Does the Gain of Total Neoadjuvant Therapy Outweigh the Harm in Rectal Cancer? Importance of the ATRESS (neoAdjuvant Therapy-RElated Shortening of Survival) Phenomenon: A Systematic Review
Abstract
Simple Summary
Abstract
1. Introduction
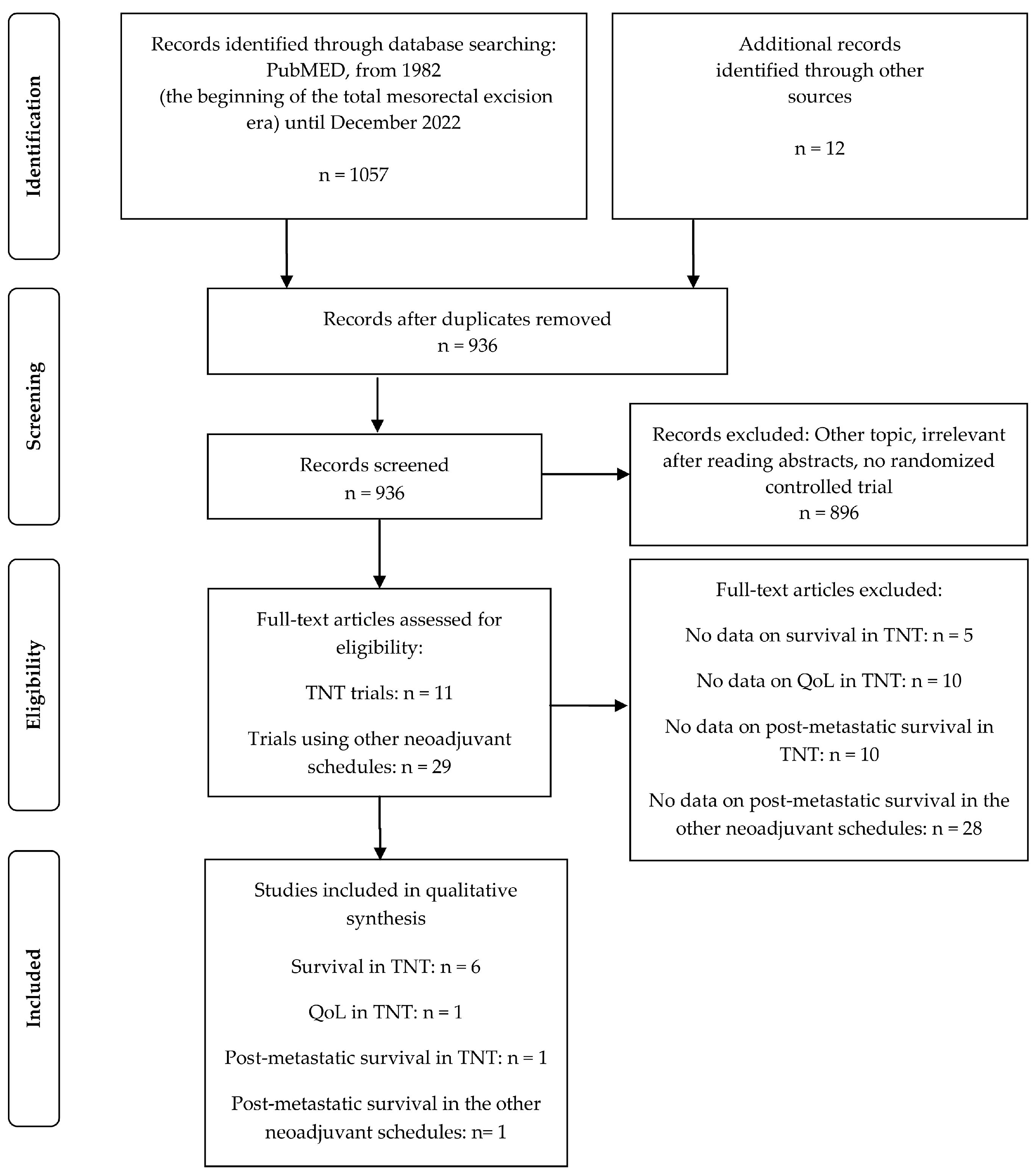
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Data Extraction
2.5. Statistical Methods
3. Results
3.1. Overview of Randomised Trials on TNT
3.2. Evaluation of QoL after TNT Given without Considering w&w
3.3. Evaluation of ATRESS after TNT
3.4. ATRESS in Other Trials Exploring Neoadjuvant Therapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Breugom, A.J.; Swets, M.; Bosset, J.-F.; Collette, L.; Sainato, A.; Cionini, L.; Glynne-Jones, R.; Counsell, N.; Bastiaannet, E.; van den Broek, C.B.M.; et al. Adjuvant chemotherapy after preoperative (chemo)radiotherapy and surgery for patients with rectal cancer: A systematic review and meta-analysis of individual patient data. Lancet Oncol. 2015, 16, 200–207. [Google Scholar] [CrossRef]
- Bujko, K.; Glimelius, B.; Valentini, V.; Michalski, W.; Spalek, M. Postoperative chemotherapy in patients with rectal cancer receiving preoperative radio(chemo)therapy: A meta-analysis of randomized trials comparing surgery ± a fluoropyrimidine and surgery + a fluoropyrimidine ± oxaliplatin. Eur. J. Surg. Oncol. 2015, 41, 713–723. [Google Scholar] [CrossRef]
- Fernandez-Martos, C.; Garcia-Albeniz, X.; Pericay, C.; Maurel, J.; Aparicio, J.; Montagut, C.; Safont, M.J.; Salud, A.; Vera, R.; Massuti, B.; et al. Chemoradiation, surgery and adjuvant chemotherapy versus induction chemotherapy followed by chemoradiation and surgery: Long-term results of the Spanish GCR-3 phase II randomized trial. Ann. Oncol. 2015, 26, 1722–1728. [Google Scholar] [CrossRef] [PubMed]
- Bahadoer, R.R.; A Dijkstra, E.; van Etten, B.; Marijnen, C.A.M.; Putter, H.; Kranenbarg, E.M.-K.; Roodvoets, A.G.H.; Nagtegaal, I.D.; Beets-Tan, R.G.H.; Blomqvist, L.K.; et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): A randomised, open-label, phase 3 trial. Lancet Oncol. 2020, 22, 29–42. [Google Scholar] [CrossRef]
- Conroy, T.; Bosset, J.-F.; Etienne, P.-L.; Rio, E.; François, E.; Mesgouez-Nebout, N.; Vendrely, V.; Artignan, X.; Bouché, O.; Gargot, D.; et al. Neoadjuvant chemotherapy with FOLFIRINOX and preoperative chemoradiotherapy for patients with locally advanced rectal cancer (UNICANCER-PRODIGE 23): A multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 702–715. [Google Scholar] [CrossRef] [PubMed]
- De Gramont, A.; Hubbard, J.; Shi, Q.; O’Connell, M.J.; Buyse, M.; Benedetti, J.; Bot, B.; O’Callaghan, C.; Yothers, G.; Goldberg, R.M.; et al. Association Between Disease-Free Survival and Overall Survival When Survival Is Prolonged After Recurrence in Patients Receiving Cytotoxic Adjuvant Therapy for Colon Cancer: Simulations Based on the 20,800 Patient ACCENT Data Set. J. Clin. Oncol. 2010, 28, 460–465. [Google Scholar] [CrossRef]
