AI-Based Risk Score from Tumour-Infiltrating Lymphocyte Predicts Locoregional-Free Survival in Nasopharyngeal Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Clinicopathological Features
2.3. Tumour Nuclei Detection and Clustering
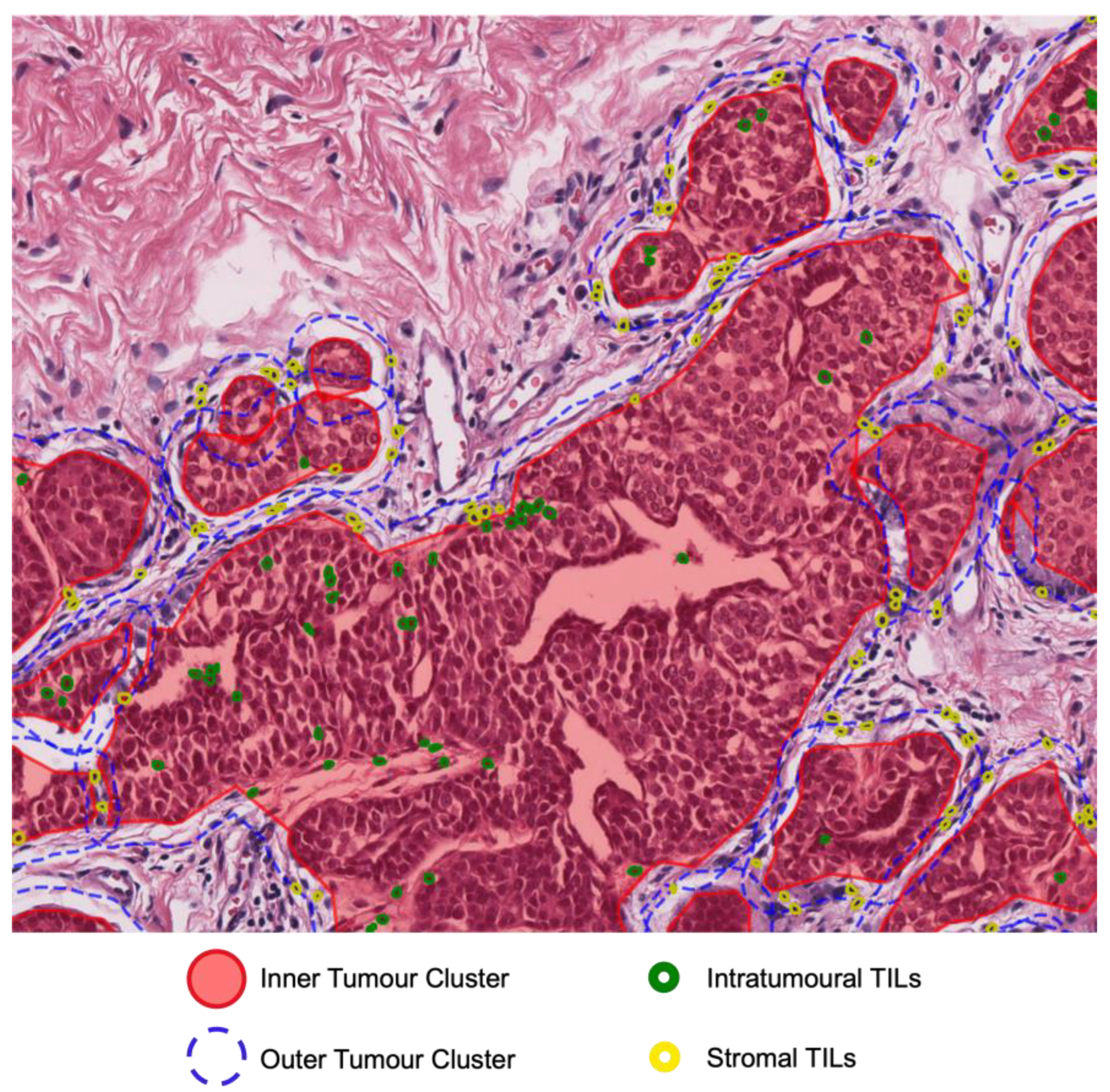
2.4. Digital TILs and Tumour Morphology
2.5. Survival Analysis
3. Results
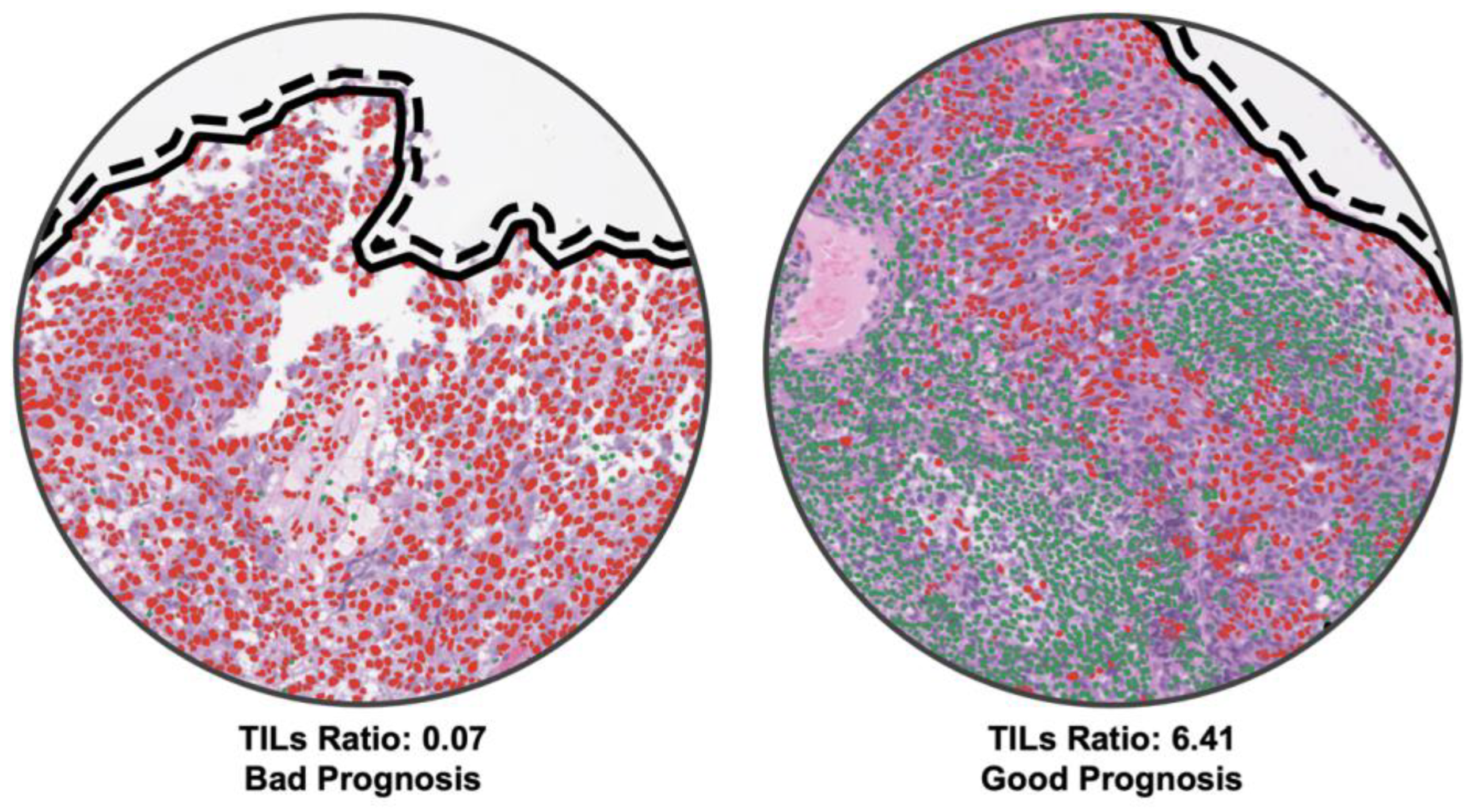
3.1. Patient Stratification with Risk Score of Digital NPC-TILs
3.2. Correlation Analysis of Predicted Risk Scores and Time to Event
3.3. Univariate and Multivariate Analyses
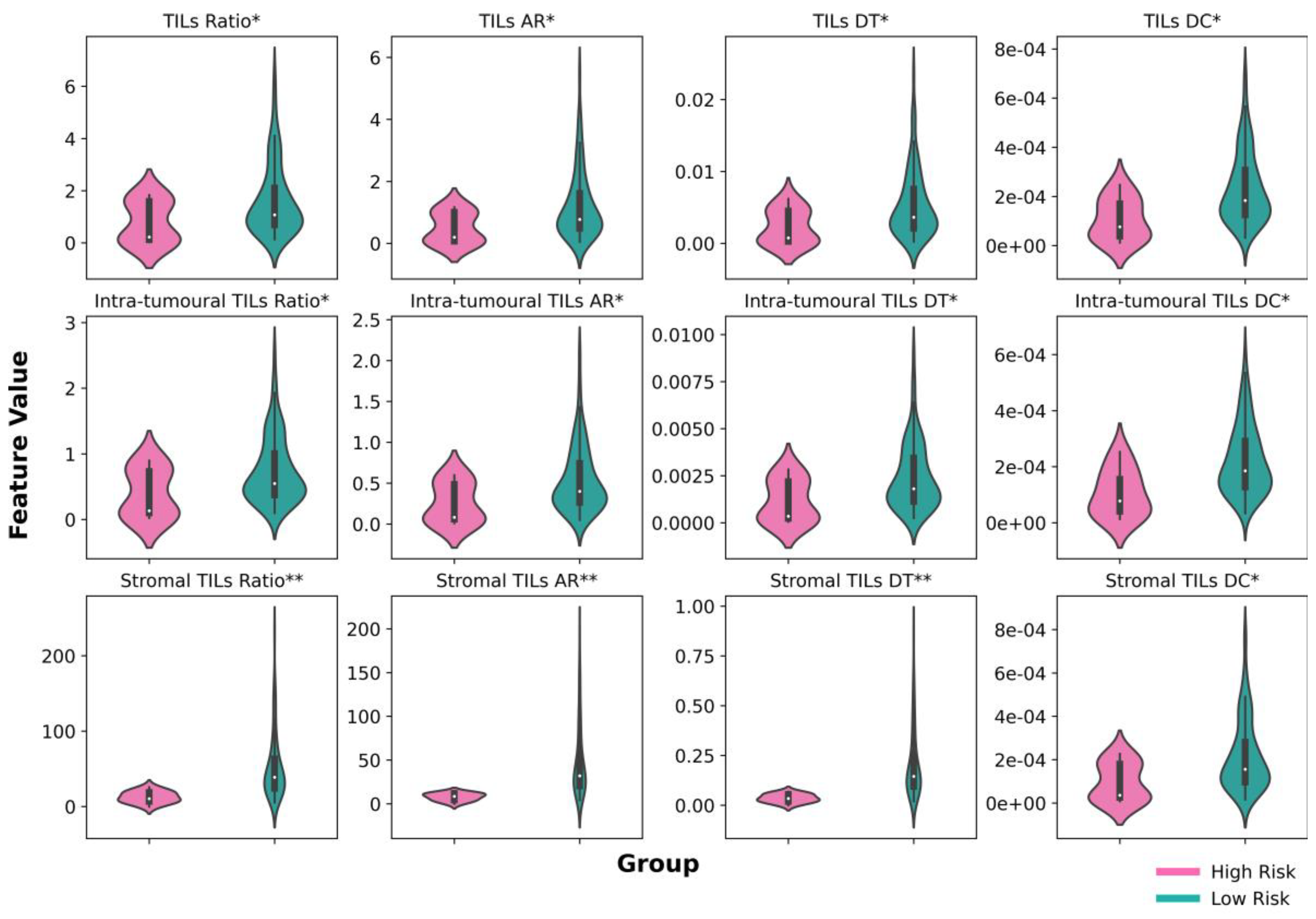
3.4. Digital NPC-TIL Scores in Low-Risk and High-Risk Groups
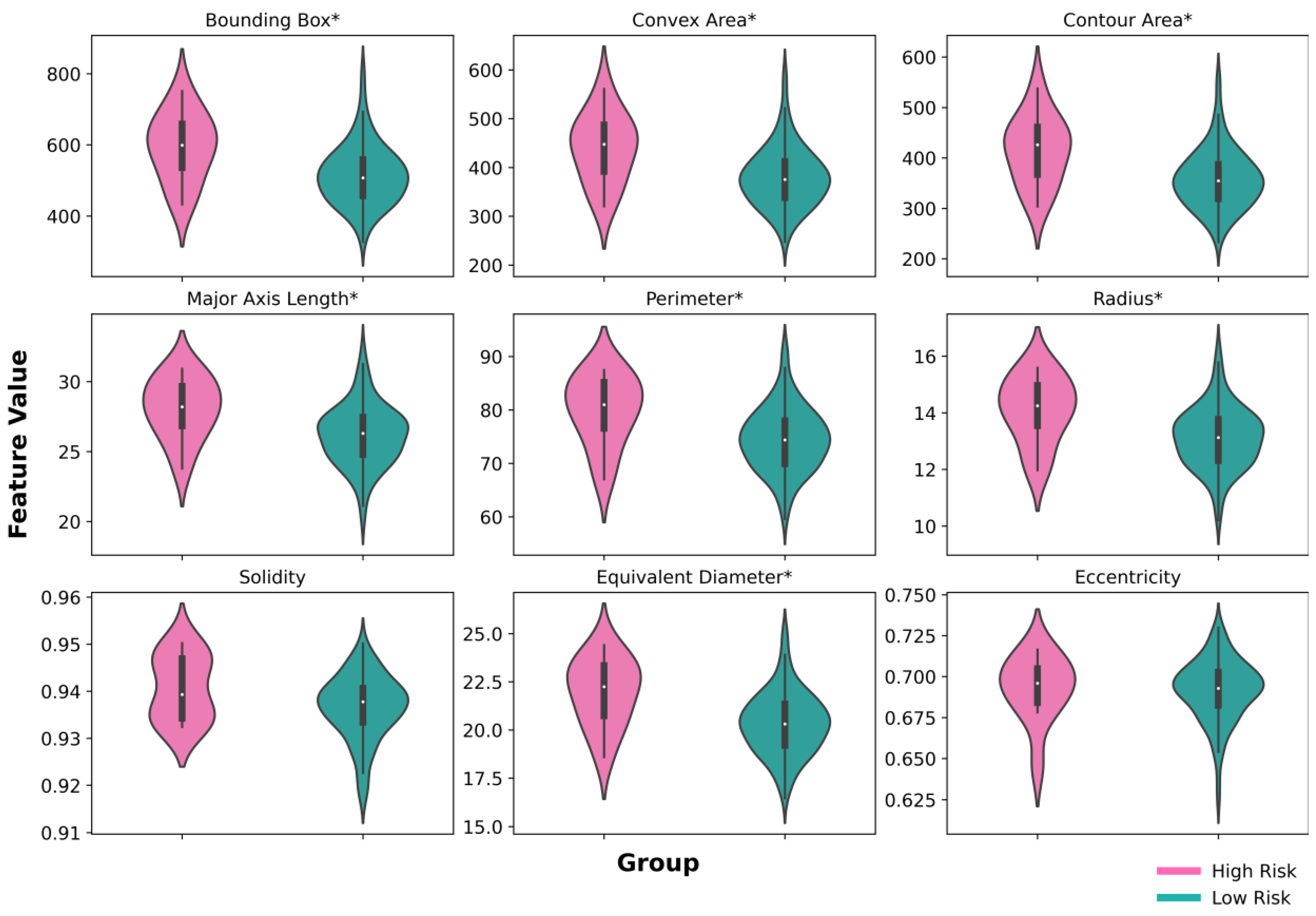
3.5. Tumour Nuclear Morphology Analysis
3.6. Model Interpretability Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Young, L.S.; Dawson, C.W.; Woodman, C.B.J.; Rabkin, C.S.; Lo, K.W. Human Herpesviruses: Nasopharyngeal Carcinoma and Other Epithelial Tumors. In Viral Infections of Humans; Kaslow, R.A., Stanberry, L.R., Powers, A.M., Eds.; Springer: New York, NY, USA, 2022; pp. 1–40. ISBN 978-1-4939-9544-8. [Google Scholar]
- Chen, Y.-P.; Chan, A.T.C.; Le, Q.-T.; Blanchard, P.; Sun, Y.; Ma, J. Nasopharyngeal Carcinoma. Lancet 2019, 394, 64–80. [Google Scholar] [CrossRef]
- Rickinson, A.B.; Lo, K.W. Nasopharyngeal Carcinoma. In Nasopharyngeal Carcinoma; Elsevier: Amsterdam, The Netherlands, 2019; pp. 1–16. ISBN 978-0-12-814936-2. [Google Scholar]
- Wong, K.C.W.; Hui, E.P.; Lo, K.-W.; Lam, W.K.J.; Johnson, D.; Li, L.; Tao, Q.; Chan, K.C.A.; To, K.-F.; King, A.D.; et al. Nasopharyngeal Carcinoma: An Evolving Paradigm. Nat. Rev. Clin. Oncol. 2021, 18, 679–695. [Google Scholar] [CrossRef]
- Chan, A.T.C. Nasopharyngeal Carcinoma. Ann. Oncol. 2010, 21, vii308–vii312. [Google Scholar] [CrossRef]
- Wibawa, M.S.; Lo, K.-W.; Young, L.S.; Rajpoot, N. Multi-Scale Attention-Based Multiple Instance Learning for Classification of Multi-Gigapixel Histology Images. In Computer Vision—ECCV 2022 Workshops; Karlinsky, L., Michaeli, T., Nishino, K., Eds.; Lecture Notes in Computer Science; Springer Nature Switzerland: Cham, Switzerland, 2023; Volume 13807, pp. 635–647. ISBN 978-3-031-25081-1. [Google Scholar]
