Patients Undergoing Systemic Anti-Cancer Therapy Who Require Surgical Intervention: What Surgeons Need to Know
Abstract
:Simple Summary
Abstract
1. Introduction
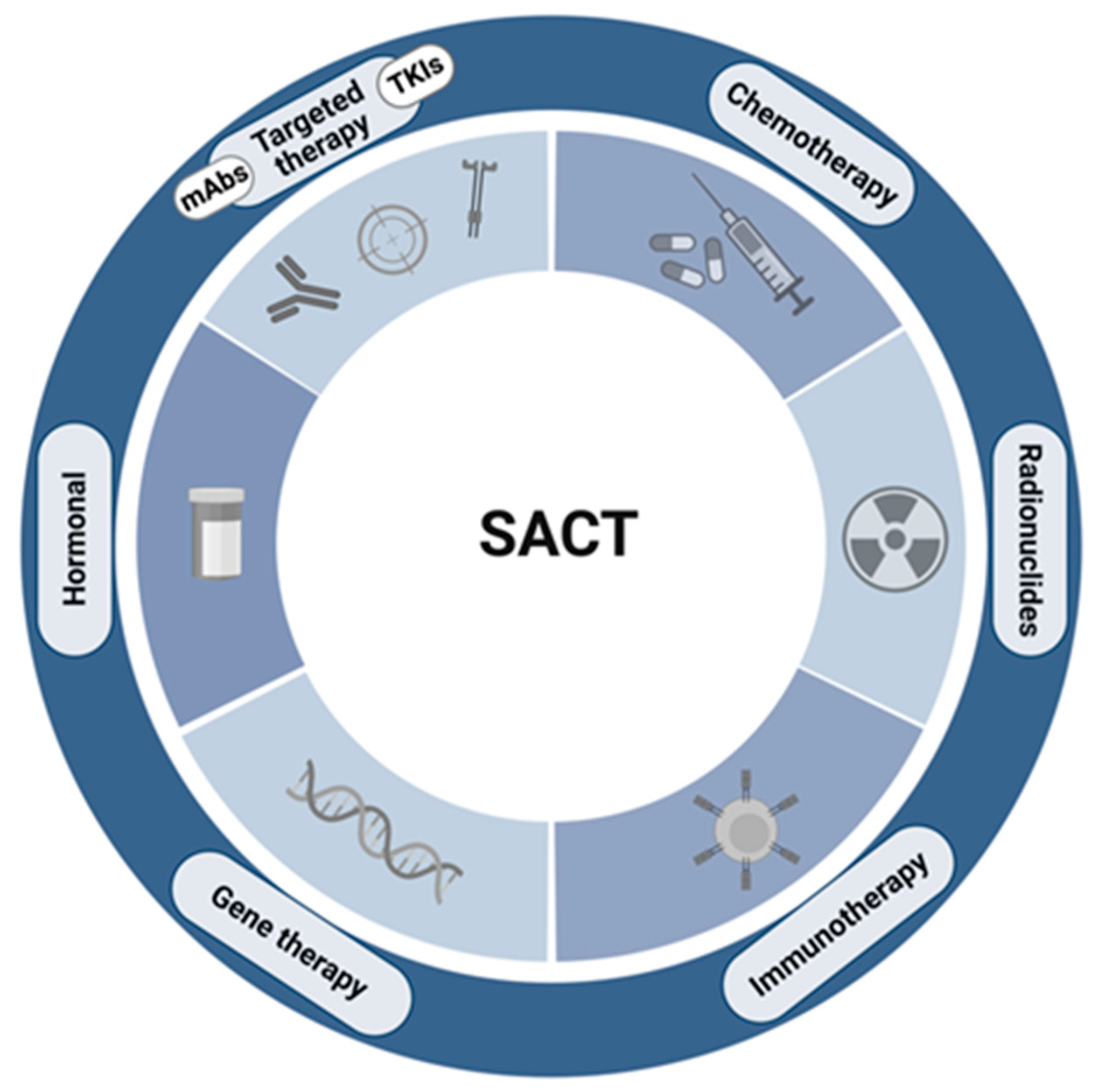
1.1. “Chemotherapy” in the 21st Century
1.2. A Brief Focus on the Wound-Healing Process
2. The Importance of Neutropenia
Colony Stimulating Factors: The Guidance
3. Thrombocytopenia
3.1. Clinical Considerations for a Patient with Thrombocytopenia Receiving Chemotherapy
3.2. Management of Thrombocytopenia: Is There a Role for Thrombopoietin Mimetics?
4. Chemotherapy
4.1. Neoadjuvant Chemotherapy: Is There Significant Risk?
4.2. Neoadjuvant Chemotherapy and Fitness for Surgery
5. Targeted Therapies: Vascular Endothelial Growth Factor Inhibition
5.1. Monoclonal Antibody Inhibitors
5.2. Does a Higher Dose of a VEGF Inhibitor Equal Higher Risk?
5.3. Tyrosine Kinase Inhibitors
5.4. VEGF Inhibitor Pharmacokinetics
6. Hormonal Therapies and Surgical Risk
7. Surgical Complications in Patients Receiving Radionuclide Therapy
8. Immunotherapy
9. Surgical Considerations in the Elective Setting
10. Surgical Considerations in the Emergency Setting
11. Patient Participation in Clinical Trials: Expedited Safety Reporting
12. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Wilkinson, H.N.; Hardman, M.J. Wound Healing: Cellular Mechanisms and Pathological Outcomes. Open Biol. 2020, 10, 200223. [Google Scholar] [CrossRef] [PubMed]
- Du, V.X.; Huskens, D.; Maas, C.; Al Dieri, R.; de Groot, P.G.; de Laat, B. New Insights into the Role of Erythrocytes in Thrombus Formation. Semin. Thromb. Hemost. 2014, 40, 72–80. [Google Scholar] [PubMed]
- Hathcock, J.J. Flow Effects on Coagulation and Thrombosis. Arter. Thromb. Vasc. Biol. 2006, 26, 1729–1737. [Google Scholar] [CrossRef]
- Golebiewska, E.M.; Poole, A.W. Platelet Secretion: From Haemostasis to Wound Healing and Beyond. Blood Rev. 2015, 29, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.H.; Liu, W.; Borjesson, D.L.; Curry, F.R.; Miller, L.S.; Cheung, A.L.; Liu, F.T.; Isseroff, R.R.; Simon, S.I. Dynamics of Neutrophil Infiltration During Cutaneous Wound Healing and Infection Using Fluorescence Imaging. J. Investig. Dermatol. 2008, 128, 1812–1820. [Google Scholar] [CrossRef] [Green Version]
- Gushiken, L.F.S.; Beserra, F.P.; Bastos, J.K.; Jackson, C.J.; Pellizzon, C.H. Cutaneous Wound Healing: An Update from Physiopathology to Current Therapies. Life 2021, 11, 665. [Google Scholar] [CrossRef]
- Singer, A.J.; Clark, R.A. Cutaneous Wound Healing. N. Engl. J. Med. 1999, 341, 738–746. [Google Scholar] [CrossRef]
- Li, Y.; Klippel, Z.; Shih, X.; Reiner, M.; Wang, H.; Page, J.H. Relationship between Severity and Duration of Chemotherapy-Induced Neutropenia and Risk of Infection among Patients with Nonmyeloid Malignancies. Support. Care Cancer 2016, 24, 4377–4383. [Google Scholar] [CrossRef]
