An Interpretable Radiomics Model Based on Two-Dimensional Shear Wave Elastography for Predicting Symptomatic Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
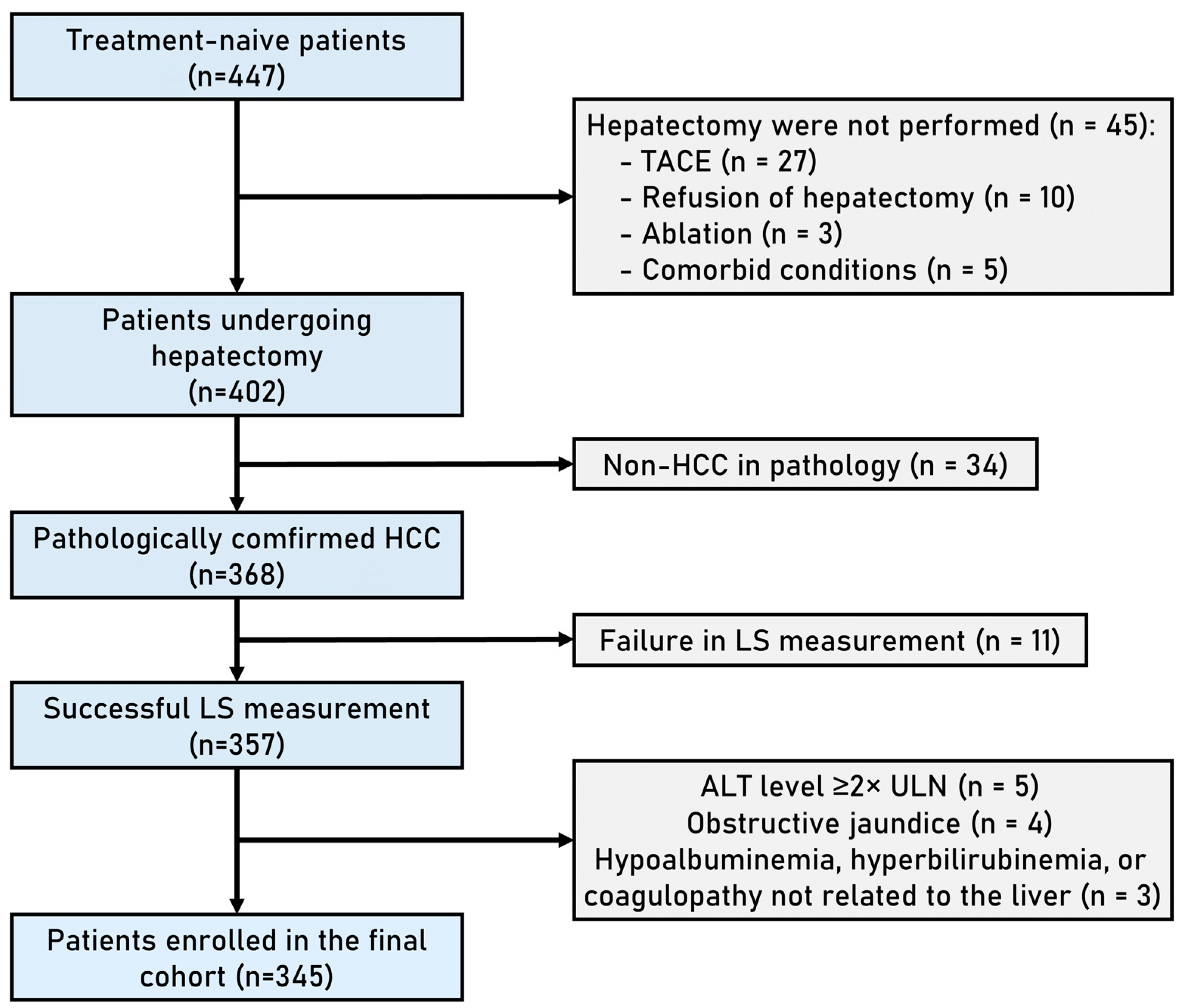
2.1. Patients
2.2. Two-Dimensional SWE Data Acquisition
2.3. Clinical Data Collection
2.4. Diagnosis and Staging of Symptomatic PHLF
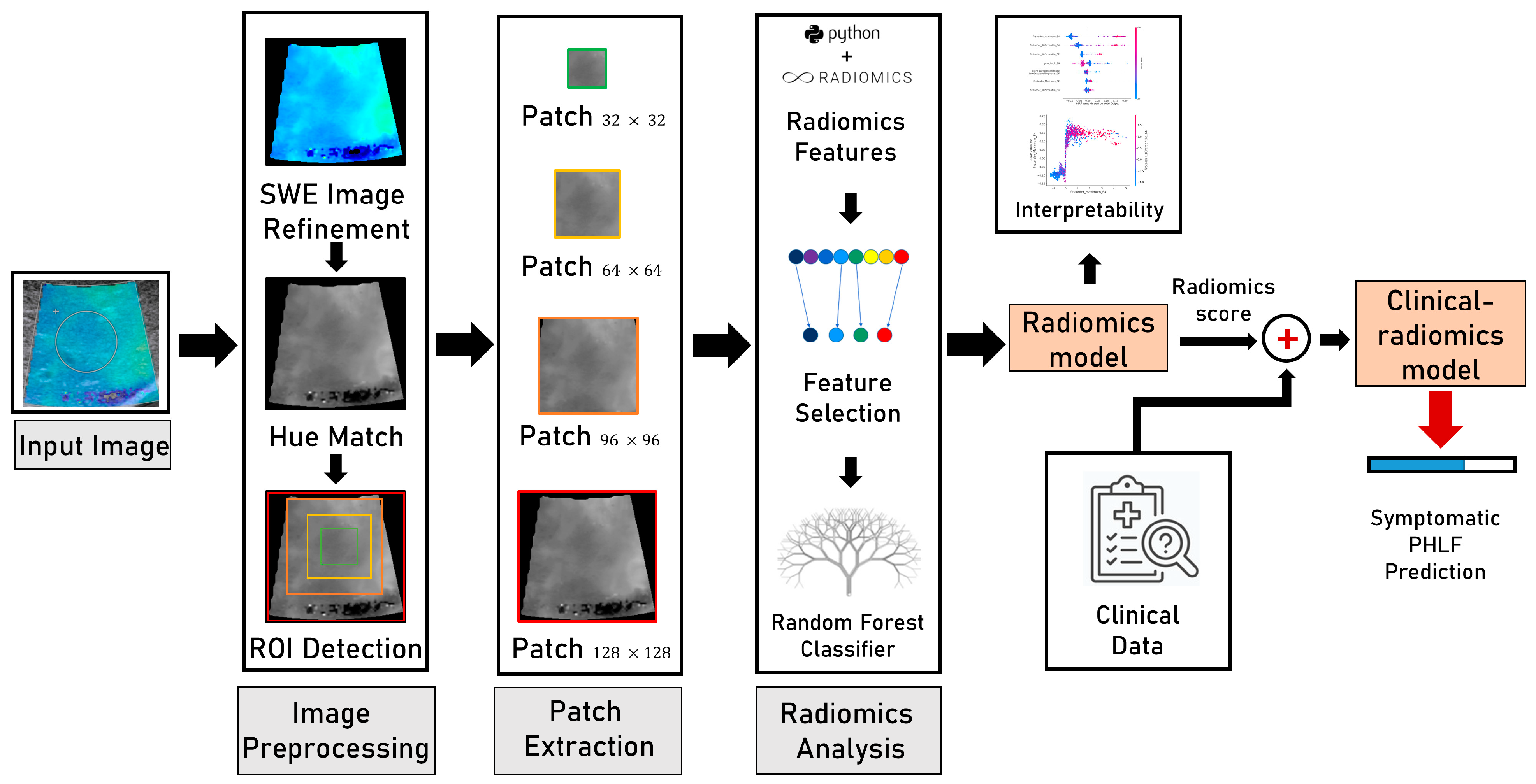
2.5. Construction of Radiomics Models
- (1)
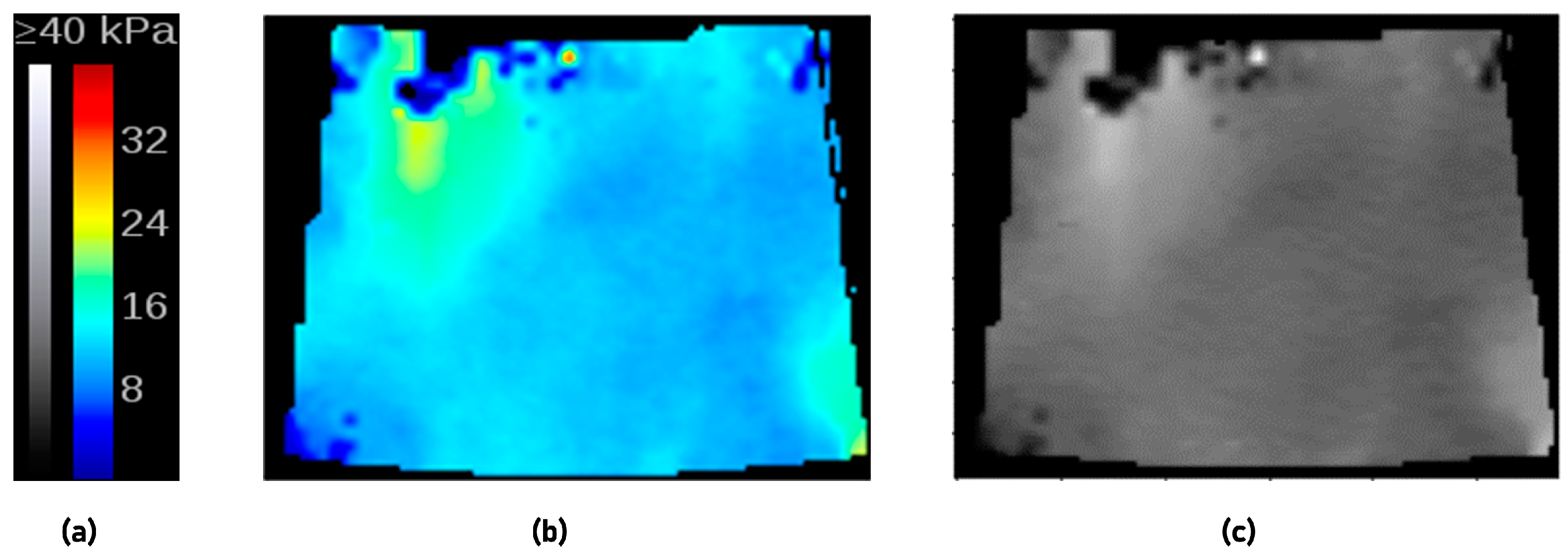
- Image preprocessing:
- (2)
- The radiomics model based on 2D-SWE images:
- (3)
- The clinical–radiomics model based on 2D-SWE images and clinical data:
2.6. Shapley Additive exPlanations
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Performance of the Clinical Model
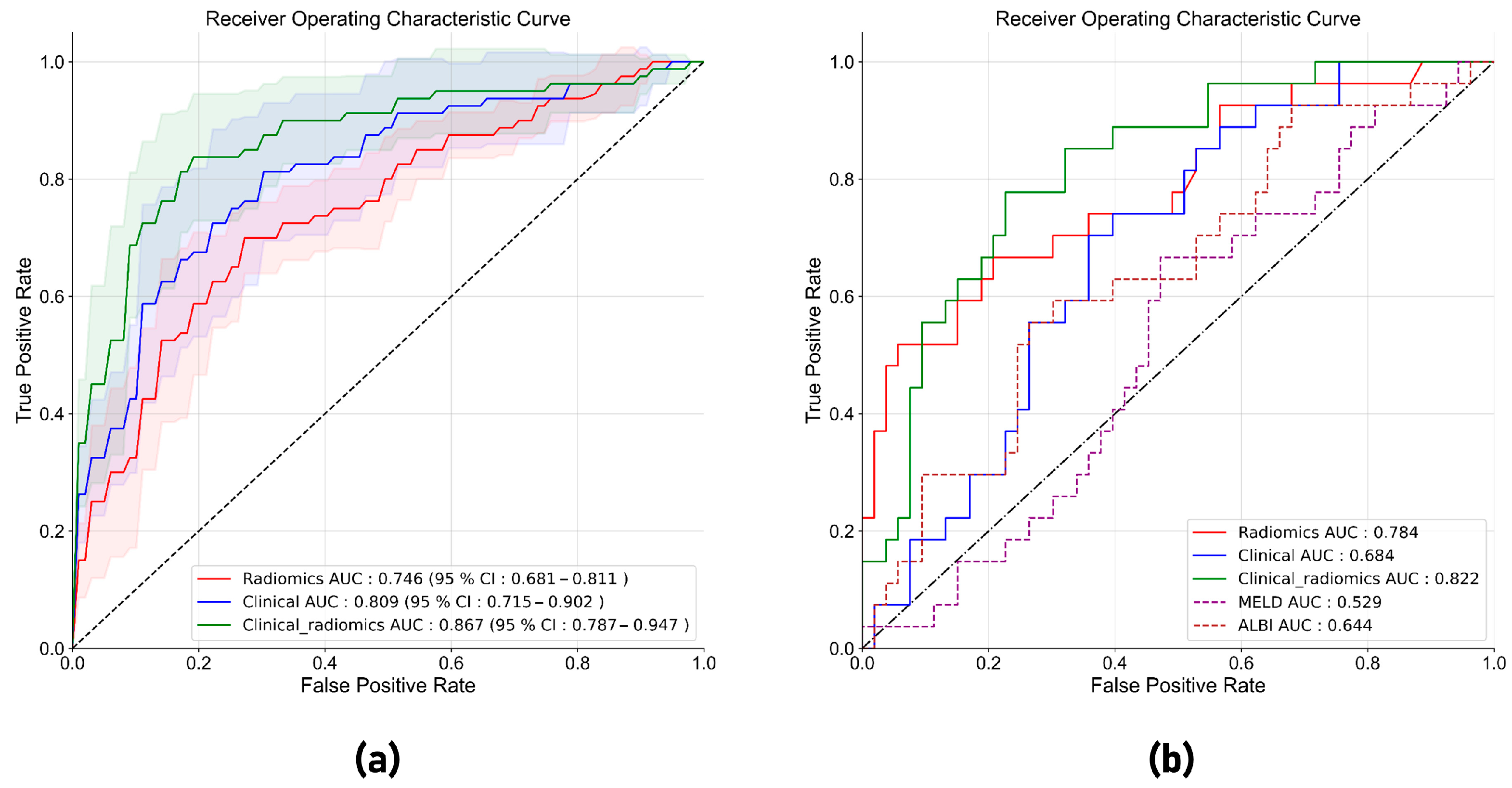
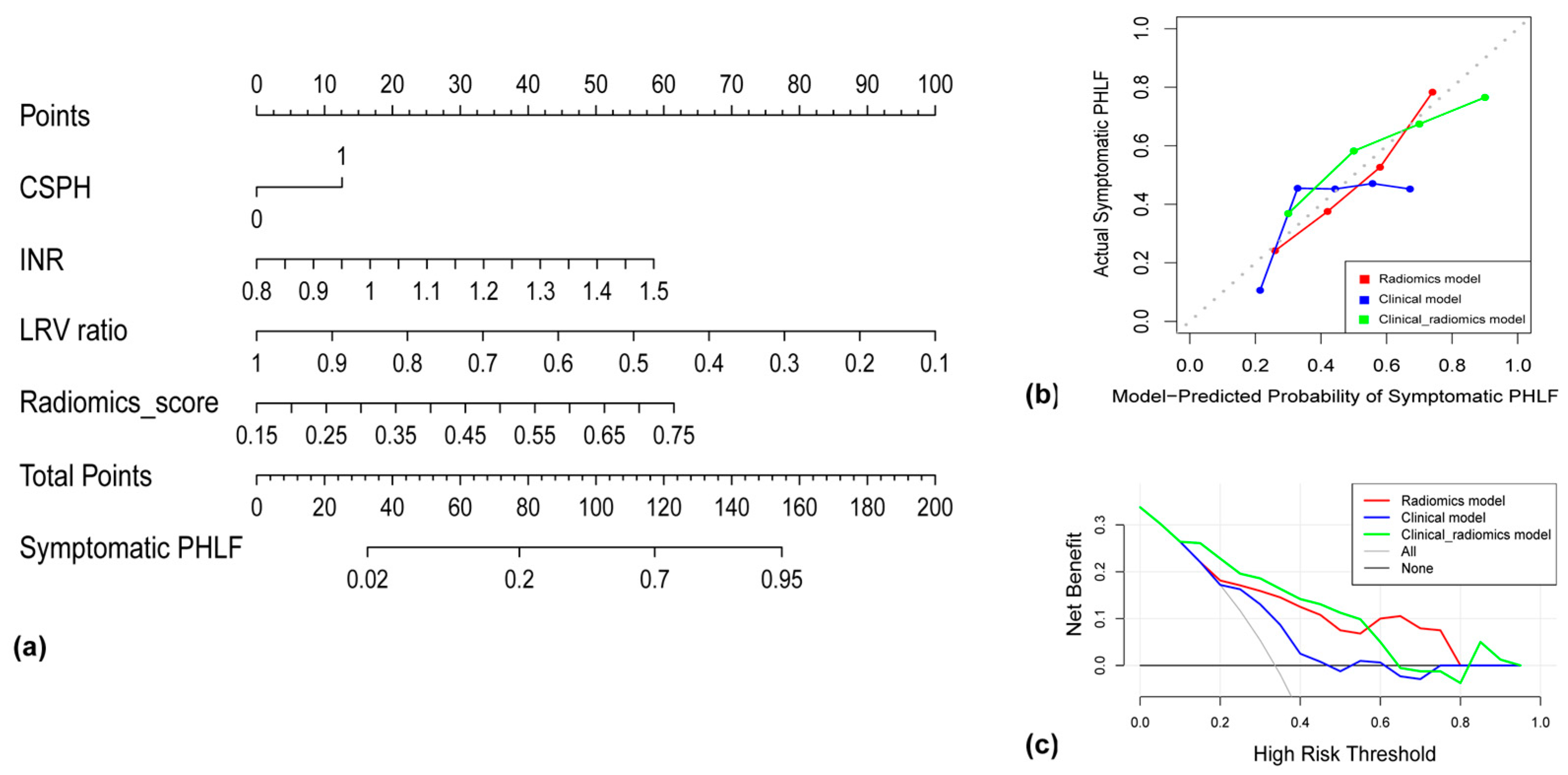
3.3. Performance of the Radiomics Model and the Clinical–Radiomics Model in Five-Fold Cross-Validation
3.4. Performance of the Radiomics Model and the Clinical–Radiomics Model in the Test Set
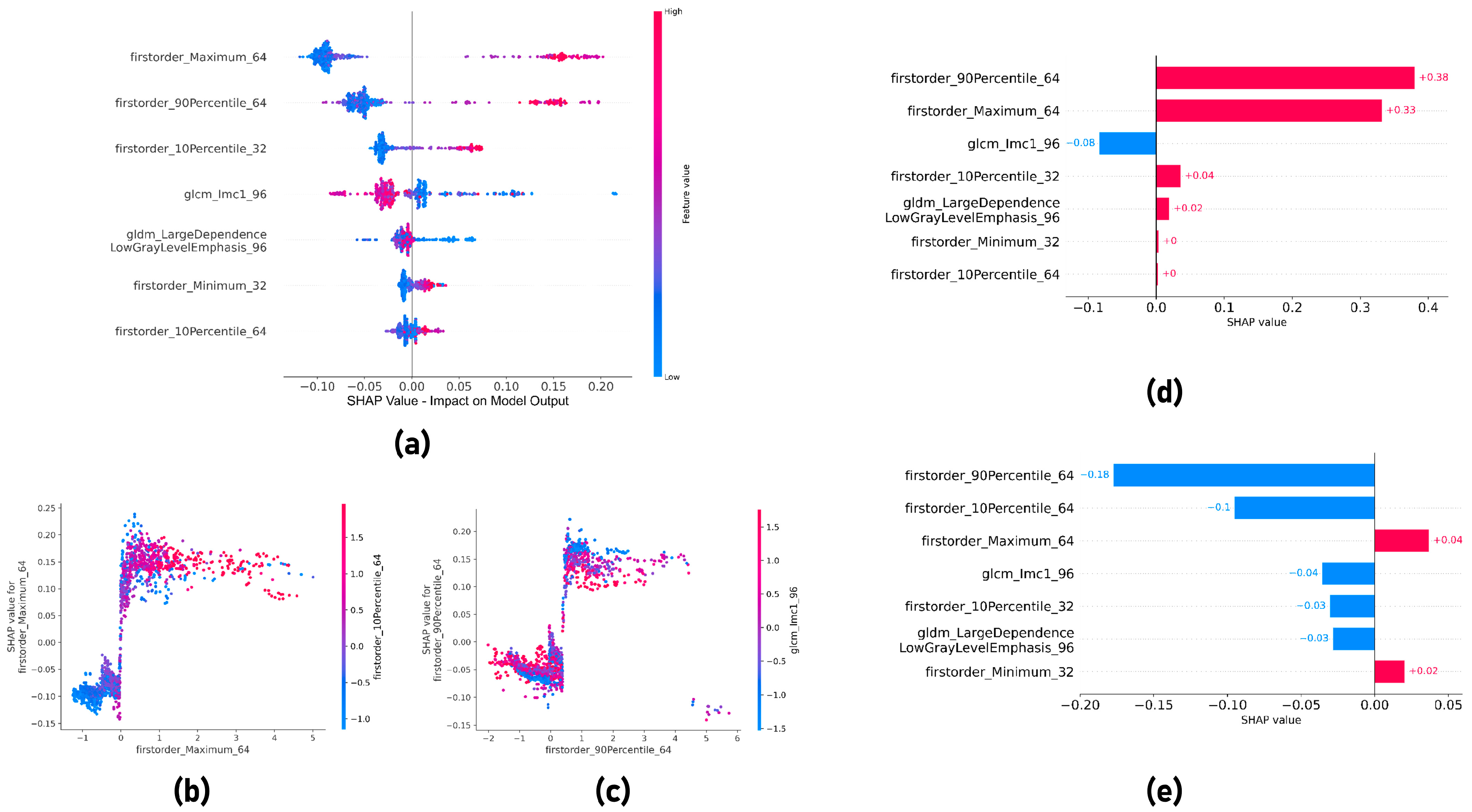
3.5. Shapley Additive exPlanations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- EASL. Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Garden, O.J.; Padbury, R.; Brooke-Smith, M.; Crawford, M.; Adam, R.; Koch, M.; Makuuchi, M.; Dematteo, R.P.; Christophi, C.; et al. Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011, 149, 713–724. [Google Scholar] [CrossRef]
- Fukushima, K.; Fukumoto, T.; Kuramitsu, K.; Kido, M.; Takebe, A.; Tanaka, M.; Itoh, T.; Ku, Y. Assessment of ISGLS definition of posthepatectomy liver failure and its effect on outcome in patients with hepatocellular carcinoma. J. Gastrointest. Surg. 2014, 18, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Hobeika, C.; Fuks, D.; Cauchy, F.; Goumard, C.; Soubrane, O.; Gayet, B.; Salamé, E.; Cherqui, D.; Vibert, E.; Scatton, O.; et al. Impact of cirrhosis in patients undergoing laparoscopic liver resection in a nationwide multicentre