Clinical-Radiomics Nomogram Based on Contrast-Enhanced Ultrasound for Preoperative Prediction of Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Image Acquisition and Clinicoradiological Characteristics Collection
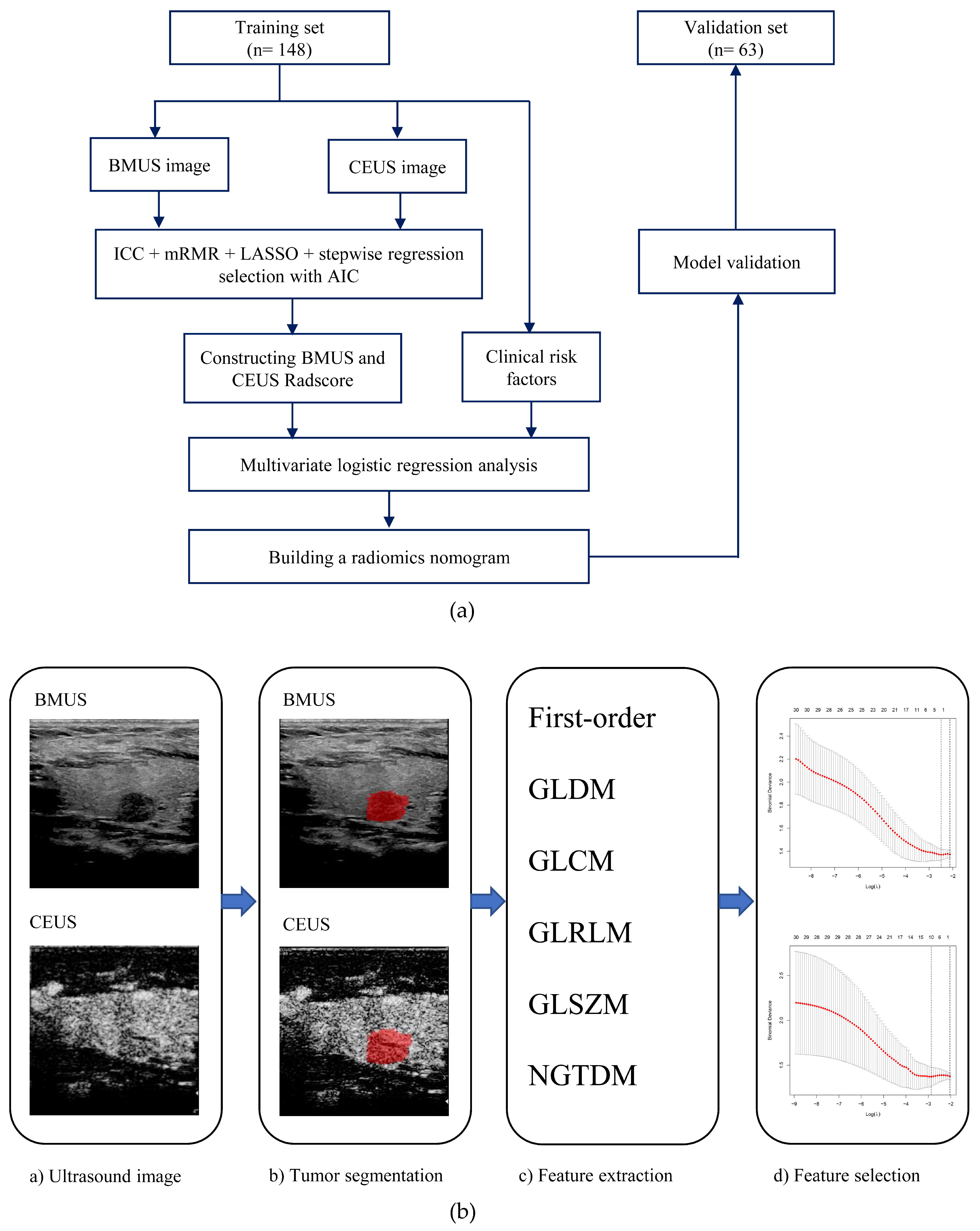
2.3. Image Segmentation and Feature Extraction
2.4. Feature Selection and Radiomics Score Construction
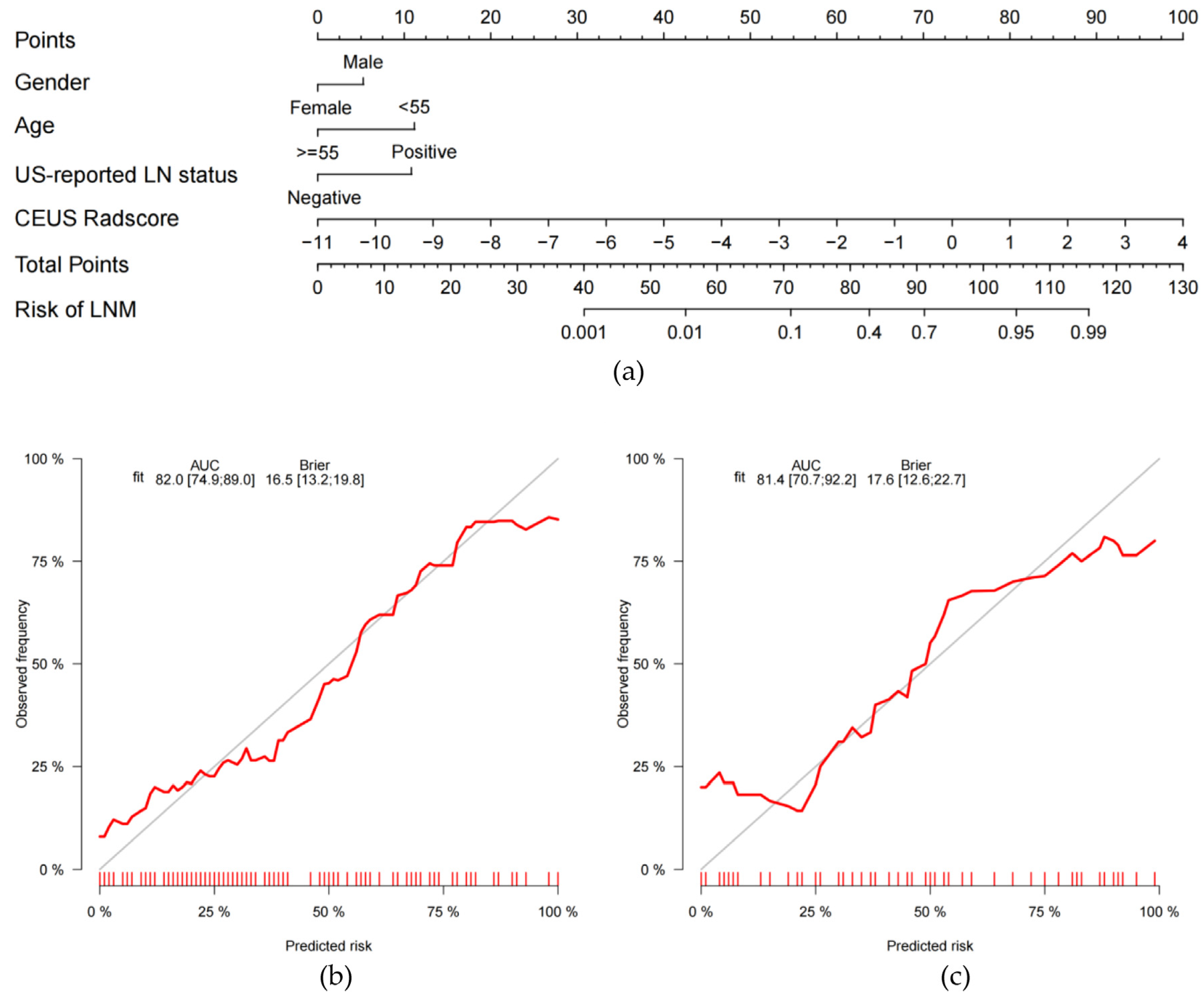
2.5. Development of the Clinical Model and the Clinical-Radiomics Nomogram
2.6. Model Validation
2.7. Statistical Analysis
3. Results
3.1. Clinicoradiological Characteristics
3.2. Radiomics Score Building
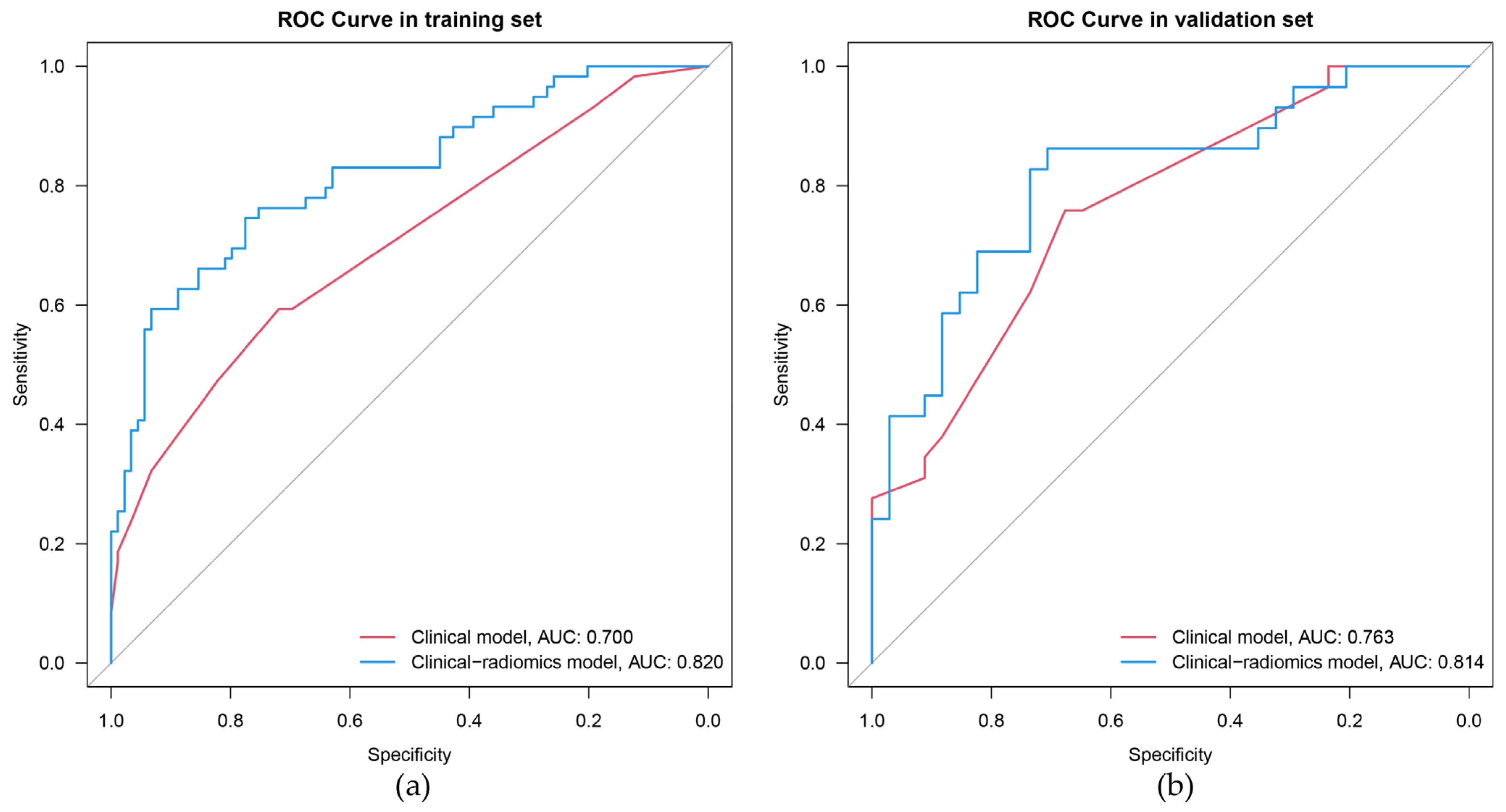
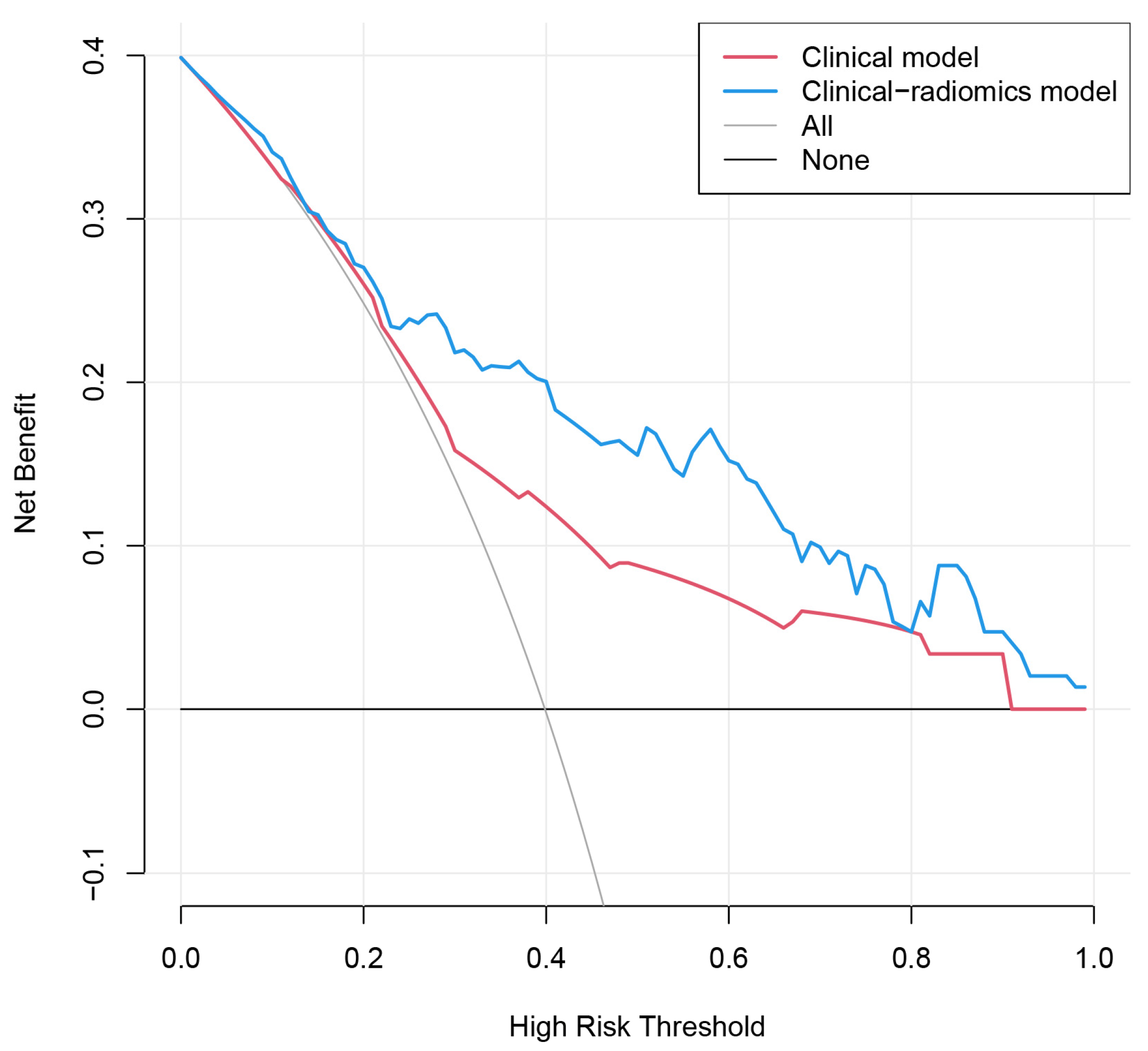
3.3. Model Building and Validation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Grimm, D. Cell and Molecular Biology of Thyroid Disorders. Int. J. Mol. Sci. 2019, 20, 2895. [Google Scholar] [CrossRef] [PubMed]
- Povoa, A.A.; Teixeira, E.; Bella-Cueto, M.R.; Melo, M.; Oliveira, M.J.; Sobrinho-Simoes, M.; Maciel, J.; Soares, P. Clinicopathological Features as Prognostic Predictors of Poor Outcome in Papillary Thyroid Carcinoma. Cancers 2020, 12, 3186. [Google Scholar] [CrossRef]
- Adam, M.A.; Pura, J.; Goffredo, P.; Dinan, M.A.; Reed, S.D.; Scheri, R.P.; Hyslop, T.; Roman, S.A.; Sosa, J.A. Presence and Number of Lymph Node Metastases Are Associated With Compromised Survival for Patients Younger Than Age 45 Years With Papillary Thyroid Cancer. J. Clin. Oncol. 2015, 33, 2370–2375. [Google Scholar] [CrossRef] [PubMed]
- Xue, T.; Liu, C.; Liu, J.J.; Hao, Y.H.; Shi, Y.P.; Zhang, X.X.; Zhang, Y.J.; Zhao, Y.F.; Liu, L.P. Analysis of the Relevance of the Ultrasonographic Features of Papillary Thyroid Carcinoma and Cervical Lymph Node Metastasis on Conventional and Contrast-Enhanced Ultrasonography. Front. Oncol. 2021, 11, 794399. [Google Scholar] [CrossRef]
- Parvathareddy, S.K.; Siraj, A.K.; Ahmed, S.O.; DeVera, F.; Al-Sobhi, S.S.; Al-Dayel, F.; Al-Kuraya, K.S. Risk Factors for Central Lymph Node Metastases and Benefit of Prophylactic Central Lymph Node Dissection in Middle Eastern Patients With cN0 Papillary Thyroid Carcinoma. Front. Oncol. 2021, 11, 819824. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Li, H. Meta-analysis of ultrasound for cervical lymph nodes in papillary thyroid cancer: Diagnosis of central and lateral compartment nodal metastases. Eur. J. Radiol. 2019, 112, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.Q.; Zhang, Z.Z.; Yu, W.J.; Ma, Z.S.; Chen, M.L.; Xie, B.J. Prophylactic Central Neck Dissection for cN1b Papillary Thyroid Carcinoma: A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 803986. [Google Scholar] [CrossRef]
