Genomic Prostate Score: A New Tool to Assess Prognosis and Optimize Radiation Therapy Volumes and ADT in Intermediate-Risk Prostate Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Biopsy and Tumor Selection Process
2.3. GPS Assay Description
2.4. Endpoints
3. Results
3.1. Patients’ Selection Process
3.2. Patients Characteristics
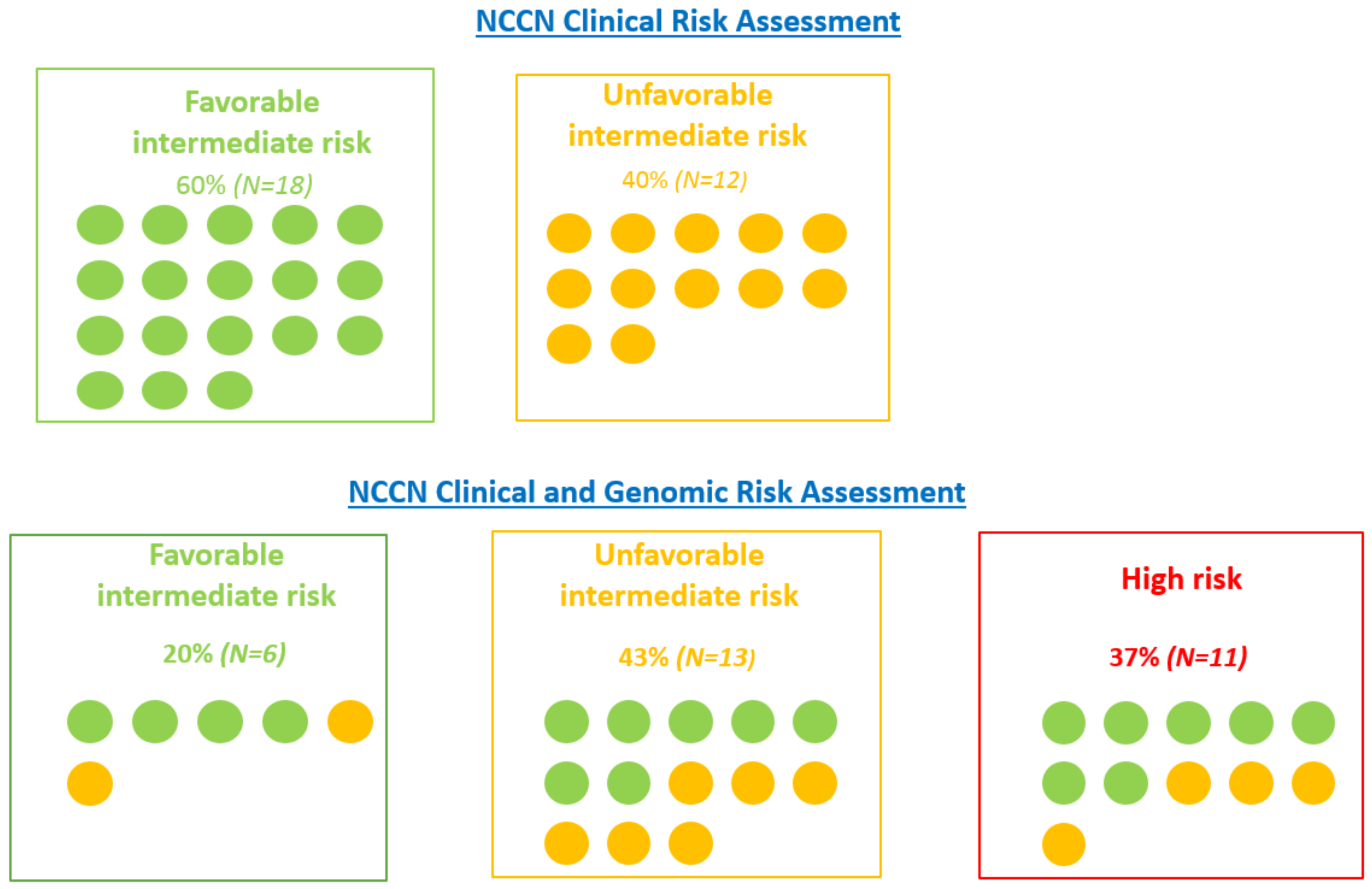
3.3. Risk Stratification
3.4. Correlation between GPS and Histological Features
3.5. GPS IMPACT on Therapeutic Decision Making and RT Volumes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Culp, M.B.; Soerjomataram, I.; Efstathiou, J.A.; Bray, F.; Jemal, A. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur. Urol. 2020, 77, 38–52. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, A.J.; Scardino, P.T.; Eastham, J.A.; Bianco, F.J.; Dotan, Z.A.; Fearn, P.A.; Kattan, M.W. Preoperative Nomogram Predicting the 10-Year Probability of Prostate Cancer Recurrence after Radical Prostatectomy. J. Natl. Cancer Inst. 2006, 98, 715–717. [Google Scholar] [CrossRef] [PubMed]
- Cooperberg, M.R.; Broering, J.M.; Carroll, P.R. Risk Assessment for Prostate Cancer Metastasis and Mortality at the Time of Diagnosis. J. Natl. Cancer Inst. 2009, 101, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Zumsteg, Z.S.; Zelefsky, M.J. Short-Term Androgen Deprivation Therapy for Patients with Intermediate-Risk Prostate Cancer Undergoing Dose-Escalated Radiotherapy: The Standard of Care? Lancet Oncol. 2012, 13, e259–e269. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, A.V.; Renshaw, A.A.; Cote, K.; Hurwitz, M.; Beard, C.; Loffredo, M.; Chen, M.-H. Impact of the Percentage of Positive Prostate Cores on Prostate Cancer-Specific Mortality for Patients with Low or Favorable Intermediate-Risk Disease. J. Clin. Oncol. 2004, 22, 3726–3732. [Google Scholar] [CrossRef] [PubMed]
- Feng, F.Y.; Qian, Y.; Stenmark, M.H.; Halverson, S.; Blas, K.; Vance, S.; Sandler, H.M.; Hamstra, D.A. Perineural Invasion Predicts Increased Recurrence, Metastasis, and Death from Prostate Cancer Following Treatment with Dose-Escalated Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, e361–e367. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, A.V.; Renshaw, A.A.; Sussman, B.; Chen, M.-H. Pretreatment PSA Velocity and Risk of Death from Prostate Cancer Following External Beam Radiation Therapy. JAMA 2005, 294, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Crocetto, F.; Russo, G.; Di Zazzo, E.; Pisapia, P.; Mirto, B.F.; Palmieri, A.; Pepe, F.; Bellevicine, C.; Russo, A.; La Civita, E.; et al. Liquid Biopsy in Prostate Cancer Management-Current Challenges and Future Perspectives. Cancers 2022, 14, 3272. [Google Scholar] [CrossRef] [PubMed]
