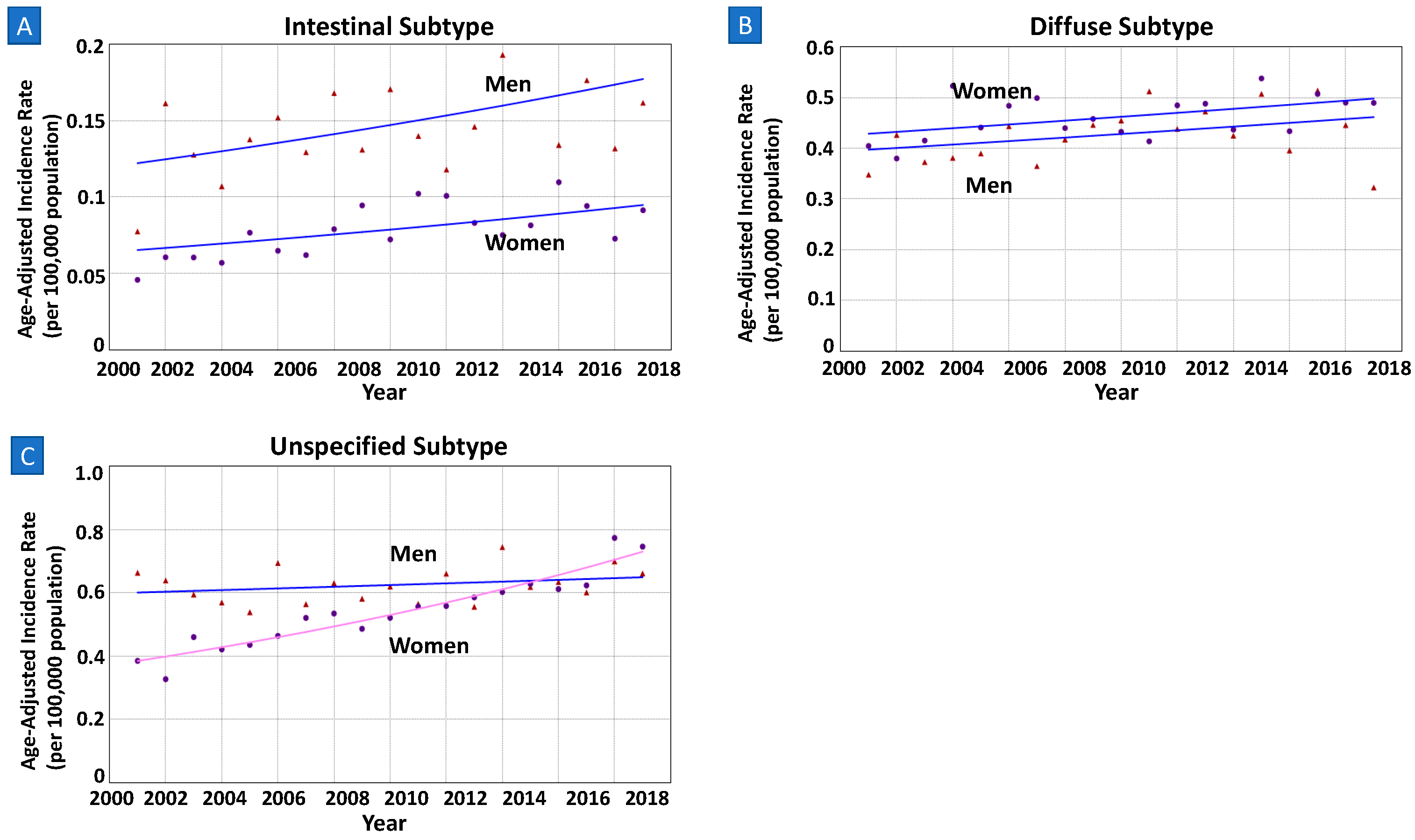
3.3.2. Sex-Specific Trends by Histopathology
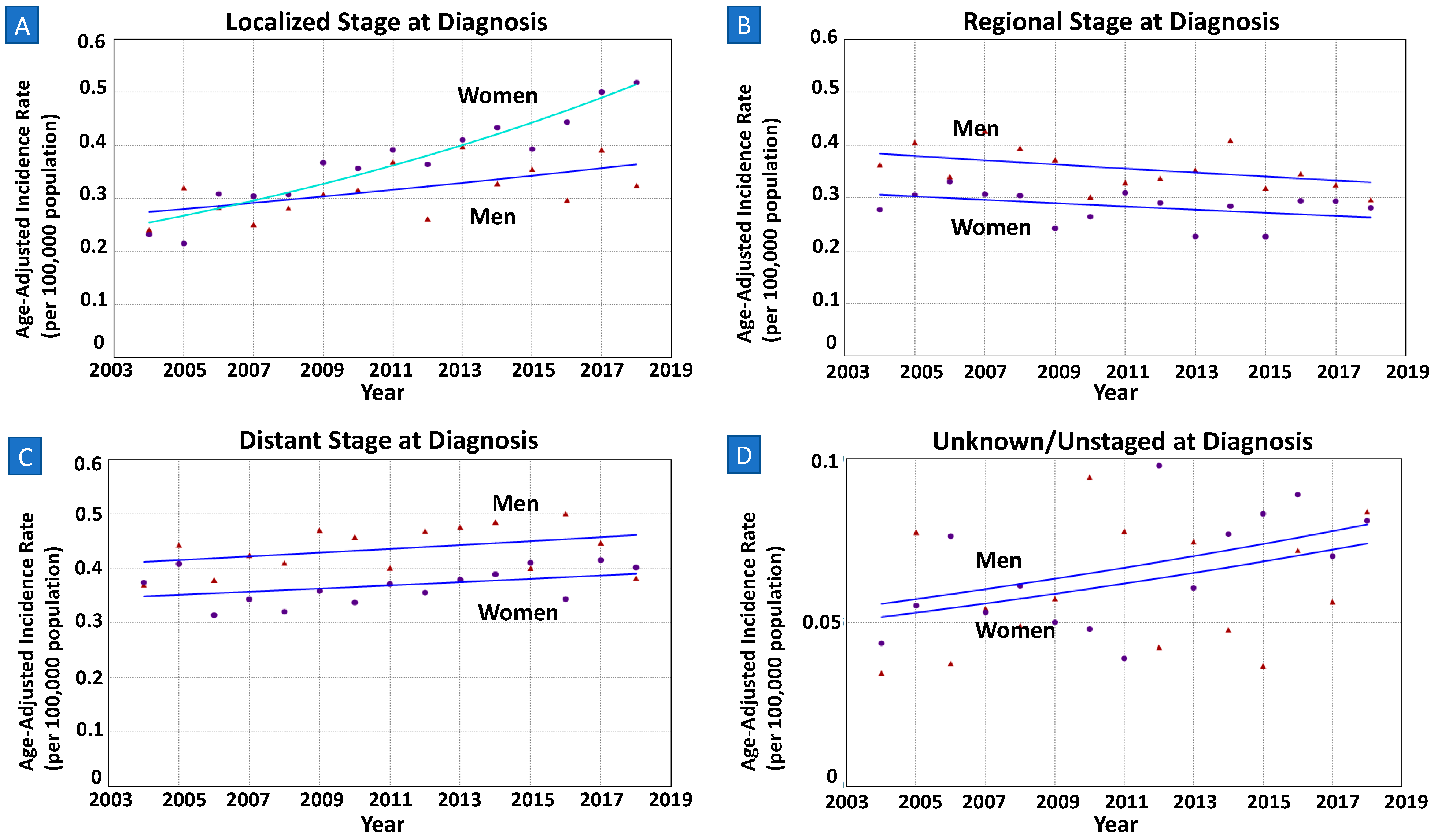
3.3.3. Sex-Specific Trends by Staging at Diagnosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| aIR | Age-adjusted incidence rates |
| aIRR | Age-adjusted incidence rate ratio |
| APC | Annual percentage change |
| AAPC | Average annual percentage change |
| AIG | Autoimmune gastritis |
| CDC | Centers of Disease Control and Prevention |
| NCI | National Cancer Institute |
| NCGC | Non-cardia gastric cancer |
| NPCR | National Program of Cancer Registries |
| PPI | Proton-pump inhibitor |
| SEER | Surveillance, Epidemiology, and End Results |
| USCS | United States Cancer Statistics |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Cancer of the Stomach-Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/stomach.html (accessed on 31 December 2022).
