Penile-Sparing Surgery for Tumour Recurrence after Previous Glansectomy/Partial Penectomy: Treatment Feasibility and Oncological Outcomes
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Penile-Sparing Surgery
2.3. Variable Definitions and Statistical Analyses
3. Results
3.1. Descriptive Analyses (Table 1)
3.2. Perioperative Findings (Table 2)
3.3. Findings at Follow-Up (Table 3)
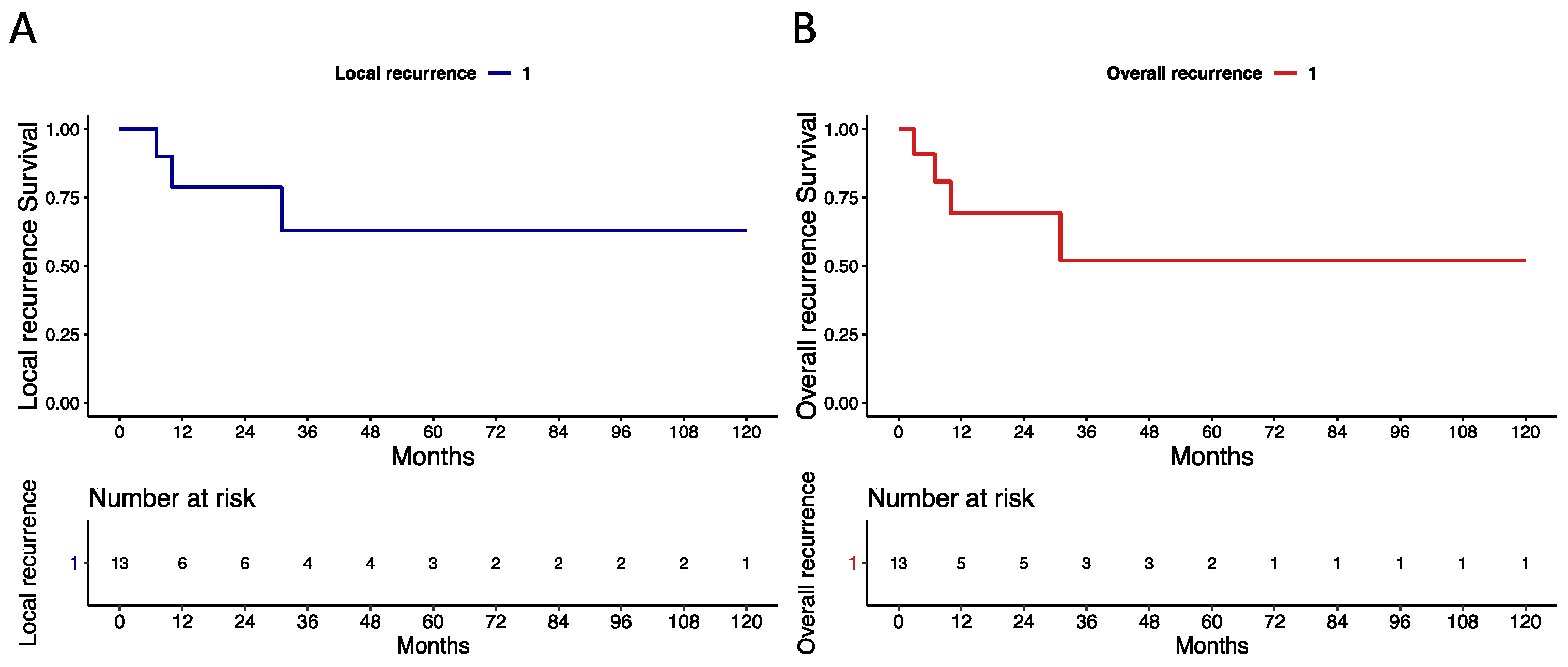
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hakenberg, O.W.; Compérat, E.M.; Minhas, S.; Necchi, A.; Protzel, C.; Watkin, N. EAU guidelines on penile cancer: 2014 update. Eur. Urol. 2015, 67, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Lindner, A.K.; Schachtner, G.; Steiner, E.; Kroiss, A.; Uprimny, C.; Steinkohl, F.; Horninger, W.; Heidegger, I.; Madersbacher, S.; Pichler, R. Organ-sparing surgery of penile cancer: Higher rate of local recurrence yet no impact on overall survival. World J. Urol. 2020, 38, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Djajadiningrat, R.S.; van Werkhoven, E.; Meinhardt, W.; van Rhijn, B.W.; Bex, A.; van der Poel, H.G.; Horenblas, S. Penile sparing surgery for penile cancer—Does it affect survival? J. Urol. 2014, 192, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, A.; Chipollini, J.; Yan, S.; Ottenhof, S.R.; Tang, D.H.; Draeger, D.; Protzel, C.; Zhu, Y.; Ye, D.-W.; Hakenberg, O.W.; et al. Penile Sparing Surgery for Penile Cancer: A Multicenter International Retrospective Cohort. J. Urol. 2018, 199, 1233–1237. [Google Scholar] [CrossRef]
- Luzzago, S.; Serino, A.; Aurilio, G.; Mistretta, F.A.; Piccinelli, M.L.; Lorusso, V.; Morelli, M.; Bianchi, R.; Catellani, M.; Cozzi, G.; et al. Penile-sparing surgery for patients with superficial or initially invasive squamous cell carcinoma of the penis: Long-term oncological outcomes. Urol. Oncol. Semin. Orig. Investig. 2021, 39, 736.e1–736.e7. [Google Scholar] [CrossRef]
- Anastasiadis, E.; Ayres, B.; Watkin, N. Update on penile sparing surgery for penile cancer. Curr. Opin. Urol. 2021, 32, 1–7. [Google Scholar] [CrossRef]
- Kokorovic, A.; Duplisea, J.; Qiao, W.; McCormick, B.; Adibi, M.; Papadopoulos, J.; Ramirez, G.; Rao, P.; Tamboli, P.; Pettaway, C. Oncologic outcomes and subsequent treatment following organ sparing surgery for penile carcinoma: The University of Texas M.D. Anderson Cancer Center Experience. Urol. Oncol. Semin. Orig. Investig. 2021, 39, 302.e19–302.e27. [Google Scholar] [CrossRef]