- Spohn, S.K.B.; Draulans, C.; Kishan, A.U.; Spratt, D.; Ross, A.; Maurer, T.; Tilki, D.; Berlin, A.; Blanchard, P.; Collins, S.; et al. Genomic Classifiers in Personalized Prostate Cancer Radiotherapy Approaches—A Systematic Review and Future Perspectives Based on International Consensus. Int. J. Radiat. Oncol. Biol. Phys. 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Klein, E.A.; Cooperberg, M.R.; Magi-Galluzzi, C.; Simko, J.P.; Falzarano, S.M.; Maddala, T.; Chan, J.M.; Li, J.; Cowan, J.E.; Tsiatis, A.C.; et al. A 17-Gene Assay to Predict Prostate Cancer Aggressiveness in the Context of Gleason Grade Heterogeneity, Tumor Multifocality, and Biopsy Undersampling. Eur. Urol. 2014, 66, 550–560. [Google Scholar] [CrossRef] [PubMed]
- Van Den Eeden, S.K.; Lu, R.; Zhang, N.; Quesenberry, C.P.; Shan, J.; Han, J.S.; Tsiatis, A.C.; Leimpeter, A.D.; Lawrence, H.J.; Febbo, P.G.; et al. A Biopsy-Based 17-Gene Genomic Prostate Score as a Predictor of Metastases and Prostate Cancer Death in Surgically Treated Men with Clinically Localized Disease. Eur. Urol. 2018, 73, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Eggener, S.E.; Rumble, R.B.; Armstrong, A.J.; Morgan, T.M.; Crispino, T.; Cornford, P.; van der Kwast, T.; Grignon, D.J.; Rai, A.J.; Agarwal, N.; et al. Molecular Biomarkers in Localized Prostate Cancer: ASCO Guideline. J. Clin. Oncol. 2020, 38, 1474–1494. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.L.; Huang, H.-C.R.; Spratt, D.E.; Davicioni, E.; Sandler, H.M.; Shipley, W.U.; Efstathiou, J.A.; Simko, J.P.; Pollack, A.; Dicker, A.P.; et al. Analysis of a Biopsy-Based Genomic Classifier in High-Risk Prostate Cancer: Meta-Analysis of the NRG Oncology/RTOG 9202, 9413, and 9902 Phase III Randomized Trials. Int. J. Radiat. Oncol. Biol. Phys. 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Berlin, A.; Murgic, J.; Hosni, A.; Pintilie, M.; Salcedo, A.; Fraser, M.; Kamel-Reid, S.; Zhang, J.; Wang, Q.; Ch’ng, C.; et al. Genomic Classifier for Guiding Treatment of Intermediate-Risk Prostate Cancers to Dose-Escalated Image Guided Radiation Therapy Without Hormone Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Cullen, J.; Kuo, H.-C.; Shan, J.; Lu, R.; Aboushwareb, T.; Van Den Eeden, S.K. The 17-Gene Genomic Prostate Score Test as a Predictor of Outcomes in Men with Unfavorable Intermediate Risk Prostate Cancer. Urology 2020, 143, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Janes, J.L.; Boyer, M.J.; Bennett, J.P.; Thomas, V.M.; De Hoedt, A.M.; Edwards, V.D.K.; Singla, P.K.; Abran, J.M.; Aboushwareb, T.; Salama, J.K.; et al. The 17-Gene Genomic Prostate Score Test Is Prognostic for Outcomes After Primary External Beam Radiation Therapy in Men With Clinically Localized Prostate Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2023, 115, 120–131. [Google Scholar] [CrossRef] [PubMed]