- Stomach (Gastric) Cancer Survival Rates. Available online: https://www.cancer.org/cancer/stomach-cancer/detection-diagnosis-staging/survival-rates.html (accessed on 31 December 2022).
- Rupp, S.K.; Stengel, A. Influencing Factors and Effects of Treatment on Quality of Life in Patients With Gastric Cancer-A Systematic Review. Front. Psychiatry 2021, 12, 656929. [Google Scholar] [CrossRef] [PubMed]
- Spagnuolo, R.; Corea, A.; Blumetti, M.; Giovinazzo, A.; Serafino, M.; Pagliuso, C.; Pagnotta, R.; Curto, G.; Cosco, C.; Cosco, V.; et al. Effects of listening to music in digestive endoscopy: A prospective intervention study led by nursing. J. Adv. Nurs. 2020, 76, 2993–3002. [Google Scholar] [CrossRef] [PubMed]
- Abraham, P.; Wang, L.; Jiang, Z.; Gricar, J.; Tan, H.; Kelly, R.J. Healthcare utilization and total costs of care among patients with advanced metastatic gastric and esophageal cancer. Future Oncol. 2021, 17, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; El Hajj, N.; Sittler, S.; Lammert, N.; Barnes, R.; Meloni-Ehrig, A. Gastric cancer: Classification, histology and application of molecular pathology. J. Gastrointest. Oncol. 2012, 3, 251–261. [Google Scholar]
- Anderson, W.F.; Rabkin, C.S.; Turner, N.; Fraumeni, J.F., Jr.; Rosenberg, P.S.; Camargo, M.C. The Changing Face of Noncardia Gastric Cancer Incidence Among US Non-Hispanic Whites. J. Natl. Cancer Inst. 2018, 110, 608–615. [Google Scholar] [CrossRef]
- National Program of Cancer Registries and Surveillance, 2020 Submission (2001–2018). Available online: https://www.cdc.gov/cancer/uscs/public-use/pdf/uscs-public-use-database-technical-documentation-us-2001-2018-508.pdf (accessed on 8 June 2022).
- List of SEER Registries. Available online: https://seer.cancer.gov/registries/list.html (accessed on 3 January 2023).
- Anderson, W.F.; Camargo, M.C.; Fraumeni, J.F., Jr.; Correa, P.; Rosenberg, P.S.; Rabkin, C.S. Age-specific trends in incidence of noncardia gastric cancer in US adults. JAMA 2010, 303, 1723–1728. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- Kim, H.J.; Fay, M.P.; Yu, B.; Barrett, M.J.; Feuer, E.J. Comparability of segmented line regression models. Biometrics 2004, 60, 1005–1014. [Google Scholar] [CrossRef]
- Feder, P.I. On Asymptotic Distribution Theory in Segmented Regression Problems—Identified Case. Ann. Statist. 1975, 3, 49–83. [Google Scholar] [CrossRef]
