PARP Inhibitors: A Major Therapeutic Option in Endocrine-Receptor Positive Breast Cancers
Abstract
:Simple Summary
Abstract
1. Introduction
2. Results
2.1. Frequency of Homologous Recombination-Related Gene Mutations
2.1.1. Frequency of Germline BRCA Mutations
2.1.2. Frequency of BRCA Somatic Alterations
2.1.3. Mutations in Other Homologous Recombination-Related Genes
| Study Design | BRCA1 | BRCA2 | RAD51 | RAD50 | MRE11 | NBN | PALB2 | ATM | ATR | BAP1 | BARD1 | BRIP1 | CHEK2 | FANC | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FAMILIAL BREAST CANCER POPULATION | |||||||||||||||
| Buys et al., Cancer 2017 [59] | 35,409 women with breast cancers eligible for genetic counselling | 24% | 24% | RAD51C 1.6% RAD51D 0.6% | NR | NR | 1.7% | 9.3% | 9.7% | NR | NR | 2% | 3.2% | 11.7% | NR |
| Other subtypes than triple negative breast cancer N = 30,612 (87%) | 17.3% | 26.1% | RAD51C 1.3% RAD51D 0.5% | NR | NR | 2% | 9.5% | 11.6% | NR | NR | 1.7% | 3% | 14.3% | NR | |
| Slavin et al., NPJ Breast Cancer 2017 [18] | 2134 BRCA negative familial breast cancers | NR | NR | RAD51D 0.19% RAD51C 0.14% | 0.2% | 0.05% | 0.05% | 0.9% | 1.5% | NR | 0% | 0.3% | 0.05% | 1.6% | FANCC 0.05% FANCM 0.3% |
| ER+/HER2- breast cancers N = 1203 (50%) | NR | NR | NR | NR | NR | 1.8% | 0.8% | NR | NR | NR | NR | NR | NR | NR | |
| Tung et al., Cancers 2015 [60] | 1781 women with breast cancers eligible for genetic counselling | 4.3% | 4.8% | NR | NR | NR | NR | 0.6% | 0.6% | NR | NR | 0.03% | 0.04% | 1.6% | NR |
| 377 women with breast cancers eligible for genetic counselling and without BRCA mutation | NR | NR | NR | NR | NR | NR | 0.02% | 0.02% | NR | NR | 0.02% | 0% | 1.3% | NR | |
| UNSELECTED PRIMARY BREAST CANCERS | |||||||||||||||
| Kurian et al. J Clin Oncol 2019 [38] | 18,601 unselected women with breast cancer | 3.2% | 3.1% | RAD51C 0.18% RAD51D 0.12% | NR | NR | NR | 1% | 0.7% | NR | NR | 0.21% | 0.22% | 1.6% | NR |
| ER+/HER2- breast cancers N = 9740 (52%) | 2% | 3.2% | RAD51C 0.11% RAD51D 0.19% | NR | NR | NR | 1% | 0.9% | NR | NR | 0.21% | 0.28% | 1.7% | NR | |
| Tung et al., J Clin Oncol 2016 [39] | 488 primary breast cancers | 3.6% | 2.4% | RAD51C 0.2% RAD51D 0.2% | NR | NR | 0.2% | 0.2% | 0.8% | NR | NR | NR | 0.8% | 2% | NR |
| ER+/HER2- breast cancers N = 301 (62%) | 1.7% | 3.3% | RAD51C 0.3% RAD51D 0% | NR | NR | 0% | 0.3% | 1% | NR | NR | NR | 0.3% | 1.3% | NR | |
| Hu et al., J Natl Cancer Inst 2020 [20] | 54,555 early breast cancers | 2.2% | 2.2% | RAD51C 0,2% RAD51D 0,1% | NR | NR | 0.3% | 1% | 1.1% | NR | NR | 0.3% | 0.3% | 1.7% | NR |
| ER+/HER2- breast cancers N = 26,620 (58%) | 0.9% | 2.1% | RAD51C 0.2% RAD51D 0.1% | NR | NR | 0.3% | 0.9% | 1.1% | NR | NR | 0.2% | 0.3% | 1.9% | NR | |
| Chen et al., Aging 2020 [47] | 524 early breast cancers | 3.4% | 2.1% | RAD51C 0.6% | NR | NR | NR | 0.7% | 0.6% | NR | NR | NR | 0.6% | 0.4% | FANCA 0.4% |
| ER+/HER2- breast cancers N = 363 (69%) | 1.1% | 4.1% | RAD51C 0.3% | NR | NR | NR | 0.6% | 0.6% | NR | NR | NR | 0.6% | 0.6% | FANCA 0.6% | |
| Wu et al., Cancer 2020 [19] | 605 non-triple negative breast cancer samples from TCGA database | Somatic 1.4% | Somatic 1.4% | RAD51B 0.5% RAD51C 0.3% RAD51D 0.3% | 0.7% | 1% | 0.5% | 0.7% | 2.4% | 1.4% | 0.5% | 1% | 0.7% | FANCA 0.8% FANCC 0.8% FANCD2 1.2% FANCE 0.3% | |
| Pereira et al., Nat commun 2016 [40] | 2433 early breast cancers | 1.7% | 1.8% | NR | NR | NR | NR | NR | NR | 3.8% | 1.6% | NR | 1% | 0.7% | FANCA 2.5 FANCD2 1.8 |
| ER+/HER2- breast cancers N = 1563 (64%) | 1% | 1% | NR | NR | NR | NR | NR | NR | 4% | 1% | NR | 1% | 1% | FANCA 2% FANCD2 2% | |
| UNSELECTED METEATATIC BREAST CANCER or INCLUDING METASTATIC BREAST CANCERS | |||||||||||||||
| Paul et al., J Clin invest 2020 [49] | 66 metastatic breast cancers | 4.5% | 4.5% | NR | NR | NR | NR | 3% | 1.5% | NR | NR | NR | NR | 1.5% | NR |
| ER+/HER2-; breast cancers N = 46 (70%) | NR | NR | RAD51C 0.2% RAD51D 0.1% | NR | NR | 0.3% | 0.9% | 1.1% | NR | NR | 0.2% | 0.3% | 1.9% | NR | |
| Rinaldi et al., Plos one 2020 [21] | 11,616 breast cancers Somatic pathogenic variant from primaries (39%) lymph nodes (12%) and metastases (43%) | 5.6% | 7.2% | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| ER+/HER2- breast cancers N = 6388 (55%) | 3.4% | 8.5% | NR | NR | NR | NR | 2.4% | 5.4% | 5% | NR | NR | NR | 2.2% | NR | |
| Angus et al. Nat genet 2019 [12] | 442 metastatic breast cancer and metastatic biopsies Results in ER+/HER2- breast cancers N = 279 (63%) | 2.2% | 6.1% | NR | NR | NR | NR | 1.1% | 6.1% | 5.4% | NR | NR | NR | NR | NR |
2.2. PARP Inhibitors in ER+ Breast Cancer
2.2.1. Efficacy in Patients with ER+ BRCA1/2 Mutated Metastatic Breast Cancer
2.2.2. Efficacy in HRD Tumors beyond Germline BRCA1/2 Mutations
2.2.3. Efficacy in Patients with BRCA Mutated ER+ Early Breast Cancer in Neoadjuvant Setting
2.2.4. Efficacy in Patients with BRCA Mutated ER+ Early Breast Cancer in Adjuvant Setting
2.3. Patient Selection for PARP Inhibitors
2.3.1. Identification of Gene Alterations
2.3.2. Genomic Scars and Genomic Instability
- Available commercial and industrial genetic tests to detect genomic instability
- Academic genomic tests to detect genomic instability and mutational signatures
- Detection of genomic instability through copy number alterations
2.3.3. Functional Homologous Recombination Deficiency and RAD51 Foci Assay
| Biomarkers | Resources | Clinical Assessment | Advantage | Limitation |
|---|---|---|---|---|
| BRCA1/2 pathogenic variant | Targeted sequencing for single nucleotide variant and small indels PCR multiplex for large deletion and duplication | BRACanalyse Myriad Genetic test Phase III clinical trials: OlympiAD [62], Embraca [64], and Brocade3 [68] in metastatic HER2- breast cancer | Easy to perform Validated in clinical trials | BRCA testing only No detection of functional silencing methylation of BRCA gene promoters and of balanced rearrangement (i.e., inversion) No information about variant of unknown significance Patented commercial test cost outsourced |
| Pathogenic variant of genes of homologous recombination beyond BRCA | Targeted sequencing | Phase II clinical trial for germline PALB2, CHEK2, and FANCA mutation and somatic BRCA1/2, ATR, and PTEN mutations [57,58] in metastatic breast cancer | Easy to perform Validated in clinical trials | Dependence on the genes assessed in the panel, and on knowledge of their implication No detection of functional silencing methylation of gene promoters (i.e., RAD51C) No information about variant of unknown significance Cost |
