UAS™—A Urine Preservative for Oncology Applications
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Pre-Evaluation of the Need for Urine Preservation
2.2. Evaluation of Urine Storage Conditions with UAS™ Preservative
2.2.1. Sample Collection
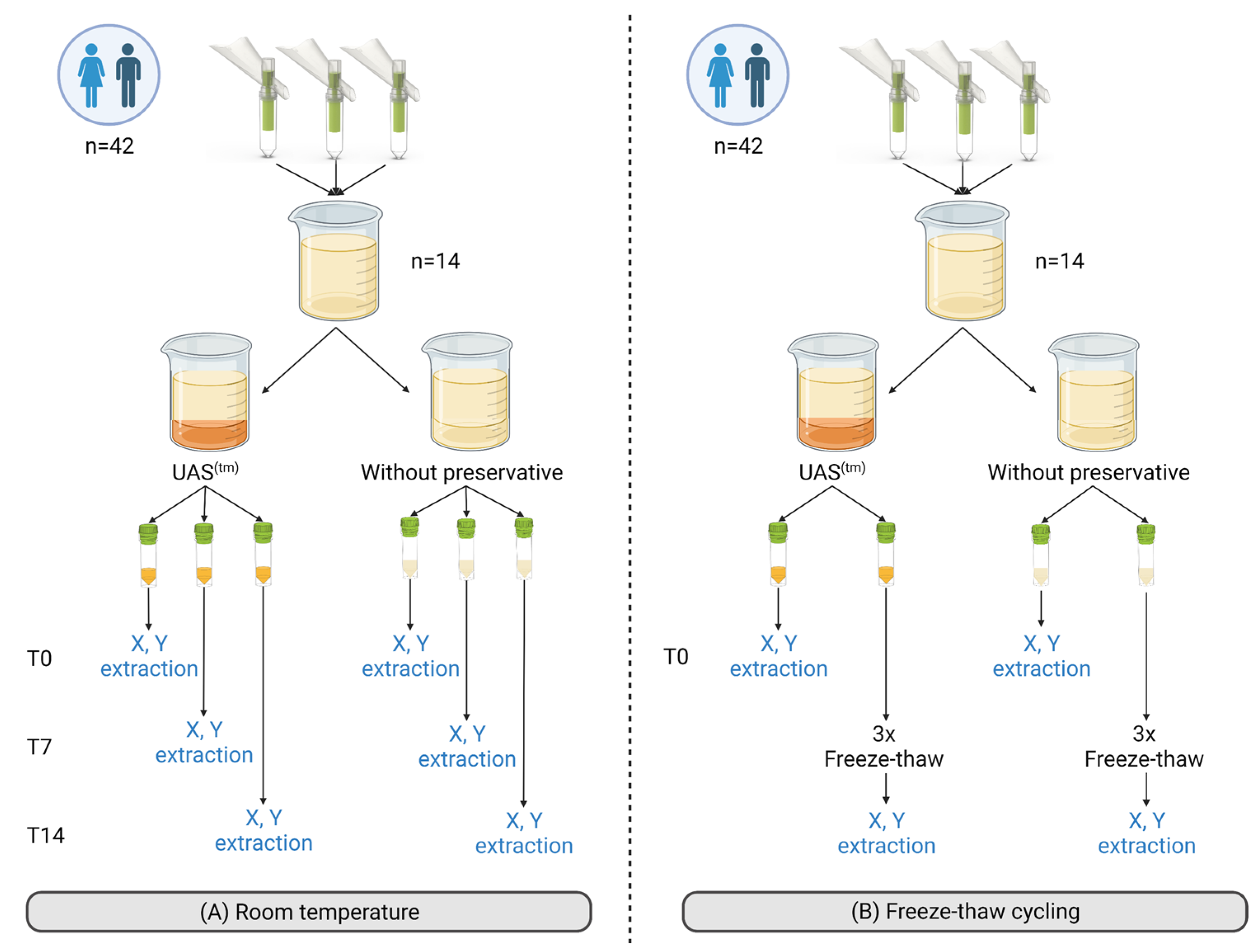
2.2.2. Experimental Set-Up
- UAS™ preservative performance during storage at room temperature
- 2.