- Sanabria, A.; Betancourt, C.; Sanchez, J.G.; Garcia, C. Prophylactic Central Neck Lymph Node Dissection in Low-Risk Thyroid Carcinoma Patients Does not Decrease the Incidence of Locoregional Recurrence: A Meta-Analysis of Randomized Trials. Ann. Surg. 2022, 276, 66–73. [Google Scholar] [CrossRef]
- Wu, Y.; Rao, K.; Liu, J.; Han, C.; Gong, L.; Chong, Y.; Liu, Z.; Xu, X. Machine Learning Algorithms for the Prediction of Central Lymph Node Metastasis in Patients With Papillary Thyroid Cancer. Front. Endocrinol. 2020, 11, 577537. [Google Scholar] [CrossRef]
- Liu, J.; Jia, X.; Gu, Y.; Chen, X.; Guan, L.; Yan, J.; Zhai, H.; Zhou, N.; Dong, Y.; Zhan, W.; et al. Thyroid Parenchyma Microcalcifications on Ultrasound for Predicting Lymph Node Metastasis in Papillary Thyroid Carcinoma: A Prospective Multicenter Study in China. Front. Oncol. 2021, 11, 609075. [Google Scholar] [CrossRef] [PubMed]
- Zhan, J.; Zhang, L.H.; Yu, Q.; Li, C.L.; Chen, Y.; Wang, W.P.; Ding, H. Prediction of cervical lymph node metastasis with contrast-enhanced ultrasound and association between presence of BRAF(V600E) and extrathyroidal extension in papillary thyroid carcinoma. Ther. Adv. Med. Oncol. 2020, 12, 1758835920942367. [Google Scholar] [CrossRef] [PubMed]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef]
- Li, X.R.; Jin, J.J.; Yu, Y.; Wang, X.H.; Guo, Y.; Sun, H.Z. PET-CT radiomics by integrating primary tumor and peritumoral areas predicts E-cadherin expression and correlates with pelvic lymph node metastasis in early-stage cervical cancer. Eur. Radiol. 2021, 31, 5967–5979. [Google Scholar] [CrossRef]
- Shi, Z.; Ma, C.; Huang, X.; Cao, D. Magnetic Resonance Imaging Radiomics-Based Nomogram From Primary Tumor for Pretreatment Prediction of Peripancreatic Lymph Node Metastasis in Pancreatic Ductal Adenocarcinoma: A Multicenter Study. J. Magn. Reson. Imaging JMRI 2022, 55, 823–839. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Li, W.; Zhang, J.; Tian, S.; Zhou, Y.; Xu, X.; Hu, H.; Lei, D.; Wu, F. Radiomics analysis of CT imaging improves preoperative prediction of cervical lymph node metastasis in laryngeal squamous cell carcinoma. Eur. Radiol. 2022, 33, 1121–1131. [Google Scholar] [CrossRef]
- Tong, Y.; Li, J.; Huang, Y.; Zhou, J.; Liu, T.; Guo, Y.; Yu, J.; Zhou, S.; Wang, Y.; Chang, C. Ultrasound-Based Radiomic Nomogram for Predicting Lateral Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma. Acad. Radiol. 2021, 28, 1675–1684. [Google Scholar] [CrossRef]
- Zhou, S.C.; Liu, T.T.; Zhou, J.; Huang, Y.X.; Guo, Y.; Yu, J.H.; Wang, Y.Y.; Chang, C. An Ultrasound Radiomics Nomogram for Preoperative Prediction of Central Neck Lymph Node Metastasis in Papillary Thyroid Carcinoma. Front. Oncol. 2020, 10, 1591. [Google Scholar] [CrossRef]