- Poh, S.S.; Soong, Y.L.; Sommat, K.; Lim, C.M.; Fong, K.W.; Tan, T.W.; Chua, M.L.; Wang, F.Q.; Hu, J.; Wee, J.T. Retreatment in Locally Recurrent Nasopharyngeal Carcinoma: Current Status and Perspectives. Cancer Commun. 2021, 41, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Chen, Q.Y.; Liu, H.; Tang, L.Q.; Mai, H.Q. Emerging Treatment Options for Nasopharyngeal Carcinoma. Drug Des. Dev. Ther. 2013, 7, 37–52. [Google Scholar] [CrossRef]
- Newton, E.; Valenzuela, D.; Foley, J.; Thamboo, A.; Prisman, E. Outcomes for the Treatment of Locoregional Recurrent Nasopharyngeal Cancer: Systematic Review and Pooled Analysis. Head Neck 2021, 43, 3979–3995. [Google Scholar] [CrossRef] [PubMed]
- Au, K.H.; Ngan, R.K.C.; Ng, A.W.Y.; Poon, D.M.C.; Ng, W.T.; Yuen, K.T.; Lee, V.H.F.; Tung, S.Y.; Chan, A.T.C.; Sze, H.C.K.; et al. Treatment Outcomes of Nasopharyngeal Carcinoma in Modern Era after Intensity Modulated Radiotherapy (IMRT) in Hong Kong: A Report of 3328 Patients (HKNPCSG 1301 Study). Oral Oncol. 2018, 77, 16–21. [Google Scholar] [CrossRef]
- Chen, M.-Y.; Jiang, R.; Guo, L.; Zou, X.; Liu, Q.; Sun, R.; Qiu, F.; Xia, Z.-J.; Huang, H.-Q.; Zhang, L.; et al. Locoregional Radiotherapy in Patients with Distant Metastases of Nasopharyngeal Carcinoma at Diagnosis. Chin. J. Cancer 2013, 32, 604–613. [Google Scholar] [CrossRef]
- Liu, K.; Xia, W.; Qiang, M.; Chen, X.; Liu, J.; Guo, X.; Lv, X. Deep Learning Pathological Microscopic Features in Endemic Nasopharyngeal Cancer: Prognostic Value and Protentional Role for Individual Induction Chemotherapy. Cancer Med. 2020, 9, 1298–1306. [Google Scholar] [CrossRef]
- Lin, J.-C.; Chen, K.Y.; Wang, W.-Y.; Jan, J.-S.; Liang, W.-M.; Tsai, C.-S.; Wei, Y.-H. Detection of Epstein-Barr Virus DNA in the Peripheral-Blood Cells of Patients With Nasopharyngeal Carcinoma: Relationship to Distant Metastasis and Survival. J. Clin. Oncol. 2016, 19, 2607–2615. [Google Scholar] [CrossRef]
- Chan, A.T.C.; Hui, E.P.; Ngan, R.K.C.; Tung, S.Y.; Cheng, A.C.K.; Ng, W.T.; Lee, V.H.F.; Ma, B.B.Y.; Cheng, H.C.; Wong, F.C.S.; et al. Analysis of Plasma Epstein-Barr Virus DNA in Nasopharyngeal Cancer after Chemoradiation to Identify High-Risk Patients for Adjuvant Chemotherapy: A Randomized Controlled Trial. JCO 2018, 36, 3091–3100. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.W.M.; Lung, M.L.; Ng, W.T. (Eds.) Nasopharyngeal Carcinoma: From Etiology to Clinical Practice; Academic Press, an imprint of Elsevier: London, UK; San Diego, CA, USA, 2019; ISBN 978-0-12-814936-2. [Google Scholar]
