Nomogram to Predict the Long-Term Overall Survival of Early-Stage Hepatocellular Carcinoma after Radiofrequency Ablation
Abstract
Simple Summary
Abstract
1. Introduction
2. Material and Methods
2.1. Patients
2.2. RFA Procedure
2.3. Treatment Effect
2.4. Statistical Analysis and Nomogram Development
3. Results
3.1. Baseline Characteristics
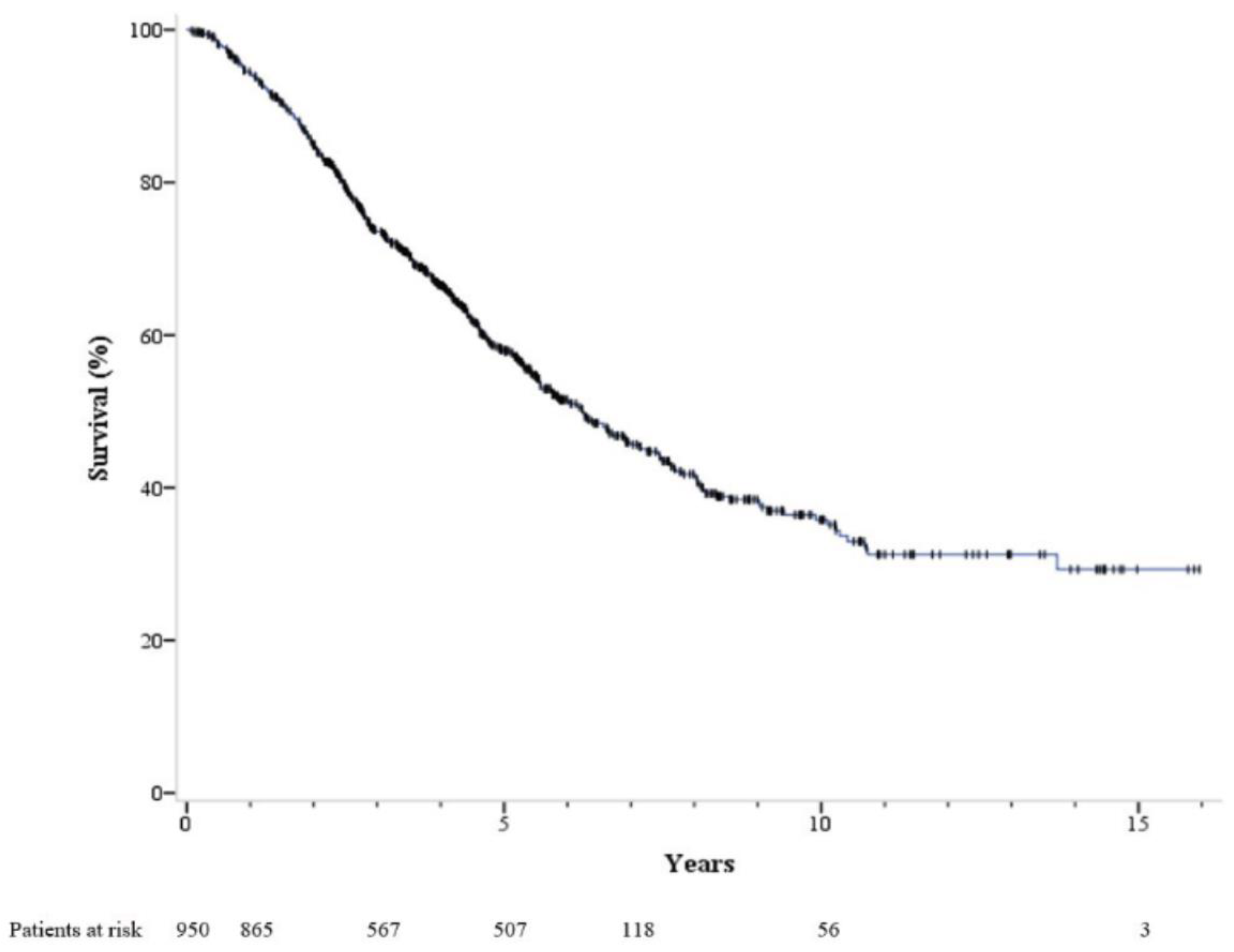
3.2. Overall Survival and Tumor Recurrence
3.3. Factors Associated with Mortality
3.4. Development of Nomogram
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Villanueva, A. Hepatocellular Carcinoma. N. Engl. J. Med. 2019, 380, 1450–1462. [Google Scholar] [CrossRef] [PubMed]
- The Cause of Death in Taiwan in 2018, Ministry of Health and Welfare (2019). 2018. Available online: https://www.mohw.gov.tw/cp-16-48057-1.html (accessed on 31 March 2023).
