Is There a Role for [18F]FDG PET-CT in Staging MALT Lymphoma?
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Imaging
2.3. Outcome Data
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
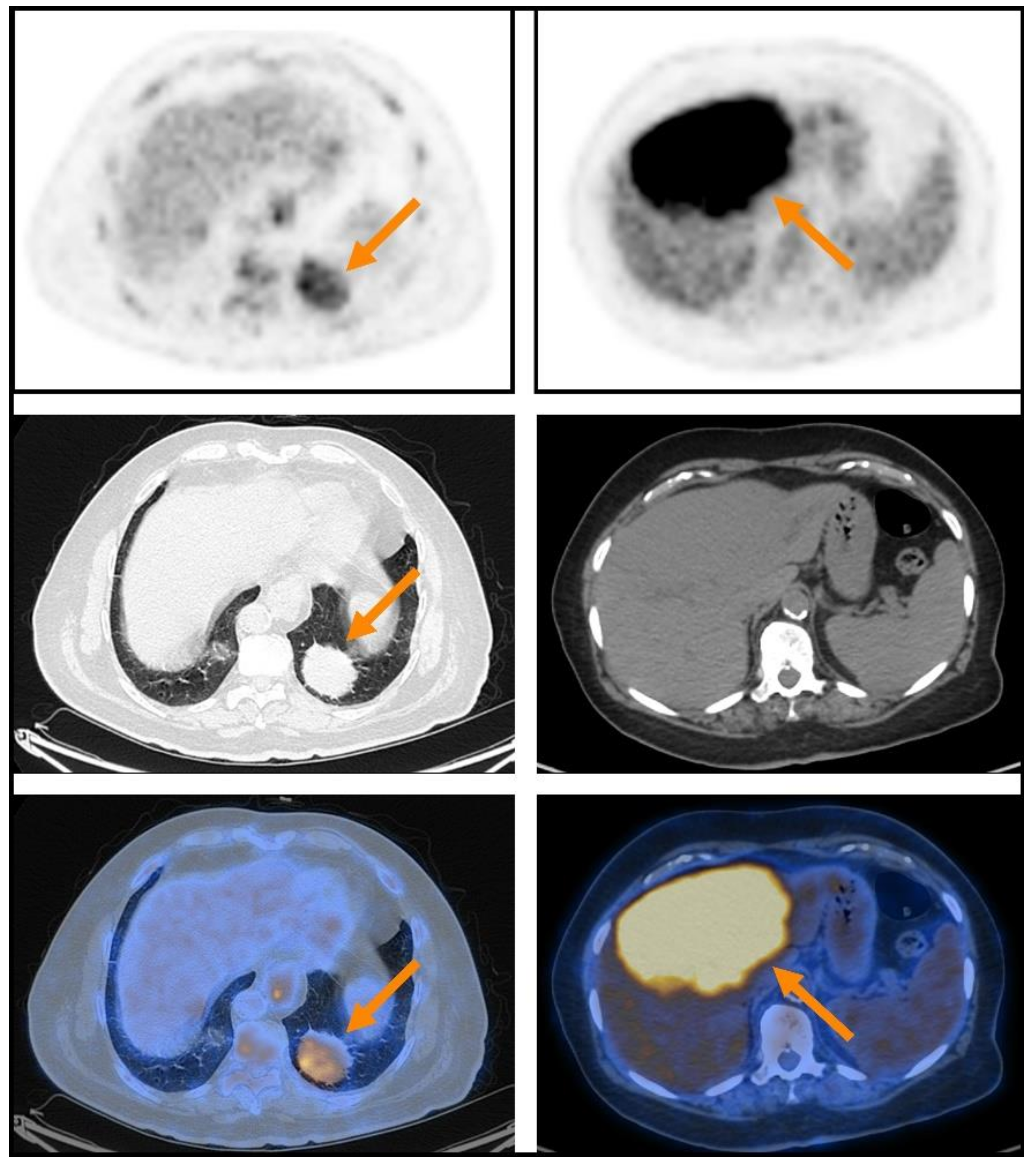
3.2. PET Characteristics of Extranodal Lesions
3.3. PET Characteristics of Nodal Lesions
3.4. PET Characteristics of Extranodal Lesions Are Associated with Staging Variables
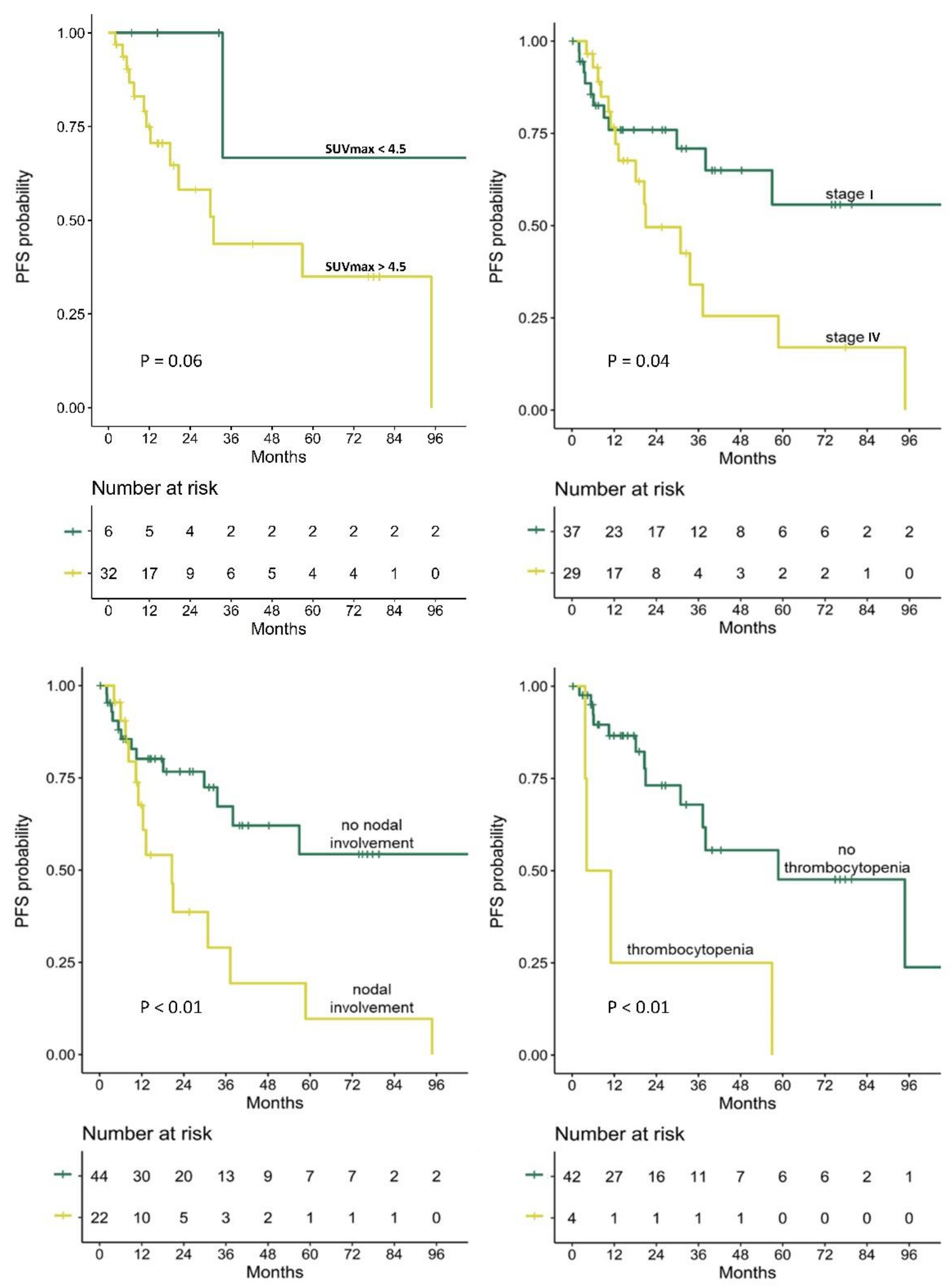
3.5. Prediction of PFS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Isaacson, P. Wright, Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer 1983, 52, 1410–1416. [Google Scholar] [CrossRef]
- Isaacson, P.G. Mucosa-associated lymphoid tissue lymphoma. Semin. Hematol. 1999, 36, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Dreyling, M.; Thieblemont, C.; Gallamini, A.; Arcaini, L.; Campo, E.; Hermine, O.; Kluin-Nelemans, J.C.; Ladetto, M.; Le Gouill, S.; Iannitto, E.; et al. ESMO Consensus conferences: Guidelines on malignant lymphoma. Part 2: Marginal zone lymphoma, mantle cell lymphoma, peripheral T-cell lymphoma. Ann. Oncol. 2013, 24, 857–877. [Google Scholar] [CrossRef] [PubMed]
- Zucca, E.; Stathis, A.; Bertoni, F. The management of nongastric MALT lymphomas. Oncology 2014, 28, 86. [Google Scholar] [PubMed]
- Cheson, B.D.; Fisher, R.I.; Barrington, S.F.; Cavalli, F.; Schwartz, L.H.; Zucca, E.; Lister, T.A. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano classification. J. Clin. Oncol. 2014, 32, 3059. [Google Scholar] [CrossRef] [PubMed]
- Albano, D.; Durmo, R.; Treglia, G.; Giubbini, R.; Bertagna, F. 18F-FDG PET/CT or PET Role in MALT Lymphoma: An Open Issue not Yet Solved—A Critical Review. Clin. Lymphoma Myeloma Leuk. 2020, 20, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Treglia, G.; Zucca, E.; Sadeghi, R.; Cavalli, F.; Giovanella, L.; Ceriani, L. Detection rate of fluorine-18-fluorodeoxyglucose positron emission tomography in patients with marginal zone lymphoma of MALT type: A meta-analysis. Hematol. Oncol. 2015, 33, 113–124. [Google Scholar] [CrossRef]
