Carcinoid Crisis: A Misunderstood and Unrecognized Oncological Emergency
Simple Summary
Abstract
1. Introduction
2. Aim
3. Materials and Methods
4. Clinical Definition and Presentation
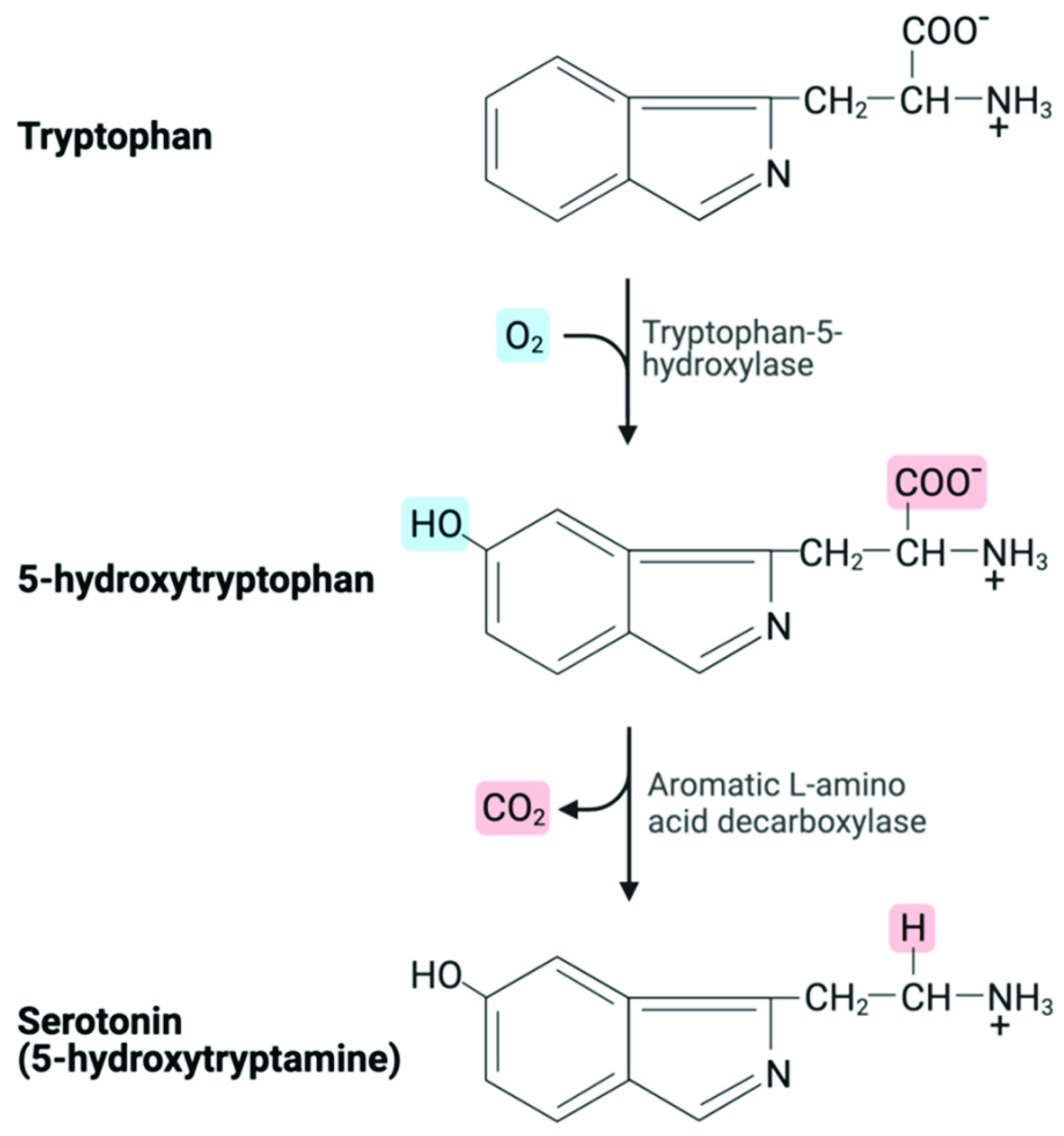
