Multimodal Prehabilitation in Patients Undergoing Complex Colorectal Surgery, Liver Resection, and Hyperthermic Intraperitoneal Chemotherapy (HIPEC): A Pilot Study on Feasibility and Potential Efficacy
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
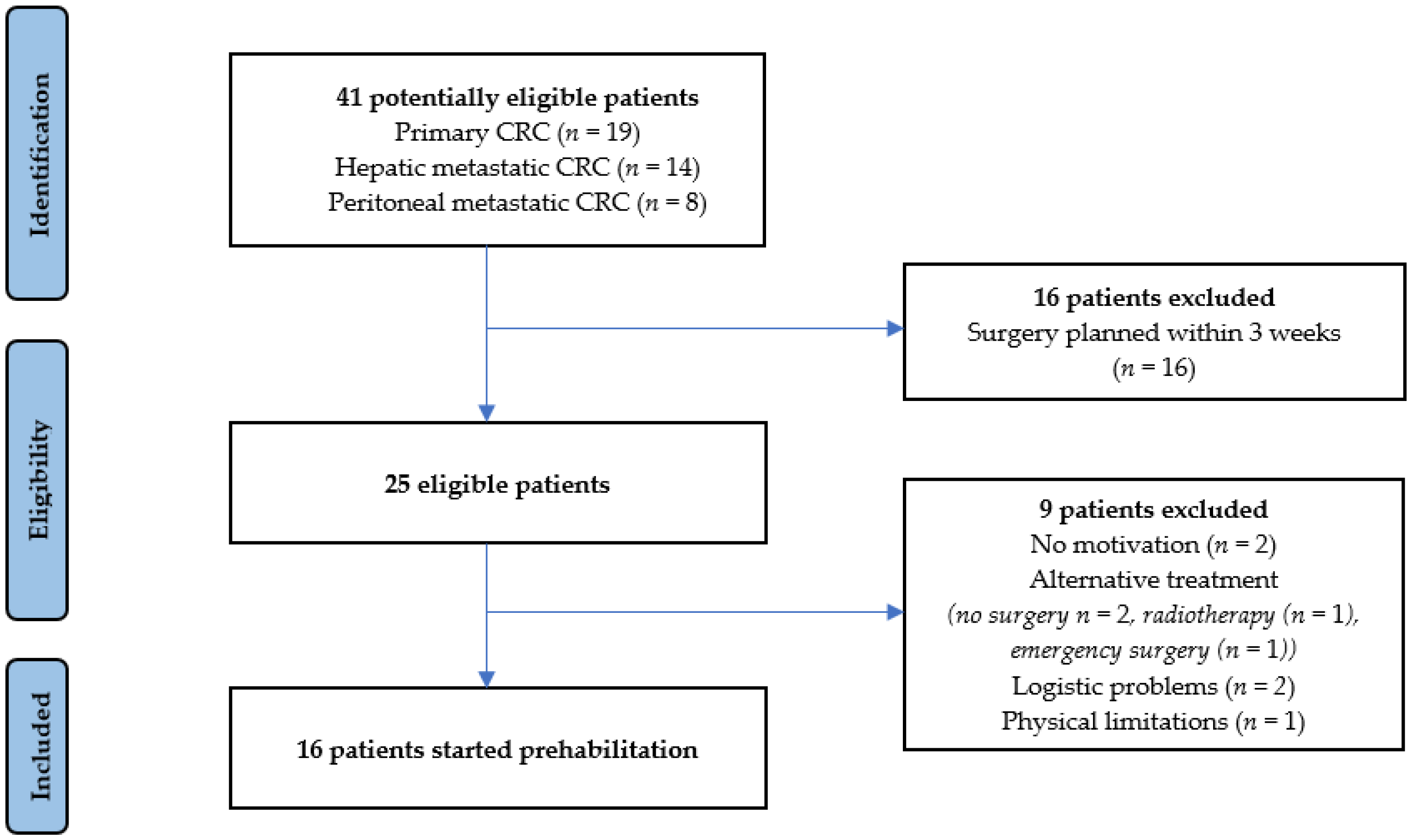
2.2. Participants
2.3. Intervention
2.4. Perioperative Care
2.5. Primary Outcome Measure
- (1)
- Accrual rate: defined as the percentage of eligible patients who participated in the prehabilitation program. Reasons for non-participation were recorded.
