Model for End-Stage Liver Disease Correlates with Disease Relapse and Death of Patients with Merkel Cell Carcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Clinical Characteristics and Laboratory Values
3.2. Clinical Outcome of Patients and Comorbidities
3.3. Univariable and Multivariable Statistics for MCC Outcome Measures
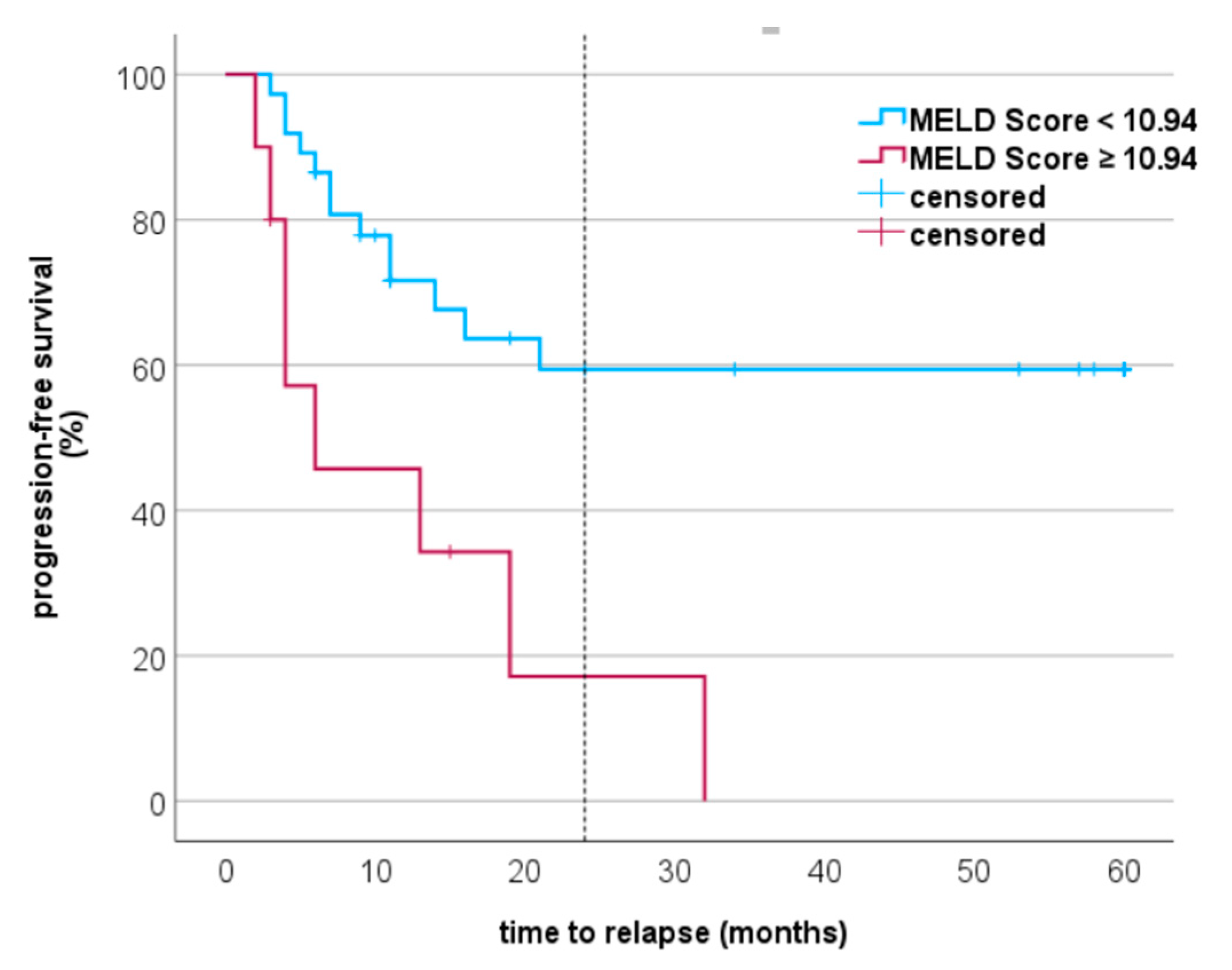
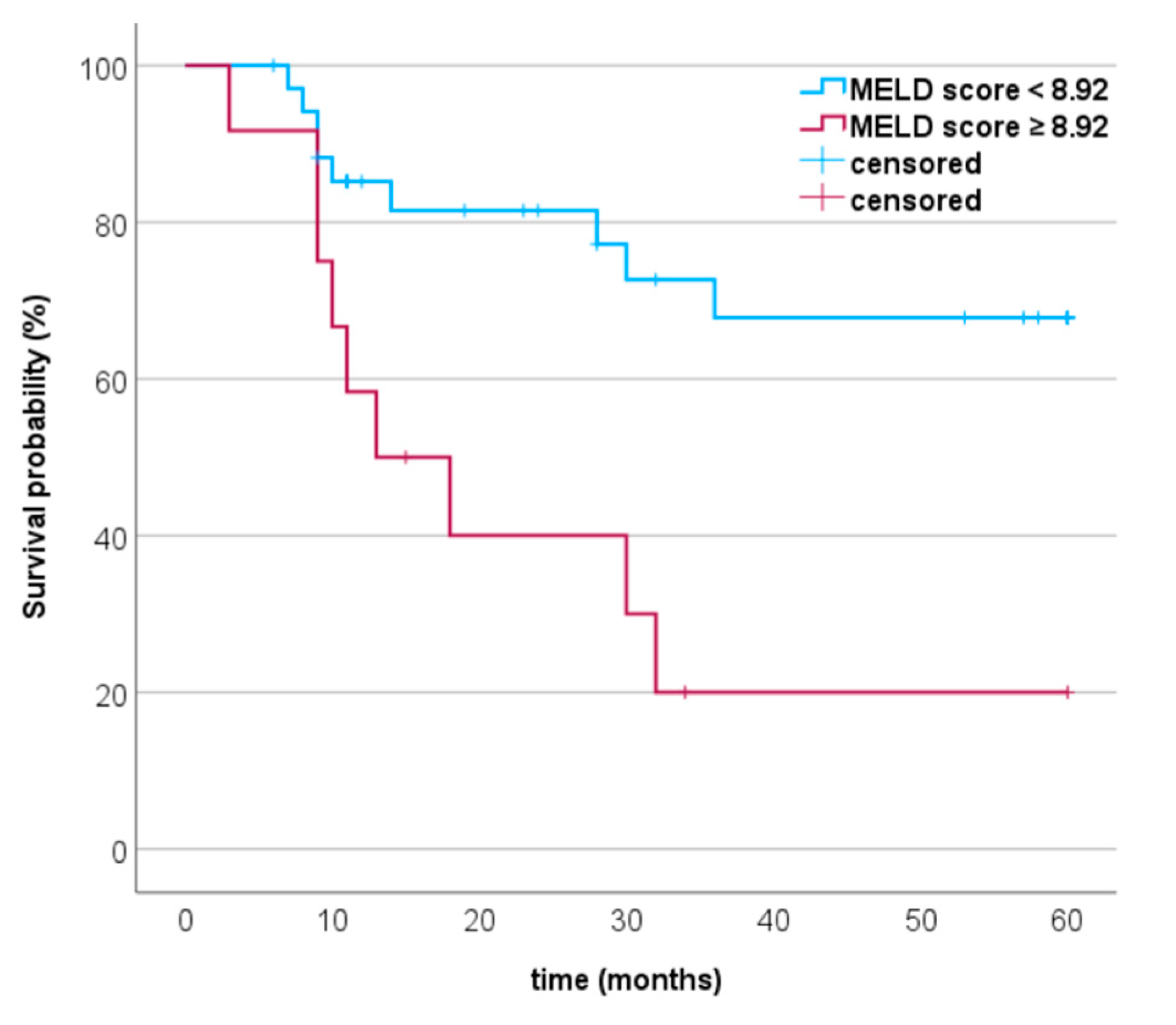
3.4. Progression-Free Survival and MCC-Specific Death in Relation to MELD Score
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Becker, J.C.; Stang, A.; DeCaprio, J.A.; Cerroni, L.; Lebbé, C.; Veness, M.; Nghiem, P. Merkel cell carcinoma. Nat. Rev. Dis. Prim. 2017, 3, 17077. [Google Scholar] [CrossRef] [PubMed]
- Su, L.D.; Lowe, L.; Bradford, C.R.; Yahanda, A.I.; Johnson, T.M.; Sondak, V.K. Immunostaining for cytokeratin 20 improves detection of micrometastatic Merkel cell carcinoma in sentinel lymph nodes. J. Am. Acad. Dermatol. 2002, 46, 661–666. [Google Scholar] [CrossRef]
- Chteinberg, E.; Sauer, C.M.; Rennspiess, D.; Beumers, L.; Schiffelers, L.; Eben, J.; Haugg, A.; Winnepenninckx, V.; Kurz, A.K.; Speel, E.-J.; et al. Neuroendocrine Key Regulator Gene Expression in Merkel Cell Carcinoma. Neoplasia 2018, 20, 1227–1235. [Google Scholar] [CrossRef]
- Fields, R.C.; Busam, K.J.; Chou, J.F.; Panageas, K.S.; Pulitzer, M.P.; Kraus, D.H.; Brady, M.S.; Coit, D.G. Recurrence and survival in patients undergoing sentinel lymph node biopsy for merkel cell carcinoma: Analysis of 153 patients from a single institution. Ann. Surg. Oncol. 2011, 18, 2529–2537. [Google Scholar] [CrossRef]
- Gambichler, T.; Said, S.; Abu Rached, N.; Scheel, C.H.; Susok, L.; Stranzenbach, R.; Becker, J.C. Pan-immune-inflammation value independently predicts disease recurrence in patients with Merkel cell carcinoma. J. Cancer Res. Clin. Oncol. 2022, 148, 3183–3189. [Google Scholar] [CrossRef] [PubMed]
- Gambichler, T.; Abu Rached, N.; Susok, L.; Becker, J.C. Serum neuron-specific enolase independently predicts outcomes of patients with Merkel cell carcinoma. Br. J. Dermatol. 2022, 187, 806–808. [Google Scholar] [CrossRef]