- Jiang, M.; Li, C.; Tang, S.; Lv, W.; Yi, A.; Wang, B.; Yu, S.; Cui, X.; Dietrich, C.F. Nomogram Based on Shear-Wave Elastography Radiomics Can Improve Preoperative Cervical Lymph Node Staging for Papillary Thyroid Carcinoma. Thyroid 2020, 30, 885–897. [Google Scholar] [CrossRef] [PubMed]
- Kent, M.S.; Mandrekar, S.J.; Landreneau, R.; Nichols, F.; Foster, N.R.; DiPetrillo, T.A.; Meyers, B.; Heron, D.E.; Jones, D.R.; Tan, A.D.; et al. A Nomogram to Predict Recurrence and Survival of High-Risk Patients Undergoing Sublobar Resection for Lung Cancer: An Analysis of a Multicenter Prospective Study (ACOSOG Z4032). Ann. Thorac. Surg. 2016, 102, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.T.; Macarulla, T.; Blanc, J.F.; Mirakhur, B.; Jong, F.A.; Belanger, B.; Bekaii-Saab, T.; Siveke, J.T. Nomogram for Predicting Survival in Patients Treated with Liposomal Irinotecan Plus Fluorouracil and Leucovorin in Metastatic Pancreatic Cancer. Cancers 2019, 11, 1068. [Google Scholar] [CrossRef]
- Iasonos, A.; Schrag, D.; Raj, G.V.; Panageas, K.S. How to build and interpret a nomogram for cancer prognosis. J. Clin. Oncol. 2008, 26, 1364–1370. [Google Scholar] [CrossRef] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed]
- Gambardella, C.; Offi, C.; Romano, R.M.; De Palma, M.; Ruggiero, R.; Candela, G.; Puziello, A.; Docimo, L.; Grasso, M.; Docimo, G. Transcutaneous laryngeal ultrasonography: A reliable, non-invasive and inexpensive preoperative method in the evaluation of vocal cords motility-a prospective multicentric analysis on a large series and a literature review. Updat. Surg. 2020, 72, 885–892. [Google Scholar] [CrossRef] [PubMed]
- Canu, G.L.; Medas, F.; Cappellacci, F.; Giordano, A.B.F.; Gurrado, A.; Gambardella, C.; Docimo, G.; Feroci, F.; Conzo, G.; Testini, M.; et al. Risk of Complications in Patients Undergoing Completion Thyroidectomy after Hemithyroidectomy for Thyroid Nodule with Indeterminate Cytology: An Italian Multicentre Retrospective Study. Cancers 2022, 14, 2472. [Google Scholar] [CrossRef]
- Marotta, V.; Sciammarella, C.; Capasso, M.; Testori, A.; Pivonello, C.; Chiofalo, M.G.; Gambardella, C.; Grasso, M.; Antonino, A.; Annunziata, A.; et al. Germline Polymorphisms of the VEGF Pathway Predict Recurrence in Nonadvanced Differentiated Thyroid Cancer. J. Clin. Endocrinol. Metab. 2017, 102, 661–671. [Google Scholar] [CrossRef]