- Park, S.H.; Lee, J.J.; Kim, H.O.; Lee, D.Y.; Suh, C.; Jung, H.Y.; Choi, K.D.; Kim, D.H.; Huh, J.; Ryu, J.S. 18F-Fluorodeoxyglucose (FDG)-positron emission tomography/computed tomography in mucosa-associated lymphoid tissue lymphoma: Variation in 18F-FDG avidity according to site involvement. Leuk. Lymphoma 2015, 56, 3288–3294. [Google Scholar] [CrossRef] [PubMed]
- Albano, D.; Bertoli, M.; Ferro, P.; Fallanca, F.; Gianolli, L.; Picchio, M.; Giubbini, R.; Bertagna, F. 18F-FDG PET/CT in gastric MALT lymphoma: A bicentric experience. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 589–597. [Google Scholar] [CrossRef]
- Albano, D.; Bosio, G.; Giubbini, R.; Bertagna, F. 18F-FDG PET/CT and extragastric MALT lymphoma: Role of Ki-67 score and plasmacytic differentiation. Leuk. Lymphoma 2017, 58, 2328–2334. [Google Scholar] [CrossRef]
- Weiler-Sagie, M.; Bushelev, O.; Epelbaum, R.; Dann, E.J.; Haim, N.; Avivi, I.; Ben-Barak, A.; Ben-Arie, Y.; Bar-Shalom, R.; Israel, O. 18F-FDG avidity in lymphoma readdressed: A study of 766 patients. J. Nucl. Med. 2010, 51, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Zanni, M.; Moulin-Romsee, G.; Servois, V.; Validire, P.; Bénamor, M.; Plancher, C.; Rouic, L.L.; Dendale, R.; Vincent-Salomon, A.; Asselain, B.; et al. Value of 18FDG PET scan in staging of ocular adnexal lymphomas: A large single-center experience. Hematology 2012, 17, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Hirose, Y.; Kaida, H.; Ishibashi, M.; Uozumi, J.; Arikawa, S.; Kurata, S.; Hayabuchi, N.; Nakahara, K.; Ohshima, K. Comparison Between Endoscopic Macroscopic Classification and F-18 FDG PET Findings in Gastric Mucosa–Associated Lymphoid Tissue Lymphoma Patients. Clin. Nucl. Med. 2012, 37, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Li, H.; Wang, H.; Xu, B.; Fan, Y.; Tian, J. SUVmax/THKmax as a biomarker for distinguishing advanced gastric carcinoma from primary gastric lymphoma. PLoS ONE 2012, 7, e50914. [Google Scholar] [CrossRef][Green Version]
- Nasser, Q.J.; Pfeiffer, M.L.; Romaguera, J.; Fowler, N.; Debnam, J.M.; Samaniego, F.; El-Sawy, T.; McLaughlin, P.; Bakhoum, M.F.; Esmaeli, B. Clinical value of magnetic resonance imaging and other baseline testing for conjunctival mucosa-associated lymphoid tissue lymphoma. Leuk. Lymphoma 2014, 55, 1013–1017. [Google Scholar] [CrossRef]