- Marrero, J.A.; Kulik, L.M.; Sirlin, C.B.; Zhu, A.X.; Finn, R.S.; Abecassis, M.M.; Roberts, L.R.; Heimbach, J.K. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2018, 68, 723–750. [Google Scholar] [CrossRef]
- Wang, J.-H.; Wang, C.-C.; Hung, C.-H.; Chen, C.-L.; Lu, S.-N. Survival comparison between surgical resection and radiofrequency ablation for patients in BCLC very early/early stage hepatocellular carcinoma. J. Hepatol. 2011, 56, 412–418. [Google Scholar] [CrossRef]
- Shiina, S.; Tateishi, R.; Arano, T.; Uchino, K.; Enooku, K.; Nakagawa, H.; Asaoka, Y.; Sato, T.; Masuzaki, R.; Kondo, Y.; et al. Radiofrequency Ablation for Hepatocellular Carcinoma: 10-Year Outcome and Prognostic Factors. Am. J. Gastroenterol. 2012, 107, 569–577. [Google Scholar] [CrossRef]
- Kim, Y.-S.; Lim, H.K.; Rhim, H.; Lee, M.W.; Choi, D.; Lee, W.J.; Paik, S.W.; Koh, K.C.; Lee, J.H.; Choi, M.S.; et al. Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: Analysis of prognostic factors. J. Hepatol. 2013, 58, 89–97. [Google Scholar] [CrossRef]
- Yang, W.; Yan, K.; Goldberg, S.N.; Ahmed, M.; Lee, J.-C.; Wu, W.; Zhang, Z.-Y.; Wang, S.; Chen, M.-H. Ten-year survival of hepatocellular carcinoma patients undergoing radiofrequency ablation as a first-line treatment. World J. Gastroenterol. 2016, 22, 2993–3005. [Google Scholar] [CrossRef]
- Kao, W.-Y.; Su, C.-W.; Chiou, Y.-Y.; Chiu, N.-C.; Liu, C.-A.; Fang, K.-C.; Huo, T.-I.; Huang, Y.-H.; Chang, C.-C.; Hou, M.-C.; et al. Hepatocellular Carcinoma: Nomograms Based on the Albumin-Bilirubin Grade to Assess the Outcomes of Radiofrequency Ablation. Radiology 2017, 285, 670–680. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Han, S.; Shim, J.H.; Kim, S.Y.; Won, H.J.; Shin, Y.M.; Kim, P.N.; An, J.; Lee, D.; Kim, K.M.; et al. A Patient-Based Nomogram for Predicting Overall Survival after Radiofrequency Ablation for Hepatocellular Carcinoma. J. Vasc. Interv. Radiol. 2015, 26, 1787–1794.e1. [Google Scholar] [CrossRef] [PubMed]
- Takuma, Y.; Shota, I.; Miyatake, H.; Uematsu, S.; Okamoto, R.; Araki, Y.; Takabatake, H.; Morimoto, Y.; Yamamoto, H. Nomograms to Predict the Disease-free Survival and Overall Survival after Radiofrequency Ablation for Hepatocellular Carcinoma. Intern. Med. 2018, 57, 457–468. [Google Scholar] [CrossRef]
- Ahmed, M.; Solbiati, L.; Brace, C.L.; Breen, D.J.; Callstrom, M.R.; Charboneau, J.W.; Chen, M.-H.; Choi, B.I.; De Baère, T.; Dodd, G.D., III; et al. Image-guided Tumor Ablation: Standardization of Terminology and Reporting Criteria—A 10-Year Update. Radiology 2014, 273, 241–260. [Google Scholar] [CrossRef] [PubMed]