- Zhang, K.; Qian, L.; Chen, J.; Zhu, Q.; Chang, C. Preoperative Prediction of Central Cervical Lymph Node Metastasis in Fine-Needle Aspiration Reporting Suspicious Papillary Thyroid Cancer or Papillary Thyroid Cancer Without Lateral Neck Metastasis. Front. Oncol. 2022, 12, 712723. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.; Wang, W. A Non-invasive Method to Diagnose Lung Adenocarcinoma. Front. Oncol. 2020, 10, 602. [Google Scholar] [CrossRef] [PubMed]
- Starkov, P.; Aguilera, T.A.; Golden, D.I.; Shultz, D.B.; Trakul, N.; Maxim, P.G.; Le, Q.T.; Loo, B.W.; Diehn, M.; Depeursinge, A.; et al. The use of texture-based radiomics CT analysis to predict outcomes in early-stage non-small cell lung cancer treated with stereotactic ablative radiotherapy. Br. J. Radiol. 2019, 92, 20180228. [Google Scholar] [CrossRef] [PubMed]
- Lambin, P.; Rios-Velazquez, E.; Leijenaar, R.; Carvalho, S.; van Stiphout, R.G.; Granton, P.; Zegers, C.M.; Gillies, R.; Boellard, R.; Dekker, A.; et al. Radiomics: Extracting more information from medical images using advanced feature analysis. Eur. J. Cancer 2012, 48, 441–446. [Google Scholar] [CrossRef]
- Liu, L.S.; Liang, J.; Li, J.H.; Liu, X.; Jiang, L.; Long, J.X.; Jiang, Y.M.; Wei, Z.X. The incidence and risk factors for central lymph node metastasis in cN0 papillary thyroid microcarcinoma: A meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 1327–1338. [Google Scholar] [CrossRef]
- Huang, Y.; Huang, Z.; Cai, H.; Zhuge, L.; Wang, S.; Yan, D.; Zhang, X.; An, C.; Niu, L.; Li, Z. Evaluation of serum B7-H3 expression, ultrasound and clinical characteristics to predict the risk of cervical lymph node metastases in papillary thyroid carcinoma by nomogram. J. Clin. Lab. Anal. 2022, 37, e24811. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Min, Y.; Chen, H.; Xiang, K.; Wang, X.; Yin, G. Construction and validation of a nomogram for predicting cervical lymph node metastasis in classic papillary thyroid carcinoma. J. Endocrinol. Investig. 2021, 44, 2203–2211. [Google Scholar] [CrossRef]
- Mao, J.; Zhang, Q.; Zhang, H.; Zheng, K.; Wang, R.; Wang, G. Risk Factors for Lymph Node Metastasis in Papillary Thyroid Carcinoma: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2020, 11, 265. [Google Scholar] [CrossRef]
- Suteau, V.; Munier, M.; Briet, C.; Rodien, P. Sex Bias in Differentiated Thyroid Cancer. Int. J. Mol. Sci. 2021, 22, 12992. [Google Scholar] [CrossRef] [PubMed]
- Xing, Z.; Qiu, Y.; Yang, Q.; Yu, Y.; Liu, J.; Fei, Y.; Su, A.; Zhu, J. Thyroid cancer neck lymph nodes metastasis: Meta-analysis of US and CT diagnosis. Eur. J. Radiol. 2020, 129, 109103. [Google Scholar] [CrossRef]
