Maintaining Engagement in Adults with Neurofibromatosis Type 1 to Use the iCanCope Mobile Application (iCanCope-NF)
Abstract
Simple Summary
Abstract
1. Introduction
2. Methodology
2.1. Participants
2.2. Procedure
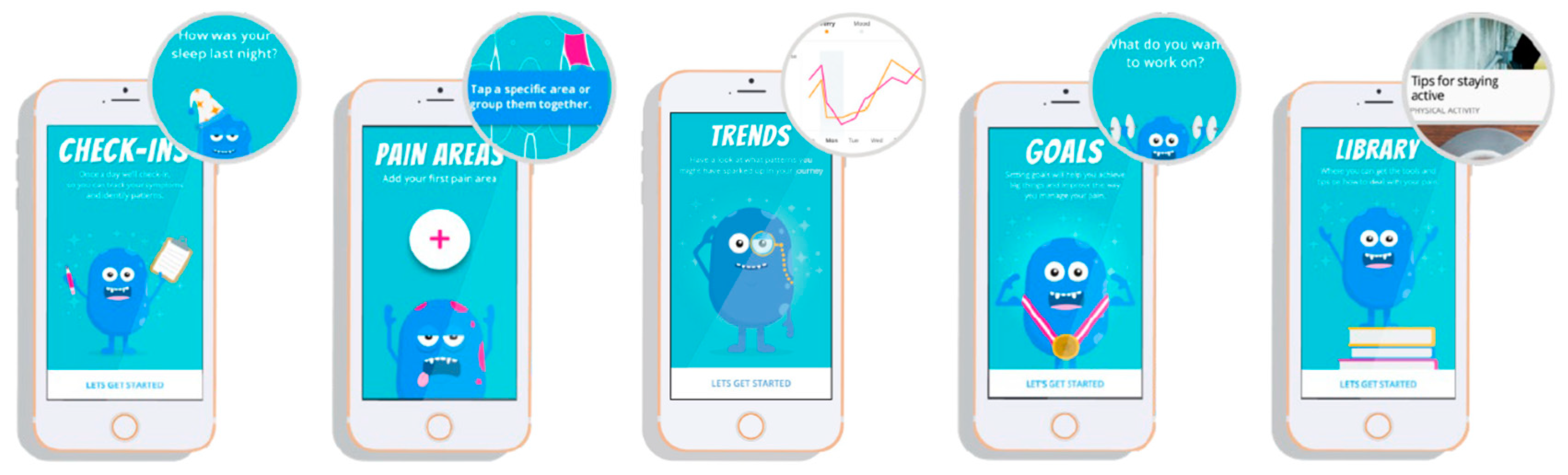
2.3. iCanCope Mobile Application
2.3.1. iCanCope Orientation
2.3.2. iCC Group
2.3.3. iCC + CM Group
2.4. Data Analysis
3. Results
3.1. Demographics
3.2. Quantitative
3.3. Qualitative
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, J.L.; Gutmann, D.H. Neurofibromatosis type 1. Handb. Clin. Neurol. 2015, 132, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Legius, E.; Messiaen, L.; Wolkenstein, P.; Pancza, P.; Avery, R.A.; Berman, Y.; Blakeley, J.; Babovic-Vuksanovic, D.; Cunha, K.S.; Ferner, R.; et al. Revised diagnostic criteria for neurofibromatosis type 1 and Legius syndrome: An international consensus recommendation. Genet. Med. 2021, 23, 1506–1513. [Google Scholar] [CrossRef]
- Gutmann, D.H.; Aylsworth, A.; Carey, J.C.; Korf, B.; Marks, J.; Pyeritz, R.E.; Rubenstein, A.; Viskochil, D. The Diagnostic Evaluation and Multidisciplinary Management of Neurofibromatosis 1 and Neurofibromatosis 2. JAMA 1997, 278, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Gutmann, D.H.; Ferner, R.E.; Listernick, R.H.; Korf, B.R.; Wolters, P.L.; Johnson, K.J. Neurofibromatosis type 1. Nat. Rev. Dis. Prim. 2017, 3, 17004. [Google Scholar] [CrossRef]
- Ly, K.I.; Blakeley, J.O. The Diagnosis and Management of Neurofibromatosis Type 1. Med. Clin. N. Am. 2019, 103, 1035–1054. [Google Scholar] [CrossRef]
- Afridi, S.K.; Leschziner, G.D.; Ferner, R.E. Prevalence and clinical presentation of headache in a National Neurofibromatosis 1 Service and impact on quality of life. Am. J. Med. Genet. A 2015, 167, 2282–2285. [Google Scholar] [CrossRef]
- Pinho, R.S.; Fusão, E.F.; Paschoal, J.; Caran, E.M.M.; Minett, T.S.C.; Vilanova, L.C.P.; Masruha, M.R. Migraine is frequent in children and adolescents with neurofibromatosis type 1. Pediatr. Int. 2014, 56, 865–867. [Google Scholar] [CrossRef] [PubMed]
- Kongkriangkai, A.M.; King, C.; Martin, L.J.; Wakefield, E.; Prada, C.E.; Kelly-Mancuso, G.; Schorry, E.K. Substantial pain burden in frequency, intensity, interference and chronicity among children and adults with neurofibromatosis Type 1. Am. J. Med. Genet. A 2019, 179, 602–607. [Google Scholar] [CrossRef]
- Iheanacho, I.; Yoo, H.K.; Yang, X.; Dodman, S.; Hughes, R.; Amin, S. Epidemiological and clinical burden associated with plexiform neurofibromas in pediatric neurofibromatosis type-1 (NF-1): A systematic literature review. Neurol. Sci. 2022, 43, 1281–1293. [Google Scholar] [CrossRef]
- Fisher, M.J.; Shih, C.S.; Rhodes, S.D.; Armstrong, A.E.; Wolters, P.L.; Dombi, E.; Zhang, C.; Angus, S.P.; Johnson, G.L.; Packer, R.J.; et al. Cabozantinib for neurofibromatosis type 1-related plexiform neurofibromas: A phase 2 trial. Nat. Med. 2021, 27, 165–173. [Google Scholar] [CrossRef]
- Foiadelli, T.; Naso, M.; Licari, A.; Orsini, A.; Magistrali, M.; Trabatti, C.; Luzzi, S.; Mosconi, M.; Savasta, S.; Marseglia, G.L. Advanced pharmacological therapies for neurofibromatosis type 1-related tumors. Acta Biomed. 2020, 91, 101–114. [Google Scholar] [CrossRef]