- UAS™ preservative performance after freeze-thaw cycling
2.2.3. Extractions
- Sample processing
- Cell-free total nucleic acid extraction
- Cellular pellet extraction
2.2.4. PCR Analysis
2.3. UAS™ Preservative Performance on Clinical Samples during Collection and Storage
2.3.1. Sample Collection
2.3.2. Experimental Set-Up
2.3.3. Cell-Free DNA Extractions
2.3.4. Analysis
2.4. Statistical Analysis
3. Results
3.1. Pre-Evaluation of the Need for Urine Preservation
3.2. Evaluation of the UAS™ Preservative for Urine Storage
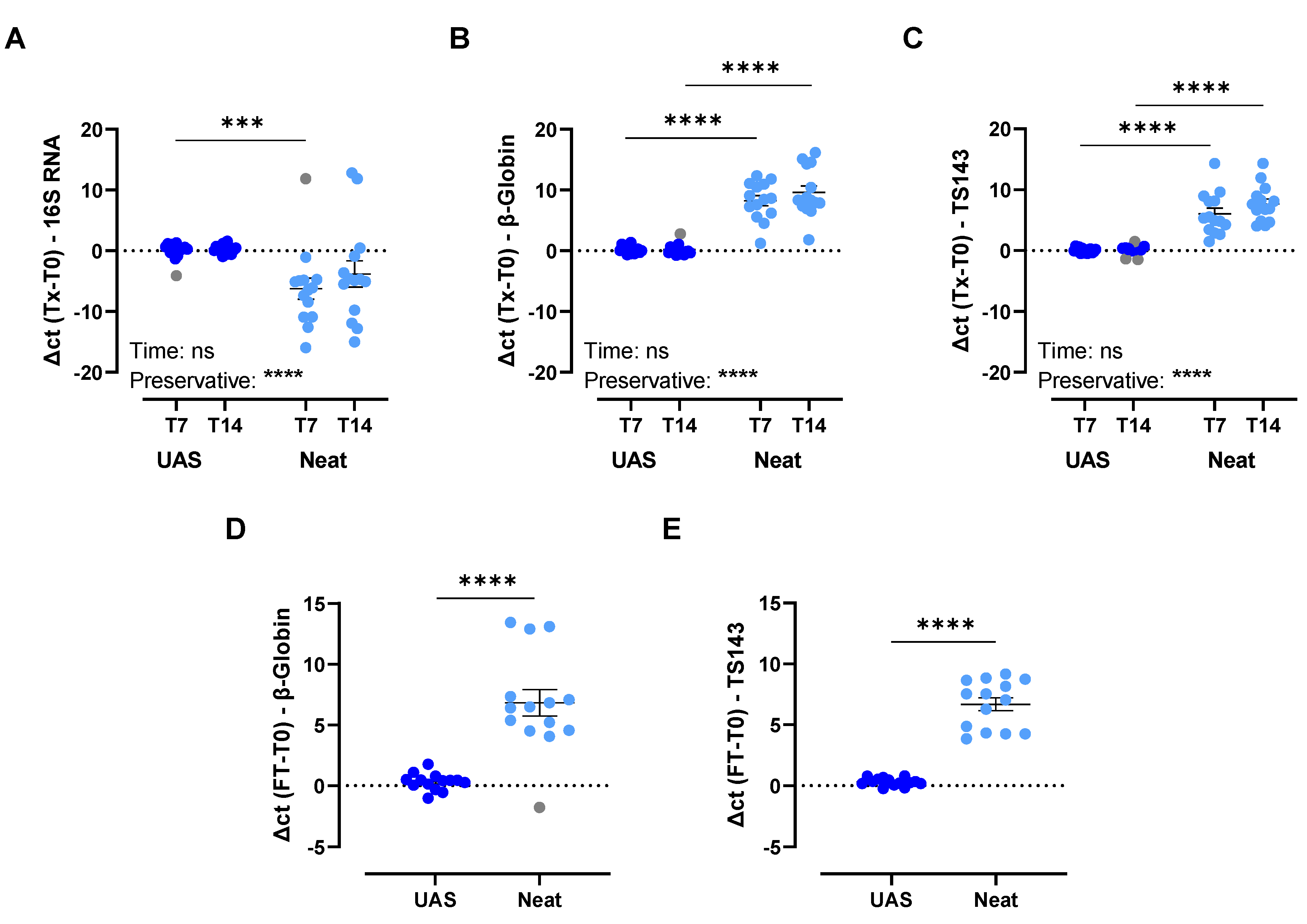
3.2.1. Storage at Room Temperature for up to 14 Days
3.2.2. Impact of Simulated Shipping Conditions
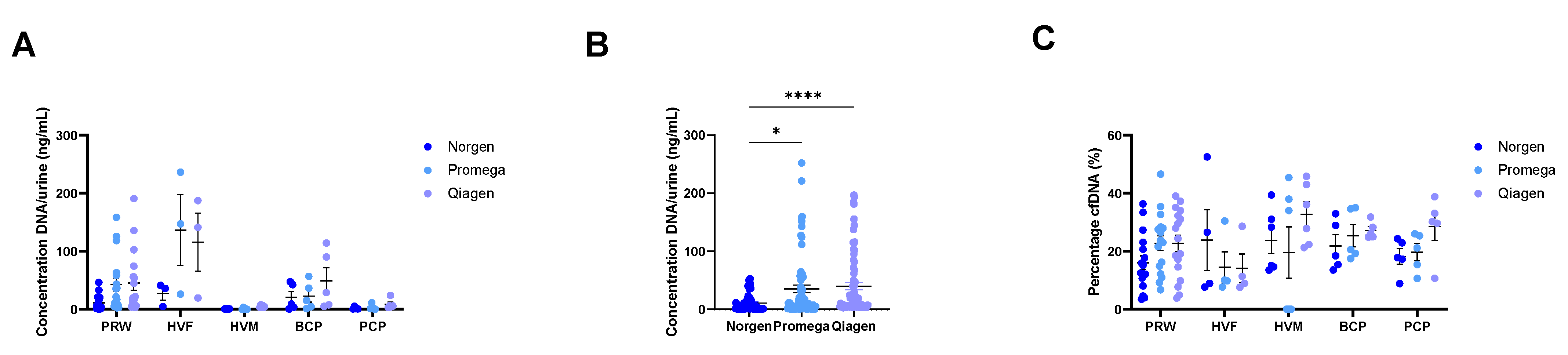
3.3. Evaluation of First-Void Urine Preserved with UAS™ and Compatibility with Three Commercially Available Isolation Methods for Urinary cfDNA
4. Discussion
4.1. Importance of Urinary Analyte Preservation
4.2. Performance of UAS™ Preservative
4.3. Clinical Applicability of First-Void Urine Preserved with UAS™
4.4. Strengths, Limitations, and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BCP | Breast cancer patient |
| cDNA | Copy DNA |
| cfDNA | Cell-free DNA |
| cfTNA | Cell-free total nucleic acids |
| EDTA | Ethylenediaminetetraacetic acid |
| FP | Female pooled urine samples |
| HVF | Healthy volunteer female |
| HVM | Healthy volunteer male |
| ISEV | International Society for Extracellular Vesicles |
| lncRNA | Long non-coding RNA |
| miRNA | microRNA |
| MP | Male pooled urine samples |
| NTC | Non-template control |
| PCP | Prostate cancer patient |
| PRW | Pregnant women |
| RT | Room temperature |
| UZA | Antwerp University Hospital |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Tsui, N.B.; Jiang, P.; Chow, K.C.; Su, X.; Leung, T.Y.; Sun, H.; Chan, K.C.; Chiu, R.W.; Lo, Y.M. High resolution size analysis of fetal DNA in the urine of pregnant women by paired-end massively parallel sequencing. PLoS ONE 2012, 7, e48319. [Google Scholar] [CrossRef] [PubMed]
- Di Meo, A.; Bartlett, J.; Cheng, Y.; Pasic, M.D.; Yousef, G.M. Liquid biopsy: A step forward towards precision medicine in urologic malignancies. Mol. Cancer 2017, 16, 80. [Google Scholar] [CrossRef] [PubMed]
