Performance and Prospects of [68Ga]Ga-FAPI PET/CT Scans in Lung Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Prognostic Value of FAP-Expression
2.1. Lung Cancer
2.2. Prognostic Value of [68Ga]Ga-FAPI Uptake in PET
3. FAPI Imaging in Lung Cancer
3.1. FAP-Expression in Lung Cancer
3.2. Imaging of Primary Tumor Lesions
3.3. Imaging of Metastatic Lesions
3.3.1. Locoregional Metastasis
3.3.2. Cerebral Metastasis
3.3.3. Lymph Node Metastasis
3.3.4. Cardiac Metastasis
3.4. Limitations of [68Ga]Ga-FAPI PET/CT in Lung Cancer
4. Conclusions and Future Perspective
Author Contributions
Funding
Conflicts of Interest
References
- European Union. ECIS—European Cancer Information System. European Commission 2020. Available online: https://ecis.jrc.ec.europa.eu (accessed on 30 September 2022).
- Telo, S.; Calderoni, L.; Vichi, S.; Zagni, F.; Castellucci, P.; Fanti, S. Alternative and New Radiopharmaceutical Agents for Lung Cancer. Curr. Radiopharm. 2020, 13, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Roma-Rodrigues, C.; Mendes, R.; Baptista, P.V.; Fernandes, A.R. Targeting Tumor Microenvironment for Cancer Therapy. Int. J. Mol. Sci. 2019, 20, 840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baghban, R.; Roshangar, L.; Jahanban-Esfahlan, R.; Seidi, K.; Ebrahimi-Kalan, A.; Jaymand, M.; Kolahian, S.; Javaheri, T.; Zare, P. Tumor microenvironment complexity and therapeutic implications at a glance. Cell Commun. Signal. 2020, 18, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindner, T.; Loktev, A.; Giesel, F.; Kratochwil, C.; Altmann, A.; Haberkorn, U. Targeting of activated fibroblasts for imaging and therapy. EJNMMI Radiopharm. Chem. 2019, 4, 16. [Google Scholar] [CrossRef]
- Puré, E.; Blomberg, R. Pro-tumorigenic roles of fibroblast activation protein in cancer: Back to the basics. Oncogene 2018, 37, 4343–4357. [Google Scholar] [CrossRef]
- Wang, H.; Wu, Q.; Liu, Z.; Luo, X.; Fan, Y.; Liu, Y.; Zhang, Y.; Hua, S.; Fu, Q.; Zhao, M.; et al. Downregulation of FAP suppresses cell proliferation and metastasis through PTEN/PI3K/AKT and Ras-ERK signaling in oral squamous cell carcinoma. Cell Death Dis. 2014, 5, e1155. [Google Scholar] [CrossRef] [Green Version]
- Mhawech-Fauceglia, P.; Yan, L.; Sharifian, M.; Ren, X.; Liu, S.; Kim, G.; Gayther, S.A.; Pejovic, T.; Lawrenson, K. Stromal Expression of Fibroblast Activation Protein Alpha (FAP) Predicts Platinum Resistance and Shorter Recurrence in patients with Epithelial Ovarian Cancer. Cancer Microenviron. 2015, 8, 23–31. [Google Scholar] [CrossRef] [Green Version]
- Shi, M.; Yu, D.H.; Chen, Y.; Zhao, C.Y.; Zhang, J.; Liu, Q.H.; Ni, C.R.; Zhu, M.H. Expression of fibroblast activation protein in human pancreatic adenocarcinoma and its clinicopathological significance. World J. Gastroenterol. 2012, 18, 840–846. [Google Scholar] [CrossRef]
- Dendl, K.; Schlittenhardt, J.; Staudinger, F.; Kratochwil, C.; Altmann, A.; Haberkorn, U.; Giesel, F.L. The Role of Fibroblast Activation Protein Ligands in Oncologic PET Imaging. PET Clin. 2021, 16, 341–351. [Google Scholar] [CrossRef]
- Chemical Reagents for Life Sciences. Available online: https://www.chemscene.com/ (accessed on 13 October 2022).