- Hwang, J.W.; Jee, S.R.; Lee, S.H.; Kim, J.H.; Seol, S.Y.; Lee, S.M. Efficacy of positron emission tomography/computed tomography in gastric mucosa-associated lymphoid tissue lymphoma. Korean J. Gastroenterol. 2016, 67, 183–188. [Google Scholar] [CrossRef]
- Mayerhoefer, M.E.; Giraudo, C.; Senn, D.; Hartenbach, M.; Weber, M.; Rausch, I.; Kiesewetter, B.; Herold, C.J.; Hacker, M.; Pones, M.; et al. Does delayed-time-point imaging improve 18F-FDG-PET in patients with MALT lymphoma?: Observations in a series of 13 patients. Clin. Nucl. Med. 2016, 41, 101. [Google Scholar] [CrossRef][Green Version]
- Perry, C.; Herishanu, Y.; Metzer, U.; Bairey, O.; Ruchlemer, R.; Trejo, L.; Naparstek, E.; Sapir, E.E.; Polliack, A. Diagnostic accuracy of PET/CT in patients with extranodal marginal zone MALT lymphoma. Eur. J. Haematol. 2007, 79, 205–209. [Google Scholar] [CrossRef]
- Qi, S.; Huang, M.Y.; Yang, Y.; Schöder, H.; Teckie, S.; Noy, A.; Chau, K.; Yahalom, J. Uptake of [18F] fluorodeoxyglucose in initial positron-emission tomography predicts survival in MALT lymphoma. Blood Adv. 2018, 2, 649–655. [Google Scholar] [CrossRef]
- Vaxman, I.; Bernstine, H.; Kleinstern, G.; Hendin, N.; Shimony, S.; Domachevsky, L.; Gurion, R.; Groshar, D.; Raanani, P.; Gafter-Gvili, A. FDG PET/CT as a diagnostic and prognostic tool for the evaluation of marginal zone lymphoma. Hematol. Oncol. 2019, 37, 168–175. [Google Scholar] [CrossRef]
- Hwang, J.P.; Lim, I.; Byun, B.H.; Kim, B.I.; Choi, C.W.; Lim, S.M. Prognostic value of SUVmax measured by pretreatment 18F-FDG PET/CT in patients with primary gastric lymphoma. Nucl. Med. Commun. 2016, 37, 1267–1272. [Google Scholar] [CrossRef] [PubMed]
- Mayerhoefer, M.E.; Staudenherz, A.; Kiesewetter, B.; Weber, M.; Simonitsch-Klupp, I.; Gibbs, P.; Dolak, W.; Lukas, J.; Raderer, M. Pre-Therapeutic Total Lesion Glycolysis on [18F] FDG-PET Enables Prognostication of 2-Year Progression-Free Survival in MALT Lymphoma Patients Treated with CD20-Antibody-Based Immunotherapy. Mol. Imaging Biol. 2019, 21, 1192–1199. [Google Scholar] [CrossRef] [PubMed]
