Long-Term Usage of Proton Pump Inhibitors Associated with Prognosis in Patients with Colorectal Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Data Source
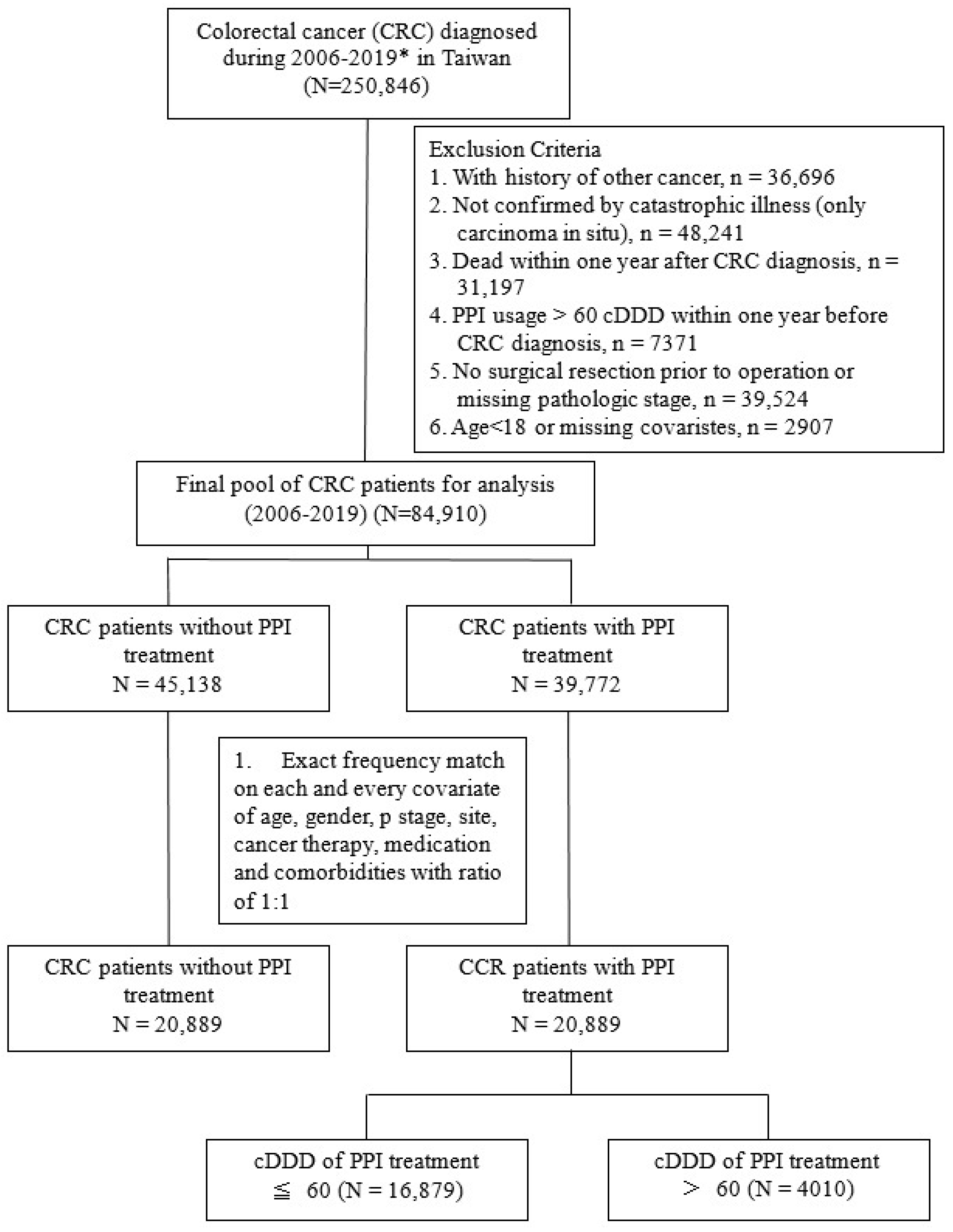