- Hashiguchi, Y.; Kasai, M.; Fukuda, T.; Ichimura, T.; Yasui, T.; Sumi, T. Chemotherapy-Induced Neutropenia and Febrile Neutropenia in Patients with Gynecologic Malignancy. Anticancer Drugs 2015, 26, 1054–1060. [Google Scholar] [CrossRef] [Green Version]
- Coccolini, F.; Improta, M.; Cicuttin, E.; Catena, F.; Sartelli, M.; Bova, R.; Angelis, N.D.; Gitto, S.; Tartaglia, D.; Cremonini, C.; et al. Surgical Site Infection Prevention and Management in Immunocompromised Patients: A Systematic Review of the Literature. World J. Emerg. Surg. 2021, 16, 33. [Google Scholar] [CrossRef]
- Jolissaint, J.S.; Harary, M.; Saadat, L.V.; Madenci, A.L.; Dieffenbach, B.V.; Al Natour, R.H.; Tavakkoli, A. Timing and Outcomes of Abdominal Surgery in Neutropenic Patients. J. Gastrointest. Surg. 2019, 23, 643–650. [Google Scholar] [CrossRef]
- Crawford, J.; Ozer, H.; Stoller, R.; Johnson, D.; Lyman, G.; Tabbara, I.; Kris, M.; Grous, J.; Picozzi, V.; Rausch, G.; et al. Reduction by Granulocyte Colony-Stimulating Factor of Fever and Neutropenia Induced by Chemotherapy in Patients with Small-Cell Lung Cancer. N. Engl. J. Med. 1991, 325, 164–170. [Google Scholar] [CrossRef]
- Smith, T.J.; Bohlke, K.; Lyman, G.H.; Carson, K.R.; Crawford, J.; Cross, S.J.; Goldberg, J.M.; Khatcheressian, J.L.; Leighl, N.B.; Perkins, C.L.; et al. Recommendations for the Use of Wbc Growth Factors: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2015, 33, 3199–3212. [Google Scholar] [CrossRef] [Green Version]
- Smith, T.J.; Khatcheressian, J.; Lyman, G.H.; Ozer, H.; Armitage, J.O.; Balducci, L.; Bennett, C.L.; Cantor, S.B.; Crawford, J.; Cross, S.J.; et al. 2006 Update of Recommendations for the Use of White Blood Cell Growth Factors: An Evidence-Based Clinical Practice Guideline. J. Clin. Oncol. 2006, 24, 3187–3205. [Google Scholar] [CrossRef] [Green Version]
- Yeo, B.; Redfern, A.D.; Mouchemore, K.A.; Hamilton, J.A.; Anderson, R.L. The Dark Side of Granulocyte-Colony Stimulating Factor: A Supportive Therapy with Potential to Promote Tumour Progression. Clin. Exp. Metastasis 2018, 35, 255–267. [Google Scholar] [CrossRef]
- Liu, Z.; Zhu, Y.; Wang, Y.; Fu, Q.; Fu, H.; Wang, Z.; Zhang, J.; Li, G.; Xu, J.; Dai, B. Prognostic Value of Granulocyte Colony-Stimulating Factor in Patients with Non-Metastatic Clear Cell Renal Cell Carcinoma. Oncotarget 2017, 8, 69961–69971. [Google Scholar] [CrossRef] [Green Version]
- Ten Berg, M.J.; van den Bemt, P.M.; Shantakumar, S.; Bennett, D.; Voest, E.E.; Huisman, A.; van Solinge, W.W.; Egberts, T.C. Thrombocytopenia in Adult Cancer Patients Receiving Cytotoxic Chemotherapy: Results from a Retrospective Hospital-Based Cohort Study. Drug Saf. 2011, 34, 1151–1160. [Google Scholar] [CrossRef]
- Kuter, D.J. Treatment of Chemotherapy-Induced Thrombocytopenia in Patients with Non-Hematologic Malignancies. Haematologica 2022, 107, 1243–1263. [Google Scholar] [CrossRef] [PubMed]
- Kuter, D.J. Managing Thrombocytopenia Associated with Cancer Chemotherapy. Oncology 2015, 29, 282–294. [Google Scholar] [PubMed]