survey. Br. J. Surg. 2020, 107, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Zou, H.; Yang, X.; Li, Q.L.; Zhou, Q.X.; Xiong, L.; Wen, Y. A Comparative Study of Albumin-Bilirubin Score with Child-Pugh Score, Model for End-Stage Liver Disease Score and Indocyanine Green R15 in Predicting Posthepatectomy Liver Failure for Hepatocellular Carcinoma Patients. Dig. Dis. 2018, 36, 236–243. [Google Scholar] [CrossRef]
- Ross, S.W.; Seshadri, R.; Walters, A.L.; Augenstein, V.A.; Heniford, B.T.; Iannitti, D.A.; Martinie, J.B.; Vrochides, D.; Swan, R.Z. Mortality in hepatectomy: Model for End-Stage Liver Disease as a predictor of death using the National Surgical Quality Improvement Program database. Surgery 2016, 159, 777–792. [Google Scholar] [CrossRef]
- Wang, Y.Y.; Zhong, J.H.; Su, Z.Y.; Huang, J.F.; Lu, S.D.; Xiang, B.D.; Ma, L.; Qi, L.N.; Ou, B.N.; Li, L.Q. Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br. J. Surg. 2016, 103, 725–734. [Google Scholar] [CrossRef]
- Fagenson, A.M.; Gleeson, E.M.; Pitt, H.A.; Lau, K.N. Albumin-Bilirubin Score vs Model for End-Stage Liver Disease in Predicting Post-Hepatectomy Outcomes. J. Am. Coll. Surg. 2020, 230, 637–645. [Google Scholar] [CrossRef]
- Dietrich, C.F.; Bamber, J.; Berzigotti, A.; Bota, S.; Cantisani, V.; Castera, L.; Cosgrove, D.; Ferraioli, G.; Friedrich-Rust, M.; Gilja, O.H.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall. Med. 2017, 38, e48. [Google Scholar]
- Samir, A.E.; Dhyani, M.; Vij, A.; Bhan, A.K.; Halpern, E.F.; Méndez-Navarro, J.; Corey, K.E.; Chung, R.T. Chung Shear-wave elastography for the estimation of liver fibrosis in chronic liver disease: Determining accuracy and ideal site for measurement. Radiology 2015, 274, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Hu, H.; Xu, Y.D.; Wang, W.P.; Ding, H.; Lu, Q. Liver failure after hepatectomy: A risk assessment using the pre-hepatectomy shear wave elastography technique. Eur. J. Radiol. 