- Hofferkamp, J.; Havener, L.A. Standards for Cancer Registries: Data Standards and Data Dictionary, 12th ed.; North American Association of Central Cancer Registries: Springfield, IL, USA, 2007. [Google Scholar]
- Xu, J.; Lin, Y.; Yang, M.; Zhang, L. Statistics and pitfalls of trend analysis in cancer research: A review focused on statistical packages. J. Cancer 2020, 11, 2957–2961. [Google Scholar] [CrossRef] [PubMed]
- Merchant, S.J.; Kim, J.; Choi, A.H.; Sun, V.; Chao, J.; Nelson, R. A rising trend in the incidence of advanced gastric cancer in young Hispanic men. Gastric Cancer 2017, 20, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Tseng, J.; Miller, J.P.; Johnson, J.; Waters, K.; Gangi, A.; Gong, J.; Burch, M. Disparities and survival in newly diagnosed gastric cancer in Hispanic patients in the United States: A propensity score matched analysis. J. Gastrointest. Oncol. 2021, 12, 1308–1325. [Google Scholar] [CrossRef] [PubMed]
- Ishaq, S.; Nunn, L. Helicobacter pylori and gastric cancer: A state of the art review. Gastroenterol. Hepatol. Bed Bench 2015, 8 (Suppl. S1), S6–S14. [Google Scholar]
- Brown, H.; Cantrell, S.; Tang, H.; Epplein, M.; Garman, K.S. Racial Differences in Helicobacter pylori Prevalence in the US: A Systematic Review. Gastro Hep Adv. 2022, 1, 857–868. [Google Scholar] [CrossRef] [PubMed]
- Thrift, A.P.; Wenker, T.N.; El-Serag, H.B. Global burden of gastric cancer: Epidemiological trends, risk factors, screening and prevention. Nat. Rev. Clin. Oncol. 2023. [Google Scholar] [CrossRef]
- Smet, A.; Kupcinskas, J.; Link, A.; Hold, G.L.; Bornschein, J. The Role of Microbiota in Gastrointestinal Cancer and Cancer Treatment: Chance or Curse? Cell. Mol. Gastroenterol. Hepatol. 2022, 13, 857–874. [Google Scholar] [CrossRef]
- Yao, Q.; Qi, X.; Xie, S.-H. Sex difference in the incidence of cardia and non-cardia gastric cancer in the United States, 1992–2014. BMC Gastroenterol. 2020, 20, 418. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.E.; Shin, D.W.; Han, K.; Kim, D.; Jeong, S.M.; Koo, H.Y.; Yu, S.J.; Park, J.; Choi, K.S. Association of the Frequency and Quantity of Alcohol Consumption With Gastrointestinal Cancer. JAMA Netw. Open 2021, 4, e2120382. [Google Scholar] [CrossRef]
- Palli, D.; Galli, M.; Caporaso, N.E.; Cipriani, F.; Decarli, A.; Saieva, C.; Fraumeni, J.F., Jr.; Buiatti, E. Family history and risk of stomach cancer in Italy. Cancer Epidemiol. Biomark. Prev. 1994, 3, 15–18. [Google Scholar]