| Mutational signatures | Whole exome sequencing | Single base substitution signature 3 Rearrangement signature 3 and Rearrangement signature 5 Preclinical studies [92] | Identification of genomic scars independently of what genes are mutated Identification of genes potentially implicated in HRD and reclassification of variant of unknown significance | Low specificity: different mutational signature and rearrangement signature in function of the homologous recombination related mutated gene Overlook HRD as a dynamic process, persistence of genomic signature despite restoration of HRD missing potential PARP inhibitor resistance Whole exome sequencing could be difficult to perform in daily clinical practice |
| HRD score (TAI, LOH, LST) | Whole exome sequencing | MyriadMychoice genetic test Phase II clinical trials [69,105] | Validated in clinical trials Identification of genomics scars independently on involved genes Identification of genes potentially implicated in HRD and reclassification of variant of unknown significance | No integration of time, or impact of previous exposure with chemotherapy lines on homologous recombination activity Patented commercial test Cost Limited access to the assay/outsourced |
| HRDetect (micro-homology mediated indels, HRD index, single base substitution signature 3, rearrangement signature 3 and 5) | Whole genome sequencing | Ad hoc analysis from phase II clinical trial triple negative breast cancer [91] | Identification of genomics scars independently on involved genes Identification of genes potentially implicated in HRD and reclassification of variant of unknown significance | No integration of time or impact of previous exposure with chemotherapy lines on homologous recombination activity No validation in prospective clinical trial Cost Limited access to the assay (research) |
| Classifier of Homologous Recombination Deficiency (CHORD) (single nucleotide variant, indels and structural variant) | Whole genome sequencing | In vitro studies only | Identification of genomics scars independently on involved genes Identification of genes potentially implicated in HRD and reclassification of variant of unknown significance Differentiation of “BRCA1-type HDR” and “BRCA2-type HRD” | No integration of time, or impact of previous exposure with chemotherapy lines on homologous recombination activity No validation in prospective clinical trial Cost Limited access to the assay |
| RAD51 foci immunohistochemistry | Fluorescent or chromogenic immunohistochemistry on FFPE samples | Retrospective study and preclinical study Ad hoc analysis from phase II clinical trial triple negative breast cancer [93] | Reduced cost and high feasibility during pathology assessment Real time assessment of homologous recombination activity | No validation in prospective clinical trial Limited to the homologous recombination pathways above RAD51 |
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Farmer, H.; McCabe, N.; Lord, C.J.; Tutt, A.N.J.; Johnson, D.A.; Richardson, T.B.; Santarosa, M.; Dillon, K.J.; Hickson, I.; Knights, C.; et al. Targeting the DNA Repair Defect in BRCA Mutant Cells as a Therapeutic Strategy. Nature 2005, 434, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Jalal, S.; Earley, J.N.; Turchi, J.J. DNA Repair: From Genome Maintenance to Biomarker and Therapeutic Target. Clin. Cancer Res. 2011, 17, 6973–6984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, J.S.; O’Carrigan, B.; Jackson, S.P.; Yap, T.A. Targeting DNA Repair in Cancer: Beyond PARP Inhibitors. Cancer Discov. 2017, 7, 20–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, R.M.M.; McIntosh, S.A.; Savage, K.I. Homologous Recombination Deficiency in Breast Cancer: Implications for Risk, Cancer Development, and Therapy. Genes Chromosom. Cancer 2020, 60, 358–372. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.L.; Oza, A.M.; Lorusso, D.; Aghajanian, C.; Oaknin, A.; Dean, A.; Colombo, N.; Weberpals, J.I.; Clamp, A.; Scambia, G.; et al. Rucaparib Maintenance Treatment for Recurrent Ovarian Carcinoma after Response to Platinum Therapy (ARIEL3): A Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet 2017, 390, 1949–1961. [Google Scholar] [CrossRef] [Green Version]
- Pujade-Lauraine, E.; Ledermann, J.A.; Selle, F.; Gebski, V.; Penson, R.T.; Oza, A.M.; Korach, J.; Huzarski, T.; Poveda, A.; Pignata, S.; et al. Olaparib Tablets as Maintenance Therapy in Patients with Platinum-Sensitive, Relapsed Ovarian Cancer and a BRCA1/2 Mutation (SOLO2/ENGOT-Ov21): A Double-Blind, Randomised, Placebo-Controlled, Phase 3 Trial. Lancet Oncol. 2017, 18, 1274–1284. [Google Scholar] [CrossRef] [Green Version]
- Moore, K.; Colombo, N.; Scambia, G.; Kim, B.-G.; Oaknin, A.; Friedlander, M.; Lisyanskaya, A.; Floquet, A.; Leary, A.; Sonke, G.S.; et al. Maintenance Olaparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2018, 379, 2495–2505. [Google Scholar] [CrossRef]
- Mirza, M.R.; Monk, B.J.; Herrstedt, J.; Oza, A.M.; Mahner, S.; Redondo, A.; Fabbro, M.; Ledermann, J.A.; Lorusso, D.; Vergote, I.; et al. Niraparib Maintenance Therapy in Platinum-Sensitive, Recurrent Ovarian Cancer. N. Engl. J. Med. 2016, 375, 2154–2164. [Google Scholar] [CrossRef]
- González-Martín, A.; Pothuri, B.; Vergote, I.; DePont Christensen, R.; Graybill, W.; Mirza, M.R.; McCormick, C.; Lorusso, D.; Hoskins, P.; Freyer, G.; et al. Niraparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2391–2402. [Google Scholar] [CrossRef] [Green Version]
- Ray-Coquard, I.; Pautier, P.; Pignata, S.; Pérol, D.; González-Martín, A.; Berger, R.; Fujiwara, K.; Vergote, I.; Colombo, N.; Mäenpää, J.; et al. Olaparib plus Bevacizumab as First-Line Maintenance in Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2416–2428. [Google Scholar] [CrossRef]
- Lord, C.J.; Ashworth, A. BRCAness Revisited. Nat. Rev. Cancer 2016, 16, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Angus, L.; Smid, M.; Wilting, S.M.; van Riet, J.; Van Hoeck, A.; Nguyen, L.; Nik-Zainal, S.; Steenbruggen, T.G.; Tjan-Heijnen, V.C.G.; Labots, M.; et al. The Genomic Landscape of Metastatic Breast Cancer Highlights Changes in Mutation and Signature Frequencies. Nat. Genet. 2019, 51, 1450–1458. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.; Martens, J.W.M.; Van Hoeck, A.; Cuppen, E. Pan-Cancer Landscape of Homologous Recombination Deficiency. Nat. Commun. 2020, 11, 5584. [Google Scholar] [CrossRef]