- (2)
- Completion rate: defined as the percentage of patients who continued the prehabilitation program until surgery. Reasons for not continuing were recorded.
- (3)
- Adherence to the program: defined as the percentage of patients who continued prehabilitation until surgery and who completed at least 80% of the prescribed supervised trainings. Prescribed supervised trainings is calculated as the number of maximal trainings that could be performed in proportion to the duration of the preoperative period.
- (4)
- Satisfaction: assessed by a self-developed, specific questionnaire on patients’ satisfaction with the prehabilitation program.
- (5)
- Safety: defined as the number of adverse events occurring during the prehabilitation program.
2.6. Secondary Outcome Measure
2.7. Statistical Analysis
3. Results
3.1. Feasibility Outcomes
3.2. Exercise Program
3.3. Nutritional Intervention Program
3.4. Psychological Support and Smoke Cessation Program
3.5. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix A.1. Exercise Program
Appendix A.1.1. Endurance Training
- -
- This supervised high-intensity interval training (HIIT) training (by either a hospital-based or first-line physiotherapist) will be performed three times a week.
- -
- The duration of the HIIT training is 28 min and the training is performed with four intervals of moderate intensity (3 min) and four intervals of high intensity (4 min).
- -
- The workload is dosed at a percentage of estimated VO2peak (baseline measurements). High intensity is considered as 90% of estimated VO2peak.
- -
- This HIIT training aims to reach levels of Borg 15–17 and >85% of the age predicted maximum heart rate, as long as the patient could perform the exercise.
- -
- Exercise may be performed on a bicycle, a rower, a treadmill, and/or on other aerobic exercise machines.
Appendix A.1.2. Resistance Training
- -
- This supervised training (by either a hospital-based or first-line physiotherapist) will be performed three times a week.
- -
- Strength training will be the same concept for all patients irrespective of estimated VO2peak.
- -
- The strength exercises are performed according to: 2 s of concentric strength and 2 s of eccentric strength.
- -
- The strength training consists of two series of ten repetitions of six exercises: leg press, chest press, abdominal crunch, lat pull down, low row, and step up.
- *
- In week 1 using 65% of calculated indirect 1RM (baseline measurements).
- *
- In week 2 using 70% of calculated indirect 1RM (baseline measurements).
- *
- In week 3 using 75% of calculated indirect 1RM (baseline measurements).
- *
- In week 4 using 80% of calculated indirect 1RM (baseline measurements).
- -
- The last series with 10 repetitions needs to be attainable. If this is not the case, the dosing will be 5–10% lower in the next session.
- -
- If in the last series it appears that exercises are too low (≥15 repetitions will be achieved), the dosing will be 5–10% higher in the next session.
Appendix A.1.3. Homework/Counselling
- -
- The homework will be performed during the days without supervised training.
- -
- Patients are instructed to aim for 60 min walking and/or cycling a day. If possible, patients can do more than 60 min of walking or cycling every day.
- -
- In case of lower exercise capacity, it is advised to walk/cycle 2–3 times a day for periods of 20 min.
- -
- Additionally, an electric bicycle, a stationary bicycle and/or a walking aid (walker) may be necessary.
- -
- Instructions on breathing techniques will be given by the physiotherapist to reduce the risk of developing pneumonia postoperatively.
Appendix A.1.4. Rest
- -
- Patients are instructed to take care of recovery and adequate rest and sleep.
- -
- From 3 days before surgery, no high-intensity interval training and strength training are performed.The patient will continue the homework/counselling (walking/cycling every day) and the dietary supplements until surgery.
Appendix A.2. Nutritional Intervention
Appendix A.2.1. Dietary Advice
- -
- Aiming for optimal energy intake based on screening and assessment.
- -
- Aiming for a total protein intake of 1.5–1.8 g/kg per day, with a minimum protein intake of 25–30 g per meal.
Appendix A.2.2. Protein Supplementation
- -
- A total of 30 g protein supplementation (provided by FrieslandCampina) before going to sleep.
- -
- An additional 30 g protein supplementation (provided by FrieslandCampina) immediately following supervised training (within 1 h).
Appendix A.2.3. Vitamin Supplementation
- -
- Vitamin D
- *
- Patients < 70 years old: 10 µg vitamin D daily.
- *
- Patients ≥ 70 years old: 20 µg vitamin D daily.
- -
- Multivitamin: 50% of the recommended daily allowance supplementation.