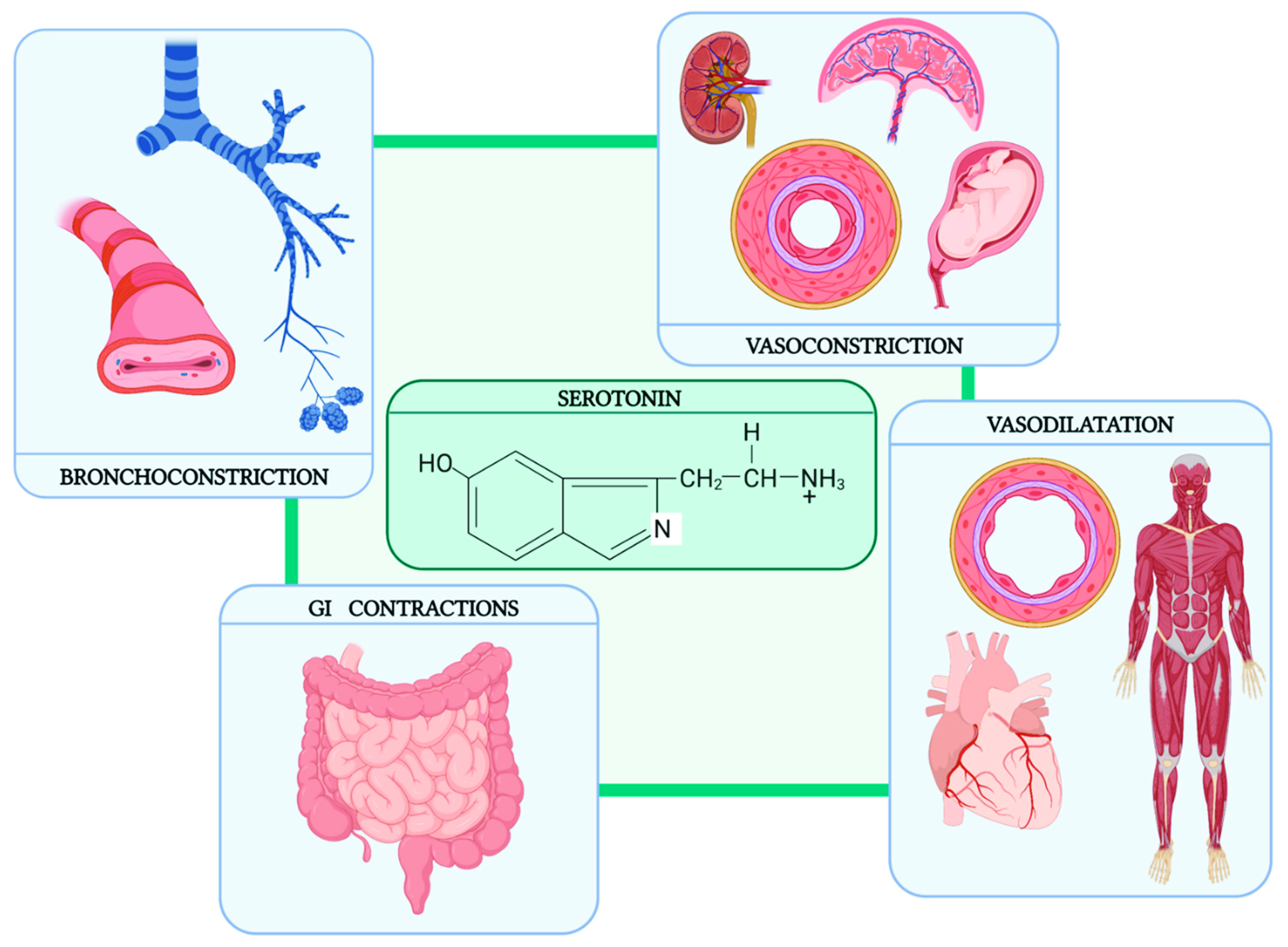
5. Etiopathogenesis of Carcinoid Crisis
6. Carcinoid Crisis Management
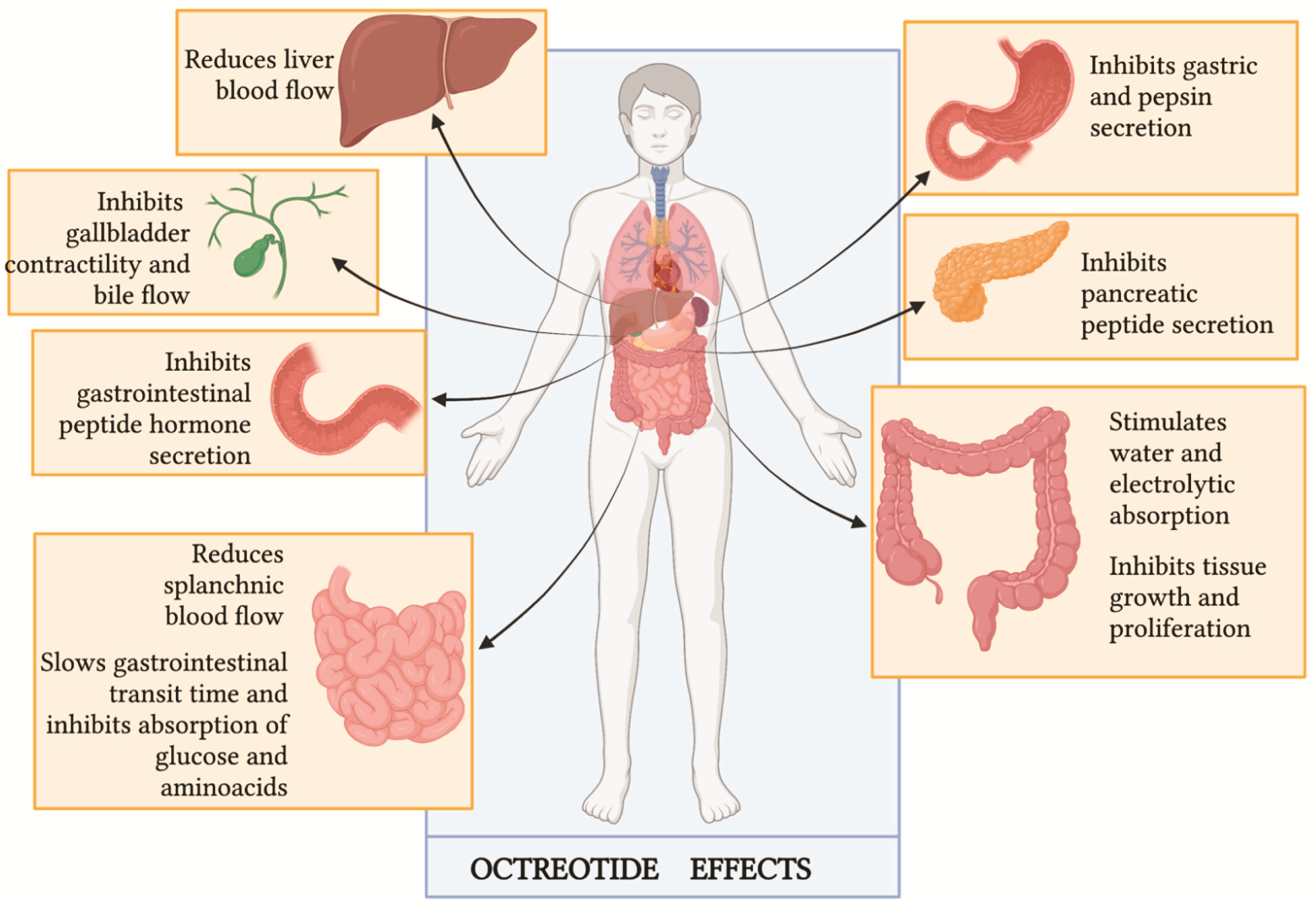
6.1. Octreotide
- -
- The evaluation of nutritional assessment with the diagnosis and correction of hydro electrolytic disorders, malnutrition and malabsorption, and the avoidance of food triggers and intensive physical exercises the previous day;
- -
- The evaluation of NET characteristics (high tumor burden, use of somatostatin analogs to control CS).