- Malone, K.E.; Daling, J.R.; Doody, D.R.; Hsu, L.; Bernstein, L.; Coates, R.J.; Marchbanks, P.A.; Simon, M.S.; McDonald, J.A.; Norman, S.A.; et al. Prevalence and Predictors of BRCA1 and BRCA2 Mutations in a Population-Based Study of Breast Cancer in White and Black American Women Ages 35 to 64 Years. Cancer Res. 2006, 66, 8297–8308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beitsch, P.D.; Whitworth, P.W.; Hughes, K.; Patel, R.; Rosen, B.; Compagnoni, G.; Baron, P.; Simmons, R.; Smith, L.A.; Grady, I.; et al. Underdiagnosis of Hereditary Breast Cancer: Are Genetic Testing Guidelines a Tool or an Obstacle? J. Clin. Oncol. 2019, 37, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wen, W.X.; Eklund, M.; Kvist, A.; Eriksson, M.; Christensen, H.N.; Torstensson, A.; Bajalica-Lagercrantz, S.; Dunning, A.M.; Decker, B.; et al. Prevalence of BRCA1 and BRCA2 Pathogenic Variants in a Large, Unselected Breast Cancer Cohort. Int. J. Cancer 2019, 144, 1195–1204. [Google Scholar] [CrossRef] [Green Version]
- Behl, S.; Hamel, N.; de Ladurantaye, M.; Lepage, S.; Lapointe, R.; Mes-Masson, A.-M.; Foulkes, W.D. Founder BRCA1/BRCA2/PALB2 Pathogenic Variants in French-Canadian Breast Cancer Cases and Controls. Sci. Rep. 2020, 10, 6491. [Google Scholar] [CrossRef] [Green Version]
- Slavin, T.P.; Maxwell, K.N.; Lilyquist, J.; Vijai, J.; Neuhausen, S.L.; Hart, S.N.; Ravichandran, V.; Thomas, T.; Maria, A.; Villano, D.; et al. The Contribution of Pathogenic Variants in Breast Cancer Susceptibility Genes to Familial Breast Cancer Risk. NPJ Breast Cancer 2017, 3, 22. [Google Scholar] [CrossRef]
- Wu, J.; Mamidi, T.K.K.; Zhang, L.; Hicks, C. Unraveling the Genomic-Epigenomic Interaction Landscape in Triple Negative and Non-Triple Negative Breast Cancer. Cancers 2020, 12, 1559. [Google Scholar] [CrossRef]
- Hu, C.; Polley, E.C.; Yadav, S.; Lilyquist, J.; Shimelis, H.; Na, J.; Hart, S.N.; Goldgar, D.E.; Shah, S.; Pesaran, T.; et al. The Contribution of Germline Predisposition Gene Mutations to Clinical Subtypes of Invasive Breast Cancer from a Clinical Genetic Testing Cohort. JNCI J. Natl. Cancer Inst. 2020, 112, 1231–1241. [Google Scholar] [CrossRef]
- Rinaldi, J.; Sokol, E.S.; Hartmaier, R.J.; Trabucco, S.E.; Frampton, G.M.; Goldberg, M.E.; Albacker, L.A.; Daemen, A.; Manning, G. The Genomic Landscape of Metastatic Breast Cancer: Insights from 11,000 Tumors. PLoS ONE 2020, 15, e0231999. [Google Scholar] [CrossRef] [PubMed]
- Winter, C.; Nilsson, M.P.; Olsson, E.; George, A.M.; Chen, Y.; Kvist, A.; Törngren, T.; Vallon-Christersson, J.; Hegardt, C.; Häkkinen, J.; et al. Targeted Sequencing of BRCA1 and BRCA2 across a Large Unselected Breast Cancer Cohort Suggests That One-Third of Mutations Are Somatic. Ann. Oncol. 2016, 27, 1532–1538. [Google Scholar] [CrossRef] [PubMed]
- Vagia, E.; Mahalingam, D.; Cristofanilli, M. The Landscape of Targeted Therapies in TNBC. Cancers 2020, 12, 916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cardoso, F.; Paluch-Shimon, S.; Senkus, E.; Curigliano, G.; Aapro, M.S.; André, F.; Barrios, C.H.; Bergh, J.; Bhattacharyya, G.S.; Biganzoli, L.; et al. 5th ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 5). Ann. Oncol. 2020, 31, 1623–1649. [Google Scholar] [CrossRef]
- Hortobagyi, G.N.; Stemmer, S.M.; Burris, H.A.; Yap, Y.S.; Sonke, G.S.; Paluch-Shimon, S.; Campone, M.; Petrakova, K.; Blackwell, K.L.; Winer, E.P.; et al. Updated Results from MONALEESA-2, a Phase III Trial of First-Line Ribociclib plus Letrozole versus Placebo plus Letrozole in Hormone Receptor-Positive, HER2-Negative Advanced Breast Cancer. Ann. Oncol. 2018, 29, 1541–1547. [Google Scholar] [CrossRef]
- Sledge, G.W.; Toi, M.; Neven, P.; Sohn, J.; Inoue, K.; Pivot, X.; Burdaeva, O.; Okera, M.; Masuda, N.; Kaufman, P.A.; et al. MONARCH 2: Abemaciclib in Combination with Fulvestrant in Women With HR+/HER2- Advanced Breast Cancer Who Had Progressed While Receiving Endocrine Therapy. J. Clin. Oncol. 2017, 35, 2875–2884. [Google Scholar] [CrossRef]
- Goetz, M.P.; Toi, M.; Campone, M.; Sohn, J.; Paluch-Shimon, S.; Huober, J.; Park, I.H.; Trédan, O.; Chen, S.-C.; Manso, L.; et al. MONARCH 3: Abemaciclib As Initial Therapy for Advanced Breast Cancer. J. Clin. Oncol. 2017, 35, 3638–3646. [Google Scholar] [CrossRef]
- Iwata, H.; Im, S.-A.; Masuda, N.; Im, Y.-H.; Inoue, K.; Rai, Y.; Nakamura, R.; Kim, J.H.; Hoffman, J.T.; Zhang, K.; et al. PALOMA-3: Phase III Trial of Fulvestrant with or without Palbociclib in Premenopausal and Postmenopausal Women with Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Metastatic Breast Cancer That Progressed on Prior Endocrine Therapy-Safety and Efficacy in Asian Patients. J. Glob. Oncol. 2017, 3, 289–303. [Google Scholar] [CrossRef]
- McLaurin, K.; Dalvi, T.; Collins, J.M.; Nordstrom, B.L.; McCutcheon, S.; Bennett, J.C.; Murphy, B.R.; Singhal, P.K.; Briceno, J.M. A Real-World Evidence Study of CDK4/6 Inhibitor Treatment Patterns and Outcomes in Metastatic Breast Cancer by GBRCA Mutation Status. J. Clin. Oncol. 2019, 37, 1563. [Google Scholar] [CrossRef]
- Frenel, J.-S.; Dalenc, F.; Pistilli, B.; Rouge, T.d.L.M.; Levy, C.; Mouret-Reynier, M.-A.; Hardy-Bessard, A.-C.; Bonichon-Lamichhane, N.; Greilsamer, C.; Delecroix, V.; et al. 304P ESR1 Mutations and Outcomes in BRCA1/2 or PALB2 Germline Mutation Carriers Receiving First Line Aromatase Inhibitor + Palbociclib (AI+P) for Metastatic Breast Cancer (MBC) in the PADA-1 Trial. Ann. Oncol. 2020, 31, S364. [Google Scholar] [CrossRef]
- Krammer, J.; Pinker-Domenig, K.; Robson, M.E.; Gönen, M.; Bernard-Davila, B.; Morris, E.A.; Mangino, D.A.; Jochelson, M.S. Breast Cancer Detection and Tumor Characteristics in BRCA1 and BRCA2 Mutation Carriers. Breast Cancer Res. Treat. 2017, 163, 565–571. [Google Scholar] [CrossRef] [PubMed]
- De Talhouet, S.; Peron, J.; Vuilleumier, A.; Friedlaender, A.; Viassolo, V.; Ayme, A.; Bodmer, A.; Treilleux, I.; Lang, N.; Tille, J.-C.; et al. Clinical Outcome of Breast Cancer in Carriers of BRCA1 and BRCA2 Mutations According to Molecular Subtypes. Sci. Rep. 2020, 10, 7073. [Google Scholar] [CrossRef] [PubMed]
- Mavaddat, N.; Barrowdale, D.; Andrulis, I.L.; Domchek, S.M.; Eccles, D.; Nevanlinna, H.; Ramus, S.J.; Spurdle, A.; Robson, M.; Sherman, M.; et al. Pathology of Breast and Ovarian Cancers among BRCA1 and BRCA2 Mutation Carriers: Results from the Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA). Cancer Epidemiol. Biomark. Prev. 2012, 21, 134–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McClain, M.R.; Nathanson, K.L.; Palomaki, G.E.; Haddow, J.E. An Evaluation of BRCA1 and BRCA2 Founder Mutations Penetrance Estimates for Breast Cancer among Ashkenazi Jewish Women. Genet. Med. 2005, 7, 34–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prevalence and Penetrance of BRCA1 and BRCA2 Mutations in a Population-Based Series of Breast Cancer Cases. Br. J. Cancer 2000, 83, 1301–1308. [CrossRef]
- Manickam, K.; Buchanan, A.H.; Schwartz, M.L.B.; Hallquist, M.L.G.; Williams, J.L.; Rahm, A.K.; Rocha, H.; Savatt, J.M.; Evans, A.E.; Butry, L.M.; et al. Exome Sequencing–Based Screening for BRCA1/2 Expected Pathogenic Variants Among Adult Biobank Participants. JAMA Netw. Open 2018, 1, e182140. [Google Scholar] [CrossRef] [Green Version]