- Schiffer, C.A.; Bohlke, K.; Delaney, M.; Hume, H.; Magdalinski, A.J.; McCullough, J.J.; Omel, J.L.; Rainey, J.M.; Rebulla, P.; Rowley, S.D.; et al. Platelet Transfusion for Patients with Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Yang, C.; Xia, Y.; Bertino, A.; Glaspy, J.; Roberts, M.; Kuter, D.J. Thrombocytopenia Caused by the Development of Antibodies to Thrombopoietin. Blood 2001, 98, 3241–3248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soff, G.A.; Ray-Coquard, I.; Rivera, L.J.M.; Fryzek, J.; Mullins, M.; Bylsma, L.C.; Park, J.K. Systematic Literature Review and Meta-Analysis on Use of Thrombopoietic Agents for Chemotherapy-Induced Thrombocytopenia. PLoS ONE 2022, 17, e0257673. [Google Scholar] [CrossRef]
- Griffiths, E.A.; Roy, V.; Alwan, L.; Bachiashvili, K.; Baird, J.; Cool, R.; Dinner, S.; Geyer, M.; Glaspy, J.; Gojo, I.; et al. Nccn Guidelines® Insights: Hematopoietic Growth Factors, Version 1.2022: Featured Updates to the Nccn Guidelines. J. Natl. Compr. Cancer Netw. 2022, 20, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, P.L.; Garcia-Manero, G.; Moore, M.; Damon, L.; Roboz, G.; Hu, K.; Yang, A.S.; Franklin, J. A Randomized Controlled Trial of Romiplostim in Patients with Low- or Intermediate-Risk Myelodysplastic Syndrome Receiving Decitabine. Leuk. Lymphoma 2013, 54, 321–328. [Google Scholar] [CrossRef]
- Fenaux, P.; Muus, P.; Kantarjian, H.; Lyons, R.M.; Larson, R.A.; Sekeres, M.A.; Becker, P.S.; Orejudos, A.; Franklin, J. Romiplostim Monotherapy in Thrombocytopenic Patients with Myelodysplastic Syndromes: Long-Term Safety and Efficacy. Br. J. Haematol. 2017, 178, 906–913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deptuła, M.; Zieliński, J.; Wardowska, A.; Pikuła, M. Wound Healing Complications in Oncological Patients: Perspectives for Cellular Therapy. Postep. Dermatol. Alergol. 2019, 36, 139–146. [Google Scholar] [CrossRef]
- Payne, W.G.; Naidu, D.K.; Wheeler, C.K.; Barkoe, D.; Mentis, M.; Salas, R.E.; Smith, D.J., Jr.; Robson, M.C. Wound Healing in Patients with Cancer. Eplasty 2008, 8, e9. [Google Scholar] [PubMed]
- Lorentzen, T.; Heidemann, L.N.; Möller, S.; Bille, C. Impact of Neoadjuvant Chemotherapy on Surgical Complications in Breast Cancer: A Systematic Review and Meta-Analysis. Eur. J. Surg. Oncol. 2022, 48, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Sanford, R.A.; Lei, X.; Barcenas, C.H.; Mittendorf, E.A.; Caudle, A.S.; Valero, V.; Tripathy, D.; Giordano, S.H.; Chavez-MacGregor, M. Impact of Time from Completion of Neoadjuvant Chemotherapy to Surgery on Survival Outcomes in Breast Cancer Patients. Ann. Surg. Oncol. 2016, 23, 1515–1521. [Google Scholar] [CrossRef]
- Zhai, Y.; Zheng, Z.; Deng, W.; Yin, J.; Bai, Z.; Liu, X.; Zhang, J.; Zhang, Z. Interval Time between Neoadjuvant Chemotherapy and Surgery in Advanced Gastric Cancer Doesn’t Affect Outcome: A Meta Analysis. Front. Surg. 2022, 9, 1047456. [Google Scholar] [CrossRef]