- Albano, D.; Bosio, G.; Camoni, L.; Farina, M.; Re, A.; Tucci, A.; Giubbini, R.; Bertagna, F. Prognostic role of baseline 18 F-FDG PET/CT parameters in MALT lymphoma. Hematol. Oncol. 2019, 37, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Cruz, E.; Marín-Oyaga, V.A.; de la Cruz Vicente, F.; Borrego-Dorado, I.; Ruiz Mercado, M.; Acevedo Banez, I.; Sole Rodriguez, M.; Fernandez Lopez, R.; Perez Vega, H.; Calderón-Cabrera, C.; et al. Role of 18F-FDG-PET/CT in the management of marginal zone B cell lymphoma. Hematol. Oncol. 2015, 33, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kim, S.; Ryu, J.S.; Lee, S.W.; Park, C.S.; Huh, J.; Suh, C. Complete metabolic response (CMR) in positron emission tomography–computed tomography (PET-CT) scans may have prognostic significance in patients with marginal zone lymphomas (MZL). Hematol. Oncol. 2018, 36, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Lister, T.A.; Crowther, D.; Sutcliffe, S.B.; Glatstein, E.; Canellos, G.P.; Young, R.C.; Rosenberg, S.A.; Coltman, C.A.; Tubiana, M. Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: Cotswolds meeting. J. Clin. Oncol. 1989, 7, 1630–1636. [Google Scholar] [CrossRef]
- Boellaard, R.; Delgado-Bolton, R.; Oyen, W.J.; Giammarile, F.; Tatsch, K.; Eschner, W.; Verzijlbergen, F.J.; Barrington, S.F.; Pike, L.C.; Weber, W.A.; et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: Version 2.0. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 328–354. [Google Scholar] [CrossRef] [PubMed]
- Lausen, B.; Lerche, R.; Schumacher, M. Maximally selected rank statistics for dose-response problems. Biom. J. 2002, 44, 131–147. [Google Scholar] [CrossRef]
- Albano, D.; Borghesi, A.; Bosio, G.; Bertoli, M.; Maroldi, R.; Giubbini, R.; Bertagna, F. Pulmonary mucosa-associated lymphoid tissue lymphoma: 18F-FDG PET/CT and CT findings in 28 patients. Br. J. Radiol. 2017, 90, 20170311. [Google Scholar] [CrossRef]
