Squalamines in Blockade of Tumor-Associated Angiogenesis and Cancer Progression
Abstract
Simple Summary
Abstract
1. Introduction
2. Squalamines for Inhibition of Tumor-Associated Angiogenesis
3. Preclinical Study of Tumor Cell Lines with Squalamine Treatment
4. Clinical Trial Studies with Squalamine
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shah, S.C.; Kayamba, V.; Peek, R.M., Jr.; Heimburger, D. Cancer Control in Low- and Middle-Income Countries: Is It Time to Consider Screening? J. Glob. Oncol. 2019, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, N.; Winer, J.; Burton, T.; Rowland, A.; Siegel, M.; Phillips, H.S.; Terrell, T.; Keller, G.A.; Levinson, A.D. Expression of vascular endothelial growth factor does not promote transformation but confers a growth advantage in vivo to Chinese hamster ovary cells. J. Clin. Investig. 1993, 91, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Folkman, J.; Haudenschild, C. Angiogenesis in vitro. Nature 1980, 288, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Folkman, J.; Shing, Y. Angiogenesis. J. Biol. Chem. 1992, 267, 10931–10934. [Google Scholar] [CrossRef]
- Folkman, J.; Ingber, D. Inhibition of angiogenesis. Semin. Cancer Biol. 1992, 3, 89–96. [Google Scholar] [PubMed]
- Ferrara, N.; Gerber, H.P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef]
- Ellis, L.M.; Hicklin, D.J. VEGF-targeted therapy: Mechanisms of anti-tumour activity. Nat. Rev. Cancer 2008, 8, 579–591. [Google Scholar] [CrossRef]
- Hu, C.J.; Wang, L.Y.; Chodosh, L.A.; Keith, B.; Simon, M.C. Differential roles of hypoxia-inducible factor 1alpha (HIF-1alpha) and HIF-2alpha in hypoxic gene regulation. Mol. Cell. Biol. 2003, 23, 9361–9374. [Google Scholar] [CrossRef]
- Koch, S.; Claesson-Welsh, L. Signal transduction by vascular endothelial growth factor receptors. Cold Spring Harb. Perspect. Med. 2012, 2, a006502. [Google Scholar] [CrossRef]
- Rousseau, S.; Houle, F.; Landry, J.; Huot, J. p38 MAP kinase activation by vascular endothelial growth factor mediates actin reorganization and cell migration in human endothelial cells. Oncogene 1997, 15, 2169–2177. [Google Scholar] [CrossRef]
- Rousseau, S.; Houle, F.; Kotanides, H.; Witte, L.; Waltenberger, J.; Landry, J.; Huot, J. Vascular endothelial growth factor (VEGF)-driven actin-based motility is mediated by VEGFR2 and requires concerted activation of stress-activated protein kinase 2 (SAPK2/p38) and geldanamycin-sensitive phosphorylation of focal adhesion kinase. J. Biol. Chem. 2000, 275, 10661–10672. [Google Scholar] [CrossRef] [PubMed]