Appendix A.3. Psychological Support
Appendix A.4. Smoking Cessation Support
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- van der Geest, L.G.M.; Lam-Boer, J.T.; Koopman, M.; Verhoef, C.; Elferink, M.A.; de Wilt, J.H. Nationwide trends in incidence, treatment and survival of colorectal cancer patients with synchronous metastases. Clin. Exp. Metastasis 2015, 32, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Höppener, D.J.; Nierop, P.M.H.; Van Amerongen, M.J.; Olthof, P.B.; Galjart, B.; Van Gulik, T.M.; De Wilt, J.H.W.; Grünhagen, D.J.; Rahbari, N.N.; Verhoef, C. The Disease-Free Interval Between Resection of Primary Colorectal Malignancy and the Detection of Hepatic Metastases Predicts Disease Recurrence But Not Overall Survival. Ann. Surg. Oncol. 2019, 26, 2812–2820. [Google Scholar] [CrossRef] [PubMed]
- Kuijpers, A.M.J.; Mirck, B.; Aalbers, A.G.J.; Nienhuijs, S.W.; de Hingh, I.H.J.T.; Wiezer, M.J.; van Ramshorst, B.; van Ginkel, R.J.; Havenga, K.; Bremers, A.J.; et al. Cytoreduction and HIPEC in The Netherlands: Nationwide Long-term Outcome Following the Dutch Protocol. Ann. Surg. Oncol. 2013, 20, 4224–4230. [Google Scholar] [CrossRef] [PubMed]
- Couwenberg, A.M.; de Beer, F.S.; Intven, M.P.; Burbach, J.P.; Smits, A.B.; Consten, E.C.; Schiphorst, A.H.; Wijffels, N.A.; de Roos, M.A.; Hamaker, M.E.; et al. The impact of postoperative complications on health-related quality of life in older patients with rectal cancer; a prospective cohort study. J. Geriatr. Oncol. 2018, 9, 102–109. [Google Scholar] [CrossRef]
- van Kooten, R.T.; Akker, E.V.D.; Putter, H.; Kranenbarg, E.M.-K.; van de Velde, C.; Wouters, M.; Tollenaar, R.; Peeters, K. The Impact of Postoperative Complications on Short- and Long-Term Health-Related Quality of Life After Total Mesorectal Excision for Rectal Cancer. Clin. Color. Cancer 2022, 21, 325–338. [Google Scholar] [CrossRef]
- Govaert, J.; Fiocco, M.; van Dijk, W.; Scheffer, A.; de Graaf, E.; Tollenaar, R.; Wouters, M.; Lamme, B.; Hess, D.; Belgers, H.; et al. Costs of complications after colorectal cancer surgery in the Netherlands: Building the business case for hospitals. Eur. J. Surg. Oncol. 2015, 41, 1059–1067. [Google Scholar] [CrossRef] [PubMed]
- Elekonawo, F.M.; Van Der Meeren, M.M.; Simkens, G.A.; De Wilt, J.H.; De Hingh, I.H.; Bremers, A.J. Comparison of 2 Perioperative Management Protocols and Their Influence on Postoperative Recovery after Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy: Standard Parenteral Nutrition, Selective Bowel Decontamination and Suprapubic Catheters? Dig. Surg. 2018, 36, 394–401. [Google Scholar]
- Barberan-Garcia, A.; Ubré, M.; Roca, J.; Lacy, A.M.; Burgos, F.; Risco, R.; Momblán, D.; Balust, J.; Blanco, I.; Martínez-Pallí, G. Personalised Prehabilitation in High-risk Patients Undergoing Elective Major Abdominal Surgery: A Randomized Blinded Controlled Trial. Ann. Surg. 2018, 267, 50–56. [Google Scholar] [CrossRef]
- Berkel, A.E.M.; Bongers, B.C.; Kotte, H.; Weltevreden, P.; de Jongh, F.H.C.; Eijsvogel, M.M.M.; Wymenga, M.; Bigirwamungu-Bargeman, M.; van der Palen, J.; van Det, M.J.; et al. Effects of Community-based Exercise Prehabilitation for Patients Scheduled for Colorectal Surgery With High Risk for Postoperative Complications: Results of a Randomized Clinical Trial. Ann. Surg. 2021, 275, e299–e306. [Google Scholar] [CrossRef]