6.2. Vasopressors
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sjoerdsma, A.; Weissbach, H.; Udenfriend, S. A clinical, physiologic and biochemical study of patients with malignant car-cinoid (argentaffinoma). Am. J. Med. 1956, 20, 520–532. [Google Scholar] [CrossRef]
- Kahil, M.E.; Brown, H.; Fred, H.L. The carcinoid crisis. Arch. Intern. Med. 1964, 114, 26–28. [Google Scholar] [CrossRef] [PubMed]
- Tomassetti, P.; Migliori, M.; Lalli, S.; Campana, D.; Tomassetti, V.; Corinaldesi, R. Epidemiology, clinical features and diagno-sis of gastroenteropancreatic endocrine tumours. Ann. Oncol. 2001, 12, S95–S99. [Google Scholar] [CrossRef] [PubMed]
- Fujie, S.; Zhou, W.; Fann, P.; Yen, Y. Carcinoid crisis 24 h after bland embolization: A case report. Biosci. Trends 2010, 4, 143–144. [Google Scholar]
- Ozgen, A.; Demirkazik, F.; Arat, A. Carcinoid crisis provoked by mammographic compression of metastatic carcinoid tu-mour of the breast. Clin. Radiol. 2001, 56, 250–251. [Google Scholar] [CrossRef]
- Salm, E.F.; Janssen, M.; Breburda, C.S.; Van Woerkens, L.J.P.; De Herder, W.W.; Zwaan, C.V.; Roelandt, J.R.T. Carcinoid crisis during transesophageal echocardiography. Intensiv. Care Med. 2000, 26, 254. [Google Scholar] [CrossRef]
- Morrisroe, K.; Sim, I.-W.; McLachlan, K.; Inder, W.J. Carcinoid crisis induced by repeated abdominal examination. Intern. Med. J. 2012, 42, 342–344. [Google Scholar] [CrossRef]
- Magabe, P.C.; Bloom, A.L. Sudden death from carcinoid crisis during image-guided biopsy of a lung mass. J. Vasc. Interv. Ra-diol. 2014, 25, 484–487. [Google Scholar] [CrossRef]
- Kinney, M.A.O.; Warner, M.E.; Nagorney, D.M.; Rubin, J.; Schroeder, D.R.; Maxson, P.M. Perianaesthetic risks and outcomes of abdominal surgery for metastatic carcinoid tumours †. Br. J. Anaesth. 2001, 87, 447–452. [Google Scholar] [CrossRef]
- Massimino, K.; Harrskog, O.; Pommier, S.; Pommier, R. Octreotide LAR and bolus octreotide are insufficient for preventing intraoperative complications in carcinoid patients. J. Surg. Oncol. 2013, 107, 842–846. [Google Scholar] [CrossRef]
- Condron, M.E.; Pommier, S.J.; Pommier, R.F. Continuous infusion of octreotide combined with perioperative octreotide bolus does not prevent intraoperative carcinoid crisis. Surgery 2016, 159, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.H.; Paciorek, A.; Mulvey, C.K.; Chan, H.; Fidelman, N.; Meng, L.; Nakakura, E.K.; Zhang, L.; Bergsland, E.K.; Van Loon, K. Periprocedural management of patients undergoing liver resection or embolotherapy for neuroendocrine tumor me-tastases. Pancreas 2019, 48, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.L.; Smith, I.E. Tryptophan in the treatment of carcinoid crisis. Cancer Chemother. Pharmacol. 1983, 10, 137–139. [Google Scholar] [CrossRef]
- Hughes, E.W.; Hodkinson, B.P. Carcinoid syndrome: The combined use of ketanserin and octreotide in the management of an acute crisis during anaesthesia. Anaesth. Intensiv. Care 1989, 17, 367–370. [Google Scholar] [CrossRef]
- Batchelor, A.; Conacher, I. Anaphylactoid or carcinoid? Br. J. Anaesth. 1992, 69, 325–327. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Parry, R.G.; Glover, S.; Dudley, C.R.K. Acute renal failure associated with carcinoid crisis. Nephrol. Dial. Transplant. 1996, 11, 2489–2490. [Google Scholar] [CrossRef]
- Koopmans, K.P.; Brouwers, A.H.; De Hooge, M.N.; Van der Horst-Schrivers, A.N.; Kema, I.P.; Wolffenbuttel, B.H.; De Vries, E.G.; Jager, P.L. Carcinoid crisis after injection of 6-18F-fluorodihydroxyphenylalanine in a patient with metastatic carcinoid. J. Nucl. Med. 2005, 46, 1240–1243. [Google Scholar]