- Zapatero, A.; Guerrero, A.; Maldonado, X.; Alvarez, A.; Gonzalez San Segundo, C.; Cabeza Rodríguez, M.A.; Macias, V.; Pedro Olive, A.; Casas, F.; Boladeras, A.; et al. High-Dose Radiotherapy with Short-Term or Long-Term Androgen Deprivation in Localised Prostate Cancer (DART01/05 GICOR): A Randomised, Controlled, Phase 3 Trial. Lancet Oncol. 2015, 16, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Murthy, V.; Maitre, P.; Kannan, S.; Panigrahi, G.; Krishnatry, R.; Bakshi, G.; Prakash, G.; Pal, M.; Menon, S.; Phurailatpam, R.; et al. Prostate-Only Versus Whole-Pelvic Radiation Therapy in High-Risk and Very High-Risk Prostate Cancer (POP-RT): Outcomes From Phase III Randomized Controlled Trial. J. Clin. Oncol. 2021, 39, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N = 30 | % |
|---|---|---|
| Age (years) | ||
| Median (range) | 70 (45–79) | - |
| PSA (ng/mL) | ||
| Median (range) | 7 (0.9–16) | - |
| Clinical T Stage | ||
| T1 | 23 | 77 |
| T2 | 7 | 23 |
| Prostate Volume (mL) | ||
| Median (range) | 40 (15–75) | - |
| Number of Positive Cores | ||
| Median (range) | 7.5 (1–17) | - |
| Number of Cores Sampled | ||
| Median (range) | 18 (18–22) | - |
| Positive Cores/Cores Sampled Ratio | ||
| <50% | 18 | 60 |
| ≥50% | 12 | 40 |
| NCCN Risk Group | ||
| Intermediate favorable | 18 | 60 |
| Intermediate unfavorable | 12 | 40 |
| Upfront Treatment | ||
| Surgery | 23 | 77 |
| Radiation therapy | 7 | 23 |
| Patient Number | NCCN Clinical Risk Group | Decision Radiation + Hormonal Therapy (Based on Clinical Factors) | GPS | NCCN + GPS Risk Group | Estimated Metastatic Risk at 10 Years (%) Based on GPS Validation Studies | Estimated Prostate Cancer Death at 10 Years (%) Based on GPS Validation Studies | Decision Radiation Based on NCCN + GPS | Impact of GPS |
|---|---|---|---|---|---|---|---|---|
| 1 | Unfavorable intermediate | RT prostate alone with ADT (short term) | 17 | Favorable intermediate | 4 | 1 | RT prostate alone without ADT | De-escalation |
| 2 | Favorable intermediate | RT prostate alone with ADT (short term) | 53 | High | 17 | 3 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 3 | Favorable intermediate | RT prostate alone without ADT | 33 | Unfavorable intermediate | 7 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 4 | Unfavorable intermediate | RT prostate alone without ADT | 37 | Unfavorable intermediate | 9 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 5 | Unfavorable intermediate | RT prostate alone without ADT | 19 | Favorable intermediate | 4 | 1 | RT prostate alone without ADT | No change |