- de Klerk, M.; van Dalen, D.; Venrooij, L.N.-V.; Meijerink, W.; Verdaasdonk, E. A multimodal prehabilitation program in high-risk patients undergoing elective resection for colorectal cancer: A retrospective cohort study. Eur. J. Surg. Oncol. 2021, 47, 2849–2856. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Carli, F.; Lee, L.; Charlebois, P.; Stein, B.; Liberman, A.S.; Kaneva, P.; Augustin, B.; Wongyingsinn, M.; Gamsa, A.; et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: A pilot study. Surg. Endosc. 2012, 27, 1072–1082. [Google Scholar] [CrossRef] [PubMed]
- van Rooijen, S.; Carli, F.; Dalton, S.O.; Johansen, C.; Dieleman, J.; Roumen, R.; Slooter, G. Preoperative modifiable risk factors in colorectal surgery: An observational cohort study identifying the possible value of prehabilitation. Acta Oncol. 2017, 56, 329–334. [Google Scholar] [CrossRef] [PubMed]
- van Kooten, R.T.; Bahadoer, R.R.; Peeters, K.C.; Hoeksema, J.H.; Steyerberg, E.W.; Hartgrink, H.H.; van de Velde, C.J.; Wouters, M.W.; Tollenaar, R.A. Preoperative risk factors for major postoperative complications after complex gastrointestinal cancer surgery: A systematic review. Eur. J. Surg. Oncol. 2021, 47, 3049–3058. [Google Scholar] [CrossRef] [PubMed]
- Strijker, D.; Meijerink, W.; Bremers, A.; de Reuver, P.; van Laarhoven, C.; Heuvel, B.V.D. Prehabilitation to improve postoperative outcomes in patients with peritoneal carcinomatosis undergoing hyperthermic intraperitoneal chemotherapy (HIPEC): A scoping review. Eur. J. Surg. Oncol. 2021, 48, 657–665. [Google Scholar] [CrossRef]
- Browne, R.H. On the use of a pilot sample for sample size determination. Stat. Med. 1995, 14, 1933–1940. [Google Scholar] [CrossRef]
- Waterland, J.L.; McCourt, O.; Edbrooke, L.; Granger, C.L.; Ismail, H.; Riedel, B.; Denehy, L. Efficacy of Prehabilitation Including Exercise on Postoperative Outcomes Following Abdominal Cancer Surgery: A Systematic Review and Meta-Analysis. Front. Surg. 2021, 8, 628848. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.; Tahir, M.R.; Bongers, B.C.; Kallen, V.L.; Slooter, G.D.; van Meeteren, N.L. Prehabilitation before major intra-abdominal cancer surgery: A systematic review of randomised controlled trials. Eur. J. Anaesthesiol. 2019, 36, 933–945. [Google Scholar] [CrossRef]
- van Rooijen, S.J.; Molenaar, C.J.; Schep, G.; van Lieshout, R.H.; Beijer, S.; Dubbers, R.; Rademakers, N.; Papen-Botterhuis, N.E.; van Kempen, S.; Carli, F.; et al. Making Patients Fit for Surgery: Introducing a Four Pillar Multimodal Prehabilitation Program in Colorectal Cancer. Am. J. Phys. Med. Rehabil. 2019, 98, 888–896. [Google Scholar] [CrossRef]
- De Backer, I.C.; Schep, G.; Hoogeveen, A.; Vreugdenhil, G.; Kester, A.D.; van Breda, E. Exercise Testing and Training in a Cancer Rehabilitation Program: The Advantage of the Steep Ramp Test. Arch. Phys. Med. Rehabil. 2007, 88, 610–616. [Google Scholar] [CrossRef]