- Larsen, L.K.; Lind, G.E.; Guldberg, P.; Dahl, C. DNA-Methylation-Based Detection of Urological Cancer in Urine: Overview of Biomarkers and Considerations on Biomarker Design, Source of DNA, and Detection Technologies. Int. J. Mol. Sci. 2019, 20, 2657. [Google Scholar] [CrossRef] [PubMed]
- Kretschmer-Kazemi Far, R.; Frank, K.; Sczakiel, G. Sampling, Logistics, and Analytics of Urine for RT-qPCR-based Diagnostics. Cancers 2021, 13, 4381. [Google Scholar] [CrossRef]
- Jordaens, S.; Zwaenepoel, K.; Tjalma, W.; Deben, C.; Beyers, K.; Vankerckhoven, V.; Pauwels, P.; Vorsters, A. Urine biomarkers in cancer detection: A systematic review of preanalytical parameters and applied methods. Int. J. Cancer 2023, 152, 2186–2205. [Google Scholar] [CrossRef]
- Dermody, S.M.; Bhambhani, C.; Swiecicki, P.L.; Brenner, J.C.; Tewari, M. Trans-Renal Cell-Free Tumor DNA for Urine-Based Liquid Biopsy of Cancer. Front. Genet. 2022, 13, 879108. [Google Scholar] [CrossRef]
- Su, Y.H.; Wang, M.; Brenner, D.E.; Ng, A.; Melkonyan, H.; Umansky, S.; Syngal, S.; Block, T.M. Human urine contains small, 150 to 250 nucleotide-sized, soluble DNA derived from the circulation and may be useful in the detection of colorectal cancer. J. Mol. Diagn. 2004, 6, 101–107. [Google Scholar] [CrossRef]
- Bryzgunova, O.E.; Laktionov, P.P. Extracellular Nucleic Acids in Urine: Sources, Structure, Diagnostic Potential. Acta Nat. 2015, 7, 48–54. [Google Scholar] [CrossRef]
- Peng, M.; Chen, C.; Hulbert, A.; Brock, M.V.; Yu, F. Non-blood circulating tumor DNA detection in cancer. Oncotarget 2017, 8, 69162–69173. [Google Scholar] [CrossRef]
- Lu, T.; Li, J. Clinical applications of urinary cell-free DNA in cancer: Current insights and promising future. Am. J. Cancer Res. 2017, 7, 2318–2332. [Google Scholar]
- Vorsters, A.; Micalessi, I.; Bilcke, J.; Ieven, M.; Bogers, J.; Van Damme, P. Detection of human papillomavirus DNA in urine. A review of the literature. Eur. J. Clin. Microbiol. Infect Dis. 2012, 31, 627–640. [Google Scholar] [CrossRef]