- Levy, I.; Sherman, M. Staging of hepatocellular carcinoma: Assessment of the CLIP, Okuda, and Child-Pugh staging systems in a cohort of 257 patients in Toronto. Gut 2002, 50, 881. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.L.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of Liver Function in Patients With Hepatocellular Carcinoma: A New Evidence-Based Approach—The ALBI Grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.-H.; Xin, Y.-N.; Dong, Q.-J.; Wang, Q.; Jiang, X.-J.; Zhan, S.-H.; Sun, Y.; Xuan, S.-Y. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: An updated meta-analysis. Hepatology 2010, 53, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, X. Prognostic value of aspartate aminotransferase to platelet ratio index as a noninvasive biomarker in patients with hepatocellular carcinoma: A meta-analysis. Cancer Manag. Res. 2018, 10, 3023–3032. [Google Scholar] [CrossRef] [PubMed]
- McGlynn, K.A.; Petrick, J.L.; London, W.T. Global epidemiology of hepatocellular carcinoma: An emphasis on demographic and regional variability. Clin. Liver Dis. 2015, 19, 223–238. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Chen, Y.-J.; Ho, H.J.; Hsu, Y.-C.; Kuo, K.N.; Wu, M.-S.; Lin, J.-T. Association Between Nucleoside Analogues and Risk of Hepatitis B Virus–Related Hepatocellular Carcinoma Recurrence Following Liver Resection. JAMA 2012, 308, 1906–1914. [Google Scholar] [CrossRef]
- Kuo, Y.-H.; Huang, T.-H.; Wang, J.-H.; Chen, Y.-Y.; Tsai, M.-C.; Chen, Y.-H.; Lu, S.-N.; Hu, T.-H.; Chen, C.-H.; Hung, C.-H. Well-Controlled Viremia Predicts the Outcome of Hepatocellular Carcinoma in Chronic Viral Hepatitis Patients Treated with Sorafenib. Cancers 2022, 14, 3971. [Google Scholar] [CrossRef]
- Kuo, Y.H.; Wang, J.H.; Chang, K.C.; Hung, C.H.; Lu, S.N.; Hu, T.H.; Yen, Y.H.; Kee, K.M.; Chen, C.H. The influence of direct-acting antivirals in hepatitis C virus related hepatocellular carcinoma after curative treatment. Investig. New Drugs 2020, 38, 202–210. [Google Scholar] [CrossRef]
- Seko, Y.; Moriguchi, M.; Takahashi, A.; Yamaguchi, K.; Umemura, A.; Okuda, K.; Kataoka, S.; Unozawa, H.; Kobayashi, K.; Ogasawara, S.; et al. Hepatitis C virus eradication prolongs overall survival in hepatocellular carcinoma patients receiving molecular-targeted agents. J. Gastroenterol. 2022, 57, 90–98. [Google Scholar] [CrossRef]