- Shin, C.M.; Kim, N.; Yang, H.J.; Cho, S.I.; Lee, H.S.; Kim, J.S.; Jung, H.C.; Song, I.S. Stomach cancer risk in gastric cancer relatives: Interaction between Helicobacter pylori infection and family history of gastric cancer for the risk of stomach cancer. J. Clin. Gastroenterol. 2010, 44, e34–e39. [Google Scholar] [CrossRef]
- Ratti, M.; Lampis, A.; Hahne, J.C.; Passalacqua, R.; Valeri, N. Microsatellite instability in gastric cancer: Molecular bases, clinical perspectives, and new treatment approaches. Cell. Mol. Life Sci. 2018, 75, 4151–4162. [Google Scholar] [CrossRef] [PubMed]
- Minalyan, A.; Benhammou, J.N.; Artashesyan, A.; Lewis, M.S.; Pisegna, J.R. Autoimmune atrophic gastritis: Current perspectives. Clin. Exp. Gastroenterol. 2017, 10, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Camargo, M.C.; Katki, H.A.; Weinstein, S.J.; Mannisto, S.; Albanes, D.; Surcel, H.M.; Rabkin, C.S. Association of Antiparietal Cell and Anti-Intrinsic Factor Antibodies with Risk of Gastric Cancer. JAMA Oncol. 2022, 8, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Torres-Bondia, F.; de Batlle, J.; Galvan, L.; Buti, M.; Barbe, F.; Pinol-Ripoll, G. Evolution of the consumption trend of proton pump inhibitors in the Lleida Health Region between 2002 and 2015. BMC Public Health 2022, 22, 818. [Google Scholar] [CrossRef] [PubMed]
- Midthune, D.N.; Fay, M.P.; Clegg, L.X.; Feuer, E.J. Modeling Reporting Delays and Reporting Corrections in Cancer Registry Data. J. Am. Stat. Assoc. 2005, 100, 61–70. [Google Scholar] [CrossRef]
- Kehm, R.D.; Yang, W.; Tehranifar, P.; Terry, M.B. 40 Years of Change in Age- and Stage-Specific Cancer Incidence Rates in US Women and Men. JNCI Cancer Spectr. 2019, 3, pkz038. [Google Scholar] [CrossRef]
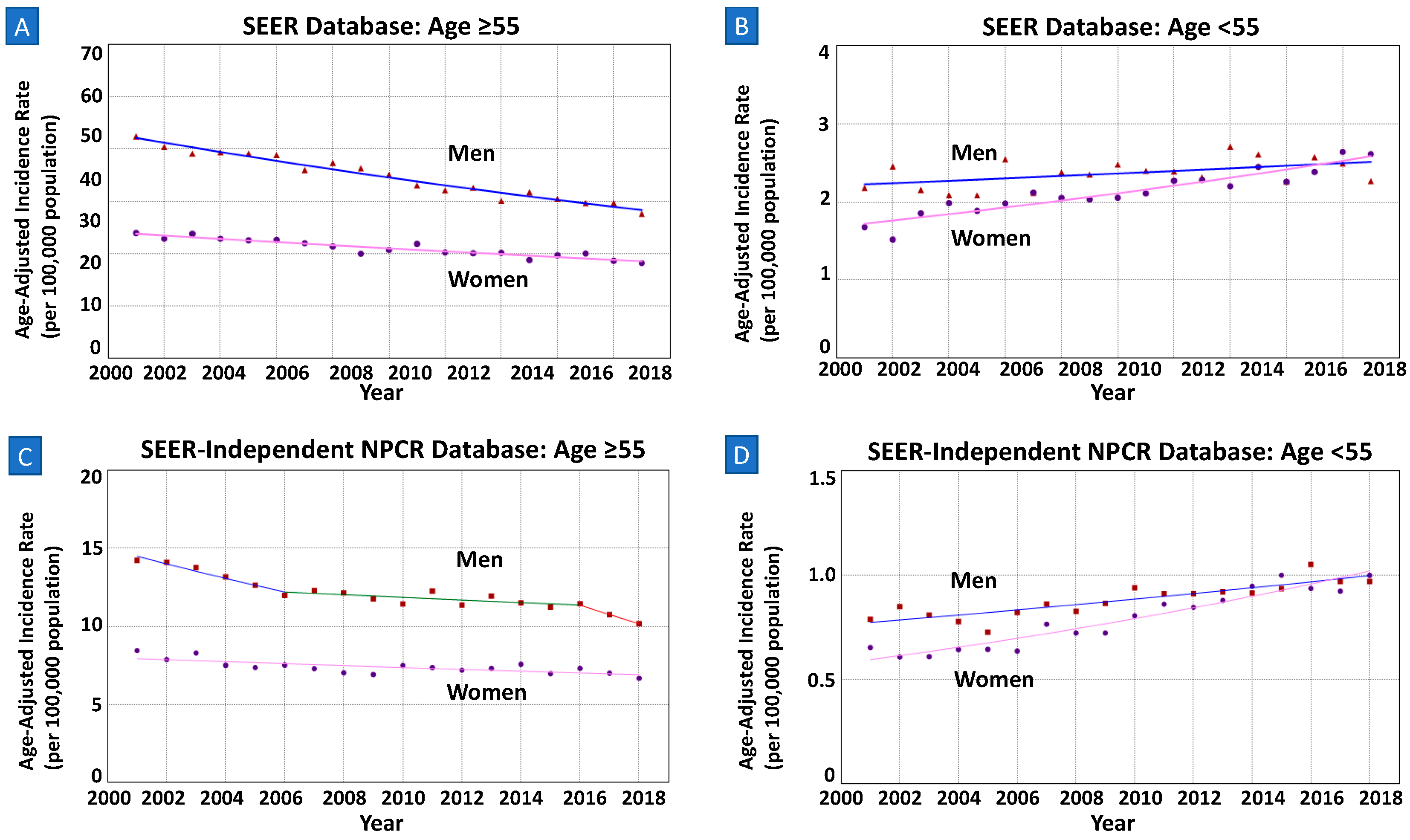
| SEER Database 2000–2018 (N = 79,068) | ||||
|---|---|---|---|---|
| Age | Overall | Women | Men | aIRR * |
| All Ages | 3.56 (3.54–3.59) | 2.91 (2.88–2.94) | 4.44 (4.39–4.48) | 0.66 |
| ≥55 | 13.59 (13.49–13.70) | 10.71 (10.59–10.84) | 17.54 (17.35–17.72) | 0.61 |
| <55 | 1.15 (1.13–1.16) | 1.09 (1.06–1.11) | 1.21 (1.18–1.24) | 0.90 |
| Age < 55 years (N = 13,791) | ||||
| Race/Ethnicity | Overall | Women | Men | aIRR * |
| Non-Hispanic White | 0.62 (0.60–0.64) | 0.60 (0.57–0.62) | 0.64 (0.61–0.67) | 0.94 |
| Non-Hispanic Black | 1.80 (1.73–1.87) | 1.52 (1.43–1.61) | 2.11 (2.00–2.23) | 0.72 |