2.3. Study Population and PPI Exposure
2.4. Confounding Factors and Frequency Matching
2.5. Study Outcomes
2.6. Statistical Methods
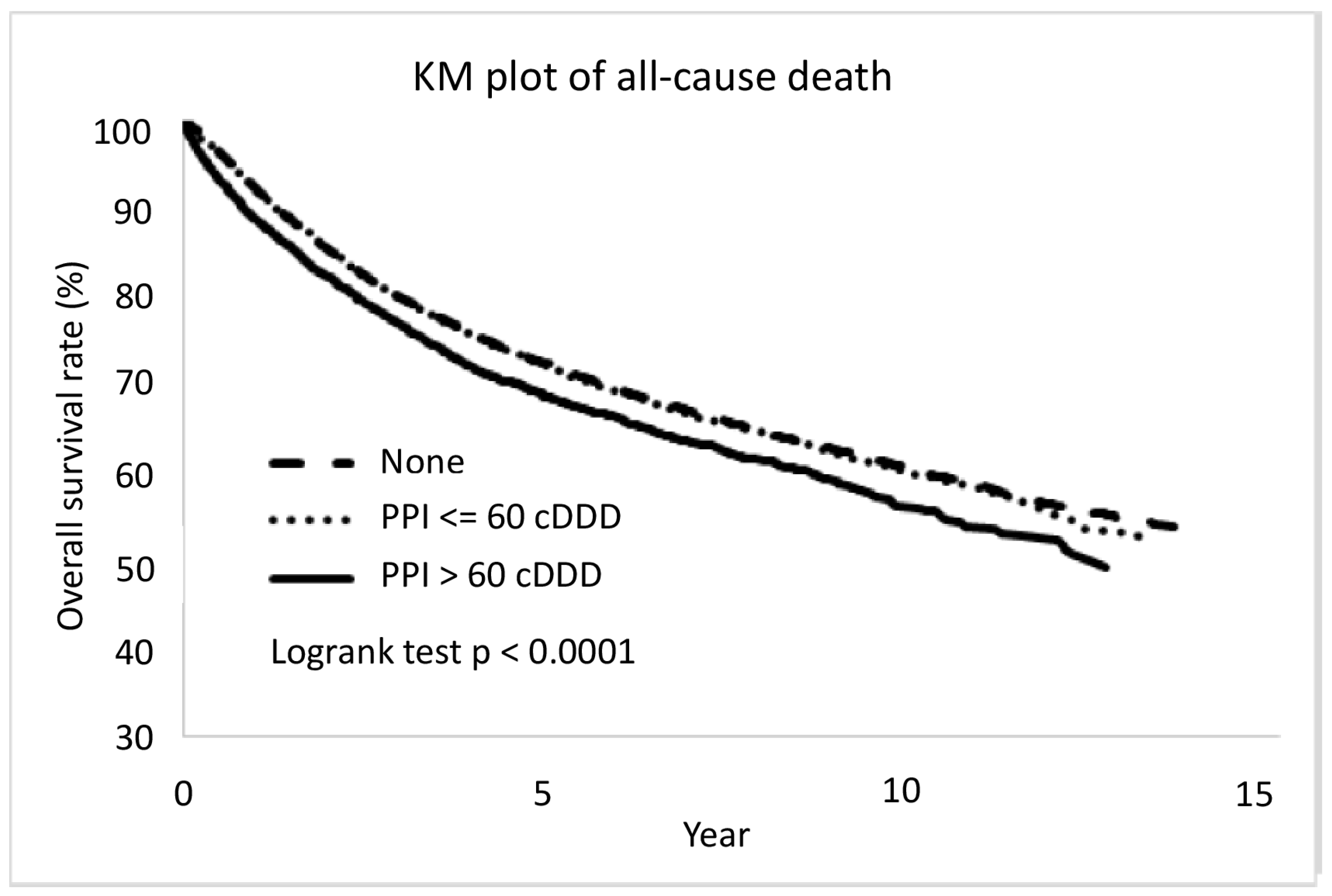
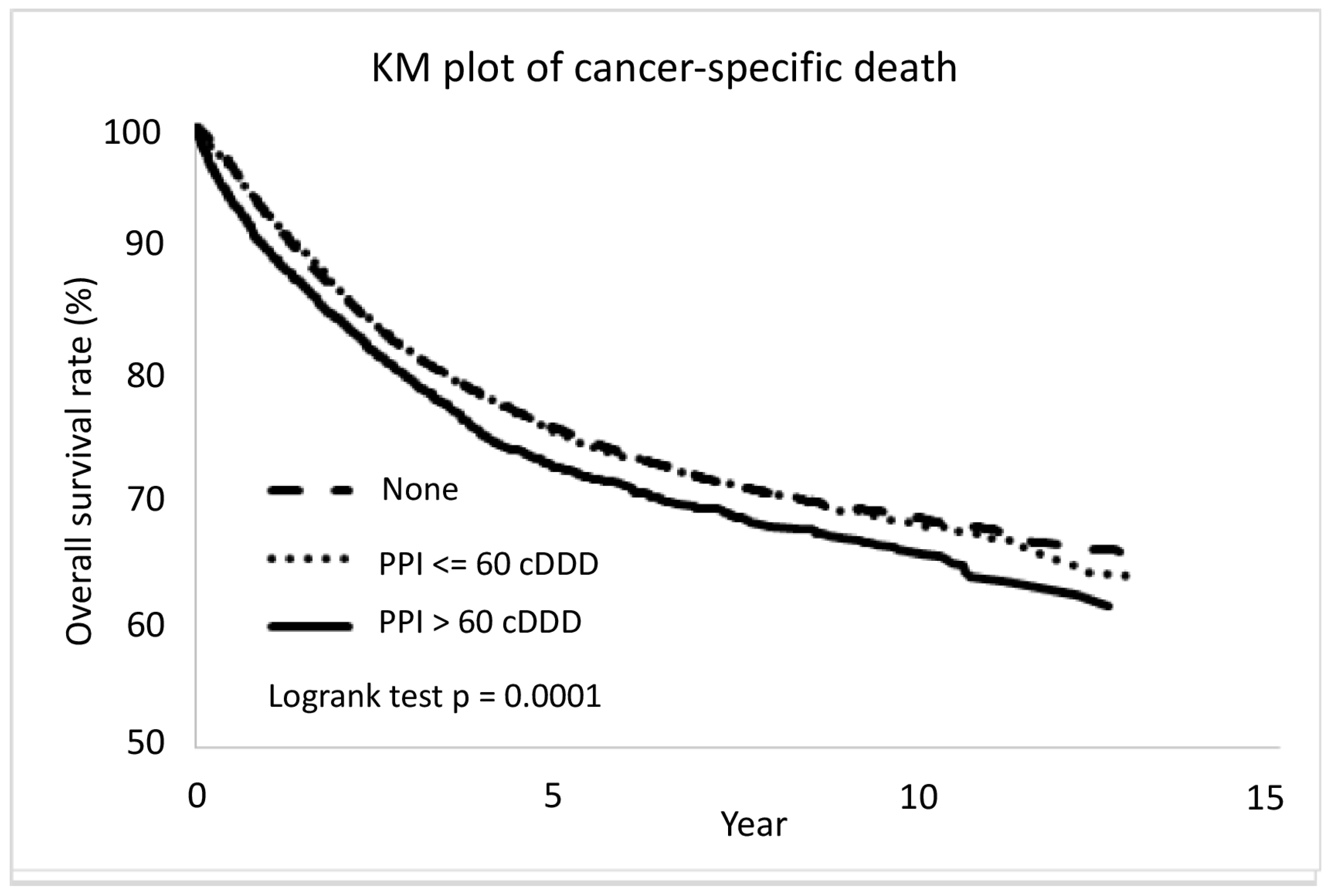