- Albersen, M.; Parnham, A.; Joniau, S.; Sahdev, V.; Christodoulidou, M.; Castiglione, F.; Nigam, R.; Malone, P.; Freeman, A.; Jameson, C.; et al. Predictive factors for local recurrence after glansectomy and neoglans reconstruction for penile squamous cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 141–146. [Google Scholar] [CrossRef]
- Roussel, E.; Peeters, E.; Vanthoor, J.; Bozzini, G.; Muneer, A.; Ayres, B.; Sri, D.; Watkin, N.; Bhattar, R.; Parnham, A.; et al. Predictors of local recurrence and its impact on survival after glansectomy for penile cancer: Time to challenge the dogma? BJU Int. 2020, 127, 606–613. [Google Scholar] [CrossRef]
- Saidian, A.; Ceballos, B.; Necchi, A.; Baumgarten, A.S.; Spiess, P.E. Salvage therapy for localized recurrences of penile cancer. Curr. Opin. Urol. 2021, 31, 214–219. [Google Scholar] [CrossRef]
- Bissada, N.K.; Yakout, H.H.; Fahmy, W.E.; Gayed, M.S.; Touijer, A.K.; Greene, G.F.; Hanash, K.A. Multi-institutional long-term experience with conservative surgery for invasive penile carcinoma. J. Urol. 2003, 169, 500–502. [Google Scholar] [CrossRef] [PubMed]
- Feldman, A.S.; McDougal, W.S. Long-term outcome of excisional organ sparing surgery for carcinoma of the penis. J. Urol. 2011, 186, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- Bandieramonte, G.; Colecchia, M.; Mariani, L.; Vullo, S.L.; Pizzocaro, G.; Piva, L.; Nicolai, N.; Salvioni, R.; Lezzi, V.; Stefanon, B.; et al. Peniscopically Controlled CO2 Laser Excision for Conservative Treatment of In Situ and T1 Penile Carcinoma: Report on 224 Patients. Eur. Urol. 2008, 54, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Musi, G.; Russo, A.; Conti, A.; Mistretta, F.A.; Di Trapani, E.; Luzzago, S.; Bianchi, R.; Renne, G.; Ramoni, S.; Ferro, M.; et al. Thulium–yttrium–aluminium–garnet (Tm:YAG) laser treatment of penile cancer: Oncological results, functional outcomes, and quality of life. World J. Urol. 2017, 36, 265–270. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Croghan, S.M.; Compton, N.; E Daniels, A.; Fitzgibbon, L.; Daly, P.J.; Cullen, I.M. Phallus Preservation in Penile Cancer Surgery: Patient-reported Aesthetic & Functional Outcomes. Urology 2021, 152, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.A.; Renshaw, A.A.; Loughlin, K.R. Squamous cell carcinoma of the penis and microscopic pathologic margins: How much margin is needed for local cure? Cancer 1999, 85, 1565–1568. [Google Scholar] [CrossRef]
- Minhas, S.; Kayes, O.; Hegarty, P.; Kumar, P.; Freeman, A.; Ralph, D. What surgical resection margins are required to achieve oncological control in men with primary penile cancer? BJU Int. 2005, 96, 1040–1043. [Google Scholar] [CrossRef]