- Huo, T.-I.; Wu, J.-C.; Lui, W.-Y.; Huang, Y.-H.; Lee, P.-C.; Chiang, J.-H.; Chang, F.-Y.; Lee, S.-D. Differential Mechanism and Prognostic Impact of Diabetes Mellitus on Patients with Hepatocellular Carcinoma Undergoing Surgical and Nonsurgical Treatment. Am. J. Gastroenterol. 2004, 99, 1479–1487. [Google Scholar] [CrossRef]
- Wang, Y.-G.; Wang, P.; Wang, B.; Fu, Z.-J.; Zhao, W.-J.; Yan, S.-L. Diabetes Mellitus and Poorer Prognosis in Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e95485. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-H.; Hsieh, S.-Y.; Chang, C.-C.; Wang, I.-K.; Huang, W.-H.; Weng, C.-H.; Hsu, C.-W.; Yen, T.-H. Hepatocellular carcinoma in hemodialysis patients. Oncotarget 2017, 8, 73154–73161. [Google Scholar] [CrossRef] [PubMed]
- Sato, M.; Tateishi, R.; Yasunaga, H.; Matsui, H.; Horiguchi, H.; Fushimi, K.; Koike, K. Mortality and hemorrhagic complications associated with radiofrequency ablation for treatment of hepatocellular carcinoma in patients on hemodialysis for end-stage renal disease: A nationwide survey. J. Gastroenterol. Hepatol. 2017, 32, 1873–1878. [Google Scholar] [CrossRef]
- Tsilimigras, D.I.; Bagante, F.; Sahara, K.; Moris, D.; Hyer, J.M.; Wu, L.; Ratti, F.; Marques, H.P.; Soubrane, O.; Paredes, A.Z.; et al. Prognosis After Resection of Barcelona Clinic Liver Cancer (BCLC) Stage 0, A, and B Hepatocellular Carcinoma: A Comprehensive Assessment of the Current BCLC Classification. Ann. Surg. Oncol. 2019, 26, 3693–3700. [Google Scholar] [CrossRef] [PubMed]
- Facciorusso, A.; El Aziz, M.A.A.; Tartaglia, N.; Ramai, D.; Mohan, B.P.; Cotsoglou, C.; Pusceddu, S.; Giacomelli, L.; Ambrosi, A.; Sacco, R. Microwave Ablation Versus Radiofrequency Ablation for Treatment of Hepatocellular Carcinoma: A Meta-Analysis of Randomized Controlled Trials. Cancers 2020, 12, 3796. [Google Scholar] [CrossRef] [PubMed]
- Pinter, M.; Trauner, M.; Peck-Radosavljevic, M.; Sieghart, W. Cancer and liver cirrhosis: Implications on prognosis and management. ESMO Open 2016, 1, e000042. [Google Scholar] [CrossRef]



| Variables | Overall (n = 950) | Training (n = 643) | Validation (n = 307) | p Value |
|---|---|---|---|---|
| Age (year) | 64.15 ± 10.30 | 64.06 ± 10.21 | 64.34 ± 10.48 | 0.523 |
| Sex | 0.721 | |||
| Male | 591 (62.2%) | 397 (61.7%) | 194 (63.2%) | |
| Female | 359 (37.8%) | 246 (38.3%) | 113 (36.8%) | |
| BMI (kg/m2) | 25.41 ± 3.95 | 25.45 ± 3.87 | 25.32 ± 4.11 | 0.375 |