- Papadogias, D.; Makras, P.; Kossivakis, K.; Kontogeorgos, G.; Piaditis, G.; Kaltsas, G. Carcinoid syndrome and carcinoid crisis secondary to a metastatic carcinoid tumour of the lung: A therapeutic challenge. Eur. J. Gastroenterol. Hepatol. 2007, 19, 1154–1159. [Google Scholar] [CrossRef]
- Van Diepen, S.; Sobey, A.; Lewanczuk, R.; Singh, G.; Sidhu, S.; Zibdawi, M.; Mullen, J.C. A case of acute respiratory distress syndrome responsive to methylene blue during a carcinoid crisis. Can. J. Anaesth. 2013, 60, 1085–1088. [Google Scholar] [CrossRef]
- Kromas, M.L.; Passi, Y.; Kuzumi, C.; Shikhar, S. Intra-operative carcinoid crisis: Revised anaesthesia management. Indian J. Anaesth. 2017, 61, 443–444. [Google Scholar] [CrossRef]
- Maddali, M.V.; Chiu, C.; Cedarbaum, E.R.; Yogeswaran, V.; Seedahmed, M.; Smith, W.; Bergsland, E.; Fidelman, N.; Kenne-dy, J.L. Carcinoid crisis–induced acute systolic heart failure. JACC Case Rep. 2020, 2, 2068–2071. [Google Scholar] [CrossRef] [PubMed]
- Dhanani, J.; Pattison, D.A.; Burge, M.; Williams, J.; Riedel, B.; Hicks, R.J.; Reade, M.C. Octreotide for resuscitation of cardiac arrest due to carcinoid crisis precipitated by novel peptide receptor radionuclide therapy (PRRT): A case report. J. Crit. Care 2020, 60, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Mahdi, M.; Ozer, M.; Tahseen, M. A Challenging case of carcinoid crisis in a patient with neuroendocrine tumor. Cureus 2021, 13, e15626. [Google Scholar] [CrossRef] [PubMed]
- Del Olmo-García, M.I.; Muros, M.A.; López-De-La-Torre, M.; Agudelo, M.; Bello, P.; Soriano, J.M.; Merino-Torres, J.-F. Pre-vention and management of hormonal crisis during theragnosis with LU-DOTA-TATE in neuroendocrine tumors. A system-atic review and approach proposal. J. Clin. Med. 2020, 9, 2203. [Google Scholar] [CrossRef]
- Seymour, N.; Sawh, S.C. Mega-dose intravenous octreotide for the treatment of carcinoid crisis: A systematic review. Can. J. Anaesth. 2013, 60, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Condron, M.E.; Jameson, N.E.; Limbach, K.E.; Bingham, A.E.; Sera, V.A.; Anderson, R.B.; Schenning, K.; Yockelson, S.; Ha-rukuni, I.; Kahl, E.A.; et al. A prospective study of the pathophysiology of carcinoid crisis. Surgery 2018, 165, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Keszthelyi, D.; Troost, F.J.; Masclee, A.A.M. Understanding the role of tryptophan and serotonin metabolism in gastrointes-tinal function. Neurogastroenterol. Motil. 2009, 21, 1239–1249. [Google Scholar] [CrossRef]
- Sirek, A.; Sirek, O.V. Serotonin: A review. Can. Med. Assoc. J. 1970, 102, 846–849. [Google Scholar]
- Robertson, J.I.; Peart, W.S.; Andrews, T.M. The mechanism of facial flushes in the carcinoid syndrome. Quart. J. Med. 1962, 31, 103–123. [Google Scholar]
- Sjoerdsma, A.; Melmon, K.L. THE carcinoid spectrum. Gastroenterology 1964, 47, 104–107. [Google Scholar]
- Borch, K.; Ahrén, B.; Ahlman, H.; Falkmer, S.; Granérus, G.; Grimelius, L. Gastric carcinoids: Biologic behavior and prognosis after differentiated treatment in relation to type. Ann. Surg. 2005, 242, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Melmon, K.L.; Sjoerdsma, A.; Mason, D.T. Distinctive clinical and therapeutic aspects of the syndrome associated with bronchial carcinoid tumors. Am. J. Med. 1965, 39, 568–581. [Google Scholar] [CrossRef]
- Oates, J.; Sjoerdsma, K.M.A.; Gillespie, L.; Mason, D. Release of a kinin peptide in the carcinoid syndrome. Lancet 1964, 1, 514–517. [Google Scholar] [CrossRef]