- Abul-Husn, N.S.; Soper, E.R.; Odgis, J.A.; Cullina, S.; Bobo, D.; Moscati, A.; Rodriguez, J.E.; Loos, R.J.F.; Cho, J.H.; Belbin, G.M.; et al. Exome Sequencing Reveals a High Prevalence of BRCA1 and BRCA2 Founder Variants in a Diverse Population-Based Biobank. Genome Med. 2019, 12, 2. [Google Scholar] [CrossRef]
- Kurian, A.W.; Ward, K.C.; Howlader, N.; Deapen, D.; Hamilton, A.S.; Mariotto, A.; Miller, D.; Penberthy, L.S.; Katz, S.J. Genetic Testing and Results in a Population-Based Cohort of Breast Cancer Patients and Ovarian Cancer Patients. J. Clin. Oncol. 2019, 37, 1305–1315. [Google Scholar] [CrossRef] [Green Version]
- Nik-Zainal, S.; Davies, H.; Staaf, J.; Ramakrishna, M.; Glodzik, D.; Zou, X.; Martincorena, I.; Alexandrov, L.B.; Martin, S.; Wedge, D.C.; et al. Landscape of Somatic Mutations in 560 Breast Cancer Whole-Genome Sequences. Nature 2016, 534, 47–54. [Google Scholar] [CrossRef]
- Pereira, B.; Chin, S.-F.; Rueda, O.M.; Vollan, H.-K.M.; Provenzano, E.; Bardwell, H.A.; Pugh, M.; Jones, L.; Russell, R.; Sammut, S.-J.; et al. The Somatic Mutation Profiles of 2,433 Breast Cancers Refine Their Genomic and Transcriptomic Landscapes. Nat. Commun. 2016, 7, 11479. [Google Scholar] [CrossRef] [Green Version]
- Koboldt, D.C.; Fulton, R.S.; McLellan, M.D.; Schmidt, H.; Kalicki-Veizer, J.; McMichael, J.F.; Fulton, L.L.; Dooling, D.J.; Ding, L.; Mardis, E.R.; et al. Comprehensive Molecular Portraits of Human Breast Tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Bertucci, F.; Ng, C.K.Y.; Patsouris, A.; Droin, N.; Piscuoglio, S.; Carbuccia, N.; Soria, J.C.; Dien, A.T.; Adnani, Y.; Kamal, M.; et al. Genomic Characterization of Metastatic Breast Cancers. Nature 2019, 569, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Polak, P.; Kim, J.; Braunstein, L.Z.; Karlic, R.; Haradhavala, N.J.; Tiao, G.; Rosebrock, D.; Livitz, D.; Kübler, K.; Mouw, K.W.; et al. A Mutational Signature Reveals Alterations Underlying Deficient Homologous Recombination Repair in Breast Cancer. Nat. Genet. 2017, 49, 1476–1486. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, P.; Bandlamudi, C.; Cheng, M.L.; Srinivasan, P.; Chavan, S.S.; Friedman, N.D.; Rosen, E.Y.; Richards, A.L.; Bouvier, N.; Selcuklu, S.D.; et al. Tumour Lineage Shapes BRCA-Mediated Phenotypes. Nature 2019, 571, 576–579. [Google Scholar] [CrossRef]
- O’Shaughnessy, J.; Brezden-Masley, C.; Cazzaniga, M.; Dalvi, T.; Walker, G.; Bennett, J.; Ohsumi, S. Prevalence of Germline BRCA Mutations in HER2-Negative Metastatic Breast Cancer: Global Results from the Real-World, Observational BREAKOUT Study. Breast Cancer Res. 2020, 22, 114. [Google Scholar] [CrossRef]
- Esteller, M.; Silva, J.M.; Dominguez, G.; Bonilla, F.; Matias-Guiu, X.; Lerma, E.; Bussaglia, E.; Prat, J.; Harkes, I.C.; Repasky, E.A.; et al. Promoter Hypermethylation and BRCA1 Inactivation in Sporadic Breast and Ovarian Tumors. J. Natl. Cancer Inst. 2000, 92, 564–569. [Google Scholar] [CrossRef]
- Chen, B.; Zhang, G.; Li, X.; Ren, C.; Wang, Y.; Li, K.; Mok, H.; Cao, L.; Wen, L.; Jia, M.; et al. Comparison of BRCA versus Non-BRCA Germline Mutations and Associated Somatic Mutation Profiles in Patients with Unselected Breast Cancer. Aging 2020, 12, 3140–3155. [Google Scholar] [CrossRef]
- Xie, Y.; Li, G.; Chen, M.; Guo, X.; Tang, L.; Luo, X.; Wang, S.; Yi, W.; Dai, L.; Wang, J. Mutation Screening of 10 Cancer Susceptibility Genes in Unselected Breast Cancer Patients. Clin. Genet. 2018, 93, 41–51. [Google Scholar] [CrossRef]
- Paul, M.R.; Pan, T.; Pant, D.K.; Shih, N.N.C.; Chen, Y.; Harvey, K.L.; Solomon, A.; Lieberman, D.; Morrissette, J.J.D.; Soucier-Ernst, D.; et al. Genomic Landscape of Metastatic Breast Cancer Identifies Preferentially Dysregulated Pathways and Targets. J. Clin. Investig. 2020, 130, 4252–4265. [Google Scholar] [CrossRef]
- Antoniou, A.C.; Casadei, S.; Heikkinen, T.; Barrowdale, D.; Pylkäs, K.; Roberts, J.; Lee, A.; Subramanian, D.; De Leeneer, K.; Fostira, F.; et al. Breast-Cancer Risk in Families with Mutations in PALB2. N. Engl. J. Med. 2014, 371, 497–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vahteristo, P.; Bartkova, J.; Eerola, H.; Syrjäkoski, K.; Ojala, S.; Kilpivaara, O.; Tamminen, A.; Kononen, J.; Aittomäki, K.; Heikkilä, P.; et al. A CHEK2 Genetic Variant Contributing to a Substantial Fraction of Familial Breast Cancer. Am. J. Hum. Genet. 2002, 71, 432–438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jerzak, K.J.; Mancuso, T.; Eisen, A. Ataxia–Telangiectasia Gene (ATM) Mutation Heterozygosity in Breast Cancer: A Narrative Review. Curr. Oncol. 2018, 25, e176–e180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renwick, A.; Thompson, D.; Seal, S.; Kelly, P.; Chagtai, T.; Ahmed, M.; North, B.; Jayatilake, H.; Barfoot, R.; Spanova, K.; et al. ATM Mutations That Cause Ataxia-Telangiectasia Are Breast Cancer Susceptibility Alleles. Nat. Genet. 2006, 38, 873–875. [Google Scholar] [CrossRef] [PubMed]
- Blazek, D.; Kohoutek, J.; Bartholomeeusen, K.; Johansen, E.; Hulinkova, P.; Luo, Z.; Cimermancic, P.; Ule, J.; Peterlin, B.M. The Cyclin K/Cdk12 Complex Maintains Genomic Stability via Regulation of Expression of DNA Damage Response Genes. Genes Dev. 2011, 25, 2158–2172. [Google Scholar] [CrossRef] [Green Version]
- Bajrami, I.; Frankum, J.R.; Konde, A.; Miller, R.E.; Rehman, F.L.; Brough, R.; Campbell, J.; Sims, D.; Rafiq, R.; Hooper, S.; et al. Genome-Wide Profiling of Genetic Synthetic Lethality Identifies CDK12 as a Novel Determinant of PARP1/2 Inhibitor Sensitivity. Cancer Res. 2014, 74, 287–297. [Google Scholar] [CrossRef] [Green Version]
- Gorthi, A.; Romero, J.C.; Loranc, E.; Cao, L.; Lawrence, L.A.; Goodale, E.; Iniguez, A.B.; Bernard, X.; Masamsetti, V.P.; Roston, S.; et al. EWS-FLI1 Increases Transcription to Cause R-Loops and Block BRCA1 Repair in Ewing Sarcoma. Nature 2018, 555, 387–391. [Google Scholar] [CrossRef]
- Tung, N.M.; Robson, M.E.; Ventz, S.; Santa-Maria, C.A.; Nanda, R.; Marcom, P.K.; Shah, P.D.; Ballinger, T.J.; Yang, E.S.; Vinayak, S.; et al. TBCRC 048: Phase II Study of Olaparib for Metastatic Breast Cancer and Mutations in Homologous Recombination-Related Genes. J. Clin. Oncol. 2020, 38, 4274–4282. [Google Scholar] [CrossRef]
- Gruber, J.J.; Afghahi, A.; Hatton, A.; Scott, D.; McMillan, A.; Ford, J.M.; Telli, M.L. Talazoparib beyond BRCA: A Phase II Trial of Talazoparib Monotherapy in BRCA1 and BRCA2 Wild-Type Patients with Advanced HER2-Negative Breast Cancer or Other Solid Tumors with a Mutation in Homologous Recombination (HR) Pathway Genes. J. Clin. Oncol. 2019, 37, 3006. [Google Scholar] [CrossRef]