2017, 86, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Long, H.; Zhong, X.; Su, L.; Huang, T.; Duan, Y.; Ke, W.; Xie, X.; Lin, M. Liver Stiffness Measured by Two-Dimensional Shear Wave Elastography for Predicting Symptomatic Post-hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma. Ann. Surg. Oncol. 2022, 29, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zheng, P.; Wang, X.; Sang, L. Effect of Q-Box size on liver stiffness measurement by two-dimensional shear wave elastography. J. Clin. Ultrasound 2021, 49, 978–983. [Google Scholar] [CrossRef]
- Gatos, I.; Tsantis, S.; Spiliopoulos, S.; Karnabatidis, D.; Theotokas, I.; Zoumpoulis, P.; Loupas, T.; Hazle, J.D.; Kagadis, G.C. A new computer aided diagnosis system for evaluation of chronic liver disease with ultrasound shear wave elastography imaging. Med. Phys. 2016, 43, 1428–1436. [Google Scholar] [CrossRef] [PubMed]
- Lambin, P.; Rios-Velazquez, E.; Leijenaar, R.; Carvalho, S.; van Stiphout, R.G.; Granton, P.; Zegers, C.M.; Gillies, R.; Boellard, R.; Dekker, A.; et al. Radiomics: Extracting more information from medical images using advanced feature analysis. Eur. J. Cancer 2012, 48, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Bera, K.A.-O.; Braman, N.; Gupta, A.A.-O.; Velcheti, V.; Madabhushi, A. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat. Rev. Clin. Oncol. 2022, 19, 132–146. [Google Scholar] [CrossRef]
- Xiao, Y.; Zeng, J.; Niu, L.; Zeng, Q.; Wu, T.; Wang, C.; Zheng, R.; Zheng, H. Computer-aided diagnosis based on quantitative elastographic features with supersonic shear wave imaging. Ultrasound Med. Biol. 2014, 40, 275–286. [Google Scholar] [CrossRef]
- Cheng, M.Q.; Xian, M.F.; Tian, W.S.; Li, M.D.; Hu, H.T.; Li, W.; Zhang, J.C.; Huang, Y.; Xie, X.Y.; Lu, M.D.; et al. RGB Three-Channel SWE-Based Ultrasomics Model: Improving the Efficiency in Differentiating Focal Liver Lesions. Front. Oncol. 2021, 11, 704218. [Google Scholar] [CrossRef]