- Friedrich, R.E.; Tuzcu, C.T. Surgery for Peripheral Nerve Sheath Tumours of the Buttocks, Legs and Feet in 90 Patients With Neurofibromatosis Type 1. In Vivo 2021, 35, 889–905. [Google Scholar] [CrossRef]
- Gottfried, O.N.; Viskochil, D.H.; Couldwell, W.T. Neurofibromatosis Type 1 and tumorigenesis: Molecular mechanisms and therapeutic implications. Neurosurg. Focus 2010, 28, E8. [Google Scholar] [CrossRef] [PubMed]
- Gross, A.M.; Wolters, P.L.; Dombi, E.; Baldwin, A.; Whitcomb, P.; Fisher, M.J.; Weiss, B.; Kim, A.; Bornhorst, M.; Shah, A.C.; et al. Selumetinib in Children with Inoperable Plexiform Neurofibromas. N. Engl. J. Med. 2020, 382, 1430–1442. [Google Scholar] [CrossRef] [PubMed]
- Klesse, L.J.; Jordan, J.T.; Radtke, H.B.; Rosser, T.; Schorry, E.; Ullrich, N.; Viskochil, D.; Knight, P.; Plotkin, S.R.; Yohay, K. The Use of MEK Inhibitors in Neurofibromatosis Type 1-Associated Tumors and Management of Toxicities. Oncologist 2020, 25, e1109–e1116. [Google Scholar] [CrossRef]
- Korf, B.R. Diagnosis and management of neurofibromatosis type 1. Curr. Neurol. Neurosci. Rep. 2001, 1, 162–167. [Google Scholar] [CrossRef]
- Valeyrie-Allanore, L.; Ismaili, N.; Bastuji-Garin, S.; Zeller, J.; Wechsler, J.; Revuz, J.; Wolkenstein, P. Symptoms associated with malignancy of peripheral nerve sheath tumours: A retrospective study of 69 patients with neurofibromatosis 1. Br. J. Dermatol. 2005, 153, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Buono, F.D.; Grau, L.E.; Sprong, M.E.; Morford, K.L.; Johnson, K.J.; Gutmann, D.H. Pain symptomology, functional impact, and treatment of people with Neurofibromatosis type 1. J. Pain Res. 2019, 12, 2555–2561. [Google Scholar] [CrossRef]
- Gatchel, R.J.; McGeary, D.D.; McGeary, C.A.; Lippe, B. Interdisciplinary chronic pain management: Past, present, and future. Am. Psychol. 2014, 69, 119–130. [Google Scholar] [CrossRef]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef]
- Hylands-White, N.; Duarte, R.V.; Raphael, J.H. An overview of treatment approaches for chronic pain management. Rheumatol. Int. 2017, 37, 29–42. [Google Scholar] [CrossRef]
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097. [Google Scholar] [CrossRef]
- Nicholas, M.; Vlaeyen, J.W.S.; Rief, W.; Barke, A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.A.; Goebel, A.; et al. The IASP classification of chronic pain for ICD-11: Chronic primary pain. Pain 2019, 160, 28–37. [Google Scholar] [CrossRef]
- Morley, S. Efficacy and effectiveness of cognitive behaviour therapy for chronic pain: Progress and some challenges. Pain 2011, 152, S99–S106. [Google Scholar] [CrossRef]
- Fenn, K.; Byrne, M. The key principles of cognitive behavioural therapy. InnovAiT 2013, 6, 579–585. [Google Scholar] [CrossRef]
- Holmes, J. All you need is cognitive behaviour therapy? BMJ 2002, 324, 288–290, discussion 290–284. [Google Scholar] [CrossRef] [PubMed]
- Thoma, N.; Pilecki, B.; McKay, D. Contemporary Cognitive Behavior Therapy: A Review of Theory, History, and Evidence. Psychodyn. Psychiatry 2015, 43, 423–461. [Google Scholar] [CrossRef]