- Bosschieter, J.; Bach, S.; Bijnsdorp, I.V.; Segerink, L.I.; Rurup, W.F.; van Splunter, A.P.; Bahce, I.; Novianti, P.W.; Kazemier, G.; van Moorselaar, R.J.A.; et al. A protocol for urine collection and storage prior to DNA methylation analysis. PLoS ONE 2018, 13, e0200906. [Google Scholar] [CrossRef]
- Locke, W.J.; Guanzon, D.; Ma, C.; Liew, Y.J.; Duesing, K.R.; Fung, K.Y.C.; Ross, J.P. DNA Methylation Cancer Biomarkers: Translation to the Clinic. Front. Genet. 2019, 10, 1150. [Google Scholar] [CrossRef] [PubMed]
- Arora, A. Stabilizing Composition and Method for Preserving a Bodily Fluid. Patent WO 2021/195768 A1, 30 March 2021. p. 110. [Google Scholar]
- Jung, M.; Klotzek, S.; Lewandowski, M.; Fleischhacker, M.; Jung, K. Changes in concentration of DNA in serum and plasma during storage of blood samples. Clin. Chem. 2003, 49, 1028–1029. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.Y.; Linehan, J.A.; Wilson, T.G.; Hoon, D.S.B. Emerging Utility of Urinary Cell-free Nucleic Acid Biomarkers for Prostate, Bladder, and Renal Cancers. Eur. Urol. Focus 2017, 3, 265–272. [Google Scholar] [CrossRef]
- Cannas, A.; Kalunga, G.; Green, C.; Calvo, L.; Katemangwe, P.; Reither, K.; Perkins, M.D.; Maboko, L.; Hoelscher, M.; Talbot, E.A.; et al. Implications of storing urinary DNA from different populations for molecular analyses. PLoS ONE 2009, 4, e6985. [Google Scholar] [CrossRef]
- Zhou, Q.; Liu, F.; Guo, L.; Chen, R.; Yuan, X.; Li, C.; Shu, L.; Liu, H.; Zhou, Y.; Wu, Y.; et al. A novel urine cell-free DNA preservation solution and its application in kidney transplantation. Nephrology 2021, 26, 684–691. [Google Scholar] [CrossRef]
- Wang, X.; Gu, H.; Palma-Duran, S.A.; Fierro, A.; Jasbi, P.; Shi, X.; Bresette, W.; Tasevska, N. Influence of Storage Conditions and Preservatives on Metabolite Fingerprints in Urine. Metabolites 2019, 9, 203. [Google Scholar] [CrossRef]