- Goncalves, M.; Gsaxner, C.; Ferreira, A.; Li, J.; Puladi, B.; Kleesiek, J.; Egger, J.; Alves, V. Radiomics in Head and Neck Cancer Outcome Predictions. Diagnostics 2022, 12, 2733. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Jiang, T.; Zhang, C.; Zhang, Y.; Huang, Z.; Zhou, H.; Huang, P. A nomogram based on clinical information, conventional ultrasound and radiomics improves prediction of malignant parotid gland lesions. Cancer Lett. 2022, 527, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Wang, J.; Xu, D.; Zhu, C.; Qin, J.; Wu, Y.; Gao, Y.; Zhang, C. Automatic Breast Volume Scanner and B-Ultrasound-Based Radiomics Nomogram for Clinician Management of BI-RADS 4A Lesions. Acad. Radiol. 2022. [Google Scholar] [CrossRef]
- Jiang, M.; Li, C.L.; Luo, X.M.; Chuan, Z.R.; Chen, R.X.; Tang, S.C.; Lv, W.Z.; Cui, X.W.; Dietrich, C.F. Radiomics model based on shear-wave elastography in the assessment of axillary lymph node status in early-stage breast cancer. Eur. Radiol. 2022, 32, 2313–2325. [Google Scholar] [CrossRef]
- Habibollahi, P.; Sultan, L.R.; Bialo, D.; Nazif, A.; Faizi, N.A.; Sehgal, C.M.; Chauhan, A. Hyperechoic Renal Masses: Differentiation of Angiomyolipomas from Renal Cell Carcinomas using Tumor Size and Ultrasound Radiomics. Ultrasound. Med. Biol. 2022, 48, 887–894. [Google Scholar] [CrossRef]
- Agyekum, E.A.; Ren, Y.Z.; Wang, X.; Cranston, S.S.; Wang, Y.G.; Wang, J.; Akortia, D.; Xu, F.J.; Gomashie, L.; Zhang, Q.; et al. Evaluation of Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma Using Clinical-Ultrasound Radiomic Machine Learning-Based Model. Cancers 2022, 14, 5266. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Ge, X.; Yu, J.; Guo, Y.; Wang, Y.; Wang, W.; Cui, L. Comparison of the application of B-mode and strain elastography ultrasound in the estimation of lymph node metastasis of papillary thyroid carcinoma based on a radiomics approach. Int. J. Comput. Assist. Radiol. Surg 2018, 13, 1617–1627. [Google Scholar] [CrossRef]
- Wang, Y.G.; Xu, F.J.; Agyekum, E.A.; Xiang, H.; Wang, Y.D.; Zhang, J.; Sun, H.; Zhang, G.L.; Bo, X.S.; Lv, W.Z.; et al. Radiomic Model for Determining the Value of Elasticity and Grayscale Ultrasound Diagnoses for Predicting BRAF(V600E) Mutations in Papillary Thyroid Carcinoma. Front. Endocrinol. 2022, 13, 872153. [Google Scholar] [CrossRef]
- Guo, S.Y.; Zhou, P.; Zhang, Y.; Jiang, L.Q.; Zhao, Y.F. Exploring the Value of Radiomics Features Based on B-Mode and Contrast-Enhanced Ultrasound in Discriminating the Nature of Thyroid Nodules. Front. Oncol. 2021, 11, 738909. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.R.; Yan, C.X.; Mo, G.Q.; Luo, Z.Y.; Zhang, Y.; Wang, Y.; Huang, P.T. Conventional US, elastography, and contrast enhanced US features of papillary thyroid microcarcinoma predict central compartment lymph node metastases. Sci. Rep. 2015, 5, 7748. [Google Scholar] [CrossRef]