- Gatos, I.; Tsantis, S.; Spiliopoulos, S.; Karnabatidis, D.; Theotokas, I.; Zoumpoulis, P.; Loupas, T.; Hazle, J.D.; Kagadis, G.C. A Machine-Learning Algorithm Toward Color Analysis for Chronic Liver Disease Classification, Employing Ultrasound Shear Wave Elastography. Ultrasound Med. Biol. 2017, 43, 1797–1810. [Google Scholar] [CrossRef]
- Salahuddin, Z.; Woodruff, H.C.; Chatterjee, A.; Lambin, P. Transparency of deep neural networks for medical image analysis: A review of interpretability methods. Comput. Biol. Med. 2021, 140, 105111. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, S.M.; Lee, S.-I. A unified approach to interpreting model predictions. Adv. Neural Inf. Process. Syst. 2017, 30, 4765–4774. [Google Scholar]
- Heimbach, J.K.; Kulik, L.M.; Finn, R.S.; Sirlin, C.B.; Abecassis, M.M.; Roberts, L.R.; Zhu, A.X.; Murad, M.H.; Marrero, J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018, 67, 358–380. [Google Scholar] [CrossRef] [PubMed]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular carcinoma. Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef]
- EASL-EORTC. Clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2012, 56, 908–943. [Google Scholar] [CrossRef]
- Bae, J.S.; Lee, D.H.; Yoo, J.; Yi, N.J.; Lee, K.W.; Suh, K.S.; Kim, H.; Lee, K.B. Association between spleen volume and the post-hepatectomy liver failure and overall survival of patients with hepatocellular carcinoma after resection. Eur. Radiol. 2021, 31, 2461–2471. [Google Scholar] [CrossRef]
- Prodeau, M.; Drumez, E.; Duhamel, A.; Vibert, E.; Farges, O.; Lassailly, G.; Mabrut, J.Y.; Hardwigsen, J.; Régimbeau, J.M.; Soubrane, O.; et al. An ordinal model to predict the risk of symptomatic liver failure in patients with cirrhosis undergoing hepatectomy. J. Hepatol. 2019, 71, 920–929. [Google Scholar] [CrossRef]
- Zhang, Q.; Xiao, Y.; Suo, J.; Shi, J.; Yu, J.; Guo, Y.; Wang, Y.; Zheng, H. Sonoelastomics for Breast Tumor Classification: A Radiomics Approach with Clustering-Based Feature Selection on Sonoelastography. Ultrasound Med. Biol. 2017, 43, 1058–1069. [Google Scholar] [CrossRef]
