1. Introduction
Neuroendocrine neoplasms (NENs) are broadly classified according to their morphological differentiation and proliferative rate in well-differentiated neuroendocrine tumours (WdNETs) (grade (G)1–2 (Ki-67 < 20%) or G3 (Ki-67 ≥ 20%, usually ≤50%)) and in poorly differentiated neuroendocrine carcinomas (PdNECs) (always G3, Ki-67 ≥ 20%) [
1]. However, this histopathological classification only partially captures the biological heterogeneity within this family of tumours, and a more granular biological subtyping is needed to deliver more personalised treatment to patients with NENs.
The molecular profiling of tumours is becoming of increasing relevance in the management of patients with advanced cancer due to its potential to identify targetable molecular alterations and predictive biomarkers that can inform new treatments. In relation to the use of next-generation sequencing (NGS) technologies in neuroendocrine neoplasms (NENs), the current recommendation from the European Society for Medical Oncology (ESMO) is to assess the tumour mutational burden (TMB), an estimate of the rate of somatic mutations within a tumour genome, in WdNETs [
2], as this may predict the tumour’s response to immunotherapy. This recommendation is based on the results of a prospective exploratory analysis of the multi-cohort phase II KEYNOTE-158 trial, which assessed the activity of the programmed death-1 inhibitor Pembrolizumab in previously treated patients with 10 different cancer types, including NETs. This analysis reported a response rate of 29% in patients with a high TMB (≥10 mutations/megabase (Mb)) using targeted NGS in diagnostic tumour tissues, as opposed to 6% in patients with a lower TMB [
3].
Overall, the published literature supports the use of the multi-omic profiling of NENs as a tool to better understand their underlying biology and to identify the NEN molecular subtypes with potential clinical implications [
4]. One of the largest studies in this regard was published by Scarpa and colleagues, who explored the whole-genome landscape of 102 sporadic pancreatic NETs (PanNETs) [
5]. This study showed that 17% of PanNETs harbour germline mutations affecting DNA repair genes (e.g.,
MUTYH,
CHEK2 and
BRCA2), or the genes
MEN1 and
VHL. Somatic mutations or fusions are most commonly found in genes involved in four pathways: chromatin remodelling, DNA damage repair, mTOR signalling activation and telomere maintenance. Integrative transcriptomic analysis identified an additional PanNET subgroup associated with hypoxia and HIF signalling.
Van Riet and colleagues explored the genomic landscape of 85 advanced NENs (69 WdNETs and 16 PdNECs) of different primary origin: 68 from different gastro-entero-pancreatic (GEP) sites, 7 from the lung and 12 of unknown origin [
6]. They showed a relatively high average TMB of 5.45 somatic mutations/Mb, with
TP53, KRAS, RB1, CSMD3, APC, CSMD1, LRATD2, TRRAP and
MYC as major drivers in PdNECs, compared to an overall low TMB in WdNETs (average of 1.09 somatic mutations/Mb), with the different repertoires of gene drivers affected by somatic aberrations in pancreatic (
MEN1, ATRX, DAXX, DMD and
CREBBP) and midgut (
CDKN1B) NETs.
Hong et al. assessed the mutational and copy number variation (CNV) profiles of 211 PanNETs, confirming that insulinomas had different genomic features than other non-functional (NF)-PanNETs [
7], and reclassified these tumours into novel molecular subtypes. Some of the subgroups identified were associated with a higher relapse risk.
The newly defined G3-WdNETs [
8] have also been genomically characterised. Williamson and colleagues showed that G3-WdNETs of pancreatic origin exhibited a
TSC1-disrupting fusion and a
CHD7–BEND2 fusion, and lacked any somatic variants in
ATRX, DAXX and
MEN1 [
9].