| Hispanic | 1.97 (1.91–2.03) | 1.90 (1.82–1.99) | 2.04 (1.95–2.13) | 0.93 |
| Asian/Pacific Islander | 2.02 (1.94–2.11) | 1.91 (1.81–2.03) | 2.15 (2.02–2.27) | 0.89 |
| Other | 1.59 (1.33–1.89) | 1.40 (1.06–1.81) | 1.80 (1.41–2.26) | 0.78 |
| Histopathology | ||||
| Intestinal Subtype a | 0.11 (0.11–0.12) | 0.08 (0.07–0.09) | 0.15 (0.14–0.16) | 0.53 |
| Diffuse Subtype b | 0.44 (0.43–0.45) | 0.46 (0.44–0.48) | 0.43 (0.41–0.44) | 1.07 |
| Other/Unspecified c | 0.58 (0.57–0.59) | 0.54 (0.52–0.56) | 0.62 (0.60–0.64) | 0.87 |
| Stage at Diagnosis (2004–2018) | ||||
| Localized | 0.34 (0.33–0.35) | 0.37 (0.35–0.39) | 0.31 (0.30–0.33) | 1.19 |
| Regional | 0.32 (0.31–0.33) | 0.28 (0.27–0.30) | 0.35 (0.34–0.37) | 0.80 |
| Distant | 0.40 (0.39–0.41) | 0.37 (0.35–0.39) | 0.43 (0.42–0.45) | 0.86 |
| Unstaged/Unknown | 0.06 (0.06–0.07) | 0.07 (0.06–0.07) | 0.06 (0.05–0.07) | 1.17 |
| SEER-Independent NPCR Database 2001–2018 (N = 90,760) | ||||
| Age Groups | Overall | Women | Men | aIRR * |
| All Ages | 2.47 (2.46–2.49) | 2.03 (2.01–2.05) | 3.06 (3.03–3.09) | 0.66 |
| ≥55 | 9.45 (9.27–9.40) | 7.37 (7.29–7.45) | 11.97 (11.85–12.08) | 0.62 |
| <55 | 0.83 (0.82–0.85) | 0.79 (0.77–0.81) | 0.88 (0.86–0.90) | 0.90 |
| (A) | |||||||
| Trends | Pairwise Comparison | ||||||
| Sex | Cases n (% of Age Group) | Years | APC (95%CI) | AAPC a (95%CI) | AAPC p-Value b | Test of Coincidence p-Value c | Test of Parallelism p-Value d |
| All Ages (N = 79,068) | |||||||
| Men | 42,965 (54.3%) | 2000–2018 | −1.73% (−1.94–−1.51) | −1.73% (−1.94–−1.51) | <0.001 | <0.001 | <0.001 |
| Women | 36,103 (45.7%) | 2000–2018 | −0.60% (−0.80–−0.40) | −0.60% (−0.80–−0.40) | <0.001 | ||
| Age ≥ 55 (N = 65,258) | |||||||
| Men | 35,747 (54.8%) | 2000–2018 | −2.16% (−2.38–−1.95) | −2.16% (−2.38–−1.95) | <0.001 | <0.001 | <0.001 |
| Women | 29,511 (45.2%) | 2000–2018 | −1.37% (−1.61–−1.12) | −1.37% (−1.61–−1.12) | <0.001 | ||
| Age < 55 (N = 13,791) | |||||||
| Men | 7212 (52.3%) | 2000–2018 | 0.68% (0.06–1.30) | 0.68% (0.06–1.30) | 0.033 | <0.001 | 0.015 |
| Women | 6579 (47.7%) | 2000–2018 | 2.28% (1.82–2.74) | 2.28% (1.82–2.74) | <0.001 | ||
| (B) | |||||||
| Trends | Pairwise Comparison | ||||||
| Sex | Cases n (% of Age Group) | Years | APC (95%CI) | AAPC a (95%CI) | AAPC p-Value b | Test of Coincidence p-Value c | Test of Parallelism p-Value d |
| All Ages (N = 90,760) | |||||||