- Gunia, S.; Koch, S.; Jain, A.; May, M. Does the width of the surgical margin of safety or premalignant dermatoses at the negative surgical margin affect outcome in surgically treated penile cancer? J. Clin. Pathol. 2014, 67, 268–271. [Google Scholar] [CrossRef]
- Slaton, J.W.; Morgenstern, N.; Levy, D.A.; Santos, M.W.; Tamboli, P.; Ro, J.Y.; Ayala, A.G.; Pettaway, C.A. Tumor stage, vascular invasion and the percentage of poorly differentiated cancer: Independent prognosticators for inguinal lymph node metastasis in penile squamous cancer. J. Urol. 2001, 165, 1138–1142. [Google Scholar] [CrossRef]
- Graafland, N.M.; Lam, W.; Leijte, J.A.; Yap, T.; Gallee, M.P.; Corbishley, C.; van Werkhoven, E.; Watkin, N.; Horenblas, S. Prognostic factors for occult inguinal lymph node involvement in penile carcinoma and assessment of the high-risk EAU subgroup: A two-institution analysis of 342 clinically node-negative patients. Eur. Urol. 2010, 58, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Ficarra, V.; Zattoni, F.; Cunico, S.C.; Galetti, T.P.; Luciani, L.; Fandella, A.; Guazzieri, S.; Maruzzi, D.; Sava, T.; Siracusano, S.; et al. Lymphatic and vascular embolizations are independent predictive variables of inguinal lymph node involvement in patients with squamous cell carcinoma of the penis: Gruppo Uro-Oncologico del Nord Est (Northeast Uro-Oncological Group) Penile Cancer Data Bas. Cancer 2005, 103, 2507–2516. [Google Scholar] [CrossRef] [PubMed]

| Age (Years) | Median (IQR) | 60 (53–63) |
|---|---|---|
| CCI, n (%) | 1 | 4 (30.5) |
| 2 | 4 (30.5) | |
| ≥3 | 5 (39.0) | |
| BMI | Median (IQR) | 27 (26–32) |
| Smoking | No | 8 (61.0) |
| Yes | 5 (39.0) | |
| Diabetes Mellitus | No | 10 (77.0) |
| Yes | 3 (23.0) | |
| HIV | No/Unknown | 12 (92.5) |
| Yes | 1 (7.5) | |
| HPV | No/Unknown | 12 (92.5) |
| Yes | 1 (7.5) | |
| Previous surgery, n (%) | Partial/total glansectomy | 11 (84.5) |
| Partial penectomy | 2 (15.5) | |
| Previous tumour size (mm) | Median (IQR) | 25 (20–30) |
| Previous histology, n (%) | Squamous cell | 11 (85.0) |
| Verrucous | 1 (7.5) | |
| Epidermoid | 1 (7.5) | |
| Previous T stage, n (%) | Unknown | 1 (7.5) |
| Tis | 1 (7.5) | |
| T1 | 5 (39.0) | |
| T2 | 6 (46.0) | |
| Previous tumour grade, n (%) | Gx | 1 (7.5) |
| G1 | 2 (15.0) | |
| G2 | 4 (30.5) | |
| G3 | 6 (47.0) | |
| Clear margin (mm) | Median (IQR) | 4.5 (3–6) |
| Previous N stage, n (%) | Nx | 4 (31.5) |