- Brattain, L.J.; Ozturk, A.; Telfer, B.A.; Dhyani, M.; Grajo, J.R.; Samir, A.E. Image Processing Pipeline for Liver Fibrosis Classification Using Ultrasound Shear Wave Elastography. Ultrasound Med. Biol. 2020, 46, 2667–2676. [Google Scholar] [CrossRef]
- Shen, Y.; Zhou, C.; Zhu, G.; Shi, G.; Zhu, X.; Huang, C.; Zhou, J.; Fan, J.; Ding, H.; Ren, N.; et al. Liver Stiffness Assessed by Shear Wave Elastography Predicts Postoperative Liver Failure in Patients with Hepatocellular Carcinoma. J. Gastrointest. Surg. 2017, 21, 1471–1479. [Google Scholar] [CrossRef]
- Luo, N.; Huang, X.; Ji, Y.; Jin, G.; Qin, Y.; Xiang, B.; Su, D.; Tang, W. A functional liver imaging score for preoperative prediction of liver failure after hepatocellular carcinoma resection. Eur. Radiol. 2022, 32, 5623–5632. [Google Scholar] [CrossRef] [PubMed]
- Hobeika, C.; Guyard, C.; Sartoris, R.; Maino, C.; Rautou, P.E.; Dokmak, S.; Bouattour, M.; Durand, F.; Weiss, E.; Vilgrain, V.; et al. Performance of non-invasive biomarkers compared with invasive methods for risk prediction of posthepatectomy liver failure in hepatocellular carcinoma. Br. J. Surg. 2022, 109, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Han, H.; Han, X.K.; Wang, W.P.; Ding, H. Nomogram for individualised prediction of liver failure risk after hepatectomy in patients with resectable hepatocellular carcinoma: The evidence from ultrasound data. Eur. Radiol. 2018, 28, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Ruan, D.; Shi, Y.; Jin, L.; Yang, Q.; Yu, W.; Ren, H.; Zheng, W.; Chen, Y.; Zheng, N.; Zheng, M. An ultrasound image-based deep multi-scale texture network for liver fibrosis grading in patients with chronic HBV infection. Liver Int. 2021, 41, 2440–2454. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | All Patients (n = 345) | Training Cohort (n = 265) | Test Cohort (n = 80) | p-Value |