| Men | 49,740 (54.8%) | 2001–2006 | −2.92% (−4.42–−1.39) | −1.55% (−2.37–−0.73) | <0.001 | <0.001 | <0.001 |
| 2006–2016 | −0.23% (−0.83–0.37) | ||||||
| 2016–2018 | −4.61% (−10.50–1.66) | ||||||
| Women | 41,020 (45.2%) | 2001–2005 | −2.36% (−5.55–0.94) | −0.19% (−0.98–−0.61) | 0.65 | ||
| 2005–2018 | 0.49% (−0.04–1.02) | ||||||
| Age ≥ 55 (N = 75,241) | |||||||
| Men | 41,585 (55.3%) | 2001–2006 | −3.39% (−5.11–1.63) | −2.06% (−3.01–−1.11) | <0.001 | <0.001 | 0.009 |
| 2006–2016 | −0.72% (−1.41–−0.02) | ||||||
| 2016–2018 | −5.39% (−12.12–1.87) | ||||||
| Women | 33,656 (44.7%) | 2001–2018 | −0.82% (−1.22–−0.43) | −0.82% (−1.22–−0.43) | <0.001 | ||
| Age < 55 (N = 15,486) | |||||||
| Men | 8144 (52.6%) | 2001–2018 | 1.51% (1.04–1.98) | 1.51% (1.04–1.98) | <0.001 | <0.001 | <0.001 |
| Women | 7342 (47.4%) | 2001–2018 | 3.22% (2.69–3.77) | 3.22% (2.69–3.77) | <0.001 | ||
| Trends | Pairwise Comparison | |||||||
|---|---|---|---|---|---|---|---|---|
| Subgroup | Sex | Cases n (% of Age Group) | Years | APC (95%CI) | AAPC a (95%CI) | AAPC p-Value b | Test of Coincidence p-Value c | Test of Parallelism p-Value d |
| Race | ||||||||
| Non-Hispanic White | Male | 2375 (17.2%) | 2000–2018 | 0.58% (−0.42–1.59) | 0.58% (−0.42–1.59) | 0.082 | <0.001 | 0.042 |
| Female | 2169 (15.7%) | 2000–2018 | 2.28% (1.38–3.19) | 2.28% (1.38–3.19) | 0.005 | |||
| Non-Hispanic Black | Male | 1395 (10.1%) | 2000–2018 | −0.59% (−1.49–0.31) | −0.59% (−1.49–0.31) | 0.19 | <0.001 | 0.062 |
| Female | 1129 (8.2%) | 2000–2018 | ||||||
| Hispanic | Male | 2172 (15.7%) | 2000–2018 | 0.84% (0.14–1.53) | 0.84% (0.14–1.53) | 0.020 | <0.001 | 0.17 |
| Female | 2027 (14.7%) | 2000–2018 | ||||||
| Asian/Pacific Islander | Male | 1170 (8.5%) | 2000–2002 | 14.73% (−10.72–47.42) | 0.10% (−2.63–2.91) | 0.94 | <0.001 | 0.32 |
| 2002–2018 | −1.59% (−2.39–−0.79) | |||||||
| Female | 1173 (8.5%) | 2000–2002 | 14.73% (−10.72–47.42) | <0.001 | 0.32 | |||
| 2002–2018 | −1.59% (−2.39–−0.79) | |||||||
| Other/Unspecified | Male | 72 (0.01%) | 2000–2018 | Could not analyze | <0.001 | - | ||
| Female | 57 (0.004%) | 2000–2018 | Could not analyze | |||||
| Histology | ||||||||
| Intestinal e | Male | 886 (6.4%) | 2000–2018 | 2.09% (0.95–3.24) | 2.09% (0.95–3.24) | 0.001 | <0.001 | 0.29 |
| Female | 478 (3.5%) | 2000–2018 | ||||||
| Diffuse f | Male | 2514 (18.2%) | 2000–2018 | 0.84% (0.20–1.47) | 0.84% (0.20–1.47) | 0.011 | 0.11 | 0.83 |