- Flechsig, P.; Mehndiratta, A.; Haberkorn, U.; Kratochwil, C.; Giesel, F.L. PET/MRI and PET/CT in Lung Lesions and Thoracic Malignancies. Semin. Nucl. Med. 2015, 45, 268–281. [Google Scholar] [CrossRef]
- Deppen, S.A.; Blume, J.D.; Kensinger, C.D.; Morgan, A.M.; Aldrich, M.C.; Massion, P.P.; Walker, R.C.; McPheeters, M.L.; Putnam, J.B., Jr.; Grogan, E.L. Accuracy of FDG-PET to diagnose lung cancer in areas with infectious lung disease: A meta-analysis. JAMA 2014, 312, 1227–1236. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Tang, G.; Hu, K.; Liu, X.; Zhou, W.; Li, H.; Huang, S.; Han, Y.; Chen, L.; Zhong, J.; et al. Comparison of (68)Ga-FAPI and (18)F-FDG PET/CT in the Evaluation of Advanced Lung Cancer. Radiology 2022, 303, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Treglia, G.; Muoio, B.; Roustaei, H.; Kiamanesh, Z.; Aryana, K.; Sadeghi, R. Head-to-Head Comparison of Fibroblast Activation Protein Inhibitors (FAPI) Radiotracers versus [(18)F]F-FDG in Oncology: A Systematic Review. Int. J. Mol. Sci. 2021, 22, 11192. [Google Scholar] [CrossRef] [PubMed]
- Gu, B.; Liu, X.; Wang, S.; Xu, X.; Liu, X.; Hu, S.; Yan, W.; Luo, Z.; Song, S. Head-to-head evaluation of [(18)F]FDG and [(68) Ga]Ga-DOTA-FAPI-04 PET/CT in recurrent soft tissue sarcoma. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2889–2901. [Google Scholar] [CrossRef] [PubMed]
- Lan, L.; Liu, H.; Wang, Y.; Deng, J.; Peng, D.; Feng, Y.; Wang, L.; Chen, Y.; Qiu, L. The potential utility of [(68) Ga]Ga-DOTA-FAPI-04 as a novel broad-spectrum oncological and non-oncological imaging agent-comparison with [(18)F]FDG. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 963–979. [Google Scholar] [CrossRef] [PubMed]
- Kuten, J.; Levine, C.; Shamni, O.; Pelles, S.; Wolf, I.; Lahat, G.; Mishani, E.; Even-Sapir, E. Head-to-head comparison of [(68)Ga]Ga-FAPI-04 and [(18)F]-FDG PET/CT in evaluating the extent of disease in gastric adenocarcinoma. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 743–750. [Google Scholar] [CrossRef]
- Jiang, D.; Chen, X.; You, Z.; Wang, H.; Zhang, X.; Li, X.; Ren, S.; Huang, Q.; Hua, F.; Guan, Y.; et al. Comparison of [(68) Ga]Ga-FAPI-04 and [(18)F]-FDG for the detection of primary and metastatic lesions in patients with gastric cancer: A bicentric retrospective study. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 732–742. [Google Scholar] [CrossRef]
- Wu, J.; Wang, Y.; Liao, T.; Rao, Z.; Gong, W.; Ou, L.; Chen, Y.; Zhang, C. Comparison of the Relative Diagnostic Performance of [(68)Ga]Ga-DOTA-FAPI-04 and [(18)F]FDG PET/CT for the Detection of Bone Metastasis in Patients With Different Cancers. Front. Oncol. 2021, 11, 737827. [Google Scholar] [CrossRef]
- Kratochwil, C.; Flechsig, P.; Lindner, T.; Abderrahim, L.; Altmann, A.; Mier, W.; Adeberg, S.; Rathke, H.; Röhrich, M.; Winter, H.; et al. (68)Ga-FAPI PET/CT: Tracer Uptake in 28 Different Kinds of Cancer. J. Nucl. Med. 2019, 60, 801–805. [Google Scholar] [CrossRef] [Green Version]
- Liu, F.; Qi, L.; Liu, B.; Liu, J.; Zhang, H.; Che, D.; Cao, J.; Shen, J.; Geng, J.; Bi, Y.; et al. Fibroblast activation protein overexpression and clinical implications in solid tumors: A meta-analysis. PLoS ONE 2015, 10, e0116683. [Google Scholar] [CrossRef]
- Liao, Y.; Ni, Y.; He, R.; Liu, W.; Du, J. Clinical implications of fibroblast activation protein-α in non-small cell lung cancer after curative resection: A new predictor for prognosis. J. Cancer Res. Clin. Oncol. 2013, 139, 1523–1528. [Google Scholar] [CrossRef] [PubMed]