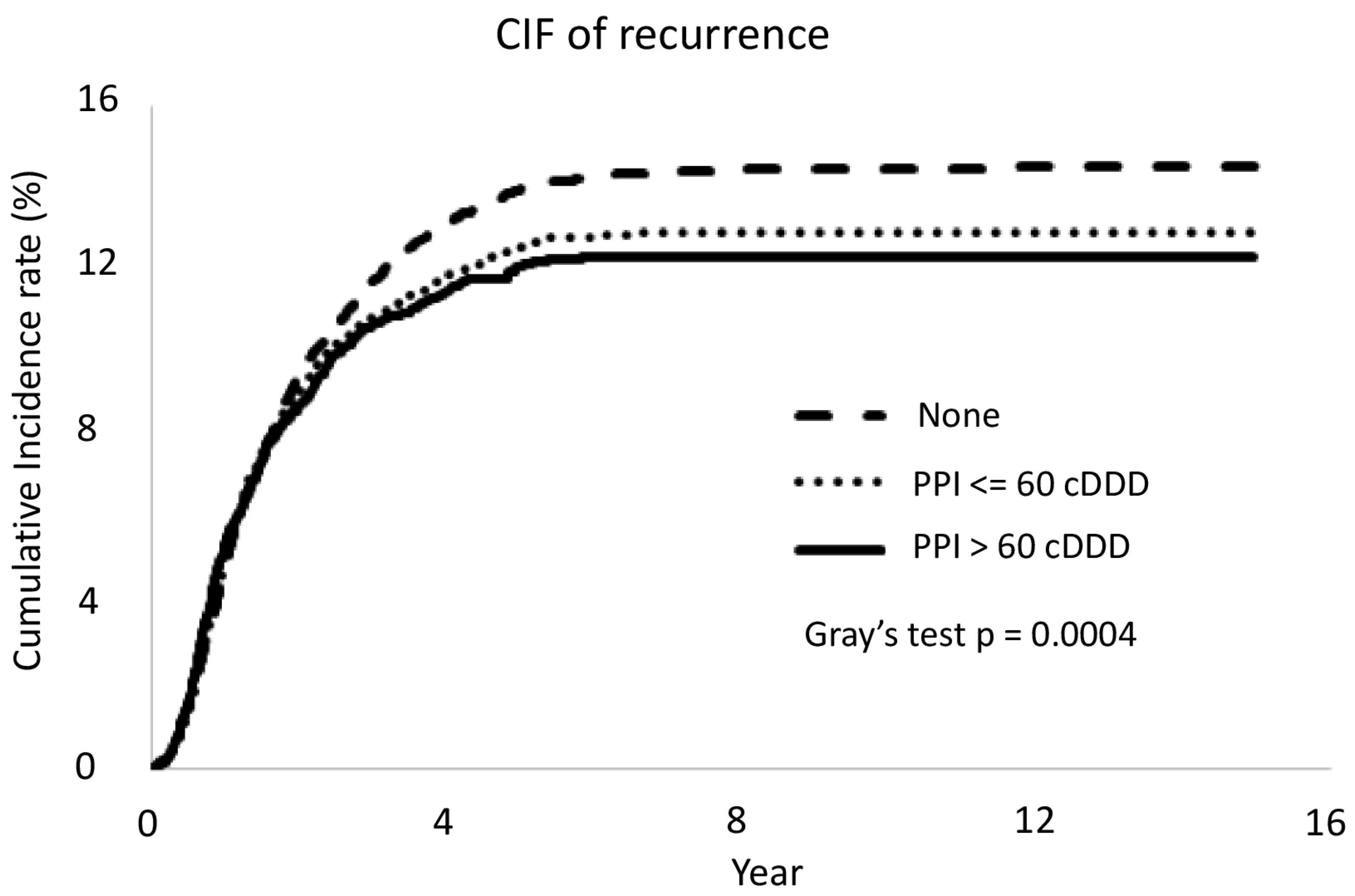
3. Results
Dose–Response Relationship
4. Discussion
4.1. Strengths of the Study
4.2. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef]
- Health Promotion Administration Ministry of Health and Welfare, Taiwan. Cancer Registry Annual Report, 2019, Taiwan. 2021. Available online: https://www.hpa.gov.tw/File/Attach/14913/File_18302.pdf (accessed on 11 August 2023).