- Watanabe, Y.; Suefuji, H.; Hirose, Y.; Kaida, H.; Suzuki, G.; Uozumi, J.; Ogo, E.; Miura, M.; Takasu, K.; Miyazaki, K.; et al. 18F-FDG uptake in primary gastric malignant lymphoma correlates with glucose transporter 1 expression and histologic malignant potential. Int. J. Hematol. 2013, 97, 43–49. [Google Scholar] [CrossRef]
| Variable | Value | |
|---|---|---|
| Age (years) | 69.4 (57.7–74.6) | |
| Female | 39/66 (59.1%) | |
| Extranodal location | Stomach | 19/66 (28.8%) |
| Orbital | 15/66 (22.7%) | |
| Subcutaneous-tissue (including breast) | 10/66 (15.2%) | |
| Gastrointestinal tract (excluding stomach) | 7/66 (10.6%) | |
| Lung | 6/66 (9.1%) | |
| Head and Neck | 4/66 (6.1%) | |
| Liver | 2/66 (3%) | |
| Other locations | 3/66 (4.5%) | |
| Clinical staging data | Stage I | 37/66 (56%) |
| Stage IV | 29/66 (44%) | |
| B symptoms | 6/58 (10.3%) | |
| Bulky disease | 11/66 (16.7%) | |
| BM involvement | 8/45 (17.8%) | |
| Nodal involvement | 22/66 (33.3%) | |
| Pathology and laboratory data | High Ki-67 index | 2/53 (3.8%) |
| High serum LDH | 3/57 (5.3%) | |
| Anemia | 14/48 (29.2%) | |
| Thrombocytopenia | 4/46 (8.7%) | |
| PET data | Detection of extranodal disease | 38/66 (57.6%) |
| Detection of nodal disease | 13/66 (19.7%) | |
| Primary clinical strategy | Watch-and-wait strategy | 27/66 (40.9%) |
| Systemic therapy | 19/66 (28.8%) | |
| Radiotherapy | 18/66 (27.3%) | |
| Surgical resection | 2/66 (3%) |
| All Studies (n = 66) | Gastric (n = 19) | Orbital (n = 15) | Subcutaneous-Tissue (n = 10) | GI (exc. Stomach) (n = 7) | Lung (n = 6) | Head and Neck (n = 4) | Liver (n = 2) | ||
|---|---|---|---|---|---|---|---|---|---|
| Extranodal lesion: | DR | 38 (57.6%) | 5 (26.3%) | 9 (60%) | 10 (100%) | 2 (28.6%) | 6 (100%) | 2 (50%) | 2 (100%) |
| SUVmax | 7.166 (4.8–9.3) | 8.3 (4.8–9.9) | 7.6 (5.1–8.6) | 5.5 (3.2–8.8) | 8.2 | 6.4 (4.1–9.5) | 20.3 | 8.0 | |
| MTV | 5.5 (3.2–22.5) | 12.1 (4.4–221) | 4.5 (3.2–6.5) | 9.8 (4.8–38.2) | 222.1 | 9.8 (4.7–19.4) | 70.0 | 601.8 | |
| TLG | 25.6 (11.4–100.7) | 57.8 (13.8–1308) | 22.8 (12.6–34.6) | 35.7 (4.8–146) | 1342.4 | 37.1 (17–100.7) | 1580.7 | 3488.5 | |
| Nodallesion: | DR | 13 (19.7%) | 3 (15.8%) | 3 (20%) | 2 (20%) | 3 (42.9%) | 1 (16.7%) | 0 (0%) | 0 (0%) |