- Socha, J.; Bujko, K. Are we already in the era of total neoadjuvant treatment for rectal cancer? Lancet Oncol. 2021, 22, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Bahadoer, R.; Dijkstra, E. Patterns of locoregional failure and distant metastases in patients treated for locally advanced rectal cancer in the RAPIDO trial. Eur. J. Surg. Oncol. 2022, 48, e34. [Google Scholar] [CrossRef]
- Fink, M.K. Does adjuvant therapy reduce postmetastatic survival? Ann. Oncol. 2019, 30, 1184–1188. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Aguilar, J.; Patil, S.; Gollub, M.J.; Kim, J.K.; Yuval, J.B.; Thompson, H.M.; Verheij, F.S.; Omer, D.M.; Lee, M.; Dunne, R.F.; et al. Organ Preservation in Patients with Rectal Adenocarcinoma Treated with Total Neoadjuvant Therapy. J. Clin. Oncol. 2022, 40, 2546–2556. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Ciseł, B.; Pietrzak, L.; Michalski, W.; Wyrwicz, L.; Rutkowski, A.; Kosakowska, E.; Cencelewicz, A.; Spałek, M.; Polkowski, W.; Jankiewicz, M.; et al. Long-course preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for clinical T4 and fixed clinical T3 rectal cancer: Long-term results of the randomized Polish II study. Ann. Oncol. 2019, 30, 1298–1303. [Google Scholar] [CrossRef]
- Bujko, K.; Wyrwicz, L.; Rutkowski, A.; Malinowska, M.; Pietrzak, L.; Kryński, J.; Michalski, W.; Olędzki, J.; Kuśnierz, J.; Zając, L.; et al. Long-course oxaliplatin-based preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: Results of a randomized phase III study. Ann. Oncol. 2016, 27, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Garant, A.; Kavan, P.; Martin, A.-G.; Azoulay, L.; Vendrely, V.; Lavoie, C.; Vasilevsky, C.-A.; Boutros, M.; Faria, J.; Nguyen, T.N.; et al. Optimizing treatment sequencing of chemotherapy for patients with rectal cancer: The KIR randomized phase II trial. Radiother. Oncol. 2020, 155, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Tang, Y.; Hu, C.; Jiang, L.-M.; Jiang, J.; Li, N.; Liu, W.-Y.; Chen, S.-L.; Li, S.; Lu, N.-N.; et al. Multicenter, Randomized, Phase III Trial of Short-Term Radiotherapy Plus Chemotherapy Versus Long-Term Chemoradiotherapy in Locally Advanced Rectal Cancer (STELLAR). J. Clin. Oncol. 2022, 40, 1681–1692. [Google Scholar] [CrossRef]