- Carnes, D.; Homer, K.E.; Miles, C.L.; Pincus, T.; Underwood, M.; Rahman, A.; Taylor, S.J. Effective delivery styles and content for self-management interventions for chronic musculoskeletal pain: A systematic literature review. Clin. J. Pain 2012, 28, 344–354. [Google Scholar] [CrossRef] [PubMed]
- Lalloo, C.; Jibb, L.A.; Rivera, J.; Agarwal, A.; Stinson, J.N. “There’s a Pain App for That”: Review of Patient-targeted Smartphone Applications for Pain Management. Clin. J. Pain 2015, 31, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Lee, H.; Kim, Y.; Kim, J.; Cho, M.; Jang, J.; Jang, H. Mobile App-Based Health Promotion Programs: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2018, 15, 2838. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, M.; Bakker, A.M.; Anderson, K.; Holtzman, S. Do pain management apps use evidence-based psychological components? A systematic review of app content and quality. Can. J. Pain 2022, 6, 33–44. [Google Scholar] [CrossRef]
- Sylvia, L.G.; Lunn, M.R.; Obedin-Maliver, J.; McBurney, R.N.; Nowell, W.B.; Nosheny, R.L.; Mularski, R.A.; Long, M.D.; Merkel, P.A.; Pletcher, M.J.; et al. Web-Based Mindfulness-Based Interventions for Well-being: Randomized Comparative Effectiveness Trial. J. Med. Internet Res. 2022, 24, e35620. [Google Scholar] [CrossRef]
- McKay, F.H.; Cheng, C.; Wright, A.; Shill, J.; Stephens, H.; Uccellini, M. Evaluating mobile phone applications for health behaviour change: A systematic review. J. Telemed. Telecare 2018, 24, 22–30. [Google Scholar] [CrossRef]
- Sama, P.R.; Eapen, Z.J.; Weinfurt, K.P.; Shah, B.R.; Schulman, K.A. An evaluation of mobile health application tools. JMIR Mhealth Uhealth 2014, 2, e19. [Google Scholar] [CrossRef] [PubMed]
- Devan, H.; Godfrey, H.K.; Perry, M.A.; Hempel, D.; Saipe, B.; Hale, L.; Grainger, R. Current practices of health care providers in recommending online resources for chronic pain self-management. J. Pain Res. 2019, 12, 2457–2472. [Google Scholar] [CrossRef] [PubMed]
- Larson, R.S. A Path to Better-Quality mHealth Apps. JMIR Mhealth Uhealth 2018, 6, e10414. [Google Scholar] [CrossRef]
- Higgins, S.T.; Silverman, K. Motivating Behavior Change among Illicit-Drug Abusers: Research on Contingency Management Interventions; American Psychological Association: Washington, DC, USA, 1999. [Google Scholar]
- Geraghty, A.W.A.; Maund, E.; Newell, D.; Santer, M.; Everitt, H.; Price, C.; Pincus, T.; Moore, M.; Little, P.; West, R.; et al. Self-management for chronic widespread pain including fibromyalgia: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0254642. [Google Scholar] [CrossRef]
- Loughney, L.; Cahill, R.; O’Malley, K.; McCaffrey, N.; Furlong, B. Compliance, adherence and effectiveness of a community-based pre-operative exercise programme: A pilot study. Perioper. Med. 2019, 8, 17. [Google Scholar] [CrossRef]
- Simon-Tuval, T.; Neumann, P.J.; Greenberg, D. Cost-effectiveness of adherence-enhancing interventions: A systematic review. Expert Rev. Pharm. Outcomes Res. 2016, 16, 67–84. [Google Scholar] [CrossRef]