- Kouri, T.; Vuotari, L.; Pohjavaara, S.; Laippala, P. Preservation of urine for flow cytometric and visual microscopic testing. Clin Chem 2002, 48, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Thongboonkerd, V.; Saetun, P. Bacterial overgrowth affects urinary proteome analysis: Recommendation for centrifugation, temperature, duration, and the use of preservatives during sample collection. J. Proteome Res. 2007, 6, 4173–4181. [Google Scholar] [CrossRef] [PubMed]
- Barra, G.B.; Santa Rita, T.H.; de Almeida Vasques, J.; Chianca, C.F.; Nery, L.F.; Santana Soares Costa, S. EDTA-mediated inhibition of DNases protects circulating cell-free DNA from ex vivo degradation in blood samples. Clin. Biochem. 2015, 48, 976–981. [Google Scholar] [CrossRef] [PubMed]
- Vorsters, A.; Van den Bergh, J.; Micalessi, I.; Biesmans, S.; Bogers, J.; Hens, A.; De Coster, I.; Ieven, M.; Van Damme, P. Optimization of HPV DNA detection in urine by improving collection, storage, and extraction. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 2005–2014. [Google Scholar] [CrossRef]
- Eisinger, S.W.; Schwartz, M.; Dam, L.; Riedel, S. Evaluation of the BD Vacutainer Plus Urine C&S Preservative Tubes compared with nonpreservative urine samples stored at 4 degrees C and room temperature. Am. J. Clin. Pathol. 2013, 140, 306–313. [Google Scholar] [CrossRef]
- Li, P.; Ning, J.; Luo, X.; Du, H.; Zhang, Q.; Zhou, G.; Du, Q.; Ou, Z.; Wang, L.; Wang, Y. New method to preserve the original proportion and integrity of urinary cell-free DNA. J. Clin. Lab. Anal. 2019, 33, e22668. [Google Scholar] [CrossRef]
- Hoppin, J.A.; Ulmer, R.; Calafat, A.M.; Barr, D.B.; Baker, S.V.; Meltzer, H.M.; Ronningen, K.S. Impact of urine preservation methods and duration of storage on measured levels of environmental contaminants. J. Expo. Sci. Environ. Epidemiol. 2006, 16, 39–48. [Google Scholar] [CrossRef]
- Bax, C.; Lotesoriere, B.J.; Sironi, S.; Capelli, L. Review and Comparison of Cancer Biomarker Trends in Urine as a Basis for New Diagnostic Pathways. Cancers 2019, 11, 1244. [Google Scholar] [CrossRef] [PubMed]
- Norgen Biotek Corp. Urine Cell-Free Circulating DNA Purification Kit: Protocol. Available online: https://norgenbiotek.com/product/urine-cell-free-circulating-dna-purification-maxi-kit (accessed on 20 June 2022).