- Cheong, C.K.; Nistala, K.R.Y.; Ng, C.H.; Syn, N.; Chang, H.S.Y.; Sundar, R.; Yang, S.Y.; Chong, C.S. Neoadjuvant Therapy in Locally Advanced Colon Cancer: A Meta-Analysis and Systematic Review. J. Gastrointest. Oncol. 2020, 11, 847–857. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Zhang, J.; Chen, D.; Wu, S.; Xue, P.; Zhu, K.; Xu, C.; Zhu, C.; Zhang, B. Neoadjuvant Chemoradiotherapy, Chemotherapy, and Radiotherapy Do Not Significantly Increase the Incidence of Anastomotic Leakage after Esophageal Cancer Surgery: A Meta-Analysis. Dis. Esophagus 2021, 35, doab089. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Xu, M.; Lou, Y.; Yuan, Y.; Wu, Y.; Zhang, L.; Xin, Y.; Zhou, F. Survival and Complications after Neoadjuvant Chemoradiotherapy Versus Neoadjuvant Chemotherapy for Esophageal Squamous Cell Cancer: A Meta-Analysis. PLoS ONE 2022, 17, e0271242. [Google Scholar] [CrossRef] [PubMed]
- An, J.Y.; Kim, K.M.; Kim, Y.M.; Cheong, J.-H.; Hyung, W.J.; Noh, S.H. Surgical Complications in Gastric Cancer Patients Preoperatively Treated with Chemotherapy: Their Risk Factors and Clinical Relevance. Ann. Surg. Oncol. 2012, 19, 2452–2458. [Google Scholar] [CrossRef]
- Reijneveld, E.A.E.; Bor, P.; Dronkers, J.J.; Argudo, N.; Ruurda, J.P.; Veenhof, C. Impact of Curative Treatment on the Physical Fitness of Patients with Esophageal Cancer: A Systematic Review and Meta-Analysis. Eur. J. Surg. Oncol. 2022, 48, 391–402. [Google Scholar] [CrossRef]
- West, M.A.; Loughney, L.; Lythgoe, D.; Barben, C.P.; Sripadam, R.; Kemp, G.J.; Grocott, M.P.W.; Jack, S. Effect of Prehabilitation on Objectively Measured Physical Fitness after Neoadjuvant Treatment in Preoperative Rectal Cancer Patients: A Blinded Interventional Pilot Study†. Br. J. Anaesth. 2015, 114, 244–251. [Google Scholar] [CrossRef] [Green Version]
- Tully, R.; Loughney, L.; Bolger, J.; Sorensen, J.; McAnena, O.; Collins, C.G.; Carroll, P.A.; Arumugasamy, M.; Murphy, T.J.; Robb, W.B.; et al. Working Group on behalf of the. The Effect of a Pre- and Post-Operative Exercise Programme Versus Standard Care on Physical Fitness of Patients with Oesophageal and Gastric Cancer Undergoing Neoadjuvant Treatment Prior to Surgery (the Periop-Og Trial): Study Protocol for a Randomised Controlled Trial. Trials 2020, 21, 638. [Google Scholar]
- Cohen, M.H.; Gootenberg, J.; Keegan, P.; Pazdur, R. Fda Drug Approval Summary: Bevacizumab (Avastin) Plus Carboplatin and Paclitaxel as First-Line Treatment of Advanced/Metastatic Recurrent Nonsquamous Non-Small Cell Lung Cancer. Oncologist 2007, 12, 713–718. [Google Scholar] [CrossRef]
- Jung, M.; Ryu, M.-H.; Oh, D.Y.; Kang, M.; Zang, D.Y.; Hwang, I.G.; Lee, K.-W.; Kim, K.H.; Shim, B.Y.; Song, E.K.; et al. Efficacy and Tolerability of Ramucirumab Monotherapy or in Combination with Paclitaxel in Gastric Cancer Patients from the Expanded Access Program Cohort by the Korean Cancer Study Group (Kcsg). Gastric Cancer 2018, 21, 819–830. [Google Scholar] [CrossRef] [Green Version]