- Yang, J.; Weng, L.; Chen, Z.; Cai, H.; Lin, X.; Hu, Z.; Li, N.; Lin, B.; Zheng, B.; Zhuang, Q.; et al. Development and Testing of a Mobile App for Pain Management Among Cancer Patients Discharged From Hospital Treatment: Randomized Controlled Trial. JMIR Mhealth Uhealth 2019, 7, e12542. [Google Scholar] [CrossRef] [PubMed]
- Bolívar, H.A.; Klemperer, E.M.; Coleman, S.R.M.; DeSarno, M.; Skelly, J.M.; Higgins, S.T. Contingency Management for Patients Receiving Medication for Opioid Use Disorder: A Systematic Review and Meta-analysis. JAMA Psychiatry 2021, 78, 1092–1102. [Google Scholar] [CrossRef] [PubMed]
- Ellis, J.D.; Struble, C.A.; Fodor, M.C.; Cairncross, M.; Lundahl, L.H.; Ledgerwood, D.M. Contingency management for individuals with chronic health conditions: A systematic review and meta-analysis of randomized controlled trials. Behav. Res. Ther. 2021, 136, 103781. [Google Scholar] [CrossRef] [PubMed]
- González-Roz, A.; Secades-Villa, R.; García-Fernández, G.; Martínez-Loredo, V.; Alonso-Pérez, F. Depression symptom profiles and long-term response to cognitive behavioral therapy plus contingency management for smoking cessation. Drug Alcohol. Depend. 2021, 225, 108808. [Google Scholar] [CrossRef] [PubMed]
- Secades-Villa, R.; González-Roz, A.; Vallejo-Seco, G.; Weidberg, S.; García-Pérez, Á.; Alonso-Pérez, F. Additive effectiveness of contingency management on cognitive behavioural treatment for smokers with depression: Six-month abstinence and depression outcomes. Drug Alcohol. Depend. 2019, 204, 107495. [Google Scholar] [CrossRef] [PubMed]
- Latimer, P.R. External contingency management for chronic pain: Critical review of the evidence. Am. J. Psychiatry 1982, 139, 1308–1312. [Google Scholar] [CrossRef]
- Stinson, J.N.; Lalloo, C.; Harris, L.; Isaac, L.; Campbell, F.; Brown, S.; Ruskin, D.; Gordon, A.; Galonski, M.; Pink, L.R.; et al. iCanCope with Pain™: User-centred design of a web- and mobile-based self-management program for youth with chronic pain based on identified health care needs. Pain Res. Manag. 2014, 19, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Birnie, K.A.; Campbell, F.; Nguyen, C.; Lalloo, C.; Tsimicalis, A.; Matava, C.; Cafazzo, J.; Stinson, J. iCanCope PostOp: User-Centered Design of a Smartphone-Based App for Self-Management of Postoperative Pain in Children and Adolescents. JMIR Form. Res. 2019, 3, e12028. [Google Scholar] [CrossRef]
- Kulandaivelu, Y.; Lalloo, C.; Ward, R.; Zempsky, W.T.; Kirby-Allen, M.; Breakey, V.R.; Odame, I.; Campbell, F.; Amaria, K.; Simpson, E.A.; et al. Exploring the Needs of Adolescents With Sickle Cell Disease to Inform a Digital Self-Management and Transitional Care Program: Qualitative Study. JMIR Pediatr. Parent. 2018, 1, e11058. [Google Scholar] [CrossRef]
- Lalloo, C.; Harris, L.R.; Hundert, A.S.; Berard, R.; Cafazzo, J.; Connelly, M.; Feldman, B.M.; Houghton, K.; Huber, A.; Laxer, R.M.; et al. The iCanCope pain self-management application for adolescents with juvenile idiopathic arthritis: A pilot randomized controlled trial. Rheumatology 2021, 60, 196–206. [Google Scholar] [CrossRef]