| HBsAg(+) | 393 (41.4%) | 265 (41.2%) | 128 (41.7%) | 0.888 |
| Anti-HCV(+) | 517 (54.4%) | 363 (56.5%) | 154 (50.2%) | 0.071 |
| Albumin (g/dL) | 3.79 ± 0.65 | 3.78 ± 0.65 | 3.82 ± 0.61 | 0.053 |
| Total bilirubin (mg/dL) | 1.15 ± 0.58 | 1.03 ± 0.54 | 1.02 ± 0.52 | 0.793 |
| AST (U/L) | 62.43 ± 44.68 | 63.41 ± 44.80 | 60.36 ± 44.41 | 0.291 |
| ALT (U/L) | 60.45 ± 48.58 | 61.13 ± 48.49 | 59.03 ± 48.81 | 0.762 |
| INR | 1.06 ± 0.09 | 1.06 ± 0.10 | 1.06 ± 0.08 | 0.058 |
| Platelet count (×103/mm3) | 130.7 ± 61.35 | 129.5 ± 61.17 | 133.0 ± 62.09 | 0.437 |
| Creatinine (mg/dL) | 1.43 ± 1.71 | 1.41 ± 1.65 | 1.44 ± 1.84 | 0.412 |
| Child-Pugh score | 0.348 | |||
| A | 830 (87.4%) | 557 (86.6%) | 273 (88.9%) | |
| B | 120 (12.6%) | 86 (13.4%) | 34 (11.1%) | |
| ALBI grade | 0.670 | |||
| 1 | 400 (42.1%) | 273 (42.5%) | 127 (41.4%) | |
| 2 | 500 (52.6%) | 339 (52.7%) | 161 (52.4%)) | |
| 3 | 50 (5.3%) | 31 (4.8%) | 19 (6.2%) | |
| Diabetes mellitus | 324 (34.1%) | 213 (33.1%) | 111 (36.2%) | 0.380 |
| End-stage renal disease | 80 (8.4%) | 54 (8.4%) | 26 (8.5%) | 1.000 |
| Tumor size | 0.034 | |||
| <3 cm | 834 (87.8%) | 575 (89.4%) | 259 (84.4%) | |
| ≥3 cm | 116 (12.2%) | 68 (10.6%) | 48 (15.6%) | |
| Tumor number | 0.614 | |||
| 1 | 749 (78.8%) | 502 (78.1%) | 247 (80.5%) | |
| 2 | 162 (17.1%) | 115 (17.9%) | 47 (15.3%) | |
| 3 | 39 (4.1%) | 26 (4.0%) | 13 (4.2%) | |
| TNM stage | 0.496 | |||
| I | 751 (79.1%) | 504 (78.4%) | 247 (80.5%) | |
| II | 198 (20.9%) | 139 (21.6%) | 60 (19.5%) | |
| BCLC stage (0/A) | 0.826 | |||
| 0 | 323 (34.0%) | 217 (33.7%) | 106 (34.0%) | |
| A | 627 (66.0%) | 426 (66.3%) | 201 (66.0%) | |
| CLIP score | 0.741 | |||
| 0 | 601 (63.6%) | 402 (62.5%) | 199 (64.8%) | |
| 1 | 297 (31.3%) | 203 (31.6%) | 94 (30.6%) | |
| 2 | 46 (4.8%) | 33 (5.1%) | 13 (4.2%)) | |
| 3 | 6 (0.6%) | 5 (0.8%) | 1 (0.3%) |
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age (≥65 vs. <65) | 1.42 (1.13–1.79) | 0.003 | 1.29 (1.02–1.63) | 0.034 |
| Sex (Male vs. Female) | 1.19 (0.94–1.52) | 0.150 | ||
| HBsAg (+) vs. (−) | 0.78 (0.64–0.95) | 0.015 | ||
| Anti-HCV (+ vs. −) | 1.20 (0.99–1.46) | 0.063 | ||
| DM (Yes vs. No) | 1.44 (1.14–1.84) | 0.002 | 1.47 (1.16–1.87) | 0.002 |
| ESRD (Yes vs. No) | 1.38 (0.96–1.99) | 0.081 | 1.41 (0.98–2.03) | 0.066 |
| AFP (≥20 vs. <20 ng/mL) | 1.25 (1.03–1.52) | 0.022 | ||
| Total bilirubin (≥1.4 vs. <1.4 mg/dL) | 1.77 (1.40–2.24) | <0.001 | ||
| Albumin (<3.5 vs. ≥3.5 g/dL) | 1.97 (1.62–2.40) | <0.001 | ||