- DeBerardinis, R.J.; Chandel, N.S. Fundamentals of cancer metabolism. Sci. Adv. 2016, 2, e1600200. [Google Scholar] [CrossRef] [PubMed]
- Harms, P.W.; Harms, K.L.; Moore, P.S.; DeCaprio, J.A.; Nghiem, P.; Wong, M.K.K.; Brownell, I. The biology and treatment of Merkel cell carcinoma: Current understanding and research priorities. Nat. Rev. Clin. Oncol. 2018, 15, 763–776. [Google Scholar] [CrossRef]
- Rui, L. Energy metabolism in the liver. Compr. Physiol. 2014, 4, 177–197. [Google Scholar] [CrossRef]
- Ruhwedel, T.; Rogasch, J.M.M.; Huang, K.; Jann, H.; Schatka, I.; Furth, C.; Amthauer, H.; Wetz, C. The Prognostic Value of the De Ritis Ratio for Progression-Free Survival in Patients with NET Undergoing 177LuLu-DOTATOC-PRRT: A Retrospective Analysis. Cancers 2021, 13, 635. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.C.; Beer, A.J.; DeTemple, V.K.; Eigentler, T.; Flaig, M.; Gambichler, T.; Grabbe, S.; Höller, U.; Klumpp, B.; Lang, S.; et al. S2k Guideline-Merkel cell carcinoma (MCC, neuroendocrine carcinoma of the skin)-Update 2022. J. Dtsch. Dermatol. Ges. 2023, 21, 305–320. [Google Scholar] [CrossRef] [PubMed]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Benjamini, Y.; Drai, D.; Elmer, G.; Kafkafi, N.; Golani, I. Controlling the false discovery rate in behavior genetics research. Behav. Brain Res. 2001, 125, 279–284. [Google Scholar] [CrossRef]
- Knittelfelder, O.; Delago, D.; Jakse, G.; Reinisch, S.; Partl, R.; Stranzl-Lawatsch, H.; Renner, W.; Langsenlehner, T. The AST/ALT (De Ritis) Ratio Predicts Survival in Patients with Oral and Oropharyngeal Cancer. Diagnostics 2020, 10, 973. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, M.; Aghalarov, S.; Atci, M.M.; Selvi, O.; Canat, H.L. Ein neuer Biomarker für Lungenmetastasen bei nicht seminomatösem Hodenkrebs: De Ritis Ratio. Aktuelle Urol. 2022, 53, 540–544. [Google Scholar] [CrossRef]
- Yilmaz, M.; Sahin, Y.; Ates, H.A.; Hacibey, I.; Cil, G. De Ritis ratio: How effectively can we use in bladder cancer management? Biomark. Med. 2020, 14, 1453–1460. [Google Scholar] [CrossRef] [PubMed]