- Buys, S.S.; Sandbach, J.F.; Gammon, A.; Patel, G.; Kidd, J.; Brown, K.L.; Sharma, L.; Saam, J.; Lancaster, J.; Daly, M.B. A Study of over 35,000 Women with Breast Cancer Tested with a 25-Gene Panel of Hereditary Cancer Genes. Cancer 2017, 123, 1721–1730. [Google Scholar] [CrossRef] [Green Version]
- Tung, N.; Battelli, C.; Allen, B.; Kaldate, R.; Bhatnagar, S.; Bowles, K.; Timms, K.; Garber, J.E.; Herold, C.; Ellisen, L.; et al. Frequency of Mutations in Individuals with Breast Cancer Referred for BRCA1 and BRCA2 Testing Using Next-Generation Sequencing with a 25-Gene Panel. Cancer 2015, 121, 25–33. [Google Scholar] [CrossRef]
- Robson, M.; Im, S.-A.; Senkus, E.; Xu, B.; Domchek, S.M.; Masuda, N.; Delaloge, S.; Li, W.; Tung, N.; Armstrong, A.; et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. N. Engl. J. Med. 2017, 377, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Robson, M.E.; Tung, N.; Conte, P.; Im, S.-A.; Senkus, E.; Xu, B.; Masuda, N.; Delaloge, S.; Li, W.; Armstrong, A.; et al. OlympiAD Final Overall Survival and Tolerability Results: Olaparib versus Chemotherapy Treatment of Physician’s Choice in Patients with a Germline BRCA Mutation and HER2-Negative Metastatic Breast Cancer. Ann. Oncol. 2019, 30, 558–566. [Google Scholar] [CrossRef]
- Litton, J.K.; Rugo, H.S.; Ettl, J.; Hurvitz, S.A.; Gonçalves, A.; Lee, K.-H.; Fehrenbacher, L.; Yerushalmi, R.; Mina, L.A.; Martin, M.; et al. Talazoparib in Patients with Advanced Breast Cancer and a Germline BRCA Mutation. N. Engl. J. Med. 2018, 379, 753–763. [Google Scholar] [CrossRef] [PubMed]
- Litton, J.K.; Hurvitz, S.A.; Mina, L.A.; Rugo, H.S.; Lee, K.-H.; Gonçalves, A.; Diab, S.; Woodward, N.; Goodwin, A.; Yerushalmi, R.; et al. Talazoparib versus Chemotherapy in Patients with Germline BRCA1/2-Mutated HER2-Negative Advanced Breast Cancer: Final Overall Survival Results from the EMBRACA Trial. Ann. Oncol. 2020, 31, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- Turner, N.C.; Telli, M.L.; Rugo, H.S.; Mailliez, A.; Ettl, J.; Grischke, E.-M.; Mina, L.A.; Balmaña, J.; Fasching, P.A.; Hurvitz, S.A.; et al. A Phase II Study of Talazoparib after Platinum or Cytotoxic Nonplatinum Regimens in Patients with Advanced Breast Cancer and Germline BRCA1/2 Mutations (ABRAZO). Clin. Cancer Res. 2019, 25, 2717–2724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ettl, J.; Quek, R.G.W.; Lee, K.-H.; Rugo, H.S.; Hurvitz, S.; Gonçalves, A.; Fehrenbacher, L.; Yerushalmi, R.; Mina, L.A.; Martin, M.; et al. Quality of Life with Talazoparib versus Physician’s Choice of Chemotherapy in Patients with Advanced Breast Cancer and Germline BRCA1/2 Mutation: Patient-Reported Outcomes from the EMBRACA Phase III Trial. Ann. Oncol. 2018, 29, 1939–1947. [Google Scholar] [CrossRef] [PubMed]
- Robson, M.; Ruddy, K.J.; Im, S.-A.; Senkus, E.; Xu, B.; Domchek, S.M.; Masuda, N.; Li, W.; Tung, N.; Armstrong, A.; et al. Patient-Reported Outcomes in Patients with a Germline BRCA Mutation and HER2-Negative Metastatic Breast Cancer Receiving Olaparib versus Chemotherapy in the OlympiAD Trial. Eur. J. Cancer 2019, 120, 20–30. [Google Scholar] [CrossRef] [Green Version]
- Diéras, V.; Han, H.S.; Kaufman, B.; Wildiers, H.; Friedlander, M.; Ayoub, J.-P.; Puhalla, S.L.; Bondarenko, I.; Campone, M.; Jakobsen, E.H.; et al. Veliparib with Carboplatin and Paclitaxel in BRCA-Mutated Advanced Breast Cancer (BROCADE3): A Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet Oncol. 2020, 21, 1269–1282. [Google Scholar] [CrossRef]
- Patsouris, A.; Tredan, O.; Nenciu, D.; Tran-Dien, A.; Campion, L.; Goncalves, A.; Arnedos, M.; Sablin, M.-P.; Gouraud, W.; Jimenez, M.; et al. RUBY: A Phase II Study Testing Rucaparib in Germline (g) BRCA Wild-Type Patients Presenting Metastatic Breast Cancer (MBC) with Homologous Recombination Deficiency (HRD). J. Clin. Oncol. 2019, 37, 1092. [Google Scholar] [CrossRef]
- Litton, J.K.; Laird, A.D.; Rugo, H.S.; Ettl, J.; Hurvitz, S.A.; Martin, M.; Roché, H.; Im, Y.-H.; Goodwin, A.; Blum, J.L.; et al. Abstract CT072: Exploration of Impact of Tumor BRCA Zygosity and Genomic Loss-of-Heterozygosity (GLOH) on Efficacy in Phase 3 EMBRACA Study of Talazoparib in Patients (Pts) with HER2-Negative (HER2-) Advanced Breast Cancer (ABC) and a Germline BRCA1/2 (gBRCA1/2) Mutation. Cancer Res. 2020, 80, CT072. [Google Scholar]
- Gennari, A.; André, F.; Barrios, C.H.; Cortés, J.; de Azambuja, E.; De Michele, A.; Dent, R.; Fenlon, D.; Gligorov, J.; Hurvitz, S.A.; et al. ESMO Clinical Practice Guideline for the Diagnosis, Staging and Treatment of Patients with Metastatic Breast Cancer. Ann. Oncol. 2021, 32, 1475–1495. [Google Scholar] [CrossRef] [PubMed]
- Fasching, P.A.; Link, T.; Hauke, J.; Seither, F.; Jackisch, C.; Klare, P.; Schmatloch, S.; Hanusch, C.; Huober, J.; Stefek, A.; et al. Neoadjuvant Paclitaxel/Olaparib in Comparison to Paclitaxel/Carboplatinum in Patients with HER2-Negative Breast Cancer and Homologous Recombination Deficiency (GeparOLA Study). Ann. Oncol. 2021, 32, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Litton, J.K.; Scoggins, M.; Hess, K.R.; Adrada, B.; Barcenas, C.H.; Murthy, R.K.; Damodaran, S.; DeSnyder, S.M.; Brewster, A.M.; Thompson, A.M.; et al. Neoadjuvant Talazoparib (TALA) for Operable Breast Cancer Patients with a BRCA Mutation (BRCA+). J. Clin. Oncol. 2018, 36, 508. [Google Scholar] [CrossRef]
- Litton, J.K.; Beck, J.T.; Jones, J.M.; Andersen, J.; Blum, J.L.; Mina, L.A.; Brig, R.; Danso, M.A.; Yuan, Y.; Abbattista, A.; et al. Neoadjuvant Talazoparib in Patients with Germline BRCA1/2 (GBRCA1/2) Mutation-Positive, Early HER2-Negative Breast Cancer (BC): Results of a Phase 2 Study. J. Clin. Oncol. 2021, 39, 505. [Google Scholar] [CrossRef]
- Tutt, A.N.J.; Garber, J.E.; Kaufman, B.; Viale, G.; Fumagalli, D.; Rastogi, P.; Gelber, R.D.; de Azambuja, E.; Fielding, A.; Balmaña, J.; et al. Adjuvant Olaparib for Patients with BRCA1- or BRCA2-Mutated Breast Cancer. N. Engl. J. Med. 2021, 384, 2394–2405. [Google Scholar] [CrossRef]
- Tung, N.M.; Zakalik, D.; Somerfield, M.R. Adjuvant PARP Inhibitors in Patients with High-Risk Early-Stage HER2-Negative Breast Cancer and Germline BRCA Mutations: ASCO Hereditary Breast Cancer Guideline Rapid Recommendation Update. J. Clin. Oncol. 2021, 39, 2959–2961. [Google Scholar] [CrossRef]
- Vlessis, K.; Purington, N.; Chun, N.; Haraldsdottir, S.; Ford, J.M. Germline Testing for Patients With BRCA1/2 Mutations on Somatic Tumor Testing. JNCI Cancer Spectr. 2020, 4, pkz095. [Google Scholar] [CrossRef] [Green Version]
- Familial Breast Cancer: Classification, Care and Managing Breast Cancer and Related Risks in People with a Family History of Breast Cancer. 2019; Volume 49, PMID: 31940157. Available online: https://pubmed.ncbi.nlm.nih.gov/31940157/ (accessed on 11 December 2021).