- Borna, R.M.; Jahr, J.S.; Kmiecik, S.; Mancuso, K.F.; Kaye, A.D. Pharmacology of octreotide: Clinical implications for anesthe-siologists and associated risks. Anesthesiol. Clin. 2017, 35, 327–339. [Google Scholar] [CrossRef]
- Lamberts, S.W.; van der Lely, A.J.; de Herder, W.W.; Hofland, L.J. Octreotide. N. Engl. J. Med. 1996, 334, 246–254. [Google Scholar] [CrossRef]
- Kvols, L.K.; Martin, J.K.; Marsh, H.M.; Moertel, C.G. Rapid reversal of carcinoid crisis with somatostatin analogue. N. Engl. J. Med. 1985, 313, 1229. [Google Scholar] [CrossRef]
- Kvols, L.K.; Moertel, C.G.; O’Connell, M.J.; Schutt, A.J.; Rubin, J.; Hahn, R.G. Treatment of the malignant carcinoid syndrome evaluation of a long-acting somatostatin analogue. N. Engl. J. Med. 1986, 315, 663–666. [Google Scholar] [CrossRef]
- Warner, R.R.; Mani, S.; Profeta, J.; Grunstein, E. Octreotide treatment of carcinoid hypertensive crisis. Mt. Sinai J. Med. A J. Transl. Pers. Med. 1994, 61, 349–355. [Google Scholar]
- Veall, M.G.R.Q.; Peacock, M.J.E.; Bax, M.N.D.S.; Reilly, M.C.S. Review of the anaesthetic management of 21 patients under-going laparotomy for carcinoid syndrome. Br. J. Anaesth. 1994, 72, 335–341. [Google Scholar] [CrossRef]
- Wonn, S.M.; Pommier, R.F. Carcinoid crisis: History, dogmas, and data. In Neuroendocrine Tumors; Springer: Berlin, Germany, 2021; pp. 87–103. [Google Scholar] [CrossRef]
- Woltering, E.A.; Wright, A.E.; Stevens, M.A.; Wang, Y.-Z.; Boudreaux, J.P.; Mamikunian, G.; Riopelle, J.M.; Kaye, A.D. Development of effective prophylaxis against intraoperative carcinoid crisis. J. Clin. Anesth. 2016, 32, 189–193. [Google Scholar] [CrossRef]
- Kinney, M.A.; Nagorney, D.M.; Clark, D.F.; O’Brien, T.D.; Turner, J.D.; Marienau, M.E.; Schroeder, D.R.; Martin, D.P. Partial hepatic resections for metastatic neuroendocrine tumors: Perioperative outcomes. J. Clin. Anesth. 2018, 51, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Kaltsas, G.; Caplin, M.; Davies, P.; Ferone, D.; Garcia-Carbonero, R.; Grozinsky-Glasberg, S.; Hörsch, D.; Janson, E.T.; Kian-manesh, R.; Kos-Kudła, B.; et al. ENETS consensus guidelines for the standards of care in neuroendocrine tumors: Pre- and perioperative therapy in patients with neuroendocrine tumors. Neuroendocrinology 2017, 105, 245–254. [Google Scholar] [CrossRef] [PubMed]
- de Keizer, B.; Van Aken, M.; Feelders, R.A.; De Herder, W.W.; Kam, B.L.R.; Van Essen, M.; Krenning, E.; Kwekkeboom, D. Hormonal crises following receptor radionuclide therapy with the radiolabeled somatostatin analogue [177Lu-DOTA0,Tyr3]octreotate. Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Stenzel, J.; Noe, S.; Holzapfel, K.; Erlmeier, F.; Eyer, F. Fatal systemic vasoconstriction in a case of metastatic small-intestinal NET. Rep. Gastrointest. Med. 2017, 2017, 9810194. [Google Scholar] [CrossRef]
- Rico, G.T.; Li, M.; Pavlakis, N.; Cehic, G.; Price, T.J. Prevention and management of carcinoid crises in patients with high-risk neuroendocrine tumours undergoing peptide receptor radionuclide therapy (PRRT): Literature review and case series from two Australian tertiary medical institutions. Cancer Treat. Rev. 2018, 66, 1–6. [Google Scholar] [CrossRef]
- Mason, D.T.; Melmon, K.L. New understanding of the mechanism of the carcinoid flush. Ann. Intern. Med. 1966, 65, 1334–1339. [Google Scholar] [CrossRef]
- Limbach, K.E.; Condron, M.E.; Bingham, A.E.; Pommier, S.J.; Pommier, R.F. Β-Adrenergic agonist administration is not asso-ciated with secondary carcinoid crisis in patients with carcinoid tumor. Am. J. Surg. 2019, 217, 932–936. [Google Scholar] [CrossRef]