- Laukhtina, E.; Mostafaei, H.; D'Andrea, D.; Pradere, B.; Quhal, F.; Mori, K.; Miura, N.; Schuettfort, V.M.; Sari Motlagh, R.; Aydh, A.; et al. Association of De Ritis ratio with oncological outcomes in patients with non-muscle invasive bladder cancer (NMIBC). World J. Urol. 2021, 39, 1961–1968. [Google Scholar] [CrossRef]
- Batur, A.F.; Aydogan, M.F.; Kilic, O.; Korez, M.K.; Gul, M.; Kaynar, M.; Goktas, S.; Akand, M. Comparison of De Ritis Ratio and other systemic inflammatory parameters for the prediction of prognosis of patients with transitional cell bladder cancer. Int. J. Clin. Pract. 2021, 75, e13743. [Google Scholar] [CrossRef]
- Wang, H.; Fang, K.; Zhang, J.; Jiang, Y.; Wang, G.; Zhang, H.; Chen, T.; Shi, X.; Li, Y.; Duan, F.; et al. The significance of De Ritis (aspartate transaminase/alanine transaminase) ratio in predicting pathological outcomes and prognosis in localized prostate cancer patients. Int. Urol. Nephrol. 2017, 49, 1391–1398. [Google Scholar] [CrossRef]
- Drácz, B.; Czompa, D.; Müllner, K.; Hagymási, K.; Miheller, P.; Székely, H.; Papp, V.; Horváth, M.; Hritz, I.; Szijártó, A.; et al. The Elevated De Ritis Ratio on Admission Is Independently Associated with Mortality in COVID-19 Patients. Viruses 2022, 14, 2360. [Google Scholar] [CrossRef]
- Wu, J.; Chen, L.; Wang, Y.; Tan, W.; Huang, Z. Prognostic value of aspartate transaminase to alanine transaminase (De Ritis) ratio in solid tumors: A pooled analysis of 9400 patients. Onco. Targets. Ther. 2019, 12, 5201–5213. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, D.; Yamamoto, K.; Kimura, T.; Shimbo, T. Aspartate aminotransferase/alanine aminotransferase ratio and subsequent cancer development. Cancer Med. 2022, 11, 798–814. [Google Scholar] [CrossRef] [PubMed]
- Loaeza-del-Castillo, A.; Paz-Pineda, F.; Oviedo-Cárdenas, E.; Sánchez-Avila, F.; Vargas-Vorácková, F. AST to platelet ratio index (APRI) for the noninvasive evaluation of liver fibrosis. Ann. Hepatol. 2008, 7, 350–357. [Google Scholar] [CrossRef]
- Kruger, F.C.; Daniels, C.R.; Kidd, M.; Swart, G.; Brundyn, K.; van Rensburg, C.; Kotze, M. APRI: A simple bedside marker for advanced fibrosis that can avoid liver biopsy in patients with NAFLD/NASH. S. Afr. Med. J. 2011, 101, 477–480. [Google Scholar]