- Soker, S.; Fidder, H.; Neufeld, G.; Klagsbrun, M. Characterization of novel vascular endothelial growth factor (VEGF) receptors on tumor cells that bind VEGF165 via its exon 7-encoded domain. J. Biol. Chem. 1996, 271, 5761–5767. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, A.A.; Krigman, H.R.; Whitaker, R.S.; Dodge, R.K.; Rodriguez, G.C. The prognostic significance of angiogenesis in epithelial ovarian carcinoma. Clin. Cancer Res. 1999, 5, 587–591. [Google Scholar]
- Paley, P.J.; Staskus, K.A.; Gebhard, K.; Mohanraj, D.; Twiggs, L.B.; Carson, L.F.; Ramakrishnan, S. Vascular endothelial growth factor expression in early stage ovarian carcinoma. Cancer 1997, 80, 98–106. [Google Scholar] [CrossRef]
- Yamamoto, S.; Konishi, I.; Mandai, M.; Kuroda, H.; Komatsu, T.; Nanbu, K.; Sakahara, H.; Mori, T. Expression of vascular endothelial growth factor (VEGF) in epithelial ovarian neoplasms: Correlation with clinicopathology and patient survival, and analysis of serum VEGF levels. Br. J. Cancer 1997, 76, 1221–1227. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Williams, J.I.; Pietras, R.J. Squalamine and cisplatin block angiogenesis and growth of human ovarian cancer cells with or without HER-2 gene overexpression. Oncogene 2002, 21, 2805–2814. [Google Scholar] [CrossRef] [PubMed]
- Petit, A.M.; Rak, J.; Hung, M.C.; Rockwell, P.; Goldstein, N.; Fendly, B.; Kerbel, R.S. Neutralizing antibodies against epidermal growth factor and ErbB-2/neu receptor tyrosine kinases down-regulate vascular endothelial growth factor production by tumor cells in vitro and in vivo: Angiogenic implications for signal transduction therapy of solid tumors. Am. J. Pathol. 1997, 151, 1523–1530. [Google Scholar]
- Gilmour, L.M.; Macleod, K.G.; McCaig, A.; Sewell, J.M.; Gullick, W.J.; Smyth, J.F.; Langdon, S.P. Neuregulin expression, function, and signaling in human ovarian cancer cells. Clin. Cancer Res. 2002, 8, 3933–3942. [Google Scholar]
- Hellstrom, I.; Goodman, G.; Pullman, J.; Yang, Y.; Hellstrom, K.E. Overexpression of HER-2 in ovarian carcinomas. Cancer Res. 2001, 61, 2420–2423. [Google Scholar]
- Slamon, D.J.; Clark, G.M.; Wong, S.G.; Levin, W.J.; Ullrich, A.; McGuire, W.L. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235, 177–182. [Google Scholar] [CrossRef]
- Slamon, D.J.; Godolphin, W.; Jones, L.A.; Holt, J.A.; Wong, S.G.; Keith, D.E.; Levin, W.J.; Stuart, S.G.; Udove, J.; Ullrich, A.; et al. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 1989, 244, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Wong, Y.F.; Cheung, T.H.; Lam, S.K.; Lu, H.J.; Zhuang, Y.L.; Chan, M.Y.; Chung, T.K. Prevalence and significance of HER-2/neu amplification in epithelial ovarian cancer. Gynecol. Obstet. Investig. 1995, 40, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Folkman, J. Tumor angiogenesis: Therapeutic implications. N. Engl. J. Med. 1971, 285, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Folkman, J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 1996, 86, 353–364. [Google Scholar] [CrossRef]