There are two main challenges to incorporating the molecular profiling of NENs into standard clinical practice. Firstly, the clinical utility of molecular profiling beyond the determination of TMB remains unclear, especially from a therapeutic perspective [
2]. In relation to the targetable alterations identified, 42 of 85 samples (49%) from the patients with advanced NEN, in a series explored by Van Riet and colleagues, harboured a potential therapeutic target, with a predominance of NEC within these patients (15/42; 36%), followed by PanNETs (11/42; 26%) [
6]. These targetable alterations were associated with the available “on-label” treatment options in 21 cases; in the other 21, they were associated with “off-label” therapies. Secondly, adequate profiling requires a minimum of 20% of tumour content; this might be difficult to achieve as the NEN tumour tissue remaining after a standard histopathological diagnostic work-up is usually of poor quantity or quality, and the efficient recovery of DNA/RNA from archival tumour tissues is challenging. In addition, it is extremely difficult to make a decision about the right technology to apply (whole-genome, whole-exome or RNA-sequencing) in an extremely volatile context regarding the cost and constant evolution of technology. Cell-free DNA may offer an easily accessible, alternative source of fresh tumour material for genomic characterisation; the profiling of its DNA fraction, namely ctDNA, has proven informative and clinically useful in different cancer types, and may also find application in patients with NENs [
10,
11]. In addition, ctDNA readouts, if detectable, can be measured over time to monitor changes in tumour burden and genomic profile.
This study aimed to assess the feasibility of ctDNA molecular profiling using a targeted NGS platform in patients with WdNETs, and its potential to guide clinical management.
2. Methods
Patients previously diagnosed with advanced NENs underwent molecular profiling (ctDNA) using the FoundationLiquid® testing platform (72 cancer-related genes) between April and November 2019, in the framework of a collaboration between The Christie NHS Foundation Trust (Manchester, UK) and Foundation Medicine (Roche®, Basel, Switzerland). This platform allows for the identification of pathogenic and likely pathogenic somatic and germline variants, herein defined as “pathological alterations,” including base substitutions, insertions, deletions, copy number alterations and chromosomal rearrangements. It also reports on high microsatellite instability (MSI-h). Patients provided written informed consent for molecular profiling to be performed; in addition, the retrospective analysis of these data was approved by the institutional Audit Committee (approval number 19/2634).
Patients with a histologically confirmed WdNET diagnosis, as per the 2019 World Health Organisation Classification parameters (WHO editorial Board, 2019), were included in this analysis; patients diagnosed with non-WdNETs, such as paraganglioma, goblet cell adenocarcinoma or PdNECs, were used for comparative purposes only. Clinical baseline characteristics, demographic and treatment data were collected. Molecular profiling information was extracted, including the success of sample analysis, the presence or absence of pathological alterations and the mutant allele frequency (MAF) for pathological alterations.
The aim of the study was to assess the feasibility and the clinical impact of ctDNA molecular profiling in WdNETs. The primary end-point was to assess the percentage of WdNET ctDNA samples that failed testing (defined as those scenarios where insufficient DNA was isolated for analysis). Secondary end-points included defining the proportion of the sample in which pathological findings were identified, and the percentage of patients for whom management changed based on molecular profiling results.
Descriptive statistical analysis using STATA v.12 was performed. The Chi-Square test, Fisher’s exact test and t-test were used, when appropriate. A two-sided p-value < 0.05 was considered statistically significant.
3. Results
Samples from 45 patients were included: 15 WdNETs and 30 non-WdNETs.
3.1. Patient Characteristics
Within the total of the 15 individual patients with WdNETs (accounting for 18 ctDNA samples) (
Table 1), 8 were female (53.33%), with a median age of 63.2 years (range 23.5–86.8). Most were small-bowel-primary patients (8 patients; 53.33%) (pancreas (5; 33.33%), gastric (1; 6.67%) and unknown primary (1; 6.67%)) and grade 2 patients (9; 60.00%) (grade 1 (5; 33.33%), grade 3 (1; 6.67%)), with a median Ki-67 of 5% (range 1–30). All patients with WdNET had a metastatic disease and seven were on treatment (three somatostatin analogues; four chemotherapy) at the time of the ctDNA sample acquisition.
3.2. Feasibility and Main Findings of ctDNA-Based Molecular Profiling
A total of 5 WdNETs samples (27.78%) failed analysis (vs. 17.65% in non-WdNETs;
p-value 0.395) (
Figure 1).