| 6 | Favorable intermediate | RT prostate alone with ADT (short term) | 39 | Unfavorable intermediate | 10 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 7 | Favorable intermediate | RT prostate alone without ADT | 40 | Unfavorable intermediate | 10 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 8 | Favorable intermediate | RT prostate alone without ADT | 30 | Unfavorable intermediate | 7 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 9 | Favorable intermediate | RT prostate alone without ADT | 46 | High | 13 | 2 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 10 | Favorable intermediate | RT prostate alone without ADT | 70 | High | 23 | 4 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 11 | Unfavorable intermediate | RT prostate alone without ADT | 25 | Unfavorable intermediate | 5 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 12 | Favorable intermediate | RT prostate alone without ADT | 47 | High | 13 | 2 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 13 | Favorable intermediate | RT prostate alone without ADT | 36 | Unfavorable intermediate | 8 | 1 | RT prostate alone without ADT | Intensification |
| 14 | Unfavorable intermediate | RT prostate alone with ADT (short term) | 39 | Unfavorable intermediate | 10 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 15 | Unfavorable intermediate | RT prostate alone without ADT | 42 | High | 11 | 1 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 16 | Favorable intermediate | RT prostate alone without ADT | 19 | Favorable intermediate | 4 | 1 | RT prostate alone without ADT | No change |
| 17 | Favorable intermediate | RT prostate alone without ADT | 18 | Favorable intermediate | 4 | 1 | RT prostate alone without ADT | No change |
| 18 | Favorable intermediate | RT prostate alone without ADT | 18 | Favorable intermediate | 4 | 1 | RT prostate alone without ADT | No change |
| 19 | Unfavorable intermediate | RT prostate alone without ADT | 40 | Unfavorable intermediate | 10 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 20 | Favorable intermediate | RT prostate alone without ADT | 56 | High | 19 | 3 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 21 | Favorable intermediate | RT prostate alone without ADT | 26 | Unfavorable intermediate | 6 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 22 | Unfavorable intermediate | RT prostate alone without ADT | 20 | Unfavorable intermediate | 4 | 1 | RT prostate alone with ADT (short term) | Intensification |
| 23 | Favorable intermediate | RT prostate alone without ADT | 18 | Favorable intermediate | 4 | 1 | RT prostate alone without ADT | no change |
| 24 | Favorable intermediate | RT prostate alone without ADT | 34 | Unfavorable intermediate | 8 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | Intensification |
| 25 | Unfavorable intermediate | RT prostate alone with ADT (short term) | 43 | High | 11 | 1 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 26 | Unfavorable intermediate | RT prostate alone without ADT | 58 | High | 20 | 3 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 27 | Favorable intermediate | RT prostate alone without ADT | 47 | High | 12 | 2 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 28 | Unfavorable intermediate | RT prostate alone with ADT (short term) | 55 | High | 18 | 3 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 29 | Favorable intermediate | RT prostate alone without ADT | 53 | High | 17 | 3 | RT of the pelvic nodes and the prostate with ADT (long term) | Intensification |