- Garcia, J.; Hurwitz, H.I.; Sandler, A.B.; Miles, D.; Coleman, R.L.; Deurloo, R.; Chinot, O.L. Bevacizumab (Avastin®) in Cancer Treatment: A Review of 15 years of Clinical Experience and Future Outlook. Cancer Treat. Rev. 2020, 86, 102017. [Google Scholar] [CrossRef]
- Trichonas, G.; Kaiser, P.K. Aflibercept for the Treatment of Age-Related Macular Degeneration. Ophthalmol. Ther. 2013, 2, 89–98. [Google Scholar] [CrossRef] [Green Version]
- Ingram, I. Fda Approves Aflibercept (Zaltrap) for Metastatic Colorectal Cancer. Oncology 2012, 26, 842–873. [Google Scholar]
- Van Cutsem, E.; Rivera, F.; Berry, S.; Kretzschmar, A.; Michael, M.; DiBartolomeo, M.; Mazier, M.A.; Canon, J.L.; Georgoulias, V.; Peeters, M.; et al. Safety and Efficacy of First-Line Bevacizumab with Folfox, Xelox, Folfiri and Fluoropyrimidines in Metastatic Colorectal Cancer: The Beat Study. Ann. Oncol. 2009, 20, 1842–1847. [Google Scholar] [CrossRef] [PubMed]
- Kozloff, M.; Yood, M.U.; Berlin, J.; Flynn, P.J.; Kabbinavar, F.F.; Purdie, D.M.; Ashby, M.A.; Dong, W.; Sugrue, M.M.; Grothey, A.; et al. Clinical Outcomes Associated with Bevacizumab-Containing Treatment of Metastatic Colorectal Cancer: The Brite Observational Cohort Study. Oncology 2009, 14, 862–870. [Google Scholar] [CrossRef]
- Li, D.B.; Ye, F.; Wu, X.R.; Wu, L.P.; Chen, J.X.; Li, B.; Zhou, Y.M. Preoperative Administration of Bevacizumab Is Safe for Patients with Colorectal Liver Metastases. World J. Gastroenterol. 2013, 19, 761–768. [Google Scholar] [CrossRef]
- Yoshimoto, T.; Yoshikawa, K.; Higashijima, J.; Miyatani, T.; Tokunaga, T.; Nishi, M.; Takasu, C.; Kashihara, H.; Takehara, Y.; Shimada, M. Bevacizumab-Associated Intestinal Perforation and Perioperative Complications in Patients Receiving Bevacizumab. Ann. Gastroenterol. Surg. 2020, 4, 151–155. [Google Scholar] [CrossRef] [Green Version]
- Scappaticci, F.A.; Fehrenbacher, L.; Cartwright, T.; Hainsworth, J.D.; Heim, W.; Berlin, J.; Kabbinavar, F.; Novotny, W.; Sarkar, S.; Hurwitz, H. Surgical Wound Healing Complications in Metastatic Colorectal Cancer Patients Treated with Bevacizumab. J. Surg. Oncol. 2005, 91, 173–180. [Google Scholar] [CrossRef]
- Cortés, J.; Caralt, M.; Delaloge, S.; Cortes-Funes, H.; Pierga, J.-Y.; Pritchard, K.I.; Bollag, D.T.; Miles, D.W. Safety of Bevacizumab in Metastatic Breast Cancer Patients Undergoing Surgery. Eur. J. Cancer 2012, 48, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Tullemans, B.M.E.; Veninga, A.; Fernandez, D.I.; Aarts, M.J.B.; Eble, J.A.; van der Meijden, P.E.J.; Heemskerk, J.W.M.; Kuijpers, M.J.E. Multiparameter Evaluation of the Platelet-Inhibitory Effects of Tyrosine Kinase Inhibitors Used for Cancer Treatment. Int. J. Mol. Sci. 2021, 22, 11199. [Google Scholar] [CrossRef]
- Tullemans, B.M.E.; Heemskerk, J.W.M.; Kuijpers, M.J.E. Acquired Platelet Antagonism: Off-Target Antiplatelet Effects of Malignancy Treatment with Tyrosine Kinase Inhibitors. J. Thromb. Haemost. 2018, 16, 1686–1699. [Google Scholar] [CrossRef] [Green Version]