|---|---|---|---|---|
| Age (year) | 55.0 (47.0–64.0) | 55.0 (47.0–64.0) | 54.0 (49.0–66.8) | 0.354 |
| Sex (male/female) | 305/40 | 238/27 | 67/13 | 0.138 |
| Underlying liver disease (HBV/HCV/coinfection of HBV and HCV/unknown) | 324/7/6/8 | 249/5/5/6 | 75/2/1/2 | 0.965 |
| TBIL (umol/L) | 13.8 (10.7–17.3) | 13.6 (10.6–16.9) | 15.0 (11.5–17.9) | 0.081 |
| ALB (g/L) | 38.3 (36.2–41.0) | 38.3 (36.2–41.0) | 38.8 (36.2–41.2) | 0.942 |
| CREA (umol/L) | 79.0 (68.0–87.0) | 79.0 (68.0–87.5) | 80.0 (68.3–87.0) | 0.940 |
| ALT (U/L) | 31.0 (21.0–43.5) | 32.0 (20.0–43.0) | 31.0 (22.0–52.8) | 0.805 |
| AST (U/L) | 35.0 (25.0–50.0) | 35.0 (26.0–50.0) | 36.0 (23.0–50.7) | 0.812 |
| GGT (U/L) | 55.0 (34.0–98.5) | 59.0 (36.0–103.0) | 50.0 (30.3–85.8) | 0.055 |
| PT (s) | 11.9 (11.3–12.6) | 11.8 (11.2–12.4) | 12.2 (11.7–12.8) | 0.002 |
| INR | 1.02 (0.97–1.07) | 1.01 (0.96–1.06) | 1.05 (1.00–1.09) | <0.001 |
| AFP (U/L) | 23.1 (4.4–516.1) | 21.2 (4.5–527.4) | 49.6 (4.1–476.3) | 0.829 |
| ALBI | −2.52 [(−2.72)–(−2.34)] | −2.53 [−(2.73)–(−2.34)] | −2.54 [−(2.67)–(−2.33)] | 0.863 |
| ALBI grade (1/2) | 137/208 | 104/161 | 33/47 | 0.748 |
| Child–Pugh score (5/6/7) | 276/53/16 | 211/39/15 | 65/14/1 | 0.234 |
| Child–Pugh grade (A/B) | 329/16 | 250/15 | 79/1 | 0.100 |
| MELD | 4.8 (2.9–6.3) | 4.6 (2.6–6.2) | 5.4 (3.9–7.3) | 0.012 |
| Cirrhosis (yes/no) | 120/225 | 90/175 | 30/50 | 0.560 |
| CSPH (yes/no) | 39/306 | 29/236 | 10/70 | 0.700 |
| Splenomegaly (yes/no) | 101/244 | 83/182 | 18/62 | 0.129 |
| Ascite (yes/no) | 22/323 | 19/246 | 3/77 | 0.273 |
| Tumor size (cm) | 5.4 (3.5–8.3) | 5.7 (3.6–8.4) | 4.5 (3.0–7.5) | 0.107 |
| BCLC stage (0/A/B/C) | 19/222/62/42 | 14/163/49/39 | 5/59/13/3 | 0.051 |
| TLV (mL) | 1242.4 (1083.4–1528.2) | 1242.4 (1086.1–1531.2) | 1230.6 (1070.5–1526.0) | 0.707 |
| RLV (mL) | 428.0 (234.7–687.5) | 433.1 (234.7–704.9) | 366.1 (226.1–633.3) | 0.229 |
| LRV | 788.6 (643.5–963.1) | 788.6 (631.6–957.7) | 787.2 (689.9–1003.6) | 0.465 |