- Howe, J.R.; Cardona, K.; Fraker, D.L.; Kebebew, E.; Untch, B.R.; Wang, Y.-Z.; Law, C.H.; Liu, E.H.; Kim, M.K.; Menda, Y.; et al. The surgical management of small bowel neuroendocrine tumors: Consensus guidelines of the north american neuroendo-crine tumor society. Pancreas 2017, 46, 715–731. [Google Scholar] [CrossRef]
- Wonn, S.M.; Ratzlaff, A.N.; Pommier, S.J.; McCully, B.H.; Pommier, R.F. A prospective study of carcinoid crisis with no perioperative octreotide. Surgery 2021, 171, 88–93. [Google Scholar] [CrossRef]
| Authors and Date | Primary Tumor Location | Clinical Presentation | Triggering Factor | Treatment |
|---|---|---|---|---|
| Kahil et al., 1964 [2] | ileum | apprehension, chest pain, abdominal cramps, diarrhea, flushing, cyanotic extremities, hypotension | increased tryptophan intake in diet | metaraminol, levarterenol (ineffective), cyproheptadine |
| Harris AL et al., 1983 [13] | ileum | prolonged continuous flushing, confusion, hypotension, coma | ileotransverse colostomy and liver biopsy | anti-serotonin and antikinin agents (5 fluorouracil, trasylol, prednisone, cimetidine, cyproheptadine, methysergide, tryptophan, aminoplex 12) |
| Hughes et al., 1989 [14] | lung | hypertension, tachycardia | anesthesia induction | ketanserin, octreotide |
| Batchelor AM et al., 1992 [15] | lung | peripheral cyanosis, myocardial infarction, flushing | rigid bronchoscopy | adrenaline, hydrocortisone, octreotide, ketanserin |
| Parry R.G. et al., 1996 [16] | hepatic metastases | acute tubular necrosis oliguria, diarrhea, flushing | liver biopsy | glucocorticoids, hemodialysis, octreotide, cyproheptadine |
| Koopmans KP et al., 2005 [17] | ileum | hypertension, peripheral cyanosis, flushing, edema, vomiting | 18F-DOPA infusion during PET | antihistamine |
| Papadogias et al., 2007 [18] | lung | hypotension, diarrhea | radioembolization (111in-octreotide infusion via intra-arterial injection) | octreotideic, alpha-interferon, glucocorticoids, and H1–H2 histamine receptor blockers |
| Van Diepen et al., 2013 [19] | small bowel | hypotension, fever, flushing | valve replacement | octreotide, vasopressin, norepinephrine, hydrocortisone, anti-serotonin, antihistamine, cyproheptadine |
| Kromas ML et al., 2017 [20] | lung | hypotension, wheezing | bronchoscopy | octreotide bolus |
| Maddali MV et al., 2020 [21] | ileum | initial hypertension and tachycardia, followed by shock and respiratory failure | TACE | dobutamine and vasopressin, then milrinone and nitroprusside (ineffective), octreotideic |
| Dhanani et al., 2020 [22] | small bowel | hypotension, loss of consciousness, cardiac arrest | Peptide Receptor Radionuclide Therapy (PRRT) | cardiopulmonary resuscitation plus adrenaline (ineffective), octreotideic |
| Mahdi et al., 2021 [23] | transverse colon (NEC) | abdominal pain, hypotension | not mentioned | empiric antibiotic therapy, norepinephrine ic (ineffective), octreotideic |
| Effects | Role in CC/CS | |
|---|---|---|
| Amines | ||
| Serotonin | vasoconstriction/vasodilatation, | diarrhea, cramps |
| bronchoconstriction, | bronchospasm | |
| fibroblastic activation | carcinoid heart disease | |
| Histamine | vasoconstriction/vasodilatation | flushing, pruritus, edema |
| bronchoconstriction | bronchospasm | |
| tachycardia | ||
| 5-Hydroxytryptophan | vasodilatation | diarrhea, cramps |
| Norepinephrine | vasoconstriction, tachycardia, hyperglycemia, hyperlipidemia, tremor | anxiety |
| Dopamine | vasodilatation, GI motility block | |
| Polypeptides | ||