- Daly, M.B.; Reiser, G.; Pal, T.; Kohlmann, W.; Senter-Jamieson, L.; Kurian, A.W.; Shannon, K.M.; Dickson, P.; Mak, J.S.; Menendez, C.S.; et al. NCCN Guidelines Index Table of Contents Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic Discussion. Risk Assess. 2020, 122, 1–122. [Google Scholar]
- Myriad Genetics. Products & Services. BRACAnalysis. Available online: http://myriad.com/products-services/hereditary-cancers/bracanalysis/ (accessed on 7 March 2021).
- Judkins, T.; Rosenthal, E.; Arnell, C.; Burbidge, L.A.; Geary, W.; Barrus, T.; Schoenberger, J.; Trost, J.; Wenstrup, R.J.; Roa, B.B. Clinical Significance of Large Rearrangements in BRCA1 and BRCA2. Cancer 2012, 118, 5210–5216. [Google Scholar] [CrossRef] [Green Version]
- BRACAnalysisTM Technical Specifications. 2. Available online: https://s3.amazonaws.com/myriad-library/technical-specifications/BRCA+Tech+Specs_Integrated.pdf (accessed on 15 December 2021).
- Eric Pujade-Lauraine on First-Line Maintenance Therapy in Ovarian Cancer—The ASCO Post. Available online: https://ascopost.com/videos/sgo-2021-virtual-annual-meeting-on-womens-cancer/eric-pujade-lauraine-on-first-line-maintenance-therapy-in-ovarian-cancer/ (accessed on 21 June 2021).
- Popova, T.; Manié, E.; Rieunier, G.; Caux-Moncoutier, V.; Tirapo, C.; Dubois, T.; Delattre, O.; Sigal-Zafrani, B.; Bollet, M.; Longy, M.; et al. Ploidy and Large-Scale Genomic Instability Consistently Identify Basal-like Breast Carcinomas with BRCA1/2 Inactivation. Cancer Res. 2012, 72, 5454–5462. [Google Scholar] [CrossRef] [Green Version]
- Abkevich, V.; Timms, K.M.; Hennessy, B.T.; Potter, J.; Carey, M.S.; Meyer, L.A.; Smith-McCune, K.; Broaddus, R.; Lu, K.H.; Chen, J.; et al. Patterns of Genomic Loss of Heterozygosity Predict Homologous Recombination Repair Defects in Epithelial Ovarian Cancer. Br. J. Cancer 2012, 107, 1776–1782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birkbak, N.J.; Wang, Z.C.; Kim, J.-Y.; Eklund, A.C.; Li, Q.; Tian, R.; Bowman-Colin, C.; Li, Y.; Greene-Colozzi, A.; Iglehart, J.D.; et al. Telomeric Allelic Imbalance Indicates Defective DNA Repair and Sensitivity to DNA-Damaging Agents. Cancer Discov. 2012, 2, 366–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Min, A.; Kim, K.; Jeong, K.; Choi, S.; Kim, S.; Suh, K.J.; Lee, K.-H.; Kim, S.; Im, S.-A. Homologous Repair Deficiency Score for Identifying Breast Cancers with Defective DNA Damage Response. Sci. Rep. 2020, 10, 12506. [Google Scholar] [CrossRef] [PubMed]
- Timms, K.M.; Abkevich, V.; Hughes, E.; Neff, C.; Reid, J.; Morris, B.; Kalva, S.; Potter, J.; Tran, T.V.; Chen, J.; et al. Association of BRCA1/2 Defects with Genomic Scores Predictive of DNA Damage Repair Deficiency among Breast Cancer Subtypes. Breast Cancer Res. 2014, 16, 475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, H.; Glodzik, D.; Morganella, S.; Yates, L.R.; Staaf, J.; Zou, X.; Ramakrishna, M.; Martin, S.; Boyault, S.; Sieuwerts, A.M.; et al. HRDetect Is a Predictor of BRCA1 and BRCA2 Deficiency Based on Mutational Signatures. Nat. Med. 2017, 23, 517–525. [Google Scholar] [CrossRef]
- Staaf, J.; Glodzik, D.; Bosch, A.; Vallon-Christersson, J.; Reuterswärd, C.; Häkkinen, J.; Degasperi, A.; Amarante, T.D.; Saal, L.H.; Hegardt, C.; et al. Whole-Genome-Sequencing of Triple Negative Breast Cancers in a Population-Based Clinical Study. Nat. Med. 2019, 25, 1526–1533. [Google Scholar] [CrossRef]
- Chopra, N.; Tovey, H.; Pearson, A.; Cutts, R.; Toms, C.; Proszek, P.; Hubank, M.; Dowsett, M.; Dodson, A.; Daley, F.; et al. Homologous Recombination DNA Repair Deficiency and PARP Inhibition Activity in Primary Triple Negative Breast Cancer. Nat. Commun. 2020, 11, 2662. [Google Scholar] [CrossRef]
- Póti, Á.; Gyergyák, H.; Németh, E.; Rusz, O.; Tóth, S.; Kovácsházi, C.; Chen, D.; Szikriszt, B.; Spisák, S.; Takeda, S.; et al. Correlation of Homologous Recombination Deficiency Induced Mutational Signatures with Sensitivity to PARP Inhibitors and Cytotoxic Agents. Genome Biol. 2019, 20, 240. [Google Scholar] [CrossRef]
- Waks, A.G.; Cohen, O.; Kochupurakkal, B.; Kim, D.; Dunn, C.E.; Buendia, J.B.; Wander, S.; Helvie, K.; Lloyd, M.R.; Marini, L.; et al. Reversion and Non-Reversion Mechanisms of Resistance to PARP Inhibitor or Platinum Chemotherapy in BRCA1/2-Mutant Metastatic Breast Cancer. Ann. Oncol. 2020, 31, 590–598. [Google Scholar] [CrossRef]
- Swisher, E.M.; Kwan, T.T.; Oza, A.M.; Tinker, A.V.; Ray-Coquard, I.; Oaknin, A.; Coleman, R.L.; Aghajanian, C.; Konecny, G.E.; O’Malley, D.M.; et al. Molecular and Clinical Determinants of Response and Resistance to Rucaparib for Recurrent Ovarian Cancer Treatment in ARIEL2 (Parts 1 and 2). Nat. Commun. 2021, 12, 2487. [Google Scholar] [CrossRef]