- Park, H.S.; Lee, K.S.; Seo, B.K.; Kim, E.S.; Cho, K.R.; Woo, O.H.; Song, S.E.; Lee, J.Y.; Cha, J. Machine Learning Models That Integrate Tumor Texture and Perfusion Characteristics Using Low-Dose Breast Computed Tomography Are Promising for Predicting Histological Biomarkers and Treatment Failure in Breast Cancer Patients. Cancers 2021, 13, 6013. [Google Scholar] [CrossRef]
- Zhan, W.W.; Zhou, P.; Zhou, J.Q.; Xu, S.Y.; Chen, K.M. Differences in sonographic features of papillary thyroid carcinoma between neck lymph node metastatic and nonmetastatic groups. J. Ultrasound Med. 2012, 31, 915–920. [Google Scholar] [CrossRef]
- Ng, F.; Ganeshan, B.; Kozarski, R.; Miles, K.A.; Goh, V. Assessment of primary colorectal cancer heterogeneity by using whole-tumor texture analysis: Contrast-enhanced CT texture as a biomarker of 5-year survival. Radiology 2013, 266, 177–184. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhou, G.; Zhang, J.; Xu, C.; Zhu, F.; Xu, P. DCE-MRI based radiomics nomogram for preoperatively differentiating combined hepatocellular-cholangiocarcinoma from mass-forming intrahepatic cholangiocarcinoma. Eur. Radiol. 2022, 32, 5004–5015. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.; Yang, P.; Zhang, X.; Xu, L.; Wang, X.; Li, X.; Zhang, L.; Xie, R.; Yang, L.; Jing, Z.; et al. Sub-region based radiomics analysis for survival prediction in oesophageal tumours treated by definitive concurrent chemoradiotherapy. EBioMedicine 2019, 44, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Yin, J.; Han, P.; Chen, N.; Kang, Q.; Qiu, Y.; Li, Y.; Lao, Q.; Sun, M.; Yang, D.; et al. Wavelet transformation can enhance computed tomography texture features: A multicenter radiomics study for grade assessment of COVID-19 pulmonary lesions. Quant. Imaging Med. Surg. 2022, 12, 4758–4770. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Training Set (n = 148) | Validation Set (n = 63) | p-Value |
|---|---|---|---|
| Lymph node metastasis | 0.406 | ||
| Negative | 89 (60.1) | 34 (54.0) | |
| Positive | 59 (39.9) | 29 (46.0) | |
| Age | 0.531 | ||
| <55 years | 125 (84.5) | 51 (81.0) | |
| ≥55 years | 23 (15.5) | 12 (19.0) | |
| Gender | 0.495 | ||
| Female | 111 (75.0) | 50 (79.4) | |
| Male | 37 (25.0) | 13 (20.6) | |
| Primary site | 0.299 | ||
| Left lobe | 61 (41.2) | 33 (52.4) | |
| Right lobe | 78 (52.7) | 26 (41.3) | |
| Isthmus | 9 (6.1) | 4 (6.3) | |
| Tumor location | 0.980 | ||
| Intra-thyroidal | 35 (23.6) | 15 (23.8) | |
| Sub-capsular | 113 (76.4) | 48 (76.2) | |
| Tumor size | 0.106 | ||
| ≤10 mm | 106 (71.6) | 38 (60.3) | |
| >10 mm | 42 (28.4) | 25 (39.7) | |
| Echogenicity | 0.583 | ||