| N0 | 8 (61.0) | |
| N1 | 1 (7.5) |
| Patient | Previous Surgery | Previous Histology | Age | Time to Surgery (Months) | Type of Surgery | Setting (LOS) | Lesion Site | Lesion Size (mm) | Histology | CLAVIEN– DINDO |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Glansectomy + iLND | pT1N0G1 squamous | 52 | 56 | Circumcision + excision | Outpatient (1) | Neoglans + foreskin | N.A. | N.A. | 0 |
| 2 | Glansectomy + iLND | pT1N0G2 squamous | 50 | 5 | Excision | Outpatient (1) | Neoglans | N.A. | pTaNxG1 squamous | 0 |
| 3 | Glansectomy | pT2NxG2 squamous | 53 | 9 | Circumcision + excision | Outpatient (1) | Neoglans + foreskin | N.A. | N.A. | 0 |
| 4 | Partial penectomy | pTisNxG3 squamous | 54 | 142 | Excision | Outpatient (1) | Neoglans | 16 | pT1NxGx squamous | 0 |
| 5 | Glansectomy + iLND | pTxN0Gx squamous | 75 | 13 | Laser ablation | Outpatient (1) | Neoglans | 6 | pT1NxGx squamous | 0 |
| 6 | Glansectomy + iLND | pT1N0G3 squamous | 34 | 151 | Laser ablation | Outpatient (1) | Neoglans | 5 | N.A. | 0 |
| 7 | Partial penectomy + iLND | pT2N1G3 epidermoid | 59 | 80 | Excision | Outpatient (1) | Neoglans | 7 | PeINNxG1 squamous | 0 |
| 8 | Partial glansectomy + iLND | pT2N0G3 squamous | 60 | 91 | Excision | Outpatient (1) | Urethra | N.A. | pTisNxG3 squamous | 0 |
| 9 | Glansectomy + sLND | pT2N0G2 squamous | 60 | 13 | Excision | Outpatient (1) | Neoglans | 4 | PeINNxG3 squamous | 0 |
| 10 | Glansectomy + sLND | pT2N0G2 verrucous | 62 | 82 | Laser ablation | Outpatient (1) | Neoglans | 15 | pT1NxG1 squamous | 0 |
| 11 | Glansectomy | pT1NxG1 squamous | 69 | 88 | Laser ablation | Outpatient (1) | Neoglans | 5 | PeINNxG1 squamous | 0 |
| 12 | Partial glansectomy | pT1NXG3 squamous | 70 | 45 | Laser ablation | Outpatient (1) | Neoglans | 9 | PeINNxG3 squamous | 0 |
| 13 | Partial glansectomy + iLND | pT2N0G3 squamous | 63 | 12 | Excision | Inpatient (4) | Neoglans | 18 | pT1NxG2 squamous | 2 (Antibiotic) |
| Patient | Type of Surgery | Histology | Follow-Up (Months) | Local Recurrence | Time Local Recurrence (Months) | Surgery Local Recurrence | Histology Local Recurrence | Regional Recurrence | Time Regional Recurrence (Months) | Surgery Regional Recurrence | Histology Regional Recurrence | Status |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Circumcision + excision | N.A. | 120 | No | - | - | - | No | - | - | - | NED |
| 2 | Excision | pTaNxG1 squamous | 44 | Yes | 7 | Excision | pTaG1 squamous | No | 7 | sLND | pN0 | NED |