- Tullemans, B.M.E.; Fernández, D.I.; Veninga, A.; Baaten, C.; Peters, L.J.F.; Aarts, M.J.B.; Eble, J.A.; Campello, E.; Spiezia, L.; Simioni, P.; et al. Tyrosine Kinase Inhibitor Sunitinib Delays Platelet-Induced Coagulation: Additive Effects of Aspirin. Thromb. Haemost. 2022, 122, 92–104. [Google Scholar]
- Karam, J.A.; Devine, C.E.; Urbauer, D.L.; Lozano, M.; Maity, T.; Ahrar, K.; Tamboli, P.; Tannir, N.M.; Wood, C.G. Phase 2 Trial of Neoadjuvant Axitinib in Patients with Locally Advanced Nonmetastatic Clear Cell Renal Cell Carcinoma. Eur. Urol. 2014, 66, 874–880. [Google Scholar] [CrossRef] [Green Version]
- Stewart, G.D.; Welsh, S.J.; Ursprung, S.; Gallagher, F.A.; Jones, J.O.; Shields, J.; Smith, C.G.; Mitchell, T.J.; Warren, A.Y.; Bex, A.; et al. A Phase Ii Study of Neoadjuvant Axitinib for Reducing the Extent of Venous Tumour Thrombus in Clear Cell Renal Cell Cancer with Venous Invasion (Naxiva). Br. J. Cancer 2022, 127, 1051–1060. [Google Scholar] [CrossRef]
- McCormick, B.; Meissner, M.A.; Karam, J.A.; Wood, C.G. Surgical Complications of Presurgical Systemic Therapy for Renal Cell Carcinoma: A Systematic Review. Kidney Cancer 2017, 1, 115–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cowey, C.L.; Amin, C.; Pruthi, R.S.; Wallen, E.M.; Nielsen, M.E.; Grigson, G.; Watkins, C.; Nance, K.V.; Crane, J.; Jalkut, M.; et al. Neoadjuvant Clinical Trial with Sorafenib for Patients with Stage Ii or Higher Renal Cell Carcinoma. J. Clin. Oncol. 2010, 28, 1502–1507. [Google Scholar] [CrossRef] [Green Version]
- Harshman, L.C.; Yu, R.J.; Allen, G.I.; Srinivas, S.; Gill, H.S.; Chung, B.I. Surgical Outcomes and Complications Associated with Presurgical Tyrosine Kinase Inhibition for Advanced Renal Cell Carcinoma (Rcc). Urol. Oncol. Semin. Orig. Investig. 2013, 31, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-C.; Chen, C.-H.; Chen, T.-C.; Yeh, C.-N.; Yeh, T.-S. Preoperative Tyrosine Kinase Inhibitors Risks Bowel Anastomotic Healing in Patients with Advanced Primary and Recurrent/Metastatic Gastrointestinal Stromal Tumors—A Rose Has Its Thorns. Eur. J. Surg. Oncol. 2019, 45, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Schlumberger, M.; Tahara, M.; Wirth, L.J.; Robinson, B.; Brose, M.S.; Elisei, R.; Habra, M.A.; Newbold, K.; Shah, M.H.; Hoff, A.O.; et al. Lenvatinib Versus Placebo in Radioiodine-Refractory Thyroid Cancer. N. Engl. J. Med. 2015, 372, 621–630. [Google Scholar] [CrossRef] [Green Version]
- Cheng, C.; Nayernama, A.; Jones, S.C.; Casey, D.; Waldron, P.E. Wound Healing Complications with Lenvatinib Identified in a Pharmacovigilance Database. J. Oncol. Pharm. Pract. 2019, 25, 1817–1822. [Google Scholar] [CrossRef]
- Sun, L.; Ma, J.-T.; Zhang, S.-L.; Zou, H.-W.; Han, C.-B. Efficacy and Safety of Chemotherapy or Tyrosine Kinase Inhibitors Combined with Bevacizumab Versus Chemotherapy or Tyrosine Kinase Inhibitors Alone in the Treatment of Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Med. Oncol. 2015, 32, 34. [Google Scholar] [CrossRef]