- Dijkstra, E.A.; Hospers, G.A.; Kranenbarg, E.M.-K.; Fleer, J.; Roodvoets, A.G.; Bahadoer, R.R.; Guren, M.G.; Tjalma, J.J.; Putter, H.; Crolla, R.M.; et al. Quality of life and late toxicity after short-course radiotherapy followed by chemotherapy or chemoradiotherapy for locally advanced rectal cancer–The RAPIDO trial. Radiother. Oncol. 2022, 171, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Schmoll, H.-J.; Mauer, M.E.; Marreaud, S.; Stein, A. Reply to P. Potemski and K. Bujko. J. Clin. Oncol. 2021, 39, 1306–1308. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, M.J.; Campbell, M.E.; Goldberg, R.M.; Grothey, A.; Seitz, J.-F.; Benedetti, J.K.; André, T.; Haller, D.G.; Sargent, D. Survival Following Recurrence in Stage II and III Colon Cancer: Findings from the ACCENT Data Set. J. Clin. Oncol. 2008, 26, 2336–2341. [Google Scholar] [CrossRef] [PubMed]
- Moertel, C.G.; Fleming, T.R.; Macdonald, J.S.; Haller, D.G.; Laurie, J.A.; Tangen, C.M.; Ungerleider, J.S.; Emerson, W.A.; Tormey, D.C.; Glick, J.H.; et al. Fluorouracil plus Levamisole as Effective Adjuvant Therapy after Resection of Stage III Colon Carcinoma: A Final Report. Ann. Intern. Med. 1995, 122, 321–326. [Google Scholar] [CrossRef]
- André, T.; Boni, C.; Navarro, M.; Tabernero, J.; Hickish, T.; Topham, C.; Bonetti, A.; Clingan, P.; Bridgewater, J.; Rivera, F.; et al. Improved Overall Survival with Oxaliplatin, Fluorouracil, and Leucovorin As Adjuvant Treatment in Stage II or III Colon Cancer in the MOSAIC Trial. J. Clin. Oncol. 2009, 27, 3109–3116. [Google Scholar] [CrossRef]
- Yothers, G.A.; O’Connell, M.J.; Colangelo, L. Fluorouracil and leucovorin (Lv) with or without oxaliplatin (Ox) for adjuvant treatment of stage II and III colon cancer: Long-term follow-up of NSABP C-07 with survival analysis (abstract 401). In Proceedings of the American Society for Clinical Oncology Gastrointestinal Cancers Symposium, Orlando, FL, USA, 22–24 January 2010. [Google Scholar]
- Schmoll, H.-J.; Twelves, C.; Sun, W.; O’Connell, M.J.; Cartwright, T.; McKenna, E.; Saif, M.; Lee, S.; Yothers, G.; Haller, D. Effect of adjuvant capecitabine or fluorouracil, with or without oxaliplatin, on survival outcomes in stage III colon cancer and the effect of oxaliplatin on post-relapse survival: A pooled analysis of individual patient data from four randomised controlled trials. Lancet Oncol. 2014, 15, 1481–1492. [Google Scholar] [CrossRef] [PubMed]
- Kanemitsu, Y.; Shimizu, Y.; Mizusawa, J.; Inaba, Y.; Hamaguchi, T.; Shida, D.; Ohue, M.; Komori, K.; Shiomi, A.; Shiozawa, M.; et al. Hepatectomy Followed by mFOLFOX6 Versus Hepatectomy Alone for Liver-Only Metastatic Colorectal Cancer (JCOG0603): A Phase II or III Randomized Controlled Trial. J. Clin. Oncol. 2021, 39, 3789–3799. [Google Scholar] [CrossRef]
- Andreou, A.; Kopetz, S.; Maru, D.M.; Chen, S.S.; Zimmitti, G.; Brouquet, A.; Shindoh, J.; Curley, S.A.; Garrett, C.; Overman, M.J.; et al. Adjuvant Chemotherapy with FOLFOX for Primary Colorectal Cancer Is Associated with Increased Somatic Gene Mutations and Inferior Survival in Patients Undergoing Hepatectomy for Metachronous Liver Metastases. Ann. Surg. 2012, 256, 642–650. [Google Scholar] [CrossRef]