| 3 | Circumcision + excision | N.A. | 110 | No | - | - | - | Yes | 3 | iLND | pN1 | NED |
| 4 | Excision | pT1NxGx squamous | 4 | No | - | - | - | No | - | - | - | NED |
| 5 | Laser ablation | pT1NxGx squamous | 71 | No | - | - | - | No | - | - | - | NED |
| 6 | Laser ablation | N.A. | LOST | No | - | - | - | No | - | - | - | LOST |
| 7 | Excision | PeINNxG1 squamous | 52 | No | - | - | - | No | - | - | - | NED |
| 8 | Excision | pTisNxG3 squamous | 29 | No | - | - | - | No | - | - | - | NED |
| 9 | Excision | PeINNxG3 squamous | 73 | Yes | 31 | Penectomy | pT1G2 squamous | No | 31 | sLND | pN0 | NED |
| 10 | Laser ablation | pT1NxG1 squamous | 37 | Yes | 10 | Penectomy | pT2G3 verrucous | No | - | - | - | NED |
| 11 | Laser ablation | PeINNxG1 squamous | 9 | No | - | - | - | No | - | - | - | NED |
| 12 | Laser ablation | PeINNxG3 squamous | 0 | No | - | - | - | No | - | - | - | NED |
| 13 | Excision | pT1NxG2 squamous | 10 | No | - | - | - | No | - | - | - | NED |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musi, G.; Molinari, F.; Mistretta, F.A.; Piccinelli, M.L.; Guzzo, S.; Tozzi, M.; Lievore, E.; Blezien, O.; Fontana, M.; Cioffi, A.; et al. Penile-Sparing Surgery for Tumour Recurrence after Previous Glansectomy/Partial Penectomy: Treatment Feasibility and Oncological Outcomes. Cancers 2023, 15, 4807. https://doi.org/10.3390/cancers15194807
Musi G, Molinari F, Mistretta FA, Piccinelli ML, Guzzo S, Tozzi M, Lievore E, Blezien O, Fontana M, Cioffi A, et al. Penile-Sparing Surgery for Tumour Recurrence after Previous Glansectomy/Partial Penectomy: Treatment Feasibility and Oncological Outcomes. Cancers. 2023; 15(19):4807. https://doi.org/10.3390/cancers15194807
Chicago/Turabian StyleMusi, Gennaro, Filippo Molinari, Francesco A. Mistretta, Mattia Luca Piccinelli, Sonia Guzzo, Marco Tozzi, Elena Lievore, Oskar Blezien, Matteo Fontana, Antonio Cioffi, and et al. 2023. "Penile-Sparing Surgery for Tumour Recurrence after Previous Glansectomy/Partial Penectomy: Treatment Feasibility and Oncological Outcomes" Cancers 15, no. 19: 4807. https://doi.org/10.3390/cancers15194807
APA StyleMusi, G., Molinari, F., Mistretta, F. A., Piccinelli, M. L., Guzzo, S., Tozzi, M., Lievore, E., Blezien, O., Fontana, M., Cioffi, A., Cullurà, D., Verri, E., Cossu Rocca, M., Nolè, F., Ferro, M., de Cobelli, O., & Luzzago, S. (2023). Penile-Sparing Surgery for Tumour Recurrence after Previous Glansectomy/Partial Penectomy: Treatment Feasibility and Oncological Outcomes. Cancers, 15(19), 4807. https://doi.org/10.3390/cancers15194807