- Qiagen. QIAamp Circulating Nucleic Acid Kit: Handbook. Available online: https://www.qiagen.com/us/products/discovery-and-translational-research/dna-rna-purification/dna-purification/cell-free-dna/qiaamp-circulating-nucleic-acid-kit/?catno=55114 (accessed on 20 June 2022).
- Promega. Maxwell® RSC ccfDNA Plasma Kit. Available online: https://be.promega.com/products/nucleic-acid-extraction/genomic-dna/maxwell-rsc-ccfdna-plasma-kit/?catNum=AS1840#protocols (accessed on 20 June 2022).


| PCR Assay | Master Mix | Forward Primer | Reverse Primer |
|---|---|---|---|
| Human β-globin qPCR [16] | 2X iTaq Universal SYBR Master mix (Bio-Rad) | 5′-ACACAACTGTGTTCACTAGC-3′ | 5′-CAACTTCATCCACGTTCACC-3′ |
| 16S qPCR | Taq DNA Polymerase + Syto 9-based in-house master mix | 5′-ATTACCGCGGCTGCTGG-3′ | 5′-CCTACGGGAGGCAGCAG-3′ |
| TS143 qPCR | 5′-GCCCTCTGCCAGTTCTA-3′ | 5′-GCCCTCTGCCAGTTCTA-3′ |
| Steps | Human β-Globin qPCR | 16S qPCR | TS143 qPCR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Initial heat activation | 5 min | 95 °C | 1× | 2 min | 95 °C | 1× | 5 min | 95 °C | 1× |
| Denaturation | 20 s | 95 °C | 45× | 30 s | 95 °C | 35× | 20 s | 95 °C | 35× |
| Annealing/Extension | 30 s | 56 °C | 20 s | 55 °C | 20 s | 55 °C | |||
| 20 s | 72 °C | 30 s | 72 °C | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jordaens, S.; Arora, A.; MacDonald, K.W.; Wood, C.; Hendrickx, J.O.; Zwaenepoel, K.; Deben, C.; Tjalma, W.; Pauwels, P.; Beyers, K.; et al. UAS™—A Urine Preservative for Oncology Applications. Cancers 2023, 15, 3119. https://doi.org/10.3390/cancers15123119
Jordaens S, Arora A, MacDonald KW, Wood C, Hendrickx JO, Zwaenepoel K, Deben C, Tjalma W, Pauwels P, Beyers K, et al. UAS™—A Urine Preservative for Oncology Applications. Cancers. 2023; 15(12):3119. https://doi.org/10.3390/cancers15123119
Chicago/Turabian StyleJordaens, Stephanie, Amit Arora, Kyle W. MacDonald, Cameron Wood, Jhana O. Hendrickx, Karen Zwaenepoel, Christophe Deben, Wiebren Tjalma, Patrick Pauwels, Koen Beyers, and et al. 2023. "UAS™—A Urine Preservative for Oncology Applications" Cancers 15, no. 12: 3119. https://doi.org/10.3390/cancers15123119
APA StyleJordaens, S., Arora, A., MacDonald, K. W., Wood, C., Hendrickx, J. O., Zwaenepoel, K., Deben, C., Tjalma, W., Pauwels, P., Beyers, K., & Vankerckhoven, V. (2023). UAS™—A Urine Preservative for Oncology Applications. Cancers, 15(12), 3119. https://doi.org/10.3390/cancers15123119