| SUVmax | 5 (4.4–10.5) | 7.7 | 4.7 | 6.2 | 4.4 | 5.0 | - | - | |
| MTV | 2.1 (1.7–9.3) | 10.8 | 1.7 | 1.1 | 2.4 | 2.1 | - | - | |
| TLG | 7.3 (5.3–81.6) | 124 | 8.3 | 4.1 | 6.4 | 7.3 | - | - |
| Caption | All Studies | Studies with Extranodal Lesion Located in Tissues with High/Heterogeneous Physiologic [18F]FDG-Uptake | Studies with Extranodal Lesion Located in Tissues with Low/Homogeneous Physiologic [18F]FDG-Uptake | p | |
|---|---|---|---|---|---|
| Extranodal lesion | DR: | 38/66 (57.6%) | 19/47 (40.4%) | 19/19 (100%) | <0.01 |
| SUVmax | 7.1 (4.8–9.3) | 7.9 (4.9–11.2) | 6.8 (4.3–9.1) | 0.25 | |
| MTV | 5.5 (3.2–22.5) | 5.4 (3.0–12.1) | 11.7 (3.6–28) | 0.40 | |
| TLG | 25.6 (11.4–100.7) | 22.8 (10.4–57.8) | 47.9 (11.7–112.2) | 0.71 | |
| Nodal lesion | DR: | 13/66 (19.7%) | 9/47 (19.9%) | 4/19 (21.1%) | 0.86 |
| Caption | Extranodal Lesion | Nodal Lesion | p |
|---|---|---|---|
| SUVmax | 10.5 (7.7–11.3) | 5.0 (4.4–9.4) | 0.04 |
| MTV | 7.7 (3.9–157.6) | 2.0 (1.5–11.6) | 0.02 |
| TLG | 49.5 (22.7–959.8) | 7.8 (4.7–75.2) | 0.02 |
| Variable | Extranodal Lesion Not Detected on PET (n = 28) | Extranodal Lesion with Low [18F]FDG-Avidity (n = 19) | Extranodal Lesion with High [18F]FDG-Avidity (n = 19) | p |
|---|---|---|---|---|
| Stage I | 21/28 (75%) | 9/19 (47.4%) | 7/19 (36.8%) | 0.02 (a) |
| Stage IV | 7/28 (25%) | 10/19 (52.6%) | 12/19 (63.2%) | 0.02 (a) |
| B symptoms | 3/24 (12.5%) | 0/17 (0%) | 3/17 (17.6%) | 0.10 |
| Bulky disease | 0/28 (0%) | 5/19 (26.3%) | 6/19 (31.6%) | <0.01 (a)(b) |
| BM involvement | 1/20 (5%) | 1/11 (9.1%) | 6/14 (42.9%) | 0.02 (a) |
| Nodal involvement | 7/28 (25%) | 6/19 (31.6%) | 9/19 (47.4%) | 0.28 |
| High Ki-67 index | 1/21 (4.8%) | 0/15 (0%) | 1/17 (5.9%) | 0.50 |
| High serum LDH | 0/25 (0%) | 3/16 (18.8%) | 0/16 (0%) | 0.02 (b) |
| Anemia | 6/18 (33.3%) | 4/15 (26.7%) | 4/15 (26.7%) | 0.88 |
| Thrombocytopenia | 1/18 (5.6%) | 1/13 (7.7%) | 2/15 (13.3%) | 0.73 |
| [18F]FDG-avid nodal disease | 3/28 (10.7%) | 2/19 (10.5%) | 8/19 (42.1%) | 0.02 (c) |
| Variable | Variable | p | HR (95% CI) |
|---|---|---|---|
| Clinical characteristics | Age | 0.37 | 1.01 (0.98–1.05) |