- Baghban, R.; Roshangar, L.; Jahanban-Esfahlan, R.; Seidi, K.; Ebrahimi-Kalan, A.; Jaymand, M.; Kolahian, S.; Javaheri, T.; Zare, P. Tumor microenvironment complexity and therapeutic implications at a glance. Cell Commun. Signal. 2020, 18, 59. [Google Scholar] [CrossRef] [PubMed]
- Prendeville, H.; Lynch, L. Diet, lipids, and antitumor immunity. Cell. Mol. Immunol. 2022, 19, 432–444. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.-Z.; Jin, W.-L. The updated landscape of tumor microenvironment and drug repurposing. Signal Transduct. Target. Ther. 2020, 5, 166. [Google Scholar] [CrossRef] [PubMed]
- Jain, T.; Sharma, P.; Are, A.C.; Vickers, S.M.; Dudeja, V. New insights into the cancer–microbiome–immune axis: Decrypting a decade of discoveries. Front. Immunol. 2021, 12, 622064. [Google Scholar] [CrossRef]
- Rothwell, P.M.; Wilson, M.; Elwin, C.-E.; Norrving, B.; Algra, A.; Warlow, C.P.; Meade, T.W. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet 2010, 376, 1741–1750. [Google Scholar] [CrossRef]
- Yang, Y.X.; Hennessy, S.; Propert, K.; Hwang, W.T.; Sedarat, A.; Lewis, J.D. Chronic proton pump inhibitor therapy and the risk of colorectal cancer. Gastroenterology 2007, 133, 748–754. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, T.I.; Jeon, S.M.; Hong, S.P.; Cheon, J.H.; Kim, W.H. The effects of metformin on the survival of colorectal cancer patients with diabetes mellitus. Int. J. Cancer 2012, 131, 752–759. [Google Scholar] [CrossRef]
- Bardou, M.; Barkun, A.; Martel, M. Effect of statin therapy on colorectal cancer. Gut 2010, 59, 1572–1585. [Google Scholar] [CrossRef]
- Ho, S.W.; Teng, Y.H.; Yang, S.F.; Yeh, H.W.; Wang, Y.H.; Chou, M.C.; Yeh, C.B. Association of proton pump inhibitors usage with risk of pneumonia in dementia patients. J. Am. Geriatr. Soc. 2017, 65, 1441–1447. [Google Scholar] [CrossRef]
- Khan, M.A.; Howden, C.W. The role of proton pump inhibitors in the management of upper gastrointestinal disorders. Gastroenterol. Hepatol. 2018, 14, 169. [Google Scholar]
- Lambert, A.A.; Lam, J.O.; Paik, J.J.; Ugarte-Gil, C.; Drummond, M.B.; Crowell, T.A. Risk of community-acquired pneumonia with outpatient proton-pump inhibitor therapy: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0128004. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Wu, M.; Jia, S.; Yang, L. Proton pump inhibitors and the risk of colorectal cancer: A systematic review and meta-analysis of observational studies. Int. J. Colorectal. Dis. 2020, 35, 2157–2169. [Google Scholar] [CrossRef] [PubMed]
- Dacha, S.; Razvi, M.; Massaad, J.; Cai, Q.; Wehbi, M. Hypergastrinemia. Gastroenterol. Rep. 2015, 3, 201–208. [Google Scholar] [CrossRef]
- Thorburn, C.M.; Friedman, G.D.; Dickinson, C.J.; Vogelman, J.H.; Orentreich, N.; Parsonnet, J. Gastrin and colorectal cancer: A prospective study. Gastroenterology 1998, 115, 275–280. [Google Scholar] [CrossRef]
- Abrahami, D.; McDonald, E.G.; Schnitzer, M.E.; Barkun, A.N.; Suissa, S.; Azoulay, L. Proton pump inhibitors and risk of colorectal cancer. Gut 2022, 71, 111–118. [Google Scholar] [CrossRef]
- Lei, W.-Y.; Wang, J.-H.; Yi, C.-H.; Liu, T.-T.; Hung, J.-S.; Wong, M.-W.; Bair, M.-J.; Vaezi, M.F.; Orr, W.C.; Chen, C.-L. Association between use of proton pump inhibitors and colorectal cancer: A nationwide population-based study. Clin. Res. Hepatol. Gastroenterol. 2020, 45, 101397. [Google Scholar] [CrossRef]
- Zhang, J.-L.; Liu, M.; Yang, Q.; Lin, S.-Y.; Shan, H.-B.; Wang, H.-Y.; Xu, G.-L. Effects of omeprazole in improving concurrent chemoradiotherapy efficacy in rectal cancer. World J. Gastroenterol. 2017, 23, 2575. [Google Scholar] [CrossRef]
- Kitazume, Y.; Kawazoe, H.; Uozumi, R.; Yoshizawa, T.; Iihara, H.; Fujii, H.; Takahashi, M.; Arai, T.; Murachi, Y.; Sato, Y.; et al. Proton pump inhibitors affect capecitabine efficacy in patients with stage II–III colorectal cancer: A multicenter retrospective study. Sci. Rep. 2022, 12, 6561. [Google Scholar] [CrossRef]
- Regulations on Human Trials. Ministry of Health and Welfare. 2016. Available online: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=L0020162 (accessed on 30 October 2023).