- Tournigand, C.; André, T.; Bonnetain, F.; Chibaudel, B.; Lledo, G.; Hickish, T.; Tabernero, J.; Boni, C.; Bachet, J.-B.; Teixeira, L.; et al. Adjuvant Therapy with Fluorouracil and Oxaliplatin in Stage II and Elderly Patients (between ages 70 and 75 years) With Colon Cancer: Subgroup Analyses of the Multicenter International Study of Oxaliplatin, Fluorouracil, and Leucovorin in the Adjuvant Treatment of Colon Cancer Trial. J. Clin. Oncol. 2012, 30, 3353–3360. [Google Scholar] [CrossRef] [PubMed]
- Klement, R.J.; Allgäuer, M.; Andratschke, N.; Blanck, O.; Boda-Heggemann, J.; Dieckmann, K.; Duma, M.; Ernst, I.; Flentje, M.; Ganswindt, U.; et al. Bayesian Cure Rate Modeling of Local Tumor Control: Evaluation in Stereotactic Body Radiation Therapy for Pulmonary Metastases. Int. J. Radiat. Oncol. 2015, 94, 841–849. [Google Scholar] [CrossRef] [PubMed]
- Klement, R.; Guckenberger, M.; Alheid, H.; Allgäuer, M.; Becker, G.; Blanck, O.; Boda-Heggemann, J.; Brunner, T.; Duma, M.; Gerum, S.; et al. Stereotactic body radiotherapy for oligo-metastatic liver disease–Influence of pre-treatment chemotherapy and histology on local tumor control. Radiother. Oncol. 2017, 123, 227–233. [Google Scholar] [CrossRef]
| Study | Number of Patients | Design | Median Follow-Up (Years) | DFS Results (TNT vs. Control) | OS Results (TNT vs. Control) | LRF Results (TNT vs. Control) | Survival After the Onset of DM in Years (TNT vs. Control) | Remarks | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| TNT | Neoadjuvant (chemo)Radiation | Adjuvant Chemotherapy | DFS (%), p-Value | OS (%), p-Value | LRF (%), p-Value | ||||||
| TNT | Control | ||||||||||
| GCR-3 [3] 2015 | 108 | CAPOX (12 weeks) + CRT: 50.4 Gy + Cape and Ox | CRT: 50.4 Gy + Cape and Ox | No postoperative chemotherapy | CAPOX 4x | 5.8 | 5-year: 62 vs. 64, p = 0.85, HR not given | 5-year: 75 vs. 78, p = 0.64, HR not given | 5-year: 5 vs. 2, p = 0.61, HR not given | No data | Pure design; only the sequence of chemotherapy differed (neoadjuvant vs. adjuvant). |
| POLISH II [12,13] 2019 | 515 | RT 5x5Gy + FOLFOX or FU+LV (6 weeks) | 50.4 Gy + 5-FU and LV or 5-FU, LV and OX | c Optional | c Optional | 7.0 | 8-year: 43 vs. 41, p = 0.65, HR 0.95 (95% CI 0.75–1.19) 3-year: 53 vs. 52, p = 0.85, HR 0.96 (95% CI 0.75–1.24) | 8-year: 49 vs. 49, p = 0.38, HR 0.90 (95% CI 0.70–1.15) 3-year: 73 vs. 65, p = 0.046, HR 0.73 (95% CI 0.53–1.01) | 8-year: 35 vs. 32, p = 0.60, HR 1.08 (95% CI 0.70–1.23) | Median 1.7 (95% CI 1.1–2.2) vs. 1.0 (95% CI 0.7–1.4), HR 0.84 (95% CI 0.61–1.17), p = 0.30. | Short-course radiation was used in the TNT group and chemoradiation in the control group. Neoadjuvant chemotherapy was used only for 6 weeks. |