- Wei, W.I.; Yuen, A.P.W.; Ng, R.W.M.; Ho, W.K.; Kwong, D.L.W.; Sham, J.S.T. Quantitative Analysis of Plasma Cell-Free Epstein-Barr Virus DNA in Nasopharyngeal Carcinoma after Salvage Nasopharyngectomy: A Prospective Study. Head Neck 2004, 26, 878–883. [Google Scholar] [CrossRef]
- Forder, A.; Stewart, G.L.; Telkar, N.; Lam, W.L.; Garnis, C. New Insights into the Tumour Immune Microenvironment of Nasopharyngeal Carcinoma. Curr. Res. Immunol. 2022, 3, 222–227. [Google Scholar] [CrossRef]
- Almangush, A.; Ruuskanen, M.; Hagström, J.; Hirvikoski, P.; Tommola, S.; Kosma, V.-M.; Nieminen, P.; Mäkitie, A.; Leivo, I. Tumor-Infiltrating Lymphocytes Associate with Outcome in Nonendemic Nasopharyngeal Carcinoma: A Multicenter Study. Hum. Pathol. 2018, 81, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Lv, S.-H.; Li, W.-Z.; Liang, H.; Liu, G.-Y.; Xia, W.-X.; Xiang, Y.-Q. Prognostic and Predictive Value of Circulating Inflammation Signature in Non-Metastatic Nasopharyngeal Carcinoma: Potential Role for Individualized Induction Chemotherapy. JIR 2021, 14, 2225–2237. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-Q.; Chen, Y.-P.; Zhang, Y.; Jiang, W.; Liu, N.; Yun, J.-P.; Sun, Y.; He, Q.-M.; Tang, X.-R.; Wen, X.; et al. Prognostic Significance of Tumor-Infiltrating Lymphocytes in Nondisseminated Nasopharyngeal Carcinoma: A Large-Scale Cohort Study: Prognostic Significance of TILs in Nondisseminated NPC. Int. J. Cancer 2018, 142, 2558–2566. [Google Scholar] [CrossRef] [PubMed]
- Ooft, M.L.; Van Ipenburg, J.A.; Braunius, W.W.; Zuur, C.I.; Koljenović, S.; Willems, S.M. Prognostic Role of Tumor Infiltrating Lymphocytes in EBV Positive and EBV Negative Nasopharyngeal Carcinoma. Oral Oncol. 2017, 71, 16–25. [Google Scholar] [CrossRef]
- Nilsson, J.S.; Sobti, A.; Swoboda, S.; Erjefält, J.S.; Forslund, O.; Lindstedt, M.; Greiff, L. Immune Phenotypes of Nasopharyngeal Cancer. Cancers 2020, 12, 3428. [Google Scholar] [CrossRef]