- Mai, R.-Y.; Ye, J.-Z.; Long, Z.-R.; Shi, X.-M.; Bai, T.; Chen, J.; Li, L.-Q.; Wu, G.-B.; Wu, F.-X. Preoperative aspartate aminotransferase-to-platelet-ratio index as a predictor of posthepatectomy liver failure for resectable hepatocellular carcinoma. Cancer Manag. Res. 2019, 11, 1401–1414. [Google Scholar] [CrossRef] [PubMed]
- Sacleux, S.-C.; Samuel, D. A Critical Review of MELD as a Reliable Tool for Transplant Prioritization. Semin. Liver Dis. 2019, 39, 403–413. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, H.; Jiang, X.; Qian, C.; Liu, Z.; Luo, D. Factors involved in cancer metastasis: A better understanding to “seed and soil” hypothesis. Mol. Cancer 2017, 16, 176. [Google Scholar] [CrossRef]
- Kaae, J.; Hansen, A.V.; Biggar, R.J.; Boyd, H.A.; Moore, P.S.; Wohlfahrt, J.; Melbye, M. Merkel cell carcinoma: Incidence, mortality, and risk of other cancers. J. Natl. Cancer Inst. 2010, 102, 793–801. [Google Scholar] [CrossRef]
| Parameters | Data | |
|---|---|---|
| Age at diagnosis, median (range), years | 78 (51–95) | |
| Sex Male vs. female, n (%) | 23 (49) vs. 24 (51) | |
| Primary MCC Head/neck (no/yes), n (%) MCPyV (negative/positive), n (%) Lactate dehydrogenase (U/L), median (range) C-reactive protein Normal/elevated, n (%) | 27/20 (57.4/42.6) 10 (21.3)/37 (78.7) 200 (109–699) 33 (70.2)/14 (29.8) | |
| Tumor stage at diagnosis (according AJCC 2018), n (%) | Early stages Advanced stages | I 18 (38.3) II 14 (29.8) III 10 (21.3) IV 5 (10.6) |
| Parameters of liver metabolism, median (range) | APRI score De Ritis score MELD score | 0.3 (0.1–0.7) 1.2 (0.3–3) 6.7 (5.3–20.1) |
| Parameters | Data | |
|---|---|---|
| MCC relapse MCC-specific | No MCC relapse, n (%) MCC relapse, n (%) Time to relapse, median (range), months No MCC-specific death, n (%) MCC-specific death, n (%) Time to death, median (range), months | 26 (55.3) 21 (44.7) 11 (2-122) 29 (61.7) 20 (38.3) 30 (3-122) |
| CCI score, median (range) | All patients Stage I Stage II Stage III Stage IV | 7 (4–15) 7 (4–9) 6.5 (5–9) 10.5 (7–14) 12 (7–15) |