- Huber, K.M.; Clayman, E.; Kumar, A.; Smith, P. The Impact of Perioperative Hormonal Therapy for Breast Cancer on Transverse Rectus Abdominis Myocutaneous Flap Abdominal Complications. Ann. Plast. Surg. 2018, 80, S348–S351. [Google Scholar] [CrossRef] [PubMed]
- Partelli, S.; Bertani, E.; Bartolomei, M.; Muffatti, F.; Grana, C.M.; Doglioni, C.; Fazio, N.; Falconi, M. Outcome of Surgical Resection after Neoadjuvant Peptide Receptor Radionuclide Therapy (Prrt) for Pancreatic Neuroendocrine Neoplasms: A Case-Matched Analysis. Endocr. Abstr. 2016, 46, P28. [Google Scholar] [CrossRef]
- Sangro, B.; Chan, S.L.; Meyer, T.; Reig, M.; El-Khoueiry, A.; Galle, P.R. Diagnosis and Management of Toxicities of Immune Checkpoint Inhibitors in Hepatocellular Carcinoma. J. Hepatol. 2020, 72, 320–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haanen, J.; Obeid, M.; Spain, L.; Carbonnel, F.; Wang, Y.; Robert, C.; Lyon, A.R.; Wick, W.; Kostine, M.; Peters, S.; et al. Management of Toxicities from Immunotherapy: Esmo Clinical Practice Guideline for Diagnosis, Treatment and Follow-up☆. Ann. Oncol. 2022, 33, 1217–1238. [Google Scholar] [CrossRef] [PubMed]
- Mays, A.C.; Yarlagadda, B.; Achim, V.; Jackson, R.; Pipkorn, P.; Huang, A.T.; Rajasekaran, K.; Sridharan, S.; Rosko, A.J.; Orosco, R.K.; et al. Examining the Relationship of Immunotherapy and Wound Complications Following Flap Reconstruction in Patients with Head and Neck Cancer. Head. Neck 2021, 43, 1509–1520. [Google Scholar] [CrossRef] [PubMed]
- Farha, N.; Alkhayyat, M.; Lindsey, A.; Mansoor, E.; Saleh, M.A. Immune Checkpoint Inhibitor Induced Colitis: A Nationwide Population-Based Study. Clin. Res. Hepatol. Gastroenterol. 2022, 46, 101778. [Google Scholar] [CrossRef]
- Marthey, L.; Mateus, C.; Mussini, C.; Nachury, M.; Nancey, S.; Grange, F.; Zallot, C.; Peyrin-Biroulet, L.; Rahier, J.F.; de Beauregard, M.B.; et al. Cancer Immunotherapy with Anti-Ctla-4 Monoclonal Antibodies Induces an Inflammatory Bowel Disease. J. Crohns Colitis 2016, 10, 395–401. [Google Scholar] [CrossRef]
- Hong, Z.N.; Weng, K.; Peng, K.; Chen, Z.; Lin, J.; Kang, M. Neoadjuvant Immunotherapy Combined Chemotherapy Followed by Surgery Versus Surgery Alone for Locally Advanced Esophageal Squamous Cell Carcinoma: A Propensity Score-Matched Study. Front. Oncol. 2021, 11, 797426. [Google Scholar] [CrossRef] [PubMed]
- Hompes, D.; Ruers, T. Review: Incidence and Clinical Significance of Bevacizumab-Related Non-Surgical and Surgical Serious Adverse Events in Metastatic Colorectal Cancer. Eur. J. Surg. Oncol. (EJSO) 2011, 37, 737–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulkarni, N.; Arulampalam, T. Laparoscopic Surgery Reduces the Incidence of Surgical Site Infections Compared to the Open Approach for Colorectal Procedures: A Meta-Analysis. Tech. Coloproctol. 2020, 24, 1017–1024. [Google Scholar] [CrossRef]