| LRV ratio | 0.67 (0.50–0.80) | 0.66 (0.48–0.79) | 0.69 (0.54–0.80) | 0.186 |
| Symptomatic PHLF (yes/no) | 107/238 | 80/185 | 27/53 | 0.546 |
| Variables | Univariate Analysis | p-Value | Multivariate Analysis | p-Value |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | |||
| Sex, female vs. male | 0.791 (0.320–1.953) | 0.791 | − | − |
| Age (years) | 1.003 (0.981–1.025) | 0.811 | − | − |
| TBIL (umol/L) | 1.033 (0.998–1.069) | 0.062 | − | − |
| ALB (g/L) | 0.900 (0.838–0.967) | 0.004 | − | − |
| CREA (umol/L) | 0.997 (0.988–1.006) | 0.562 | − | − |
| ALT (U/L) | 1.001 (0.998–1.005) | 0.446 | − | − |
| AST (U/L) | 1.002 (0.999–1.006) | 0.234 | − | − |
| GGT (U/L) | 1.003 (1.000–1.005) | 0.024 | − | − |
| PT (s) | 1.343 (1.058–1.706) | 0.015 | − | − |
| INR | 2461.350 (70.906–85,440.280) | <0.001 | 2424.484 (49.342–119,130.427) | <0.001 |
| AFP (U/L) | 1.000(1.000–1.000) | 0.244 | − | − |
| ALBI score | 4.533 (1.947–10.557) | <0.001 | − | − |
| Child–Pugh score | 2.031 (1.292–3.193) | 0.002 | − | − |
| Child–Pugh grade, B vs. A | 3.782 (1.299–11.013) | 0.015 | − | − |
| MELD | 1.115(1.018–1.222) | 0.019 | − | − |
| Cirrhosis, yes vs. no | 2.499 (1.450–4.307) | 0.001 | − | − |
| CSPH, yes vs. no | 3.308 (1.507–7.260) | 0.003 | 4.670 (0.001–0.023) | 0.001 |
| Splenomegaly, yes vs. no | 1.618 (0.931–2.811) | 0.088 | − | − |
| Ascites, yes vs. no | 2.218 (0.865–5.689) | 0.097 | − | − |
| Tumor size (cm) | 1.177 (1.090–1.272) | <0.001 | − | − |
| BCLC stage | 1.536 (1.113–2.118) | 0.009 | − | − |
| TLV (mL) | 1.001 (1.000–1.002) | 0.001 | − | − |
| RLV (mL) | 1.002 (1.001–1.003) | <0.001 | − | − |
| LRV (mL) | 0.997 (0.996–0.998) | <0.001 | − | − |
| LRV ratio | 0.009 (0.002–0.039) | <0.001 | 0.004 (0.001–0.023) | <0.001 |
| Model | AUC (CI) | Accuracy ±STD | Sensitivity ±STD | Specificity ±STD | PPV ±STD | NPV ±STD |
|---|---|---|---|---|---|---|
| Radiomics | 0.746 (0.681–0.811) | 0.698 ± 0.054 | 0.725 ± 0.064 | 0.686 ± 0.098 | 0.511 ± 0.060 | 0.853 ± 0.019 |