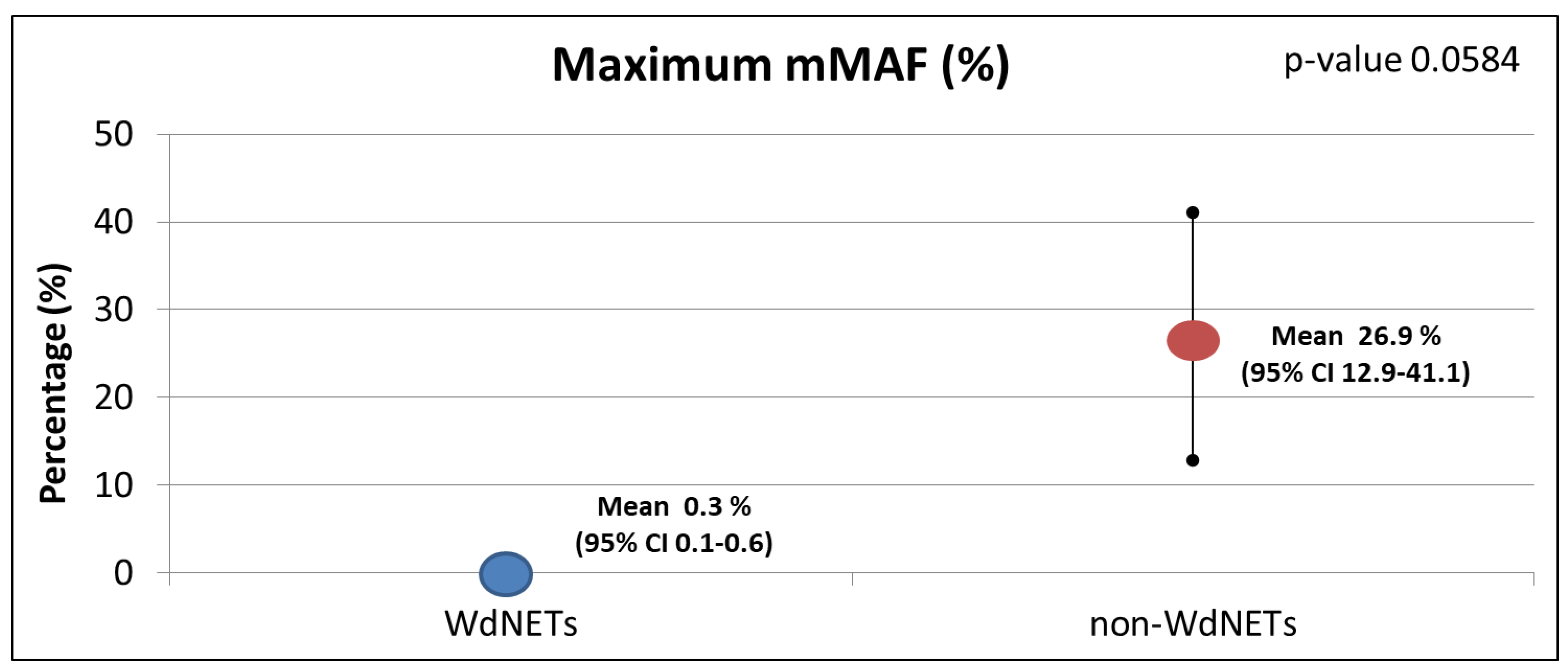
Of the 13 WdNET samples with a successful ctDNA analysis, pathological alterations were identified in 6 (46.15%) (vs. 82.14% in non-WdNETs;
p-value 0.018) (
Figure 2). In addition, there was a lower maximum MAF in WdNETs (mean 0.33) vs. non-WdNETs (mean 26.99), even though differences did not reach statistical significance (
p-value 0.0584) (
Figure 3). The rate of findings of unclear significance was similar between WdNETs (69.23%) and non-WdNETs (78.57%) (
p-value 0.517).
Within the WdNET cohort, there was a higher presence of pathological mutations in G2 tumours (grade 1: 0%, grade 2: 66.67%;
p-value 0.07) and in patients who were not receiving ongoing, concomitant anti-cancer systemic therapy at the time of the ctDNA sampling (no treatment: 66.67%, on treatment: 28.57%;
p-value 0.286;
Figure 4).