| iso/hyperechoic | 7 (4.7) | 3 (4.8) | |
| hypoechoic | 58 (39.2) | 20 (31.7) | |
| marked hypoechoic | 83 (56.1) | 40 (63.5) | |
| Aspect ratio > 1 | 0.757 | ||
| Absent | 93 (62.8) | 41 (65.1) | |
| Present | 55 (37.2) | 22 (34.9) | |
| Margin | 0.579 | ||
| Smooth | 7 (4.7) | 3 (4.8) | |
| Ill-defined | 12 (8.1) | 8 (12.7) | |
| Irregular | 129 (87.2) | 52 (82.5) | |
| Microcalcification | 0.571 | ||
| Absent | 39 (26.4) | 19 (30.2) | |
| Present | 109 (73.6) | 44 (69.8) | |
| Enhancement pattern | 0.329 | ||
| Hyper-enhancement | 7 (4.7) | 1 (1.6) | |
| Iso-enhancement | 34 (23.0) | 11 (17.5) | |
| Hypo-enhancement | 107 (72.3) | 51 (81.0) | |
| US-reported LN status | 0.062 | ||
| Negative | 130 (87.8) | 49 (77.8) | |
| Positive | 18 (12.2) | 14 (22.2) | |
| BMUS Radscore, | 0.662 | ||
| Median (Interquartile range) | −0.40 (−0.71, −0.07) | −0.32 (−0.84, 0.10) | |
| CEUS Radscore, | 0.185 | ||
| Median (Interquartile range) | −0.54 (−1.20, 0.29) | −0.37 (−0.87, 0.36) |
| Characteristic | Training Set | Validation Set | ||||
|---|---|---|---|---|---|---|
| LNM− | LNM+ | p-Value | LNM− | LNM+ | p-Value | |
| Age | 0.017 | 0.023 | ||||
| <55 years | 70 (78.7) | 55 (93.2) | 24 (70.6) | 27 (93.1) | ||
| ≥55 years | 19 (21.3) | 4 (6.8) | 10 (29.4) | 2 (6.9) | ||
| Gender | 0.042 | 0.060 | ||||
| Female | 72 (80.9) | 39 (66.1) | 30 (88.2) | 20 (69.0) | ||
| Male | 17 (19.1) | 20 (33.9) | 4 (11.8) | 9 (31.0) | ||
| Primary site | 0.642 | 0.401 | ||||
| Left lobe | 34 (38.2) | 27 (45.8) | 17 (50.0) | 16 (55.2) | ||
| Right lobe | 49 (55.1) | 29 (49.2) | 16 (47.1) | 10 (34.5) | ||
| Isthmus | 6 (6.7) | 3 (5.1) | 1 (2.9) | 3 (10.3) | ||
| Tumor location | 0.118 | 0.020 | ||||
| Intra-thyroidal | 25 (28.1) | 10 (16.9) | 12 (35.3) | 3 (10.3) | ||
| Sub-capsular | 64 (71.9) | 49 (83.1) | 22 (64.7) | 26 (89.7) | ||
| Tumor size | 0.002 | <0.001 | ||||
| >10 mm | 72 (80.9) | 34 (57.6) | 27 (79.4) | 11 (37.9) | ||
| ≤10 mm | 17 (19.1) | 25 (42.4) | 7 (20.6) | 18 (62.1) | ||
| Echogenicity | 0.409 | 0.497 | ||||
| iso/hyperechoic | 5 (5.6) | 2 (3.4) | 1 (2.9) | 2 (6.9) | ||
| hypoechoic | 31 (34.8) | 27 (45.8) | 13 (38.2) | 7 (24.1) | ||
| marked hypoechoic | 53 (59.6) | 30 (50.8) | 20 (58.8) | 20 (69.0) | ||
| Aspect ratio > 1 | 0.309 | 0.029 | ||||
| Absent | 53 (59.6) | 40 (67.8) | 18 (52.9) | 23 (79.3) | ||
| Present | 36 (40.4) | 19 (32.2) | 16 (47.1) | 6 (20.7) | ||
| Margin | 1.000 | 0.146 | ||||
| Smooth | 4 (4.5) | 3 (5.1) | 1 (2.9) | 2 (6.9) | ||
| Ill-defined | 7 (7.9) | 5 (8.5) | 2 (5.9) | 6 (20.7) | ||
| Irregular | 78 (87.6) | 51 (86.4) | 31 (91.2) | 21 (72.4) | ||
| Microcalcification | 0.083 | 0.336 | ||||