- Lalloo, C.; Nishat, F.; Zempsky, W.; Bakshi, N.; Badawy, S.; Ko, Y.J.; Dampier, C.; Stinson, J.; Palermo, T.M. Characterizing user engagement with a digital intervention for pain self-management among youth with sickle cell disease and caregivers: Sub-analysis of a randomized controlled trial (Preprint). J. Med. Internet Res. 2022, 24, e40096. [Google Scholar] [CrossRef]
- Buono, F.D.; Lalloo, C.; Larkin, K.; Zempsky, W.T.; Ball, S.; Grau, L.E.; Pham, Q.; Stinson, J. Innovation in the treatment of persistent pain in adults with Neurofibromatosis Type 1 (NF1): Implementation of the iCanCope mobile application. Contemp. Clin. Trials Commun. 2022, 25, 100883. [Google Scholar] [CrossRef] [PubMed]
- Pham, Q.; Graham, G.; Lalloo, C.; Morita, P.P.; Seto, E.; Stinson, J.N.; Cafazzo, J.A. An Analytics Platform to Evaluate Effective Engagement With Pediatric Mobile Health Apps: Design, Development, and Formative Evaluation. JMIR Mhealth Uhealth 2018, 6, e11447. [Google Scholar] [CrossRef] [PubMed]
- Strauss, A.; Corbin, J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 2nd ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Lalloo, C.; Hundert, A.; Harris, L.; Pham, Q.; Campbell, F.; Chorney, J.; Dick, B.; Simmonds, M.; Cafazzo, J.; Stinson, J. Capturing Daily Disease Experiences of Adolescents With Chronic Pain: mHealth-Mediated Symptom Tracking. JMIR Mhealth Uhealth 2019, 7, e11838. [Google Scholar] [CrossRef] [PubMed]
- Rodas, J.D.; Sorkhou, M.; George, T.P. Contingency Management for Treatment of Cannabis Use Disorder in Co-Occurring Mental Health Disorders: A Systematic Review. Brain Sci. 2022, 13, 36. [Google Scholar] [CrossRef]
- Stanger, C.; Budney, A.J. Contingency Management: Using Incentives to Improve Outcomes for Adolescent Substance Use Disorders. Pediatr. Clin. N. Am. 2019, 66, 1183–1192. [Google Scholar] [CrossRef]
- Lobato, L.; Bethony, J.M.; Pereira, F.B.; Grahek, S.L.; Diemert, D.; Gazzinelli, M.F. Impact of gender on the decision to participate in a clinical trial: A cross-sectional study. BMC Public Health 2014, 14, 1156. [Google Scholar] [CrossRef]
- Samulowitz, A.; Gremyr, I.; Eriksson, E.; Hensing, G. “Brave Men” and “Emotional Women”: A Theory-Guided Literature Review on Gender Bias in Health Care and Gendered Norms towards Patients with Chronic Pain. Pain Res. Manag. 2018, 2018, 6358624. [Google Scholar] [CrossRef]
| ICC (N = 38) | ICC + CM (N = 38) | p-Value | |
|---|---|---|---|
| Age, mean (SD) | 41.9 (12.9) | 40.5 (13.6) | 0.663 |
| Race (n; %) | 0.558 | ||
| White | 33 (78%) | 28 (74%) | |
| Black | 2 (5%) | 4 (11%) | |
| Asian | 1 (3%) | 2 (5%) | |
| Hispanic | 2 (5%) | 2 (5%) | |
| Gender (n; %) | 0.443 | ||
| Male | 11 (30%) | 12 (29%) | |
| Female | 26 (67%) | 24 (71%) | |
| Transgender | 0 | 0 | |
| Other | 1 (3%) | 0 | |
| Highest Education (n; %) | 0.577 | ||
| Advanced Degree (e.g., Masters, PhD, MD) | 4 (10%) | 4 (10%) | |
| Bachelor’s Degree | 13 (31%) | 10 (26%) | |
| Associate degree | 8 (19%) | 9 (23%) | |
| Some of College | 7 (17%) | 6 (15%) | |
| Technical School | 2 (5%) | 1 (3%) | |
| High School | 7 (17%) | 10 (26%) | |
| Age at diagnosis in years, mean (SD) | 11.7 (13.1) | 10.4 (11.9) | 0.664 |