| KIR [14] 2021 | 180 a | FOLFOX (12 weeks) + HDRBT | HDRBT | FOLFOX (12 weeks) | FOLFOX (24 weeks) | 4.0 | 5-year: 72.3 vs. 68.3, p = 0.74, HR not given | 5-year: 83.8 vs. 82.2, p = 0.53, HR not given | 5-year: 6.3 vs. 5.8, p = 0.71, HR not given | No data | The use of HDRBT, which is not a widely accepted standard. |
| RAPIDO [4,8] 2021 | 912 | RT 5x5Gy + CAPOX or FOLFOX (18 weeks) | 50.4 Gy + Cape | No postoperative chemotherapy | d Optional; no postoperative chemotherapy or CAPOX/FOLFOX (24 weeks) | 4.6 | b 3-year: 23.7 vs. 30.4, p = 0.019, HR 0.75 (95% CI 0.60–0.93) | 3-year: 89.1 vs. 88.8, p = 0.59, HR 0.92 (95% CI 0.67–1.25) | 5-year: 10 vs. 7, p = 0.038, HR 1.60 (95% CI 1.02–2.49) | 2.4 (IQR 0.8–4.1) vs. 3.1 (IQR 1.4–6.6) years, HR 1.40 (95% CI 1.01–1.94), p = 0.04 | Short-course radiation was used in the TNT group and chemoradiation in the control group. |
| PRODIGE 23 [5] 2021 | 461 | FOLFIRINOX (12 weeks) + CRT: 50.4 Gy+Cape | 50.4 Gy + Cape | mFOLFOX or Cape (12 weeks) | mFOLFOX 12x or Cape 8x | 3.9 | 3-year: 75.7 vs. 68.5, p = 0.034, HR 0.69 (95%CI 0.49–0.97) | 3-year: 90.8 vs. 87.7, p = 0.077, HR 0.65 (95% CI 0.40–1.05) | 3-year: 4.3 vs. 5.7, p = 0.51, HR 0.65, 95% CI 0.40–1.05 | No data | Irinotecan was used only in the TNT group. |
| STELLAR [15] 2022 | 599 | RT 5x5 Gy + CAPOX (12 weeks) | 50 Gy + Cape | CAPOX (6 weeks) | CAPOX (18 weeks) | 2.9 | 3-year: 64.5 vs. 62.3, p = 0.883, HR 0.883 (95% CI NA–1.11) | 3-year: 86.5 vs. 75.1, p = 0.033, HR 0.67, (95% CI 0.46–0.97) | 3-year: 8.4 vs. 11, p = 0.46, HR 0.80 (95% CI 0.45–1.44) | No data | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Socha, J.; Bujko, K. Does the Gain of Total Neoadjuvant Therapy Outweigh the Harm in Rectal Cancer? Importance of the ATRESS (neoAdjuvant Therapy-RElated Shortening of Survival) Phenomenon: A Systematic Review. Cancers 2023, 15, 1016. https://doi.org/10.3390/cancers15041016
Socha J, Bujko K. Does the Gain of Total Neoadjuvant Therapy Outweigh the Harm in Rectal Cancer? Importance of the ATRESS (neoAdjuvant Therapy-RElated Shortening of Survival) Phenomenon: A Systematic Review. Cancers. 2023; 15(4):1016. https://doi.org/10.3390/cancers15041016
Chicago/Turabian StyleSocha, Joanna, and Krzysztof Bujko. 2023. "Does the Gain of Total Neoadjuvant Therapy Outweigh the Harm in Rectal Cancer? Importance of the ATRESS (neoAdjuvant Therapy-RElated Shortening of Survival) Phenomenon: A Systematic Review" Cancers 15, no. 4: 1016. https://doi.org/10.3390/cancers15041016
APA StyleSocha, J., & Bujko, K. (2023). Does the Gain of Total Neoadjuvant Therapy Outweigh the Harm in Rectal Cancer? Importance of the ATRESS (neoAdjuvant Therapy-RElated Shortening of Survival) Phenomenon: A Systematic Review. Cancers, 15(4), 1016. https://doi.org/10.3390/cancers15041016