| 30 | Unfavorable intermediate | RT of the pelvic nodes and the prostate with ADT (short term) | 39 | Unfavorable intermediate | 10 | 1 | RT of the pelvic nodes and the prostate with ADT (short term) | No change |
| Trial Name | Full Name of Trial | Common Name | Phase | Participants (Number) | Status (July 2022) |
|---|---|---|---|---|---|
| NRG GU009 NCT04513717 | Two studies for patients with high-risk prostate cancer testing less intense treatment for patients with a low gene risk score and testing a more intense treatment with a high gene risk score. | PREDICT-RT | III | 2478 | Recruiting |
| NRG GU010 NCT05050084 | Two studies for patients with unfavorable intermediate-risk prostate cancer testing less intense treatment for patients with a low gene risk score and testing a more intense treatment with a high gene risk score. | GUIDANCE | III | 2050 | Recruiting |
| NCT04396808 | Genomics in Michigan to adjust outcomes in prostate cancer for men with newly diagnosed favorable-risk prostate cancer. | G-MAJOR | III | 350 | Recruiting |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belkacemi, Y.; Debbi, K.; Coraggio, G.; Bendavid, J.; Nourieh, M.; To, N.H.; Cherif, M.A.; Saldana, C.; Ingels, A.; De La Taille, A.; et al. Genomic Prostate Score: A New Tool to Assess Prognosis and Optimize Radiation Therapy Volumes and ADT in Intermediate-Risk Prostate Cancer. Cancers 2023, 15, 945. https://doi.org/10.3390/cancers15030945
Belkacemi Y, Debbi K, Coraggio G, Bendavid J, Nourieh M, To NH, Cherif MA, Saldana C, Ingels A, De La Taille A, et al. Genomic Prostate Score: A New Tool to Assess Prognosis and Optimize Radiation Therapy Volumes and ADT in Intermediate-Risk Prostate Cancer. Cancers. 2023; 15(3):945. https://doi.org/10.3390/cancers15030945
Chicago/Turabian StyleBelkacemi, Yazid, Kamel Debbi, Gabriele Coraggio, Jérome Bendavid, Maya Nourieh, Nhu Hanh To, Mohamed Aziz Cherif, Carolina Saldana, Alexandre Ingels, Alexandre De La Taille, and et al. 2023. "Genomic Prostate Score: A New Tool to Assess Prognosis and Optimize Radiation Therapy Volumes and ADT in Intermediate-Risk Prostate Cancer" Cancers 15, no. 3: 945. https://doi.org/10.3390/cancers15030945
APA StyleBelkacemi, Y., Debbi, K., Coraggio, G., Bendavid, J., Nourieh, M., To, N. H., Cherif, M. A., Saldana, C., Ingels, A., De La Taille, A., & Loganadane, G. (2023). Genomic Prostate Score: A New Tool to Assess Prognosis and Optimize Radiation Therapy Volumes and ADT in Intermediate-Risk Prostate Cancer. Cancers, 15(3), 945. https://doi.org/10.3390/cancers15030945