- Levinger, I.; Goodman, C.; Hare, D.L.; Jerums, G.; Toia, D.; Selig, S. The reliability of the 1RM strength test for untrained middle-aged individuals. J. Sci. Med. Sport 2009, 12, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Health Council of the Netherlands. Evaluation of the Dietary Reference Values for Vitamin D; Health Council of the Netherlands: The Hague, The Netherlands, 2012. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H.; Wilmore, D.W. Evidence-Based Surgical Care and the Evolution of Fast-Track Surgery. Ann. Surg. 2008, 248, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Mazzotta, A.D.; Kawaguchi, Y.; Pantel, L.; Tribillon, E.; Bonnet, S.; Gayet, B.; Soubrane, O. Conditional cumulative incidence of postoperative complications stratified by complexity classification for laparoscopic liver resection: Optimization of in-hospital observation. Surgery 2022, 173, 422–427. [Google Scholar] [CrossRef]
- Dunne, D.F.J.; Jack, S.; Jones, R.P.; Jones, L.; Lythgoe, D.T.; Malik, H.Z.; Poston, G.J.; Palmer, D.H.; Fenwick, S.W. Randomized clinical trial of prehabilitation before planned liver resection. Br. J. Surg. 2016, 103, 504–512. [Google Scholar] [CrossRef]
- Heil, T.C.; Driessen, E.J.M.; Argillander, T.E.; Melis, R.J.F.; Maas, H.A.A.M.; Rikkert, M.G.M.O.; de Wilt, J.H.W.; van Munster, B.C.; Perry, M. Implementation of prehabilitation in colorectal cancer surgery: Qualitative research on how to strengthen facilitators and overcome barriers. Support. Care Cancer 2022, 30, 7373–7386. [Google Scholar] [CrossRef]
- Molenaar, C.J.L.; Janssen, L.; van der Peet, D.L.; Winter, D.C.; Roumen, R.M.H.; Slooter, G.D. Conflicting Guidelines: A Systematic Review on the Proper Interval for Colorectal Cancer Treatment. World J. Surg. 2021, 45, 2235–2250. [Google Scholar] [CrossRef]
- Carli, F.; Charlebois, P.; Stein, B.; Feldman, L.; Zavorsky, G.; Kim, D.J.; Scott, S.; E Mayo, N. Randomized clinical trial of prehabilitation in colorectal surgery. Br. J. Surg. 2010, 97, 1187–1197. [Google Scholar] [CrossRef]
- Vermillion, S.A.; James, A.; Dorrell, R.D.; Brubaker, P.; Mihalko, S.L.; Hill, A.R.; Clark, C.J. Preoperative exercise therapy for gastrointestinal cancer patients: A systematic review. Syst. Rev. 2018, 7, 103. [Google Scholar] [CrossRef]
| Characteristic | Prehabilitation Group (n = 16) | Control Group (n = 47) | p-Value |
|---|---|---|---|
| Age, mean years (SD) | 67 (13.1) | 68 (9.7) | p = 0.938 |
| Male sex, n (%) | 9 (56.3) | 29 (61.7) | p = 0.772 |
| Current smoker, n (%) | 3 (18.8) | 8 (17.0) | p = 0.875 |
| Charlson comorbidity index (CCI) score, mean score (SD) | 7.6 (2.0) | 7.6 (1.8) | p = 0.988 |
| Neoadjuvant therapy, n (%) | p = 0.064 | ||
| Chemotherapy | 7 (43.8) | 7 (14.9) | |
| Radiotherapy | 0 | 1 (2.1) | |
| Chemoradiation | 2 (12.5) | 3 (6.4) | |
| ASA score, n (%) | p = 0.941 | ||
| II | 8 (50) | 24 (51.1) | |
| III | 8 (50) | 23 (48.9) | |
| Surgical procedure for, n (%) | p = 0.998 | ||
| Primary CRC | 9 (56.2) | 26 (55.3) | |
| Left hemicolectomy | 2 (12.5) | 6 (12.8) | |
| Right hemicolectomy | 2 (12.5) | 6 (12.8) | |
| APR | 5 (31.2) | 14 (29.8) | |
| Hepatic metastatic CRC | 4 (25.0) | 12 (25.5) | |
| Segmental resection | 3 (18.8) | 9 (19.1) | |
| Hemihepatectomy | 1 (6.2) | 3 (6.4) | |
| IMM classification | |||
| Grade I | 1 (6.3) | 4 (8.5) | |
| Grade II | 2 (12.5) | 5 (10.6) | |
| Grade III | 1 (6.3) | 3 (6.4) | |
| Peritoneal metastatic CRC | |||
| Single organ resection + | 3 (18.8) | 9 (19.1) | |
| HIPEC | 0 | 0 | |
| Multiple organ resection + | 3 (18.8) | 9 (19.1) | |
| HIPEC | |||
| CCR score | |||
| 0 | 3 (18.8) | 9 (19.1) | |
| 1 | 0 | 0 | |
| 2 | 0 | 0 | |
| 3 | 0 | 0 | |
| Surgical technique, n (%) | p = 0.978 | ||