| PT (INR ≥1.2 vs. <1.2) | 1.58 (1.22–2.03) | <0.001 | ||
| AST (≥37 vs. <37 U/L) | 1.47 (1.19–1.83) | <0.001 | ||
| ALT (≥40 vs. <40 U/L) | 1.07 (0.88–1.29) | 0.507 | ||
| AAR (≥1 vs. <1) | 1.45 (1.19–1.77) | <0.001 | ||
| Platelet (<15 vs. ≥15 × 104/uL) | 1.42 (1.15–1.76) | 0.001 | ||
| ALBI grade | ||||
| 1 | 1 | 1 | ||
| 2 | 2.36 (1.88–2.95) | <0.001 | 2.05 (1.54–2.73) | <0.001 |
| 3 | 3.83 (2.59–5.68) | <0.001 | 3.49 (2.19–5.59) | <0.001 |
| APRI (≥1 vs. <1) | 1.87 (1.54–2.27) | <0.001 | 1.58 (1.23–2.02) | <0.001 |
| FIB-4 (≥3.25 vs. <3.25) | 1.77 (1.43–2.18) | <0.001 | ||
| Child-Pugh class (B vs. A) | 2.25 (1.76–2.88) | <0.001 | ||
| Tumor size (≥3 cm vs. <3 cm) | 1.41 (1.08–1.84) | 0.011 | 1.65 (1.15–2.37) | 0.007 |
| Tumor number (>1 vs. 1) | 1.38 (1.10–1.72) | 0.005 | 1.43 (1.08–1.89) | 0.013 |
| Training Cohort | Validation Cohort | ||
|---|---|---|---|
| Variables | C-Index (95% CI) | Variables | C-Index (95% CI) |
| Nomogram | 0.645 (0.610–0.679) | Nomogram | 0.683 (0.631–0.734) |
| TNM | 0.519 (0.493–0.546) | TNM | 0.537 (0.497–0.577) |
| BCLC | 0.553 (0.525–0.582) | BCLC | 0.618 (0.579–0.657) |
| CLIP | 0.557 (0.525–0.589) | CLIP | 0.592 (0.545–0.639) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuo, Y.-H.; Huang, T.-H.; Yen, Y.-H.; Lu, S.-N.; Wang, J.-H.; Hung, C.-H.; Chen, C.-H.; Tsai, M.-C.; Kee, K.-M. Nomogram to Predict the Long-Term Overall Survival of Early-Stage Hepatocellular Carcinoma after Radiofrequency Ablation. Cancers 2023, 15, 3156. https://doi.org/10.3390/cancers15123156
Kuo Y-H, Huang T-H, Yen Y-H, Lu S-N, Wang J-H, Hung C-H, Chen C-H, Tsai M-C, Kee K-M. Nomogram to Predict the Long-Term Overall Survival of Early-Stage Hepatocellular Carcinoma after Radiofrequency Ablation. Cancers. 2023; 15(12):3156. https://doi.org/10.3390/cancers15123156
Chicago/Turabian StyleKuo, Yuan-Hung, Tzu-Hsin Huang, Yi-Hao Yen, Sheng-Nan Lu, Jing-Houng Wang, Chao-Hung Hung, Chien-Hung Chen, Ming-Chao Tsai, and Kwong-Ming Kee. 2023. "Nomogram to Predict the Long-Term Overall Survival of Early-Stage Hepatocellular Carcinoma after Radiofrequency Ablation" Cancers 15, no. 12: 3156. https://doi.org/10.3390/cancers15123156
APA StyleKuo, Y.-H., Huang, T.-H., Yen, Y.-H., Lu, S.-N., Wang, J.-H., Hung, C.-H., Chen, C.-H., Tsai, M.-C., & Kee, K.-M. (2023). Nomogram to Predict the Long-Term Overall Survival of Early-Stage Hepatocellular Carcinoma after Radiofrequency Ablation. Cancers, 15(12), 3156. https://doi.org/10.3390/cancers15123156