3.3. Identified Pathological Alterations and Impact on Management
A total of six pathological alterations were identified within the WdNET samples, including the CDKN2A mutation (one sample), CHEK2 mutation (one sample), TP53 mutation (two samples), FGFR2 amplification (one sample), IDH2 mutation (one sample), CTNNB1 mutation (one sample), NF1 mutation (one sample) and PALB2 mutation (one sample). Concomitant alterations were identified in two samples (one had two alterations (the CHEK2 and TP53 mutations) and another had three (the CTNNB1, NF1 and PALB2 mutations)). The other four samples had one unique pathological alteration each.
None (0% of samples) of the identified pathological findings were considered potentially targetable. Thus, ctDNA-based molecular profiling did not change therapeutic management for any of the patients with a WdNET (0% of patients).
4. Discussion
Although feasible, the role of molecular profiling using ctDNA seems to be limited in clinical decision making for patients with advanced WdNETs. The rate of identification of pathological alterations and the reported mMAF were significantly lower than in non-WdNETs. This is despite WdNETs having a similar sample failure rate to that described for non-Wd NETs, suggesting that the results are not associated with an increased rate of analysis failure in WdNETs (or a small amount of tumour-derived DNA in the bloodstream), but rather with a lower prevalence of significant alterations in this group of patients. Therefore, molecular profiling may be more relevant in non-WdNETs than in WdNETs. This is in line with the findings of genomic profiling studies of NEN tumour tissue showing that somatic mutations are less frequent in WdNETs than in PdNECs [
6,
12].
Although molecular profiling of WdNETs has been widely utilised to better understand the biology of these malignancies, true precision medicine therapeutic approaches in this patient group are currently non-existent [
13]. Other series exploring targetable alterations in WdNETs have reported a higher rate of targetable alterations [
6,
10], which may be due to the differing definitions of “targetable” used, which ideally should follow evidence-based definitions [
14]. It would also be of interest to understand how many of those patients were actually matched to a specific treatment based on the molecular alteration identified. While there are widely available data on this for other malignancies, data in WdNETs are scarce. The MOSCATO-01 clinical trial prospectively evaluated the clinical benefit of utilising high-throughput genomic analyses to identify actionable molecular alterations and match patients with a specific targeted therapy [
15]. Of the total of 1035 patients included, 199 patients were matched with a specific treatment; within the group that received matched treatment, 11% of patients achieved an objective response, and a progression-free survival (PFS)2/PFS1 ratio of >1.3 was identified in 33% of patients. Ten patients with “thyroid and other endocrine glands” were included in this study. Of these, only two received a “matched” treatment. This corroborates the challenges of identifying targetable alterations in NENs.
Despite in-depth research on the identification of relevant molecular pathways in NETs [
16], the development of precision medicine approaches represents one of the most relevant challenges in the current management of patients with NENs [
17]. Beyond developments in the arena of nuclear medicine, which is rapidly developing new theragnostic approaches [
18], predictive biomarkers for systemic therapy selection in WdNETs are lacking [
19,
20,
21].
Interestingly, the findings of this study corroborate previous evidence suggesting that the dysregulation of cell-cycle/DNA damage repair (e.g.,
TP53, CDKN2A, CHEK2, PALB2) is a recurrent, critical biological vulnerability of WdNETs [
5], highlighting the rationale for its therapeutic exploitation. Ongoing trials are evaluating the potential role of targeting such alterations. In addition, trials evaluating peptide-receptor radionuclide therapies in combination with DNA damage repair inhibitors, for patients with WdNETs expressing somatostatin receptors (e.g., ClinicalTrials.gov NCT04086485, NCT05053854), do also exist.
In addition to the potential therapeutic impact of molecular alterations, the identification of specific, presumed somatic mutations in ctDNA should trigger germ-line testing in selected cases, where there is the potential for a known underlying hereditary syndrome in patients with WdNETs, such as multiple endocrine neoplasia (MEN) syndromes, Von Hippel–Lindau disease (VHL), Neurofibromatosis 1 (NF1) syndrome and Tuberous sclerosis (TS) [
22].