- Kim, K.J.; Li, B.; Winer, J.; Armanini, M.; Gillett, N.; Phillips, H.S.; Ferrara, N. Inhibition of vascular endothelial growth factor-induced angiogenesis suppresses tumour growth in vivo. Nature 1993, 362, 841–844. [Google Scholar] [CrossRef]
- Hurwitz, H.; Fehrenbacher, L.; Novotny, W.; Cartwright, T.; Hainsworth, J.; Heim, W.; Berlin, J.; Baron, A.; Griffing, S.; Holmgren, E.; et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N. Engl. J. Med. 2004, 350, 2335–2342. [Google Scholar] [CrossRef]
- Abajo, A.; Rodriguez, J.; Bitarte, N.; Zarate, R.; Boni, V.; Ponz, M.; Chopitea, A.; Bandres, E.; Garcia-Foncillas, J. Dose-finding study and pharmacogenomic analysis of fixed-rate infusion of gemcitabine, irinotecan and bevacizumab in pretreated metastatic colorectal cancer patients. Br. J. Cancer 2010, 103, 1529–1535. [Google Scholar] [CrossRef]
- Randall, L.M.; Monk, B.J. Bevacizumab toxicities and their management in ovarian cancer. Gynecol. Oncol. 2010, 117, 497–504. [Google Scholar] [CrossRef]
- von Minckwitz, G.; Untch, M.; Blohmer, J.U.; Costa, S.D.; Eidtmann, H.; Fasching, P.A.; Gerber, B.; Eiermann, W.; Hilfrich, J.; Huober, J.; et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J. Clin. Oncol. 2012, 30, 1796–1804. [Google Scholar] [CrossRef]
- Garcia, J.; Hurwitz, H.I.; Sandler, A.B.; Miles, D.; Coleman, R.L.; Deurloo, R.; Chinot, O.L. Bevacizumab (Avastin(R)) in cancer treatment: A review of 15 years of clinical experience and future outlook. Cancer Treat. Rev. 2020, 86, 102017. [Google Scholar] [CrossRef]
- Oza, A.M.; Dubois, F.; Hegg, R.; Hernandez, C.A.; Finocchiaro, G.; Ghiringhelli, F.; Zamagni, C.; Nick, S.; Irahara, N.; Perretti, T.; et al. A Long-Term Extension Study of Bevacizumab in Patients With Solid Tumors. Oncologist 2021, 26, e2254–e2264. [Google Scholar] [CrossRef] [PubMed]
- Lugano, R.; Ramachandran, M.; Dimberg, A. Tumor angiogenesis: Causes, consequences, challenges and opportunities. Cell Mol. Life Sci. 2020, 77, 1745–1770. [Google Scholar] [CrossRef] [PubMed]
- Dobbin, S.J.H.; Mangion, K.; Berry, C.; Roditi, G.; Basak, S.; Sourbron, S.; White, J.; Venugopal, B.; Touyz, R.M.; Jones, R.J.; et al. Cardiotoxicity and myocardial hypoperfusion associated with anti-vascular endothelial growth factor therapies: Prospective cardiac magnetic resonance imaging in patients with cancer. Eur. J. Heart Fail. 2020, 22, 1276–1277. [Google Scholar] [CrossRef] [PubMed]
- Touyz, R.M.; Herrmann, J. Cardiotoxicity with vascular endothelial growth factor inhibitor therapy. NPJ Precis. Oncol. 2018, 2, 13. [Google Scholar] [CrossRef]
- Gressett, S.M.; Shah, S.R. Intricacies of bevacizumab-induced toxicities and their management. Ann. Pharmacother. 2009, 43, 490–501. [Google Scholar] [CrossRef]