| Female | 2766 (20.1%) | 2000–2018 | ||||||
| Other/Unspecified g | Male | 3736 (27.1%) | 2000–2018 | 0.43% (−0.4–1.21) | 0.43% (−0.4–1.21) | 0.26 | <0.001 | <0.001 |
| Female | 3274 (23.7%) | 2000–2018 | 3.62% (2.99–4.26) | 3.62% (2.99–4.26) | <0.001 | |||
| Stage at Diagnosis | ||||||||
| Localized | Male | 1503 (10.9%) | 2004–2018 | 2.04% (0.33–3.78) | 2.04% (0.33–3.78) | 0.023 | 0.004 | 0.025 |
| Female | 1780 (12.9%) | 2004–2018 | 5.17% (4.04–6.31) | 5.17% (4.04–6.31) | <0.001 | |||
| Regional | Male | 1692 (12.3%) | 2004–2018 | −1.08% (−1.94–−0.20) | −1.08% (−1.94–−0.20) | 0.018 | <0.001 | 0.47 |
| Female | 1352 (9.8%) | 2004–2018 | ||||||
| Distant | Male | 2050 (14.9%) | 2004–2018 | 0.81% (0.04–1.58) | 0.81% (0.04–1.58) | 0.039 | 0.001 | 0.94 |
| Female | 1756 (12.7%) | 2004–2018 | ||||||
| Unknown/Unstaged | Male | 288 (2.1%) | 2004–2018 | 2.61% (0.20–5.08) | 2.61% (0.20–5.08) | 0.035 | 0.58 | 0.36 |
| Female | 317 (2.3%) | 2004–2018 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, J.; Abboud, Y.; Burch, M.; Gong, J.; Waters, K.; Ghaith, J.; Jiang, Y.; Park, K.; Liu, Q.; Watson, R.; et al. Rising Incidence of Non-Cardia Gastric Cancer among Young Women in the United States, 2000–2018: A Time-Trend Analysis Using the USCS Database. Cancers 2023, 15, 2283. https://doi.org/10.3390/cancers15082283
Oh J, Abboud Y, Burch M, Gong J, Waters K, Ghaith J, Jiang Y, Park K, Liu Q, Watson R, et al. Rising Incidence of Non-Cardia Gastric Cancer among Young Women in the United States, 2000–2018: A Time-Trend Analysis Using the USCS Database. Cancers. 2023; 15(8):2283. https://doi.org/10.3390/cancers15082283
Chicago/Turabian StyleOh, Janice, Yazan Abboud, Miguel Burch, Jun Gong, Kevin Waters, Jenan Ghaith, Yi Jiang, Kenneth Park, Quin Liu, Rabindra Watson, and et al. 2023. "Rising Incidence of Non-Cardia Gastric Cancer among Young Women in the United States, 2000–2018: A Time-Trend Analysis Using the USCS Database" Cancers 15, no. 8: 2283. https://doi.org/10.3390/cancers15082283
APA StyleOh, J., Abboud, Y., Burch, M., Gong, J., Waters, K., Ghaith, J., Jiang, Y., Park, K., Liu, Q., Watson, R., Lo, S. K., & Gaddam, S. (2023). Rising Incidence of Non-Cardia Gastric Cancer among Young Women in the United States, 2000–2018: A Time-Trend Analysis Using the USCS Database. Cancers, 15(8), 2283. https://doi.org/10.3390/cancers15082283