- Caroff, D.A.; Chan, C.; Kleinman, K.; Calderwood, M.S.; Wolf, R.; Wick, E.C.; Platt, R.; Huang, S. Association of Open Approach vs. Laparoscopic Approach with Risk of Surgical Site Infection after Colon Surgery. JAMA Netw. Open 2019, 2, e1913570. [Google Scholar] [CrossRef] [PubMed]

| Molecule | Mechanism | Half-Life | Interval Recommendation * |
|---|---|---|---|
| Bevacizumab | mAb VEGF-A inhibition | 20 days | Discontinue for ≥28 days prior to and after surgery |
| Ramucirumab | mAb VEGFR2 antagonist | 13.4 days | Discontinue for ≥4 weeks prior to surgery and after surgery if there are wound healing complications |
| Aflibercept | Protein decoy for VEGF A-D and PIGF | 11 days | Withhold within the previous or next 28 days in the event of a performed or planned intraocular surgery |
| Axitinib | TKI of VEGFR-1-3 | 2.5–6.1 h | Discontinue ≥ 24 h prior to scheduled surgery |
| Sorafenib | TKI of VEGFR, PDGFR, c-Kit and RET | 25–48 h | No specific interval recommendation |
| Sunitinib | Multi-targeted TKI including PDGFRα, PDGFRβ, VEGFR1, VEGFR2, VEGFR3 | 40–60 h | Discontinue for ≥3 weeks prior to surgery and for ≥2 weeks after major surgery |
| Imatinib | Multi-targeted TKI including BCR-ABL, c-KIT, and PDGFRA | 20 h | No specific interval recommendation |
| Lenvatinib | Multi-targeted TKI including VEGFR-1-3 and FGFR-1-4 | 28 h | No specific interval recommendation |
| Cabozantinib | Multi-targeted TKI including VEGFR-1-3 | 99 h | Discontinue for ≥28 days prior to scheduled surgery |
| Pazopanib | Multi-targeted TKI including VEGFR1-3, PDGFRβ and FGFR1 | 21–51 h | Discontinue for ≥7 days prior to scheduled surgery |
| Regorafenib | Multi-targeted TKI including VEGFR1-3, PDGFR and FGFR1-2 | 20–30 h | No specific interval recommendation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robinson, M.D.; McNamara, M.G.; Clouston, H.W.; Sutton, P.A.; Hubner, R.A.; Valle, J.W. Patients Undergoing Systemic Anti-Cancer Therapy Who Require Surgical Intervention: What Surgeons Need to Know. Cancers 2023, 15, 3781. https://doi.org/10.3390/cancers15153781
Robinson MD, McNamara MG, Clouston HW, Sutton PA, Hubner RA, Valle JW. Patients Undergoing Systemic Anti-Cancer Therapy Who Require Surgical Intervention: What Surgeons Need to Know. Cancers. 2023; 15(15):3781. https://doi.org/10.3390/cancers15153781
Chicago/Turabian StyleRobinson, Matthew D., Mairéad G. McNamara, Hamish W. Clouston, Paul A. Sutton, Richard A. Hubner, and Juan W. Valle. 2023. "Patients Undergoing Systemic Anti-Cancer Therapy Who Require Surgical Intervention: What Surgeons Need to Know" Cancers 15, no. 15: 3781. https://doi.org/10.3390/cancers15153781
APA StyleRobinson, M. D., McNamara, M. G., Clouston, H. W., Sutton, P. A., Hubner, R. A., & Valle, J. W. (2023). Patients Undergoing Systemic Anti-Cancer Therapy Who Require Surgical Intervention: What Surgeons Need to Know. Cancers, 15(15), 3781. https://doi.org/10.3390/cancers15153781