- Liu, W.; Chen, G.; Zhang, C.; Liao, X.; Xie, J.; Liang, T.; Liao, W.; Song, L.; Zhang, X. Prognostic Significance of Tumor-Infiltrating Lymphocytes and Macrophages in Nasopharyngeal Carcinoma: A Systematic Review and Meta-Analysis. Eur. Arch. Otorhinolaryngol. 2022, 279, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Song, A.H.; Jaume, G.; Williamson, D.F.K.; Lu, M.Y.; Vaidya, A.; Miller, T.R.; Mahmood, F. Artificial Intelligence for Digital and Computational Pathology. Nat. Rev. Bioeng. 2023, 1, 930–949. [Google Scholar] [CrossRef]
- Ng, W.T.; But, B.; Choi, H.C.; De Bree, R.; Lee, A.W.; Lee, V.H.; López, F.; Mäkitie, A.A.; Rodrigo, J.P.; Saba, N.F.; et al. Application of Artificial Intelligence for Nasopharyngeal Carcinoma Management—A Systematic Review. CMAR 2022, 14, 339–366. [Google Scholar] [CrossRef]
- Bibault, J.-E.; Burgun, A.; Fournier, L.; Dekker, A.; Lambin, P. Artificial Intelligence in Oncology. In Artificial Intelligence in Medicine; Elsevier: Amsterdam, The Netherlands, 2021; pp. 361–381. ISBN 978-0-12-821259-2. [Google Scholar]
- Abels, E.; Pantanowitz, L.; Aeffner, F.; Zarella, M.D.; Laak, J.; Bui, M.M.; Vemuri, V.N.; Parwani, A.V.; Gibbs, J.; Agosto-Arroyo, E.; et al. Computational Pathology Definitions, Best Practices, and Recommendations for Regulatory Guidance: A White Paper from the Digital Pathology Association. J. Pathol. 2019, 249, 286–294. [Google Scholar] [CrossRef]
- Li, C.; Jing, B.; Ke, L.; Li, B.; Xia, W.; He, C.; Qian, C.; Zhao, C.; Mai, H.; Chen, M.; et al. Development and Validation of an Endoscopic Images-Based Deep Learning Model for Detection with Nasopharyngeal Malignancies. Cancer Commun. 2018, 38, 59. [Google Scholar] [CrossRef] [PubMed]
- Diao, S.; Hou, J.; Yu, H.; Zhao, X.; Sun, Y.; Lambo, R.L.; Xie, Y.; Liu, L.; Qin, W.; Luo, W. Computer-Aided Pathologic Diagnosis of Nasopharyngeal Carcinoma Based on Deep Learning. Am. J. Pathol. 2020, 190, 1691–1700. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Zhong, L.-Z.; Zhao, X.; Dong, D.; Yao, J.-J.; Wang, S.-Y.; Liu, Y.; Zhu, D.; Wang, Y.; Wang, G.-J.; et al. A Deep-Learning-Based Prognostic Nomogram Integrating Microscopic Digital Pathology and Macroscopic Magnetic Resonance Images in Nasopharyngeal Carcinoma: A Multi-Cohort Study. Ther. Adv. Med. Oncol. 2020, 12, 175883592097141. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Guo, Y.; Ou, X.; Wang, J.; Hu, C. Automatic T Staging Using Weakly Supervised Deep Learning for Nasopharyngeal Carcinoma on MR Images. J. Magn. Reson. Imaging 2020, 52, 1074–1082. [Google Scholar] [CrossRef]