- Personal Data Protection Act. National Development Council. 2023. Available online: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=I0050021 (accessed on 30 October 2023).
- Lu, J.-F.R.; Chiang, T.-L. Evolution of Taiwan’s health care system. Health Econ. Policy Law 2011, 6, 85–107. [Google Scholar]
- Hsieh, C.-Y.; Su, C.-C.; Shao, S.-C.; Sung, S.-F.; Lin, S.-J.; Yang, Y.-H.K.; Lai, E.-C.C. Taiwan’s national health insurance research database: Past and future. Clin. Epidemiol. 2019, 11, 349. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.-W.; Chiang, C.-J.; Lin, L.-J.; Huang, C.-W.; Lee, W.-C.; Lee, M.-Y.; Cheng-Yi, S.; Lin, H.-L.; Lin, M.-M.; Wang, Y.-P.; et al. Accuracy of long-form data in the Taiwan cancer registry. J. Formos. Med. Assoc. 2021, 120, 2037–2041. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborating Center for Drugs Statistics Methodology. ATC Index with DDDs 2003; WHO: Oslo, Norway, 2003; Available online: https://www.whocc.no/atc_ddd_index/ (accessed on 30 October 2023).
- Wu, C.-L.; Lei, W.-Y.; Wang, J.-S.; Lin, C.-E.; Chen, C.-L.; Wen, S.-H. Acid suppressants use and the risk of dementia: A population-based propensity score-matched cohort study. PLoS ONE 2020, 15, e0242975. [Google Scholar] [CrossRef]
- Patlolla, J.M.; Zhang, Y.; Li, Q.; Steele, V.E.; Rao, C.V. Anti-carcinogenic properties of omeprazole against human colon cancer cells and azoxymethane-induced colonic aberrant crypt foci formation in rats. Int. J. Oncol. 2012, 40, 170–175. [Google Scholar] [PubMed]
- Zeng, X.; Liu, L.; Zheng, M.; Sun, H.; Xiao, J.; Lu, T.; Huang, G.; Chen, P.; Zhang, J.; Zhu, F.; et al. Pantoprazole, an FDA-approved proton-pump inhibitor, suppresses colorectal cancer growth by targeting T-cell-originated protein kinase. Oncotarget 2016, 7, 22460. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Lee, H.J.; Park, J.-M.; Han, Y.-M.; Kangwan, N.; Oh, J.Y.; Lee, D.Y.; Hahm, K.B. Targeted molecular ablation of cancer stem cells for curing gastrointestinal cancers. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 1059–1070. [Google Scholar] [CrossRef]
- Ikemura, K.; Hiramatsu, S.; Okuda, M. Drug repositioning of proton pump inhibitors for enhanced efficacy and safety of cancer chemotherapy. Front. Pharmacol. 2017, 8, 911. [Google Scholar] [CrossRef]
- Patel, A.; Spychalski, P.; Antoszewska, M.; Regula, J.; Kobiela, J. Proton pump inhibitors and colorectal cancer: A systematic review. World J. Gastroenterol. 2021, 27, 7716–7733. [Google Scholar] [CrossRef]
- Winsett, O.E.; Townsend, C.M.; Glass, E.J.; Thompson, J.C. Gastrin stimulates growth of colon cancer. Surgery 1986, 99, 302–307. [Google Scholar]
- Sasaki, T.; Mori, S.; Kishi, S.; Fujiwara-Tani, R.; Ohmori, H.; Nishiguchi, Y.; Hojo, Y.; Kawahara, I.; Nakashima, C.; Fujii, K.; et al. Effect of proton pump inhibitors on colorectal cancer. Int. J. Mol. Sci. 2020, 21, 3877. [Google Scholar] [CrossRef]