| Kallikrein | conversion of kininogens in kinins (bradykinin and kallidin) | flushing, bronchospasm |
| Bradykinin | vasodilatation, bronchoconstriction, edema | flushing, bronchospasm |
| Somatostatin | GH, TSH, prolactin, insulin, glucagon release inhibition | diabetes, cholelithiasis, steatorrhea, hypochloridria |
| Motilin | GI motility stimulation | diarrhea, cramps |
| Pancreatic Polypeptide | pancreatic secretion regulation (inhibits the secretion of fluids, bicarbonate, and digestive enzymes) | |
| Vasoactive Intestinal Peptide | vasodilatation, smooth muscle relaxation induction, secretion of water into pancreatic juice, and bile stimulation | profuse diarrhea, hypokalemia, achlorhydria |
| Neuropeptide K (tachykinin family) | bronchoconstriction, bradycardia | |
| Substance P (tachykinin family) | bronchoconstriction | |
| bradycardia | ||
| Neurokinin A (tachykinin family) | bronchoconstriction | |
| bradycardia | ||
| Neurokinin B (tachykinin family) | bronchoconstriction | |
| bradycardia | ||
| Corticotropin (ACTH) | cortisol release | Cushing Syndrome |
| Gastrin | hydrochloric acid release by the stomach | Zollinger Ellison Syndrome |
| Growth Hormone | cell metabolism stimulation | acromegaly |
| Peptide YY | anorectic effect | |
| Glucagon | glucose and fatty acid release | necrolytic migratory erythema, weight loss hyperglycemia |
| Beta-endorphin | pain relief | |
| Neurotensin | gastrin and motilin release inhibition, vasodilatation | |
| Chromogranin A | vasostatin precursor, pancreastatin, catestatin, and parastatin that inhibit hormone released by neuroendocrine cells | |
| Prostaglandins | vasoconstriction/vasodilatation |
| Variation | Type of Paper | Number of Patients | Number of CC | Octreotide Dose and Regimen |
|---|---|---|---|---|
| Kvols et al., 1986 [36] | Case report-retrospective study | 25 | 1 | a bolus of 50 μg of octreotide intraoperatively |
| Kinney et al. [9] | Retrospective study | 119 | 15 (none of the pts received onctreotide intraoperatively) |
|
| Massimino et al. [10] | Retrospective study | 97 | 23 | 87 pts received prophylactic octreotide (median dose 500 μg—range 100–1100 μg) + intraoperative bolus if necessary (median dose 350 μg—range 100–5500 μg) |
| Woltering et al. [41] | Retrospective study | 150 | 6 | Continuous high-dose octreotide infusion: 500 μg/h |
| Condron et al. [11] | Prospective study | 127 | 38 | Continuous high-dose octreotide infusion: 100 μg/h |
| Kinney et al. [42] | Retrospective study | 169 | 0 |
|
| Kwon et al. [12] | Retrospective study | 75 | 24 |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bardasi, C.; Benatti, S.; Luppi, G.; Garajovà, I.; Piacentini, F.; Dominici, M.; Gelsomino, F. Carcinoid Crisis: A Misunderstood and Unrecognized Oncological Emergency. Cancers 2022, 14, 662. https://doi.org/10.3390/cancers14030662
Bardasi C, Benatti S, Luppi G, Garajovà I, Piacentini F, Dominici M, Gelsomino F. Carcinoid Crisis: A Misunderstood and Unrecognized Oncological Emergency. Cancers. 2022; 14(3):662. https://doi.org/10.3390/cancers14030662
Chicago/Turabian StyleBardasi, Camilla, Stefania Benatti, Gabriele Luppi, Ingrid Garajovà, Federico Piacentini, Massimo Dominici, and Fabio Gelsomino. 2022. "Carcinoid Crisis: A Misunderstood and Unrecognized Oncological Emergency" Cancers 14, no. 3: 662. https://doi.org/10.3390/cancers14030662
APA StyleBardasi, C., Benatti, S., Luppi, G., Garajovà, I., Piacentini, F., Dominici, M., & Gelsomino, F. (2022). Carcinoid Crisis: A Misunderstood and Unrecognized Oncological Emergency. Cancers, 14(3), 662. https://doi.org/10.3390/cancers14030662