- Peng, H.; Dong, D.; Fang, M.-J.; Li, L.; Tang, L.-L.; Chen, L.; Li, W.-F.; Mao, Y.-P.; Fan, W.; Liu, L.-Z.; et al. Prognostic Value of Deep Learning PET/CT-Based Radiomics: Potential Role for Future Individual Induction Chemotherapy in Advanced Nasopharyngeal Carcinoma. Clin. Cancer Res. 2019, 25, 4271–4279. [Google Scholar] [CrossRef] [PubMed]
- Jing, B.; Zhang, T.; Wang, Z.; Jin, Y.; Liu, K.; Qiu, W.; Ke, L.; Sun, Y.; He, C.; Hou, D.; et al. A Deep Survival Analysis Method Based on Ranking. Artif. Intell. Med. 2019, 98, 1–9. [Google Scholar] [CrossRef] [PubMed]
- An, X.; Wang, F.-H.; Ding, P.-R.; Deng, L.; Jiang, W.-Q.; Zhang, L.; Shao, J.-Y.; Li, Y.-H. Plasma Epstein-Barr Virus DNA Level Strongly Predicts Survival in Metastatic/Recurrent Nasopharyngeal Carcinoma Treated with Palliative Chemotherapy. Cancer 2011, 117, 3750–3757. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.-L.; Guo, R.; Zhang, N.; Deng, B.; Chen, L.; Cheng, Z.-B.; Huang, J.; Hu, W.-H.; Huang, S.H.; Luo, W.-J.; et al. Effect of Radiotherapy Alone vs. Radiotherapy with Concurrent Chemoradiotherapy on Survival without Disease Relapse in Patients with Low-Risk Nasopharyngeal Carcinoma: A Randomized Clinical Trial. JAMA 2022, 328, 728–736. [Google Scholar] [CrossRef]
- Li, X.-Y.; Luo, D.-H.; Guo, L.; Mo, H.-Y.; Sun, R.; Guo, S.-S.; Liu, L.-T.; Yang, Z.-C.; Yang, J.-H.; Qiu, F.; et al. Deintensified Chemoradiotherapy for Pretreatment Epstein-Barr Virus DNA-Selected Low-Risk Locoregionally Advanced Nasopharyngeal Carcinoma: A Phase II Randomized Noninferiority Trial. JCO 2022, 40, 1163–1173. [Google Scholar] [CrossRef]
- Graham, S.; Vu, Q.D.; Raza, S.E.A.; Azam, A.; Tsang, Y.W.; Kwak, J.T.; Rajpoot, N. Hover-Net: Simultaneous Segmentation and Classification of Nuclei in Multi-Tissue Histology Images. Med. Image Anal. 2019, 58, 101563. [Google Scholar] [CrossRef] [PubMed]
- Gamper, J.; Alemi Koohbanani, N.; Benet, K.; Khuram, A.; Rajpoot, N. PanNuke: An Open Pan-Cancer Histology Dataset for Nuclei Instance Segmentation and Classification. In Digital Pathology; Reyes-Aldasoro, C.C., Janowczyk, A., Veta, M., Bankhead, P., Sirinukunwattana, K., Eds.; Lecture Notes in Computer Science; Springer International Publishing: Cham, Switzerland, 2019; Volume 