- Imhann, F.; Bonder, M.J.; Vila, A.V.; Fu, J.; Mujagic, Z.; Vork, L.; Tigchelaar, E.F.; Jankipersadsing, S.A.; Cenit, M.C.; Harmsen, H.J.M.; et al. Proton pump inhibitors affect the gut microbiome. Gut 2016, 65, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Sheflin, A.M.; Whitney, A.K.; Weir, T.L. Cancer-promoting effects of microbial dysbiosis. Curr. Oncol. Rep. 2014, 16, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bruno, G.; Zaccari, P.; Rocco, G.; Scalese, G.; Panetta, C.; Porowska, B.; Pontone, S.; Severi, C. Proton pump inhibitors and dysbiosis: Current knowledge and aspects to be clarified. World J. Gastroenterol. 2019, 25, 2706. [Google Scholar] [CrossRef] [PubMed]
- Wong, G.G.; Ha, V.; Chu, M.P.; Dersch-Mills, D.; Ghosh, S.; Chambers, C.R.; Sawyer, M.B. Effects of proton pump inhibitors on FOLFOX and CapeOx regimens in colorectal cancer. Clin. Color. Cancer 2019, 18, 72–79. [Google Scholar] [CrossRef]

| PPI Non-Users | PPI Users | ||
|---|---|---|---|
| Covariate | N (%), n = 20,889 | N (%), n = 20,889 | p Value |
| Age (year) | 1.000 | ||
| 18–55 | 6541 (31.3) | 6541 (31.3) | |
| 56–65 | 6349 (30.4) | 6349 (30.4) | |
| 66–75 | 4765 (22.8) | 4765 (22.8) | |
| >75 | 3234 (15.5) | 3234 (15.5) | |
| Sex | 1.000 | ||
| Male | 11,594 (55.5) | 11,594 (55.5) | |
| Female | 9295 (44.5) | 9295 (44.5) | |
| Cancer site | 1.000 | ||
| Colon left | 6190 (29.6) | 6190 (29.6) | |
| Colon right | 3834 (18.4) | 3834 (18.4) | |
| Colon unspecified | 4277 (20.5) | 4277 (20.5) | |
| Rectum | 6588 (31.5) | 6588 (31.5) | |
| Pathological stage | 1.000 | ||
| I | 4543 (21.8) | 4543 (21.8) | |
| II | 6118 (29.3) | 6118 (29.3) | |
| III | 7700 (36.9) | 7700 (36.9) | |
| IV | 2528 (12.1) | 2528 (12.1) | |
| Cancer treatment | |||
| Chemotherapy | 9424 (45.1) | 9424 (45.1) | 1.000 |
| Radiotherapy | 2282 (10.9) | 2282 (10.9) | 1.000 |
| Surgery | 20,889 (100) | 20,889 (100) | 1.000 |
| Targeted therapy | 1853 (8.9) | 1853 (8.9) | 1.000 |
| Comorbidity | |||
| Coronary heart disease | 942 (4.5) | 942 (4.5) | 1.000 |
| Congestive heart failure | 48 (0.2) | 48 (0.2) | 1.000 |
| Asthma | 181 (0.9) | 181 (0.9) | 1.000 |
| Interstitial lung disease | (0) | (0) | 1.000 |
| COPD | 206 (1) | 206 (1) | 1.000 |
| Liver cirrhosis | 14 (0.1) | 14 (0.1) | 1.000 |
| Diabetes mellitus | 2999 (14.4) | 2999 (14.4) | 1.000 |
| CKD | 169 (0.8) | 169 (0.8) | 1.000 |
| Stroke | 484 (2.3) | 484 (2.3) | 1.000 |
| Dementia | 68 (0.3) | 68 (0.3) | 1.000 |
| Hypertension | 6808 (32.6) | 6808 (32.6) | 1.000 |
| PUD | 2315 (11.1) | 2315 (11.1) | 1.000 |
| GI bleeding | 1533 (7.3) | 1533 (7.3) | 1.000 |
| Medication | |||
| NSAIDs usage | 16,283 (78) | 16,283 (78) | 1.000 |
| Steroids usage | 13,635 (65.3) | 13,635 (65.3) | 1.000 |
| CCI | 1.000 | ||
| 0 | 12,548 (60.1) | 12,548 (60.1) | |
| 1–2 | 5807 (27.8) | 5807 (27.8) | |
| ≥3 | 2534 (12.1) | 2534 (12.1) | |
| Urbanization | 0.0002 | ||