| Comorbidities for CCI score, n (%) | History of myocardial infarction Congestive heart failure Peripheral vascular disease Cerebrovascular accident or TIA Hemiplegia Dementia COPD Connective tissue disease Peptic ulcer disease Moderate to severe liver disease Uncomplicated DM DM with end-organ damage Moderate to severe CKD Solid tumor (localized) Solid tumor (metastatic) Leukemia Lymphoma | 10 (21.3) 3 (6.4) 3 (6.4) 5 (10.3) 1 (2.1) 7 (14.9) 5 (10.6) 4 (8.5) 1 (2.1) 1 (2.1) 8 (17) 5 (10.6) 1 (2.1) 32 (68.1) 15 (31.9) 2 (4.3) 2 (4.3) |
| Parameters | p Value | Rank | p Value (Adjusted) |
|---|---|---|---|
| Elevated CRP | 0.001 | 1 | 0.01 * |
| MCC relapse | 0.003 | 2 | 0.01 * |
| MELD score | 0.003 | 3 | 0.01 * |
| CCI score | 0.01 | 4 | 0.025 * |
| MCC stage at diagnosis | 0.018 | 5 | 0.036 * |
| APRI score | 0.15 | 6 | 0.25 |
| Age | 0.28 | 7 | 0.4 |
| MCPyV | 0.39 | 8 | 0.49 |
| Immunosupression | 0.78 | 9 | 0.87 |
| Gender | 0.91 | 10 | 0.91 |
| Parameters | Hazard Ratio (HR) | 95% Confidence Interval (CI) | p Value |
|---|---|---|---|
| Elevated CRP | 2.3 | 0.79–6.4 | 0.13 |
| MCC stage at diagnosis | 2.9 | 1.23–6.6 | 0.015 * |
| MCC relapse | 2.1 | 0.64–6.7 | 0.22 |
| CCI score | 0.96 | 0.77–1.2 | 0.7 |
| MELD score | 1.2 | 1.04–1.3 | 0.009 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gambichler, T.; Becker, J.C.; Susok, L.; Käpynen, R.; Abu Rached, N. Model for End-Stage Liver Disease Correlates with Disease Relapse and Death of Patients with Merkel Cell Carcinoma. Cancers 2023, 15, 3195. https://doi.org/10.3390/cancers15123195
Gambichler T, Becker JC, Susok L, Käpynen R, Abu Rached N. Model for End-Stage Liver Disease Correlates with Disease Relapse and Death of Patients with Merkel Cell Carcinoma. Cancers. 2023; 15(12):3195. https://doi.org/10.3390/cancers15123195
Chicago/Turabian StyleGambichler, Thilo, Jürgen C. Becker, Laura Susok, Riina Käpynen, and Nessr Abu Rached. 2023. "Model for End-Stage Liver Disease Correlates with Disease Relapse and Death of Patients with Merkel Cell Carcinoma" Cancers 15, no. 12: 3195. https://doi.org/10.3390/cancers15123195
APA StyleGambichler, T., Becker, J. C., Susok, L., Käpynen, R., & Abu Rached, N. (2023). Model for End-Stage Liver Disease Correlates with Disease Relapse and Death of Patients with Merkel Cell Carcinoma. Cancers, 15(12), 3195. https://doi.org/10.3390/cancers15123195