- Kilvaer, T.K.; Khanehkenari, M.R.; Hellevik, T.; Al-Saad, S.; Paulsen, E.E.; Bremnes, R.M.; Busund, L.T.; Donnem, T.; Martinez, I.Z. Cancer Associated Fibroblasts in Stage I-IIIA NSCLC: Prognostic Impact and Their Correlations with Tumor Molecular Markers. PLoS ONE 2015, 10, e0134965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.; Chen, M.; Han, Z.; Jiang, F.; Xu, C.; Qin, Y.; Ding, N.; Liu, Y.; Zhang, T.; An, Z.; et al. Clinical significance of FAP-α on microvessel and lymphatic vessel density in lung squamous cell carcinoma. J. Clin. Pathol. 2018, 71, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Hou, Z.; Yan, J.; Qiu, W.; Liang, L.; Meng, M.; Li, L.; Wang, X.; Xie, Y.; Jiang, L.; et al. The prognostic significance of fibroblast activation protein-α in human lung adenocarcinoma. Ann. Transl. Med. 2020, 8, 224. [Google Scholar] [CrossRef] [PubMed]
- Inamura, K. Update on Immunohistochemistry for the Diagnosis of Lung Cancer. Cancers 2018, 10, 72. [Google Scholar] [CrossRef] [Green Version]
- Mona, C.E.; Benz, M.R.; Hikmat, F.; Grogan, T.R.; Lückerath, K.; Razmaria, A.; Riahi, R.; Slavik, R.; Girgis, M.D.; Carlucci, G.; et al. Correlation of (68)Ga-FAPi-46 PET biodistribution with FAP expression by immunohistochemistry in patients with solid cancers: A prospective translational exploratory study. J. Nucl. Med. 2021, 63, 1021–1026. [Google Scholar] [CrossRef]
- Wei, Y.; Cheng, K.; Fu, Z.; Zheng, J.; Mu, Z.; Zhao, C.; Liu, X.; Wang, S.; Yu, J.; Yuan, S. [(18)F]AlF-NOTA-FAPI-04 PET/CT uptake in metastatic lesions on PET/CT imaging might distinguish different pathological types of lung cancer. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 1671–1681. [Google Scholar] [CrossRef]
- Rong, X.; Lv, J.; Liu, Y.; Wang, Z.; Zeng, D.; Li, Y.; Li, S.; Wu, J.; Shen, Z.; Shi, M.; et al. PET/CT Imaging of Activated Cancer-Associated Fibroblasts Predict Response to PD-1 Blockade in Gastric Cancer Patients. Front. Oncol. 2021, 11, 802257. [Google Scholar] [CrossRef]
- Chen, X.; Liu, X.; Wang, L.; Zhou, W.; Zhang, Y.; Tian, Y.; Tan, J.; Dong, Y.; Fu, L.; Wu, H. Expression of fibroblast activation protein in lung cancer and its correlation with tumor glucose metabolism and histopathology. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2938–2948. [Google Scholar] [CrossRef]
- Giesel, F.L.; Kratochwil, C.; Schlittenhardt, J.; Dendl, K.; Eiber, M.; Staudinger, F.; Kessler, L.; Fendler, W.P.; Lindner, T.; Koerber, S.A.; et al. Head-to-head intra-individual comparison of biodistribution and tumor uptake of (68)Ga-FAPI and (18)F-FDG PET/CT in cancer patients. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 4377–4385. [Google Scholar] [CrossRef]
- Röhrich, M.; Leitz, D.; Glatting, F.M.; Wefers, A.K.; Weinheimer, O.; Flechsig, P.; Kahn, N.; Mall, M.A.; Giesel, F.L.; Kratochwil, C.; et al. Fibroblast Activation Protein-Specific PET/CT Imaging in Fibrotic Interstitial Lung Diseases and Lung Cancer: A Translational Exploratory Study. J. Nucl. Med. 2022, 63, 127–133. [Google Scholar] [CrossRef]
- Hao, B.; Wu, J.; Pang, Y.; Sun, L.; Chen, H. 68Ga-FAPI PET/CT in Assessment of Leptomeningeal Metastases in a Patient With Lung Adenocarcinoma. Clin. Nucl. Med. 2020, 45, 784–786. [Google Scholar] [CrossRef] [PubMed]
- Shang, Q.; Zhao, L.; Pang, Y.; Meng, T.; Chen, H. Differentiation of Reactive Lymph Nodes and Tumor Metastatic Lymph Nodes With 68Ga-FAPI PET/CT in a Patient With Squamous Cell Lung Cancer. Clin. Nucl. Med. 2022, 47, 458–461. [Google Scholar] [CrossRef] [PubMed]
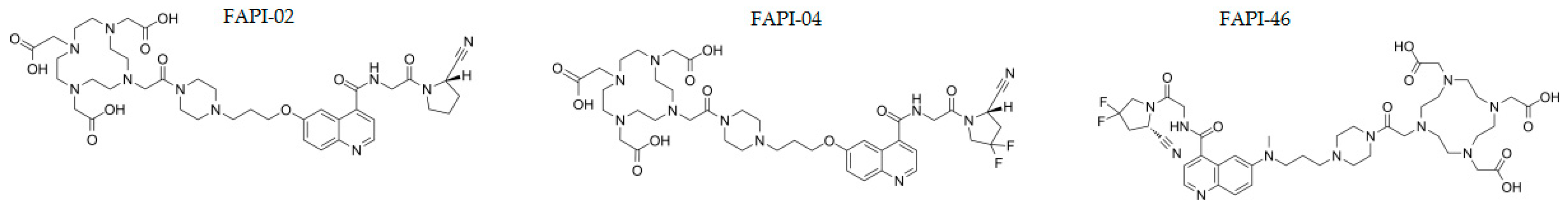