11435, pp. 11–19. ISBN 978-3-030-23936-7. [Google Scholar]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep Residual Learning for Image Recognition. In Proceedings of the 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Las Vegas, NV, USA, 27–30 June 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 770–778. [Google Scholar]
- Deng, J.; Dong, W.; Socher, R.; Li, L.J.; Li, K.; Fei-Fei, L. ImageNet: A Large-Scale Hierarchical Image Database. In Proceedings of the 2009 IEEE Conference on Computer Vision and Pattern Recognition, Miami, FL, USA, 20–25 June 2009; IEEE: Piscataway, NJ, USA, 2009; pp. 248–255. [Google Scholar]
- Kim, H.E.; Cosa-Linan, A.; Santhanam, N.; Jannesari, M.; Maros, M.E.; Ganslandt, T. Transfer Learning for Medical Image Classification: A Literature Review. BMC Med. Imaging 2022, 22, 69. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Yang, D.M.; Rong, R.; Zhan, X.; Xiao, G. Pathology Image Analysis Using Segmentation Deep Learning Algorithms. Am. J. Pathol. 2019, 189, 1686–1698. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Kumar, N.; Patil, A.; Kurian, N.C.; Rane, S.; Graham, S.; Vu, Q.D.; Zwager, M.; Raza, S.E.A.; Rajpoot, N.; et al. MoNuSAC2020: A Multi-Organ Nuclei Segmentation and Classification Challenge. IEEE Trans. Med. Imaging 2021, 40, 3413–3423. [Google Scholar] [CrossRef] [PubMed]
- Macenko, M.; Niethammer, M.; Marron, J.S.; Borland, D.; Woosley, J.T.; Guan, X.; Schmitt, C.; Thomas, N.E. A Method for Normalizing Histology Slides for Quantitative Analysis. In Proceedings of the 2009 IEEE International Symposium on Biomedical Imaging: From Nano to Macro, Boston, MA, USA, 28 June–1 July 2009; pp. 1107–1110. [Google Scholar]
- Schubert, E.; Sander, J.; Ester, M.; Kriegel, H.P.; Xu, X. DBSCAN Revisited, Revisited: Why and How You Should (Still) Use DBSCAN. ACM Trans. Database Syst. 2017, 42, 1–21. [Google Scholar] [CrossRef]
- Harrell, F.E., Jr.; Lee, K.L.; Mark, D.B. Multivariable Prognostic Models: Issues in Developing Models, Evaluating Assumptions and Adequacy, and Measuring and Reducing Errors. Stat. Med. 1996, 15, 361–387. [Google Scholar] [CrossRef]
- Fotso, S. Others PySurvival: Open Source Package for Survival Analysis Modeling. 2019. Available online: http://www.pysurvival.io/ (accessed on 3 April 2023).