- Vollebergh, M.A.; Lips, E.H.; Nederlof, P.M.; Wessels, L.F.A.; Schmidt, M.K.; van Beers, E.H.; Cornelissen, S.; Holtkamp, M.; Froklage, F.E.; de Vries, E.G.E.; et al. An ACGH Classifier Derived from BRCA1-Mutated Breast Cancer and Benefit of High-Dose Platinum-Based Chemotherapy in HER2-Negative Breast Cancer Patients. Ann. Oncol. 2011, 22, 1561–1570. [Google Scholar] [CrossRef] [PubMed]
- Schouten, P.C.; Grigoriadis, A.; Kuilman, T.; Mirza, H.; Watkins, J.A.; Cooke, S.A.; van Dyk, E.; Severson, T.M.; Rueda, O.M.; Hoogstraat, M.; et al. Robust BRCA1-like Classification of Copy Number Profiles of Samples Repeated across Different Datasets and Platforms. Mol. Oncol. 2015, 9, 1274–1286. [Google Scholar] [CrossRef] [PubMed]
- Vollebergh, M.A.; Lips, E.H.; Nederlof, P.M.; Wessels, L.F.A.; Wesseling, J.; Vd Vijver, M.J.; de Vries, E.G.E.; van Tinteren, H.; Jonkers, J.; Hauptmann, M.; et al. Genomic Patterns Resembling BRCA1- and BRCA2-Mutated Breast Cancers Predict Benefit of Intensified Carboplatin-Based Chemotherapy. Breast Cancer Res. 2014, 16, R47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stuppia, L.; Antonucci, I.; Palka, G.; Gatta, V. Use of the MLPA Assay in the Molecular Diagnosis of Gene Copy Number Alterations in Human Genetic Diseases. Int. J. Mol. Sci. 2012, 13, 3245–3276. [Google Scholar] [CrossRef]
- Lips, E.H.; Laddach, N.; Savola, S.P.; Vollebergh, M.A.; Oonk, A.M.; Imholz, A.L.; Wessels, L.F.; Wesseling, J.; Nederlof, P.M.; Rodenhuis, S. Quantitative Copy Number Analysis by Multiplex Ligation-Dependent Probe Amplification (MLPA) of BRCA1-Associated Breast Cancer Regions Identifies BRCAness. Breast Cancer Res. 2011, 13, R107. [Google Scholar] [CrossRef] [Green Version]
- Lips, E.H.; Benard-Slagter, A.; Opdam, M.; Scheerman, C.E.; Wesseling, J.; Hogervorst, F.B.L.; Linn, S.C.; Savola, S.; Nederlof, P.M. BRCAness DigitalMLPA Profiling Predicts Benefit of Intensified Platinum-Based Chemotherapy in Triple-Negative and Luminal-Type Breast Cancer. Breast Cancer Res. 2020, 22, 79. [Google Scholar] [CrossRef]
- Mutter, R.W.; Riaz, N.; Ng, C.K.; Delsite, R.; Piscuoglio, S.; Edelweiss, M.; Martelotto, L.G.; Sakr, R.A.; King, T.A.; Giri, D.D.; et al. Bi-Allelic Alterations in DNA Repair Genes Underpin Homologous Recombination DNA Repair Defects in Breast Cancer. J. Pathol. 2017, 242, 165–177. [Google Scholar] [CrossRef]
- Castroviejo-Bermejo, M.; Cruz, C.; Llop-Guevara, A.; Gutiérrez-Enríquez, S.; Ducy, M.; Ibrahim, Y.H.; Gris-Oliver, A.; Pellegrino, B.; Bruna, A.; Guzmán, M.; et al. A RAD51 Assay Feasible in Routine Tumor Samples Calls PARP Inhibitor Response beyond BRCA Mutation. EMBO Mol. Med. 2018, 10. [Google Scholar] [CrossRef]
- Kochupurakkal, B.S.; Parmar, K.; Lazaro, J.-B.; Unitt, C.; Zeng, Q.; Reavis, H.; Ganesa, C.; Zhou, S.; Liu, J.; Palakurthi, S.; et al. Abstract 2796: Development of a RAD51-Based Assay for Determining Homologous Recombination Proficiency and PARP Inhibitor Sensitivity. Cancer Res. 2017, 77, 2796. [Google Scholar] [CrossRef]
- Cruz, C.; Castroviejo-Bermejo, M.; Gutiérrez-Enríquez, S.; Llop-Guevara, A.; Ibrahim, Y.H.; Gris-Oliver, A.; Bonache, S.; Morancho, B.; Bruna, A.; Rueda, O.M.; et al. RAD51 Foci as a Functional Biomarker of Homologous Recombination Repair and PARP Inhibitor Resistance in Germline BRCA-Mutated Breast Cancer. Ann. Oncol. 2018, 29, 1203. [Google Scholar] [CrossRef]
- Mayer, E.L.; Abramson, V.; Jankowitz, R.; Falkson, C.; Marcom, P.K.; Traina, T.; Carey, L.; Rimawi, M.; Specht, J.; Miller, K.; et al. TBCRC 030: A Phase II Study of Preoperative Cisplatin versus Paclitaxel in Triple-Negative Breast Cancer: Evaluating the Homologous Recombination Deficiency (HRD) Biomarker. Ann. Oncol. 2020, 31, 1518–1525. [Google Scholar] [CrossRef] [PubMed]
- Pujol, P.; Barberis, M.; Beer, P.; Friedman, E.; Piulats, J.M.; Capoluongo, E.D.; Foncillas, J.G.; Ray-Coquard, I.; Penault-Llorca, F.; Foulkes, W.D.; et al. Clinical Practice Guidelines for BRCA1 and BRCA2 Genetic Testing. Eur. J. Cancer 2021, 146, 30–47. [Google Scholar] [CrossRef] [PubMed]
| OLYMPIAD | EMBRACA | BROCADE3 | LUCY | TBCRC 048 | |
|---|---|---|---|---|---|
| Study design | Phase III randomized N = 302 | Phase III randomized N = 431 | Phase III randomized N = 509 | Phase IIIb single arm N = 256 | Phase II single arm N = 54 |
| Overall population | |||||