| Absent | 28 (31.5) | 11 (18.6) | 12 (35.3) | 7 (24.1) | ||
| Present | 61 (68.5) | 48 (81.4) | 22 (64.7) | 22 (75.9) | ||
| Enhancement pattern | 0.155 | 0.860 | ||||
| Hyper-enhancement | 2 (2.2) | 5 (8.5) | 0 (0.0) | 1 (3.4) | ||
| Iso-enhancement | 23 (25.8) | 11 (18.6) | 6 (17.6) | 5 (17.2) | ||
| Hypo-enhancement | 64 (71.9) | 43 (72.9) | 28 (82.4) | 23 (79.3) | ||
| US-reported LN status | <0.001 | 0.031 | ||||
| Negative | 85 (95.5) | 45 (76.3) | 30 (88.2) | 19 (65.5) | ||
| Positive | 4 (4.5) | 14 (23.7) | 4 (11.8) | 10 (34.5) | ||
| BMUS Radscore | 0.001 | 0.004 | ||||
| Median (Interquartile range) | −0.51 (−0.85, −0.21) | −0.25 (−0.50, 0.04) | −0.53 (−1.00, −0.16) | −0.02 (−0.52, 0.28) | ||
| CEUS Radscore | <0.001 | 0.002 | ||||
| Median (Interquartile range) | −0.89 (−1.71, −0.28) | 0.12 (−0.54, 0.66) | −0.66 (−1.18, −0.07) | 0.10 (−0.37, 0.75) | ||
| Characteristics | Odds Ratio (95%CI) | p-Value |
|---|---|---|
| Clinical model | ||
| Gender (male vs. female) | 2.18 (0.95, 5.00) | 0.067 |
| Age (≥55 years vs. <55 years) | 0.30 (0.09, 0.96) | 0.042 |
| Tumor size (>10 mm vs. ≤10 mm) | 2.22 (1.00, 4.95) | 0.051 |
| US-reported LN status (positive vs. negative) | 4.86 (1.40, 16.83) | 0.013 |
| Clinical-radiomics model | ||
| Gender (male vs. female) | 2.22 (0.86, 5.74) | 0.100 |
| Age (≥55 years vs. <55 years) | 0.18 (0.05, 0.70) | 0.013 |
| US-reported LN status (positive vs. negative) | 5.16 (1.40, 18.98) | 0.014 |
| CEUS Radscore | 2.75 (1.79, 4.23) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, L.; Zhang, Z.; Guo, S.; Zhao, Y.; Zhou, P. Clinical-Radiomics Nomogram Based on Contrast-Enhanced Ultrasound for Preoperative Prediction of Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma. Cancers 2023, 15, 1613. https://doi.org/10.3390/cancers15051613
Jiang L, Zhang Z, Guo S, Zhao Y, Zhou P. Clinical-Radiomics Nomogram Based on Contrast-Enhanced Ultrasound for Preoperative Prediction of Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma. Cancers. 2023; 15(5):1613. https://doi.org/10.3390/cancers15051613
Chicago/Turabian StyleJiang, Liqing, Zijian Zhang, Shiyan Guo, Yongfeng Zhao, and Ping Zhou. 2023. "Clinical-Radiomics Nomogram Based on Contrast-Enhanced Ultrasound for Preoperative Prediction of Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma" Cancers 15, no. 5: 1613. https://doi.org/10.3390/cancers15051613
APA StyleJiang, L., Zhang, Z., Guo, S., Zhao, Y., & Zhou, P. (2023). Clinical-Radiomics Nomogram Based on Contrast-Enhanced Ultrasound for Preoperative Prediction of Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma. Cancers, 15(5), 1613. https://doi.org/10.3390/cancers15051613