- Steck, H.; Krishnapuram, B.; Dehing-oberije, C.; Lambin, P.; Raykar, V.C. On Ranking in Survival Analysis: Bounds on the Concordance Index. Adv. Neural Inf. Process. Syst. 2007, 20, 1–8. [Google Scholar]
- Budczies, J.; Klauschen, F.; Sinn, B.V.; Győrffy, B.; Schmitt, W.D.; Darb-Esfahani, S.; Denkert, C. Cutoff Finder: A Comprehensive and Straightforward Web Application Enabling Rapid Biomarker Cutoff Optimization. PLoS ONE 2012, 7, e51862. [Google Scholar] [CrossRef]
- Luo, W. Nasopharyngeal Carcinoma Ecology Theory: Cancer as Multidimensional Spatiotemporal “Unity of Ecology and Evolution” Pathological Ecosystem. Theranostics 2023, 13, 1607–1631. [Google Scholar] [CrossRef]
- Wang, H.-Y.; Sun, B.-Y.; Zhu, Z.-H.; Chang, E.T.; To, K.-F.; Hwang, J.S.G.; Jiang, H.; Kam, M.K.-M.; Chen, G.; Cheah, S.-L.; et al. Eight-Signature Classifier for Prediction of Nasopharyngeal Carcinoma Survival. JCO 2011, 29, 4516–4525. [Google Scholar] [CrossRef]
- Zhou, J.; Deng, Y.; Huang, Y.; Wang, Z.; Zhan, Z.; Cao, X.; Cai, Z.; Deng, Y.; Zhang, L.; Huang, H.; et al. An Individualized Prognostic Model in Patients with Locoregionally Advanced Nasopharyngeal Carcinoma Based on Serum Metabolomic Profiling. Life 2023, 13, 1167. [Google Scholar] [CrossRef] [PubMed]
- Sobti, A.; Sakellariou, C.; Nilsson, J.S.; Askmyr, D.; Greiff, L.; Lindstedt, M. Exploring Spatial Heterogeneity of Immune Cells in Nasopharyngeal Cancer. Cancers 2023, 15, 2165. [Google Scholar] [CrossRef] [PubMed]
- Niazi, M.K.K.; Parwani, A.V.; Gurcan, M.N. Digital Pathology and Artificial Intelligence. Lancet Oncol. 2019, 20, e253–e261. [Google Scholar] [CrossRef] [PubMed]
- Chua, M.L.K.; Wee, J.T.S.; Hui, E.P.; Chan, A.T.C. Nasopharyngeal Carcinoma. Lancet 2016, 387, 1012–1024. [Google Scholar] [CrossRef]
- Young, L.S.; Yap, L.F.; Murray, P.G. Epstein–Barr Virus: More than 50 Years Old and Still Providing Surprises. Nat. Rev. Cancer 2016, 16, 789–802. [Google Scholar] [CrossRef] [PubMed]
- Lo, A.K.-F.; Dawson, C.W.; Lung, H.L.; Wong, K.-L.; Young, L.S. The Role of EBV-Encoded LMP1 in the NPC Tumor Microenvironment: From Function to Therapy. Front. Oncol. 2021, 11, 640207. [Google Scholar] [CrossRef]
- Hau, P.M.; Lung, H.L.; Wu, M.; Tsang, C.M.; Wong, K.-L.; Mak, N.K.; Lo, K.W. Targeting Epstein-Barr Virus in Nasopharyngeal Carcinoma. Front. Oncol. 2020, 10, 600. [Google Scholar] [CrossRef]
- Zink, D.; Fischer, A.H.; Nickerson, J.A. Nuclear Structure in Cancer Cells. Nat. Rev. Cancer 2004, 4, 677–687. [Google Scholar] [CrossRef]



| Variable | Sub-Variable | Count | % or Mean (SD) |
|---|---|---|---|
| Age | 367 | 45.64 (11.30) | |
| Sex | Male | 260 | 70.84% |
| Female | 107 | 29.16% | |
| T | T1 | 30 | 8.17% |
| T2 | 49 | 13.35% | |
| T3 | 198 | 53.95% | |
| T4 | 90 | 24.52% | |
| N | N0 | 36 | 9.81% |
| N1 | 144 | 39.24% | |
| N2 | 127 | 34.60% | |
| N3 | 60 | 16.35% | |
| Stage | I | 8 | 2.18% |
| II | 30 | 8.17% | |
| III | 194 | 52.36% | |
| IV | 135 | 36.78% | |
| EBV DNA copies | ≤4000 | 200 | 54.50% |
| >4000 | 167 | 45.50% |
| Features | Discovery Set C-Index (Mean ± SD) | Validation Set C-Index (Mean ± SD) |
|---|---|---|
| Clinical | 0.873 ± 0.007 | 0.644 ± 0.124 |