| Population | Germline BRCA1/2 mutations ≤2 previous cytotoxic regimens for advanced breast cancer Previous taxane and/or anthracycline DFI > 12 months after platinum treatment No limit of previous endocrine therapy, unless one prior endocrine therapy | Germline BRCA1/2 mutations ≤3 previous cytotoxic regimens for advanced breast cancer Previous taxane and/or anthracycline DFI > 6 months after platinum treatment No limit of previous endocrine therapy | Germline BRCA1/2 mutations ≤2 previous cytotoxic regimens for advanced breast cancer Previous taxane allowed but given more than 6 or 12 months before study start in (neo)adjuvant or metastatic setting, respectively DFI > 12 months after platinum treatment No limit of previous endocrine therapy | Germline or somatic BRCA1/2 mutations ≤2 previous cytotoxic regimens for advanced breast cancer Previous taxane and/or anthracycline DFI > 12 months after platinum treatment No limit of previous endocrine therapy, unless one prior endocrine therapy | Germline or somatic mutations in DNA repair gene other than BRCA1/2 (cohort 1) Or somatic pathogenic variant of BRCA1 or BRCA2 genes or in other DNA repair genes (1) (cohort 2) No limit of prior cytotoxic regimen or endocrine therapy for advanced breast cancer DFI > 12 months after platinum treatment |
| BRCA testing | Central testing with BRCAnalysis Myriads genetics | Central testing with BRCAnalysis Myriads genetics | Central testing with BRCAnalysis Myriads genetics | BRCA mutation testing in certified laboratory | Genomic profiling of metastatic tumor tissue or blood |
| PARP inhibitors, experimental arm | Olaparib 300 mg twice daily continuously | Talazoparib 1 mg once daily continuously | Carboplatin + paclitaxel + veliparib 120 mg twice daily on days 2–5 | Olaparib 300 mg twice daily continuously | Olaparib 300 mg twice daily continuously |
| Control arm treatment | Chemotherapy of choice of investigator among capecitabine, eribulin, or vinorelbine No crossover allowed | Chemotherapy of choice of investigator among capecitabine, eribulin, gemcitabine, or vinorelbine No crossover allowed | Carboplatin + paclitaxel + placebo Crossover allowed | NA | NA |
| Prior chemotherapy n (%) | 215 (71%) | 265 (61%) | 96 (18.8%) | 115 (45%) | 44 (81%) |
| Prior platinum n (%) | 86 (28%) | 76 (17%) | 43 (8%) | 81 (32%) | 3 (6%) |
| ORR (%) | 59.9% versus 28.8% in control arm | 62.6% versus 27.2% in control arm | 75.8% versus 74.1% in control arm | 48.6% | Cohort 1 29.6% Cohort 2 38.5% gPALB2 mutation: 82% sBRCA1/2 mutations: 50% |
| Median time to response | 1.5 months | 2.6 months | NR | NR | NR |
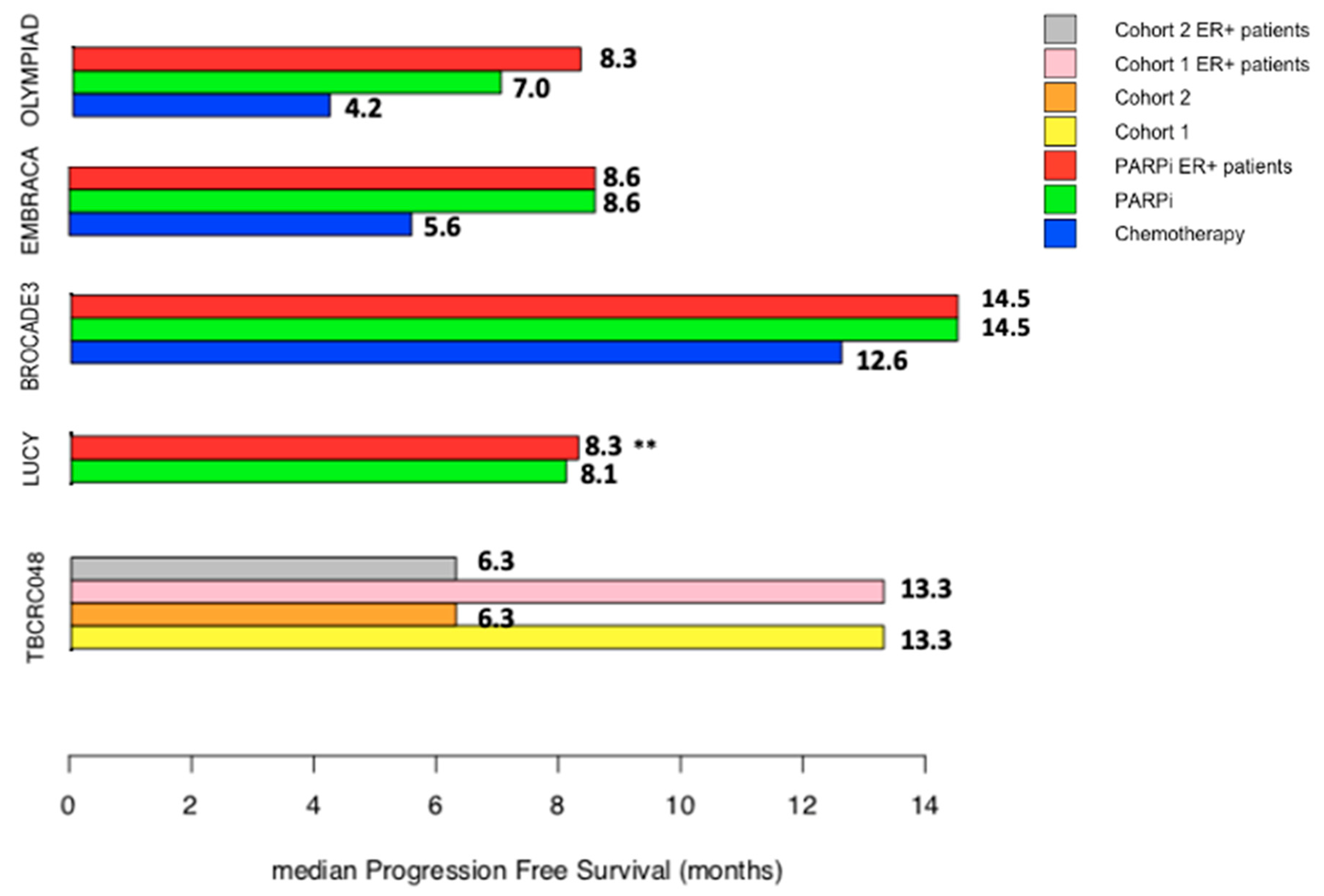
| PFS | 7.0 vs. 4.2 months Hazard ratio 0.58 (95% CI 0.43 to 0.80) p < 0.001 | 8.6 vs. 5.6 months Hazard ratio 0.54 (95% CI 0.41–0.71) p < 0.001 | 14.5 versus 12.6 months Hazard ratio 0·71 (95% CI 0.57–0.88) p = 0·0016 | 8.11 months (95% CI 6.93–8.67) No comparison, single arm | Cohort 1: 13.3 months (90%CI 12—NA) Cohort 2: 6.3 months (90%CI 4.4 months—NA) No comparison |
| OS | 19.3 vs. 17.1 months Hazard ratio 0.90 (95% CI 0.66–1.23) p = 0.513 | 19.3 versus 19.5 months Hazard ratio 0.85 (95% CI 0.670–1.073) p= 0.17 | 33.5 vs. 28.2 months Hazard ratio 0.95 (95% CI 0.73–1.23) p = 0·67 | NR | NR |
| PARP inhibitor after progression in control arm | 8.2% | 25% | 44% | NA | NA |
| ER+/HER2- patients | |||||
| Number (%) | 152 (50.3%) | 241 (56%) | 266 (53%) | 131 (51%) | 41 (76%) |
| ORR (%) | 65.4% vs. 36.4% | 63.2% vs. 37.9% | NR | NR | 30% |
| Median PFS with PARP inhibitors, Hazard ratio compared to control arm (2) | 8.3 months Hazard ratio 0.82 (95% CI 0.55–1.26) | 8.6 months Hazard ratio 0.47 (95%CI 0.32–0.71) | 14.5 months Hazard ratio 0.69 (95%CI 0.52–0.92) | 8.3 months NA | Median PFS 13.3 months for gPALB2 mutation and 6.3 months for sBRCA1/2 mutations NA |
| Median OS with PARP inhibitors Hazard ratio compared with control arm | 21.8 versus 21.3 months Hazard ratio 0.86 (95% CI 0.55–1.36) | NR Hazard ratio of 0.827 (0.56–1.14) | Median OS of 32.4 vs. 27.1 months NR | NR | NR |
| Previous endocrine therapy n (%) | 136 (45%) | 219 (91%) | 91 (34%) | NR | NR |
| Prior chemotherapy n (%) | 117 (77%) | NR | 63 (23.6%) | NR | NR |
| Prior platinum n (%) | 35 (23%) | NR | NR | NR | 0 (0%) |
| Prior CDK4/6 inhibitors n (%) | NR | 22 (9%) | NR | NR | 40 (97.5%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collet, L.; Péron, J.; Penault-Llorca, F.; Pujol, P.; Lopez, J.; Freyer, G.; You, B. PARP Inhibitors: A Major Therapeutic Option in Endocrine-Receptor Positive Breast Cancers. Cancers 2022, 14, 599. https://doi.org/10.3390/cancers14030599
Collet L, Péron J, Penault-Llorca F, Pujol P, Lopez J, Freyer G, You B. PARP Inhibitors: A Major Therapeutic Option in Endocrine-Receptor Positive Breast Cancers. Cancers. 2022; 14(3):599. https://doi.org/10.3390/cancers14030599
Chicago/Turabian StyleCollet, Laetitia, Julien Péron, Frédérique Penault-Llorca, Pascal Pujol, Jonathan Lopez, Gilles Freyer, and Benoît You. 2022. "PARP Inhibitors: A Major Therapeutic Option in Endocrine-Receptor Positive Breast Cancers" Cancers 14, no. 3: 599. https://doi.org/10.3390/cancers14030599
APA StyleCollet, L., Péron, J., Penault-Llorca, F., Pujol, P., Lopez, J., Freyer, G., & You, B. (2022). PARP Inhibitors: A Major Therapeutic Option in Endocrine-Receptor Positive Breast Cancers. Cancers, 14(3), 599. https://doi.org/10.3390/cancers14030599