The limitations of this study include the small sample size, the heterogeneity of the tumour type and treatment administered and the potential selection bias at the time of selecting patients for molecular profiling, as non-consecutive patients were considered for this. In addition, the series included a mix of advanced-stage and prior-line therapy patients, and there was no access to concomitant tissue profiling, which would have been of interest. However, a strength of this study was that all patients were tested with identical technologies and within the same time frame. In addition, the presence of a cohort of patients with non-WdNETs allowed us to put the findings into context, providing our results with more robustness and allowing for clinical interpretation.
Finally, the NGS platform used here included 70 ‘pan-cancer’-related genes, yet excluded a number of genes commonly altered in WdNETs, such as MUTYH, ATRX, DAXX and MEN1; a WdNET-specific gene panel, developed on the basis of more recent NGS data from large NEN datasets, may allow for the increased sensitivity of ctDNA detection in these patients.
5. Conclusions
The use of molecular profiling utilising ctDNA in WdNETs is feasible, but the results are currently unlikely to identify targetable alterations that may impact patient management. While patients with WdNETs should still be offered molecular profiling (if available and reimbursed), it is important to manage patient expectations in relation to the likelihood of the results impacting their management. It is possible that, due to the nature of these malignancies, which have generally low numbers of somatic mutations, the evolution of the field from exclusive ctDNA profiling to a combination of mutational analyses and epigenetic changes (including methylation analyses) will have an impact on the expansion of molecular profiling’s use as a tool for neuroendocrine tumours, expanding from prognosis to the uncovering of new targets.
Author Contributions
Study design: A.L.; Data collection: A.L., J.B. and M.F.; Data analysis: A.L.; Preparation of first manuscript draft: A.L.; Recruitment of patients: A.L., J.B., M.F., Z.K., W.M., M.G.M., R.A.H. and J.W.V.; Review and approval of final manuscript: A.L., J.B., M.F., Z.K., W.M., M.G.M., R.A.H. and J.W.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding; access to FoundationOne Liquid was provided by Roche®.
Institutional Review Board Statement
The retrospective analysis of these data was approved by the institutional Audit Committee (approval number 19/2634) on 4 December 2019.
Informed Consent Statement
Patients provided written informed consent for molecular profiling to be performed.
Data Availability Statement
Data can be made available upon request.
Acknowledgments
Angela Lamarca has been partially-funded by The Christie Charity. Access to FoundationOne Liquid was provided by Roche®. The salary of Zain Kapacee was funded by The Christie Charity. The salary of Melissa Frizziero was funded by a European Neuroendocrine Tumour Society Centre of Excellence Young Investigator grant.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. Access to FoundationOne Liquid® was provided by Roche®. Angela Lamarca: travel and educational support from Ipsen, Pfizer, Bayer, AAA, Sirtex, Novartis, Mylan and Delcath; speaker honoraria from Merck, Pfizer, Ipsen, Incyte, AAA, QED, Servier, Astra Zeneca and EISAI; advisory and consultancy honoraria from EISAI, Nutricia Ipsen, QED, Roche, Servier, Boston Scientific and Albireo Pharma; member of the Knowledge Network and NETConnect Initiatives funded by Ipsen. Melissa Frizziero has no conflicts of interest to declare. Jorge Barriuso: J.B. reports grants, personal fees and non-financial support from Ipsen; personal fees and non-financial support from Pfizer, Novartis; non-financial support from AAA, Nanostring, Roche; grants and personal fees from Servier; and personal fees from Nutricia outside the submitted work. Zainul Kapacee has received educational support from EISAI. Mairéad G McNamara: received research grant support from Servier, Ipsen and NuCana. She has received travel and accommodation support from Bayer and Ipsen and speaker honoraria from Advanced Accelerator Applications (UK & Ireland) Ltd., Pfizer, Ipsen, NuCana and Mylan. She has served on advisory boards for Celgene, Ipsen, Sirtex and Baxalta. Richard Hubner has served on the advisory board for Roche, BMS, Eisai, Celgene, Beigene, Ipsen and BTG. He has received speaker fees from Eisai, Ipsen, Mylan and PrimeOncology, and has received travel and educational support from Bayer, BMS, IPSEN and Roche, all outside of the scope of this work. Juan W Valle: consulting or advisory role for Agios, AstraZeneca, Delcath Systems, Keocyt, Genoscience Pharma, Incyte, Ipsen, Merck, Mundipharma EDO, Novartis, PCI Biotech, Pfizer, Pieris Pharmaceuticals, QED and Wren Laboratories; member of the Speakers’ Bureau for Imaging Equipment Limited Ipsen Novartis Nucana; and received travel grants from Celgene and Nucana.