- Loktev, A.; Lindner, T.; Mier, W.; Debus, J.; Altmann, A.; Jäger, D.; Giesel, F.; Kratochwil, C.; Barthe, P.; Roumestand, C.; et al. A Tumor-Imaging Method Targeting Cancer-Associated Fibroblasts. J. Nucl. Med. 2018, 59, 1423–1429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giesel, F.L.; Heussel, C.P.; Lindner, T.; Röhrich, M.; Rathke, H.; Kauczor, H.U.; Debus, J.; Haberkorn, U.; Kratochwil, C. FAPI-PET/CT improves staging in a lung cancer patient with cerebral metastasis. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1754–1755. [Google Scholar] [CrossRef]
- Fu, W.; Liu, L.; Liu, H.; Zhou, Z.; Chen, Y. Increased FAPI Uptake in Brain Metastasis From Lung Cancer on 68Ga-FAPI PET/CT. Clin. Nucl. Med. 2021, 46, e1–e2. [Google Scholar] [CrossRef]
- Liu, Y.; Tao, Y.; Wang, F.; Huang, Z. Mediastinum-type lung cancer on 68Ga-FAPI PET/CT with cardiac insufficiency as the first symptom. J. Nucl. Cardiol. 2021. [Google Scholar] [CrossRef]
- Riihimäki, M.; Hemminki, A.; Fallah, M.; Thomsen, H.; Sundquist, K.; Sundquist, J.; Hemminki, K. Metastatic sites and survival in lung cancer. Lung Cancer 2014, 86, 78–84. [Google Scholar] [CrossRef]
- Li, Y.; Lin, X.; Li, Y.; Lv, J.; Hou, P.; Liu, S.; Chen, P.; Wang, M.; Zhou, C.; Wang, X. Clinical Utility of F-18 Labeled Fibroblast Activation Protein Inhibitor (FAPI) for Primary Staging in Lung Adenocarcinoma: A Prospective Study. Mol. Imaging Biol. 2022, 24, 309–320. [Google Scholar] [CrossRef]
- Tang, W.; Wu, J.; Yang, S.; Wang, Q.; Chen, Y. Organizing Pneumonia With Intense 68Ga-FAPI Uptake Mimicking Lung Cancer on 68Ga-FAPI PET/CT. Clin. Nucl. Med. 2022, 47, 223–225. [Google Scholar] [CrossRef]
- Liu, H.; Wang, Y.; Zhang, W.; Cai, L.; Chen, Y. Elevated [(68)Ga]Ga-DOTA-FAPI-04 activity in degenerative osteophyte in a patient with lung cancer. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1671–1672. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Liu, H.; Ou, L.; Jiang, G.; Zhang, C. FAPI Uptake in a Vertebral Body Fracture in a Patient With Lung Cancer: A FAPI Imaging Pitfall. Clin. Nucl. Med. 2021, 46, 520–522. [Google Scholar] [CrossRef] [PubMed]
- Ballal, S.; Yadav, M.P.; Moon, E.S.; Kramer, V.S.; Roesch, F.; Kumari, S.; Bal, C. First-In-Human Results on the Biodistribution, Pharmacokinetics, and Dosimetry of [(177)Lu]Lu-DOTA.SA.FAPi and [(177)Lu]Lu-DOTAGA.(SA.FAPi)(2). Pharmaceuticals 2021, 14, 1212. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Watabe, T.; Kaneda-Nakashima, K.; Shirakami, Y.; Naka, S.; Ooe, K.; Toyoshima, A.; Nagata, K.; Haberkorn, U.; Kratochwil, C.; et al. Fibroblast activation protein targeted therapy using [(177)Lu]FAPI-46 compared with [(225)Ac]FAPI-46 in a pancreatic cancer model. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 871–880. [Google Scholar] [CrossRef]
- Watabe, T.; Liu, Y.; Kaneda-Nakashima, K.; Shirakami, Y.; Lindner, T.; Ooe, K.; Toyoshima, A.; Nagata, K.; Shimosegawa, E.; Haberkorn, U.; et al. Theranostics Targeting Fibroblast Activation Protein in the Tumor Stroma: (64)Cu- and (225)Ac-Labeled FAPI-04 in Pancreatic Cancer Xenograft Mouse Models. J. Nucl. Med. 2020, 61, 563–569. [Google Scholar] [CrossRef]
- Ferdinandus, J.; Costa, P.F.; Kessler, L.; Weber, M.; Hirmas, N.; Kostbade, K.; Bauer, S.; Schuler, M.; Ahrens, M.; Schildhaus, H.U.; et al. Initial Clinical Experience with (90)Y-FAPI-46 Radioligand Therapy for Advanced-Stage Solid Tumors: A Case Series of 9 Patients. J. Nucl. Med. 2022, 63, 727–734. [Google Scholar] [CrossRef]
- Dopper, D.M. Gelabeld FAPI Heeft Grote Potentie als Theranosticum. Available online: https://www.oncologie.nu/nieuws/gelabeld-fapi-heeft-grote-potentie-als-theranosticum/ (accessed on 13 October 2022).