| Open | 14 (87.5) | 41 (87.2) | |
| Laparoscopic | 2 (12.5) | 6 (12.8) |
| Accrual Rate, n (%) | 16/25 (64%) |
| Completion rate, n (%) | 14/16 (88%) |
| Duration of prehabilitation program, mean days (SD; min–max) | 26.2 (10.7; 7–46) |
| Prescribed supervised training sessions, mean (SD; min–max) | 9.2 (4.7; 1–18) |
| Completed supervised training sessions, mean (SD; min–max) | 8.2 (4.1; 1–14) |
| Adherence rate exercise program, n (%) | 11/16 (69%) |
| Adherence rate nutritional intervention, n of patients with reported protein and vitamin suppletion according to prescriptions (%) | 16/16 (100%) |
| Adherence rate smoke cessation program, n of current smokers with successful smoking cessation prior to surgery (%) | 2/3 (67%) |
| Postoperative Outcome | Prehabilitation Group (n = 16) | Control Group (n = 47) | p-Value |
|---|---|---|---|
| Overall postoperative complication rate, n (%) | 6 (37.5) | 33 (70.2) | p = 0.020 * |
| Clavien–Dindo Classification, grade #, n (%) | |||
| I | 3 (18.8) | 7 (14.9) | |
| II | 1 (6.3) | 9 (19.1) | |
| IIIa | 1 (6.3) | 6 (12.8) | |
| IIIb | 0 | 2 (4.3) | |
| IVa | 1 (6.3) | 3 (6.4) | |
| IVb | 0 | 3 (6.4) | |
| V | 0 | 3 (6.4) | p = 0.342 * |
| Severe postoperative complications (Clavien–Dindo > IIIa) rate, n (%) | 2 (12.5) | 17 (36.2) | p = 0.075 * |
| Length of stay, median days (IQR) | 6 (5–9) | 9 (5–14) | p = 0.160 $ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strijker, D.; Meijerink, W.J.H.J.; van Heusden-Schotalbers, L.A.G.; van den Berg, M.G.A.; van Asseldonk, M.J.M.D.; Drager, L.D.; de Wilt, J.H.W.; van Laarhoven, K.J.H.M.; van den Heuvel, B. Multimodal Prehabilitation in Patients Undergoing Complex Colorectal Surgery, Liver Resection, and Hyperthermic Intraperitoneal Chemotherapy (HIPEC): A Pilot Study on Feasibility and Potential Efficacy. Cancers 2023, 15, 1870. https://doi.org/10.3390/cancers15061870
Strijker D, Meijerink WJHJ, van Heusden-Schotalbers LAG, van den Berg MGA, van Asseldonk MJMD, Drager LD, de Wilt JHW, van Laarhoven KJHM, van den Heuvel B. Multimodal Prehabilitation in Patients Undergoing Complex Colorectal Surgery, Liver Resection, and Hyperthermic Intraperitoneal Chemotherapy (HIPEC): A Pilot Study on Feasibility and Potential Efficacy. Cancers. 2023; 15(6):1870. https://doi.org/10.3390/cancers15061870
Chicago/Turabian StyleStrijker, Dieuwke, Wilhelmus J. H. J. Meijerink, Linda A. G. van Heusden-Schotalbers, Manon G. A. van den Berg, Monique J. M. D. van Asseldonk, Luuk D. Drager, Johannes H. W. de Wilt, Kees J. H. M. van Laarhoven, and Baukje van den Heuvel. 2023. "Multimodal Prehabilitation in Patients Undergoing Complex Colorectal Surgery, Liver Resection, and Hyperthermic Intraperitoneal Chemotherapy (HIPEC): A Pilot Study on Feasibility and Potential Efficacy" Cancers 15, no. 6: 1870. https://doi.org/10.3390/cancers15061870
APA StyleStrijker, D., Meijerink, W. J. H. J., van Heusden-Schotalbers, L. A. G., van den Berg, M. G. A., van Asseldonk, M. J. M. D., Drager, L. D., de Wilt, J. H. W., van Laarhoven, K. J. H. M., & van den Heuvel, B. (2023). Multimodal Prehabilitation in Patients Undergoing Complex Colorectal Surgery, Liver Resection, and Hyperthermic Intraperitoneal Chemotherapy (HIPEC): A Pilot Study on Feasibility and Potential Efficacy. Cancers, 15(6), 1870. https://doi.org/10.3390/cancers15061870