| Female | 0.48 | 1.32 (0.61–2.83) | |
| Stage I (vs stage IV) | 0.05 * | 0.45 (0.21–0.98) | |
| B symptoms | 0.10 | 2.52 (0.84–7.62) | |
| Bulky disease | 0.69 | 0.78 (0.23–2.62) | |
| BM involvement | 0.44 | 1.51 (0.54–4.20) | |
| Nodal involvement | <0.01 * | 2.90 (1.34–6.24) | |
| High Ki-67 index | 0.14 | 5.09 (0.59–43.85) | |
| High serum LDH | 0.50 | 0.05 (0.01–399.32) | |
| Anemia | 0.53 | 1.35 (0.52–3.50) | |
| Thrombocytopenia | <0.01 *^ | 4.85 (1.53–15.40) | |
| PET characteristics | Extranodal lesion detected (vs not detected) on PET | 0.77 | 0.89 (0.41–1.93) |
| SUVmax of detected extranodal lesions | 0.02 *^ | 1.10 (1.01–1.19) | |
| MTV of detected extranodal lesions | 0.26 | 1.00 (1.00–1.00) | |
| TLG of detected extranodal lesions | 0.11 | 1.00 (1.00–1.00) | |
| Nodal disease detected (vs not detected) on PET | 0.21 | 1.82 (0.72–4.63) | |
| SUVmax of detected nodal disease | 0.67 | 1.03 (0.91–1.16) | |
| MTV of detected nodal disease | 0.56 | 1.02 (0.95–1.11) | |
| TLG of detected nodal disease | 0.71 | 1.00 (0.99–1.02) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cohen, D.; Perry, C.; Hazut-Krauthammer, S.; Kesler, M.; Herishanu, Y.; Luttwak, E.; Even-Sapir, E.; Avivi, I. Is There a Role for [18F]FDG PET-CT in Staging MALT Lymphoma? Cancers 2022, 14, 750. https://doi.org/10.3390/cancers14030750
Cohen D, Perry C, Hazut-Krauthammer S, Kesler M, Herishanu Y, Luttwak E, Even-Sapir E, Avivi I. Is There a Role for [18F]FDG PET-CT in Staging MALT Lymphoma? Cancers. 2022; 14(3):750. https://doi.org/10.3390/cancers14030750
Chicago/Turabian StyleCohen, Dan, Chava Perry, Shir Hazut-Krauthammer, Mikhail Kesler, Yair Herishanu, Efrat Luttwak, Einat Even-Sapir, and Irit Avivi. 2022. "Is There a Role for [18F]FDG PET-CT in Staging MALT Lymphoma?" Cancers 14, no. 3: 750. https://doi.org/10.3390/cancers14030750
APA StyleCohen, D., Perry, C., Hazut-Krauthammer, S., Kesler, M., Herishanu, Y., Luttwak, E., Even-Sapir, E., & Avivi, I. (2022). Is There a Role for [18F]FDG PET-CT in Staging MALT Lymphoma? Cancers, 14(3), 750. https://doi.org/10.3390/cancers14030750