References
- Nagtegaal, I.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, M.K.; Carneiro, F.; Cree, I.A.; the WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mosele, F.; Remon, J.; Mateo, J.; Westphalen, C.; Barlesi, F.; Lolkema, M.; Normanno, N.; Scarpa, A.; Robson, M.; Meric-Bernstam, F.; et al. Recommendations for the use of next-generation sequencing (NGS) for patients with metastatic cancers: A report from the ESMO Precision Medicine Working Group. Ann. Oncol. 2020, 31, 1491–1505. [Google Scholar] [CrossRef]
- Marabelle, A.; Fakih, M.; Lopez, J.; Shah, M.; Shapira-Frommer, R.; Nakagawa, K.; Chung, H.C.; Kindler, H.L.; Lopez-Martin, J.A.; Miller, W.H.; et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: Prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 2020, 21, 1353–1365. [Google Scholar] [CrossRef]
- Jiang, R.; Hong, X.; Zhao, Y.; Wu, W. Application of multiomics sequencing and advances in the molecular mechanisms of pancreatic neuroendocrine neoplasms. Cancer Lett. 2021, 499, 39–48. [Google Scholar] [CrossRef]
- Scarpa, A.; Chang, D.K.; Nones, K.; Corbo, V.; Patch, A.-M.; Bailey, P.; Lawlor, R.T.; Johns, A.L.; Miller, D.K.; Mafficini, A.; et al. Whole-genome landscape of pancreatic neuroendocrine tumours. Nature 2017, 543, 65–71. [Google Scholar] [CrossRef]
- Van Riet., J.; Van De Werken, H.J.G.; Cuppen, E.; Eskens, F.A.L.M.; Tesselaar, M.; Van Veenendaal, L.M.; Klümpen, H.J.; Dercksen, M.W.; Valk, G.D.; Lolkema, M.P. The genomic landscape of 85 advanced neuroendocrine neoplasms reveals subtype-heterogeneity and potential therapeutic targets. Nat. Commun. 2021, 12, 4612. [Google Scholar] [CrossRef]
- Hong, X.; Qiao, S.; Li, F.; Wang, W.; Jiang, R.; Wu, H.; Chen, H.; Liu, L.; Peng, J.; Wang, J.; et al. Whole-genome sequencing reveals distinct genetic bases for insulinomas and non-functional pancreatic neuroendocrine tumours: Leading to a new classification system. Gut 2020, 69, 877–887. [Google Scholar] [CrossRef] [Green Version]
- De Mestier, L.; Lamarca, A.; Hernando, J.; Zandee, W.; Alonso-Gordoa, T.; Perrier, M.; Walenkamp, A.M.; Chakrabarty, B.; Landolfi, S.; Van Velthuysen, M.L.F.; et al. Treatment outcomes of advanced digestive well-differentiated grade 3 NETs. Endocr. Relat. Cancer 2021, 28, 549–561. [Google Scholar] [CrossRef]
- Williamson, L.M.; Steel, M.; Grewal, J.K.; Thibodeau, M.L.; Zhao, E.Y.; Loree, J.M.; Yang, K.C.; Gorski, S.M.; Mungall, A.; Mungall, K.L.; et al. Genomic characterization of a well-differentiated grade 3 pancreatic neuroendocrine tumor. Mol. Case Stud. 2019, 5, a003814. [Google Scholar] [CrossRef]
- Burak, G.I.; Ozge, S.; Cem, M.; Gulgun, B.; Zeynep, D.Y.; Atil, B. The emerging clinical relevance of genomic profiling in neuroendocrine tumours. BMC Cancer 2021, 21, 234. [Google Scholar] [CrossRef]
- Shah, D.; Lamarca, A.; Valle, J.; McNamara, M. The Potential Role of Liquid Biopsies in Advancing the Understanding of Neuroendocrine Neoplasms. J. Clin. Med. 2021, 10, 403. [Google Scholar] [CrossRef]