| Number of NF1 surgeries, mean (SD) | 2.84 (1.5) | 2.8 (1.4) | 0.85 |
| Parental History of NF1 (n; %) | 0.408 | ||
| yes | 13 (34%) | 10 (26%) | |
| maybe | 6 (16%) | 4 (11%) | |
| no | 19 (50%) | 22 (58%) |
| ICC Engagement Category | Grouping | Total Count Across All Users | Mean per User | SD | p-Value |
|---|---|---|---|---|---|
| Goals Achieved | iCC | 121 | 3.2 | 9.5 | 0.017 |
| app recommended | 1 | <0.001 | |||
| user-generated | 120 | 3.2 | 9.5 | ||
| iCC + CM | 1020 | 29.1 | 63.9 | ||
| app recommended | 183 | 1.6 | 2.1 | <0.001 | |
| user-generated | 854 | 14.5 | 13.3 | ||
| Goals Created | iCC | 110 | 2.9 | 6.4 | 0.008 |
| app recommended | 10 | 1.91 | 0.3 | 0.032 | |
| user-generated | 99 | 1.82 | 0.3 | ||
| iCC + CM | 415 | 11.8 | 18.7 | ||
| app recommended | 77 | 1.1 | 0.2 | <0.001 | |
| user-generated | 361 | 6.3 | 0.9 | ||
| Articles Read | iCC | 957 | 25.86 | 45.283 | 0.002 |
| iCC + CM | 2805 | 80.1 | 88.2 | ||
| Check-ins | iCC | 1996 | 53.9 | 27.1 | 0.378 |
| iCC + CM | 2407 | 68.7 | 97.8 |
| Most Preferred Articles | Total Count of Views | Least Preferred Articles | Total Count of Views |
|---|---|---|---|
| Treatments for NF1 Pain | 250 | Setting goals related to physical activity | 6 |
| What is fatigue and how can I cope with it? | 191 | Talking to your healthcare team | 6 |
| Reclined Twist (Yoga Pose) | 174 | Pacing yourself | 6 |
| Balancing School, Work and Leisure Activities | 140 | Maintaining a relationship with a boyfriend or girlfriend | 6 |
| Can heat or cold help my pain | 136 | Developing and sticking to your healthcare plan | 6 |
| Common Causes of Pain in NF1 | 129 | 3-sentence health summary | 6 |
| Relaxation and Chronic Pain | 120 | Dealing with setbacks | 4 |
| Rest Time | 111 | Tips for staying connected to family and friends | 4 |
| Progressive Muscle Relaxation with Tension | 103 | How to help friends understand chronic pain | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buono, F.D.; Larkin, K.; Pham, Q.; De Sousa, D.; Zempsky, W.T.; Lalloo, C.; Stinson, J.N. Maintaining Engagement in Adults with Neurofibromatosis Type 1 to Use the iCanCope Mobile Application (iCanCope-NF). Cancers 2023, 15, 3213. https://doi.org/10.3390/cancers15123213
Buono FD, Larkin K, Pham Q, De Sousa D, Zempsky WT, Lalloo C, Stinson JN. Maintaining Engagement in Adults with Neurofibromatosis Type 1 to Use the iCanCope Mobile Application (iCanCope-NF). Cancers. 2023; 15(12):3213. https://doi.org/10.3390/cancers15123213
Chicago/Turabian StyleBuono, Frank D., Kaitlyn Larkin, Quynh Pham, Diane De Sousa, William T. Zempsky, Chitra Lalloo, and Jennifer N. Stinson. 2023. "Maintaining Engagement in Adults with Neurofibromatosis Type 1 to Use the iCanCope Mobile Application (iCanCope-NF)" Cancers 15, no. 12: 3213. https://doi.org/10.3390/cancers15123213
APA StyleBuono, F. D., Larkin, K., Pham, Q., De Sousa, D., Zempsky, W. T., Lalloo, C., & Stinson, J. N. (2023). Maintaining Engagement in Adults with Neurofibromatosis Type 1 to Use the iCanCope Mobile Application (iCanCope-NF). Cancers, 15(12), 3213. https://doi.org/10.3390/cancers15123213