| Digital NPC-TILs | 0.923 ± 0.024 | 0.785 ± 0.066 |
| TM * | 0.908 ± 0.017 | 0.624 ± 0.031 |
| Digital NPC-TILs and Clinical | 0.932 ± 0.027 | 0.670 ± 0.142 |
| Digital NPC-TILs and TM * | 0.936 ± 0.020 | 0.679 ± 0.120 |
| Clinical and TM * | 0.939 ± 0.010 | 0.629 ± 0.086 |
| All Features | 0.959 ± 0.008 | 0.689 ± 0.132 |
| Covariate | Sub-Covariate | HR | Lower HR 95% | Upper HR 95% | p-Values |
|---|---|---|---|---|---|
| Age | 1.03 | 0.96 | 1.11 | 0.3566 | |
| Gender | Female | references | |||
| Male | 1.64 | 0.25 | 10.70 | 0.6066 | |
| T | 1 | references | |||
| 2 | 0.38 | 0.01 | 19.01 | 0.6273 | |
| 3 | 2.89 | 0.29 | 28.75 | 0.3661 | |
| 4 | 1.58 | 0.12 | 20.92 | 0.7291 | |
| N | 0 | references | |||
| 1 | 0.77 | 0.10 | 5.79 | 0.8018 | |
| 2 | 0.44 | 0.05 | 3.82 | 0.4546 | |
| 3 | 0.76 | 0.07 | 7.88 | 0.8145 | |
| Stage | I | references | |||
| II | 0.32 | 0 | 39.50 | 0.6425 | |
| III | 1.50 | 0.12 | 18.11 | 0.7514 | |
| IV | 1.36 | 0.11 | 17.03 | 0.8096 | |
| EBV DNA copies | ≤4000 | references | |||
| >4000 | 1.49 | 0.30 | 7.44 | 0.6273 | |
| Digital NPC-TILs | 1.58 | 1.13 | 2.19 | <0.05 | |
| Covariate | Sub-Covariate | HR | Lower HR 95% | Upper HR 95% | p-Values |
|---|---|---|---|---|---|
| Age | 1.05 | 0.96 | 1.14 | 0.285 | |
| Gender | Female | references | |||
| Male | 1.20 | 0.15 | 9.62 | 0.866 | |
| T | 1 | references | |||
| 2 | 0.47 | 0.01 | 30.02 | 0.7200 | |
| 3 | 2.78 | 0.21 | 36.08 | 0.4352 | |
| 4 | 1.20 | 0.06 | 24.18 | 0.9073 | |
| N | 0 | references | |||
| 1 | 0.56 | 0.06 | 5.2 | 0.6107 | |
| 2 | 0.38 | 0.04 | 4.13 | 0.4290 | |
| 3 | 0.71 | 0.03 | 16.7 | 0.8291 | |
| Stage | I | references | |||
| II | 0.44 | 0 | 88.01 | 0.7593 | |
| III | 0.96 | 0.05 | 17.89 | 0.9780 | |
| IV | 1.55 | 0.08 | 30.61 | 0.7723 | |
| EBV DNA copies | ≤4000 | references | |||
| >4000 | 1.04 | 0.17 | 6.34 | 0.963 | |
| Digital NPC-TILs | 1.59 | 1.11 | 2.28 | <0.05 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wibawa, M.S.; Zhou, J.-Y.; Wang, R.; Huang, Y.-Y.; Zhan, Z.; Chen, X.; Lv, X.; Young, L.S.; Rajpoot, N. AI-Based Risk Score from Tumour-Infiltrating Lymphocyte Predicts Locoregional-Free Survival in Nasopharyngeal Carcinoma. Cancers 2023, 15, 5789. https://doi.org/10.3390/cancers15245789
Wibawa MS, Zhou J-Y, Wang R, Huang Y-Y, Zhan Z, Chen X, Lv X, Young LS, Rajpoot N. AI-Based Risk Score from Tumour-Infiltrating Lymphocyte Predicts Locoregional-Free Survival in Nasopharyngeal Carcinoma. Cancers. 2023; 15(24):5789. https://doi.org/10.3390/cancers15245789
Chicago/Turabian StyleWibawa, Made Satria, Jia-Yu Zhou, Ruoyu Wang, Ying-Ying Huang, Zejiang Zhan, Xi Chen, Xing Lv, Lawrence S. Young, and Nasir Rajpoot. 2023. "AI-Based Risk Score from Tumour-Infiltrating Lymphocyte Predicts Locoregional-Free Survival in Nasopharyngeal Carcinoma" Cancers 15, no. 24: 5789. https://doi.org/10.3390/cancers15245789
APA StyleWibawa, M. S., Zhou, J.-Y., Wang, R., Huang, Y.-Y., Zhan, Z., Chen, X., Lv, X., Young, L. S., & Rajpoot, N. (2023). AI-Based Risk Score from Tumour-Infiltrating Lymphocyte Predicts Locoregional-Free Survival in Nasopharyngeal Carcinoma. Cancers, 15(24), 5789. https://doi.org/10.3390/cancers15245789