- Venizelos, A.; Elvebakken, H.; Perren, A.; Nikolaienko, O.; Deng, W.; Lothe, I.M.B.; Couvelard, A.; Hjortland, G.O.; Sundlöv, A.; Svensson, J.; et al. The molecular characteristics of high-grade gastroenteropancreatic neuroendocrine neoplasms. Endocr. Relat. Cancer 2021, 29, 1–14. [Google Scholar] [CrossRef]
- Rindi, G.; Wiedenmann, B. Neuroendocrine neoplasia of the gastrointestinal tract revisited: Towards precision medicine. Nat. Rev. Endocrinol. 2020, 16, 590–607. [Google Scholar] [CrossRef]
- Mateo, J.; Chakravarty, D.; Dienstmann, R.; Jezdic, S.; Gonzalez-Perez, A.; Lopez-Bigas, N.; Ng, C.K.Y.; Bedard, P.; Tortora, G.; Douillard, J.-Y.; et al. A framework to rank genomic alterations as targets for cancer precision medicine: The ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). Ann. Oncol. 2018, 29, 1895–1902. [Google Scholar] [CrossRef]
- Massard, C.; Michiels, S.; Ferté, C.; Le Deley, M.-C.; Lacroix, L.; Hollebecque, A.; Verlingue, L.; Ileana, E.; Rosellini, S.; Ammari, S.; et al. High-Throughput Genomics and Clinical Outcome in Hard-to-Treat Advanced Cancers: Results of the MOSCATO 01 Trial. Cancer Discov. 2017, 7, 586–595. [Google Scholar] [CrossRef] [Green Version]
- Patel, P.; Galoian, K. Molecular challenges of neuroendocrine tumors. Oncol. Lett. 2018, 15, 2715–2725. [Google Scholar] [CrossRef]
- Barriuso, J.; Lamarca, A. Clinical and Translational Research Challenges in Neuroendocrine Tumours. Curr. Med. Chem. 2020, 27, 4823–4839. [Google Scholar] [CrossRef]
- Langbein, T.; Weber, W.A.; Eiber, M. Future of Theranostics: An Outlook on Precision Oncology in Nuclear Medicine. J. Nucl. Med. 2019, 60, 13S–19S. [Google Scholar] [CrossRef] [Green Version]
- Megdanova-Chipeva, V.G.; Lamarca, A.; Backen, A.; McNamara, M.G.; Barriuso, J.; Sergieva, S.; Gocheva, L.; Mansoor, W.; Manoharan, P.; Valle, J.W. Systemic Treatment Selection for Patients with Advanced Pancreatic Neuroendocrine Tumours (PanNETs). Cancers 2020, 12, 1988. [Google Scholar] [CrossRef]
- Barriuso, J.; Custodio, A.; Afonso, R.; Alonso, V.; Astudillo, A.; Capdevila, J.; García-Carbonero, R.; Grande, E.; Jimenez-Fonseca, P.; Marazuela, M.; et al. Prognostic and predictive biomarkers for somatostatin analogs, peptide receptor radionuclide therapy and serotonin pathway targets in neuroendocrine tumours. Cancer Treat. Rev. 2018, 70, 209–222. [Google Scholar] [CrossRef]
- De Dosso, S.; Treglia, G.; Pascale, M.; Tamburello, A.; Santhanam, P.; Kroiss, A.S.; Pereira Mestre, R.; Saletti, P.; Giovanella, L. Detection rate of unknown primary tu-mour by using somatostatin receptor PET/CT in patients with metastatic neuroendocrine tumours: A meta-analysis. Endocrine 2019, 64, 456–468. [Google Scholar] [CrossRef]
- Bocchini, M.; Nicolini, F.; Severi, S.; Bongiovanni, A.; Ibrahim, T.; Simonetti, G.; Grassi, I.; Mazza, M. Biomarkers for Pancreatic Neuroendocrine Neoplasms (PanNENs) Management—An Updated Review. Front. Oncol. 2020, 10, 831. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).