| Clinical | 0.809 (0.715–0.902) | 0.739 ± 0.051 | 0.713 ± 0.170 | 0.751 ± 0.035 | 0.549 ± 0.057 | 0.865 ± 0.078 |
| Clinical–radiomics | 0.867 (0.787–0.947) | 0.800 ± 0.081 | 0.800 ± 0.0.073 | 0.800 ± 0.103 | 0.652 ± 0.120 | 0.901 ± 0.035 |
| Model | AUC | Accuracy | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|
| Radiomics | 0.784 | 0.725 | 0.660 | 0.754 | 0.581 | 0.816 |
| Clinical | 0.684 | 0.650 | 0.550 | 0.698 | 0.484 | 0.755 |
| Clinical–radiomics | 0.822 | 0.750 | 0.704 | 0.773 | 0.612 | 0.836 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhong, X.; Salahuddin, Z.; Chen, Y.; Woodruff, H.C.; Long, H.; Peng, J.; Xie, X.; Lin, M.; Lambin, P. An Interpretable Radiomics Model Based on Two-Dimensional Shear Wave Elastography for Predicting Symptomatic Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma. Cancers 2023, 15, 5303. https://doi.org/10.3390/cancers15215303
Zhong X, Salahuddin Z, Chen Y, Woodruff HC, Long H, Peng J, Xie X, Lin M, Lambin P. An Interpretable Radiomics Model Based on Two-Dimensional Shear Wave Elastography for Predicting Symptomatic Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma. Cancers. 2023; 15(21):5303. https://doi.org/10.3390/cancers15215303
Chicago/Turabian StyleZhong, Xian, Zohaib Salahuddin, Yi Chen, Henry C. Woodruff, Haiyi Long, Jianyun Peng, Xiaoyan Xie, Manxia Lin, and Philippe Lambin. 2023. "An Interpretable Radiomics Model Based on Two-Dimensional Shear Wave Elastography for Predicting Symptomatic Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma" Cancers 15, no. 21: 5303. https://doi.org/10.3390/cancers15215303
APA StyleZhong, X., Salahuddin, Z., Chen, Y., Woodruff, H. C., Long, H., Peng, J., Xie, X., Lin, M., & Lambin, P. (2023). An Interpretable Radiomics Model Based on Two-Dimensional Shear Wave Elastography for Predicting Symptomatic Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma. Cancers, 15(21), 5303. https://doi.org/10.3390/cancers15215303