- Kratochwil, C.; Giesel, F.L.; Rathke, H.; Fink, R.; Dendl, K.; Debus, J.; Mier, W.; Jäger, D.; Lindner, T.; Haberkorn, U. [(153)Sm]Samarium-labeled FAPI-46 radioligand therapy in a patient with lung metastases of a sarcoma. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3011–3013. [Google Scholar] [CrossRef]
| n | P/M | SUVmax [68Ga]Ga-FAPI | SUVmax [18F]FDG | TBR [68Ga]Ga-FAPI | TBR [18F]FDG | |
|---|---|---|---|---|---|---|
| Giesel et al. [32] | 8 | M | 6.68 | 11.48 | NR | NR |
| Kratochwil et al. [21] | 25 | P + M | >12 | NR | >7.5 | NR |
| Röhrich et al. [33] | 15 | P | >15 1 | NR | >3.5 1 | NR |
| Wang et al. [14] | 27 | P | 13.7 | 10.4 | 34.2 | 25.9 |
| Hao et al. [34] | 1 | P | 7.64 | 6.03 | NR | NR |
| Shang et al. [35] | 1 | P | 7.7 | 2.7 | NR | NR |
| n | Location of Metastasis | SUVmax [68Ga]Ga-FAPI | SUVmax [18F]FDG | TBR [68Ga]Ga-FAPI | TBR [18F]FDG | |
|---|---|---|---|---|---|---|
| Fu et al. [38] | 1 | brain | 2.3 | 5.9 | higher | lower |
| Li et al. [41] | 17 | brain | 1.56 | 7.34 | 9.53 | 1.01 |
| Wang et al. [14] | 256 1 | lymph | 12.8 | 6.9 | 11.6 | 4.3 |
| 255 1 | distant (total) | 12.9 | 5.8 | 40.5 | 6.2 | |
| 23 1 | brain | 9.0 | 7.4 | 314.4 | 1.0 | |
| 109 1 | bone | 15.6 | 7.0 | 31.3 | 5.0 | |
| 66 1 | pleural | 11.5 | 4.3 | 28.7 | 10.9 | |
| 31 1 | lung | 4.0 | 2.9 | 10.1 | 7.3 | |
| 11 1 | liver | 5.9 | 6.7 | 8.0 | 2.9 | |
| 12 1 | adrenal gland | 15.5 | 8.0 | 17.6 | 5.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borgonje, P.E.; Andrews, L.M.; Herder, G.J.M.; de Klerk, J.M.H. Performance and Prospects of [68Ga]Ga-FAPI PET/CT Scans in Lung Cancer. Cancers 2022, 14, 5566. https://doi.org/10.3390/cancers14225566
Borgonje PE, Andrews LM, Herder GJM, de Klerk JMH. Performance and Prospects of [68Ga]Ga-FAPI PET/CT Scans in Lung Cancer. Cancers. 2022; 14(22):5566. https://doi.org/10.3390/cancers14225566
Chicago/Turabian StyleBorgonje, Paula E., Louise M. Andrews, Gerarda J. M. Herder, and John M. H. de Klerk. 2022. "Performance and Prospects of [68Ga]Ga-FAPI PET/CT Scans in Lung Cancer" Cancers 14, no. 22: 5566. https://doi.org/10.3390/cancers14225566