| High | 5006 (24) | 4669 (22.4) | |
| Median | 10,284 (49.2) | 10,396 (49.8) | |
| Low | 5599 (26.8) | 5824 (27.9) | |
| Region | 0.0000 | ||
| North | 9140 (43.8) | 8866 (42.4) | |
| Central | 4678 (22.4) | 5723 (27.4) | |
| East | 343 (1.6) | 478 (2.3) | |
| South | 6728 (32.2) | 5822 (27.9) | |
| SES (monthly income) | 0.0226 | ||
| ≤20.1 K | 7394 (35.4) | 7118 (34.1) | |
| 20.1–22.8 K | 3049 (14.6) | 3105 (14.9) | |
| 22.8–42 K | 5613 (26.9) | 5641 (27) | |
| ≥42 K | 4833 (23.1) | 5025 (24.1) |
| All-Cause Death | CRC-Specific Death | Recurrence * | ||||
|---|---|---|---|---|---|---|
| IP (95% CI) | Event (%) | IP (95% CI) | Event (%) | IP (95% CI) | Event (%) | |
| PPI non-users | 57.1 (55.7, 58.5) | 6454 (30.9) | 41.4 (40.2, 42.6) | 4677 (22.4) | 22.6 (21.8, 23.4) | 2837 (13.6) |
| PPI users | 63.1 (61.5, 64.8) | 5520 (26.4) | 46.8 (45.3, 48.2) | 4087 (19.6) | 23.9 (22.9,24.8) | 2422 (11.6) |
| cDDD ≤ 60 | 61.2 (59.4, 63.1) | 4361 (25.8) | 45.5 (44.0, 47.1) | 3243 (19.2) | 23.9 (22.9,25.0) | 1973 (11.7) |
| cDDD > 60 | 71.5 (67.5, 75.8) | 1159 (28.9) | 52.1 (48.6, 55.7) | 844 (21.0) | 23.6 (21.5,25.9) | 449 (11.2) |
| All-Cause Death | Cancer-Specific Death | Recurrence * | ||||
|---|---|---|---|---|---|---|
| Adjusted HR (95% CI) | p Value | Adjusted HR (95% CI) | p Value | Adjusted HR (95% CI) | p Value | |
| PPI non-users | 1 | 1 | 1 | |||
| PPI users | 1.05 (1.02, 1.09) | 0.0055 | 1.04 (1.00, 1.08) | 0.0436 | 0.89 (0.84, 0.94) | <0.0001 |
| cDDD ≤ 60 | 1.04 (1.00, 1.08) | 0.0496 | 1.03 (0.99, 1.08) | 0.1611 | 0.90 (0.85, 0.95) | 0.0003 |
| cDDD > 60 | 1.10 (1.04, 1.18) | 0.0021 | 1.09 (1.01, 1.17) | 0.0210 | 0.84 (0.76, 0.95) | 0.0012 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.-C.; Fang, C.-Y.; Yu, B.-H.; Chang, C.-M.; Hsu, T.-W.; Hung, C.-L.; Hung, S.-K.; Chiou, W.-Y.; Tsai, J.-H. Long-Term Usage of Proton Pump Inhibitors Associated with Prognosis in Patients with Colorectal Cancer. Cancers 2023, 15, 5304. https://doi.org/10.3390/cancers15215304
Wu C-C, Fang C-Y, Yu B-H, Chang C-M, Hsu T-W, Hung C-L, Hung S-K, Chiou W-Y, Tsai J-H. Long-Term Usage of Proton Pump Inhibitors Associated with Prognosis in Patients with Colorectal Cancer. Cancers. 2023; 15(21):5304. https://doi.org/10.3390/cancers15215304
Chicago/Turabian StyleWu, Chin-Chia, Chuan-Yin Fang, Ben-Hui Yu, Chun-Ming Chang, Ta-Wen Hsu, Chung-Lin Hung, Shih-Kai Hung, Wen-Yen Chiou, and Jui-Hsiu Tsai. 2023. "Long-Term Usage of Proton Pump Inhibitors Associated with Prognosis in Patients with Colorectal Cancer" Cancers 15, no. 21: 5304. https://doi.org/10.3390/cancers15215304
APA StyleWu, C.-C., Fang, C.-Y., Yu, B.-H., Chang, C.-M., Hsu, T.-W., Hung, C.-L., Hung, S.-K., Chiou, W.-Y., & Tsai, J.-H. (2023). Long-Term Usage of Proton Pump Inhibitors Associated with Prognosis in Patients with Colorectal Cancer. Cancers, 15(21), 5304. https://doi.org/10.3390/cancers15215304