- Chen, W.; Hill, H.; Christie, A.; Kim, M.S.; Holloman, E.; Pavia-Jimenez, A.; Homayoun, F.; Ma, Y.; Patel, N.; Yell, P.; et al. Targeting renal cell carcinoma with a HIF-2 antagonist. Nature 2016, 539, 112–117. [Google Scholar] [CrossRef]
- Saharinen, P.; Eklund, L.; Alitalo, K. Therapeutic targeting of the angiopoietin-TIE pathway. Nat. Rev. Drug Discov. 2017, 16, 635–661. [Google Scholar] [CrossRef]
- Pan, B.; Lentzsch, S. The application and biology of immunomodulatory drugs (IMiDs) in cancer. Pharmacol. Ther. 2012, 136, 56–68. [Google Scholar] [CrossRef]
- Li, Y.L.; Zhao, H.; Ren, X.B. Relationship of VEGF/VEGFR with immune and cancer cells: Staggering or forward? Cancer Biol. Med. 2016, 13, 206–214. [Google Scholar] [CrossRef]
- Yang, J.; Yan, J.; Liu, B. Targeting VEGF/VEGFR to Modulate Antitumor Immunity. Front. Immunol. 2018, 9, 978. [Google Scholar] [CrossRef]
- Fukumura, D.; Kloepper, J.; Amoozgar, Z.; Duda, D.G.; Jain, R.K. Enhancing cancer immunotherapy using antiangiogenics: Opportunities and challenges. Nat. Rev. Clin. Oncol. 2018, 15, 325–340. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Fu, Y.; Xie, Q.; Zhu, B.; Wang, J.; Zhang, B. Anti-angiogenic Agents in Combination With Immune Checkpoint Inhibitors: A Promising Strategy for Cancer Treatment. Front. Immunol. 2020, 11, 1956. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, K.; Nagano, T.; Tachihara, M.; Yamamoto, M.; Nishimura, Y. Interaction between Immunotherapy and Antiangiogenic Therapy for Cancer. Molecules 2020, 25, 3900. [Google Scholar] [CrossRef] [PubMed]
- Bejarano, L.; Jordao, M.J.C.; Joyce, J.A. Therapeutic Targeting of the Tumor Microenvironment. Cancer Discov. 2021, 11, 933–959. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef]
- Dudek, A.Z.; Liu, L.C.; Gupta, S.; Logan, T.F.; Singer, E.A.; Joshi, M.; Zakharia, Y.N.; Lang, J.M.; Schwarz, J.K.; Al-Janadi, A.; et al. Phase Ib/II Clinical Trial of Pembrolizumab With Bevacizumab for Metastatic Renal Cell Carcinoma: BTCRC-GU14-003. J. Clin. Oncol. 2020, 38, 1138–1145. [Google Scholar] [CrossRef]
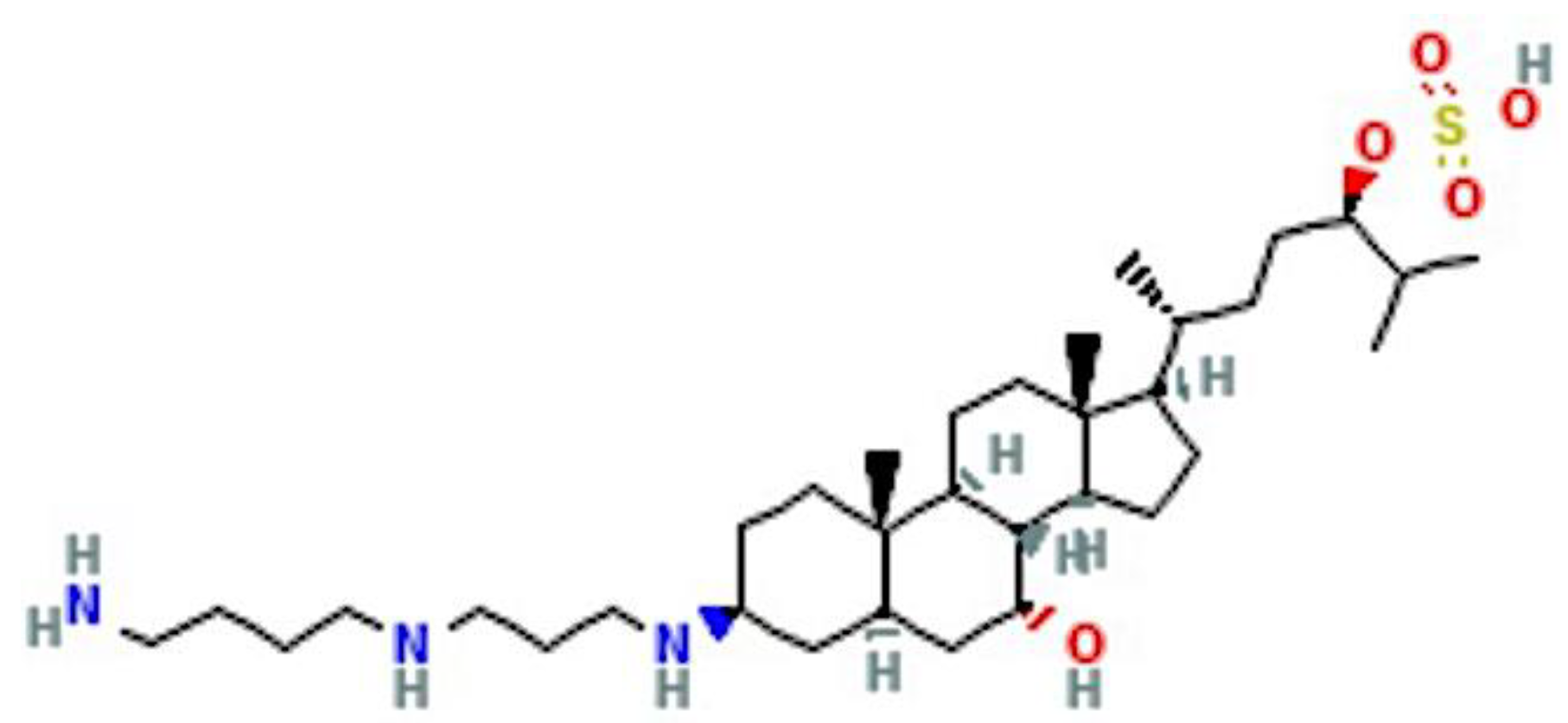
- Mammari, N.; Salles, E.; Beaussart, A.; El-Kirat-Chatel, S.; Varbanov, M. Squalamine and Its Aminosterol Derivatives: Overview of Biological Effects and Mechanisms of Action of Compounds with Multiple Therapeutic Applications. Microorganisms 2022, 10, 1205. [Google Scholar] [CrossRef]
- Zasloff, M.; Adams, A.P.; Beckerman, B.; Campbell, A.; Han, Z.; Luijten, E.; Meza, I.; Julander, J.; Mishra, A.; Qu, W.; et al. Squalamine as a broad-spectrum systemic antiviral agent with therapeutic potential. Proc. Natl. Acad. Sci. USA 2011, 108, 15978–15983. [Google Scholar] [CrossRef]
- Yun, S.S.; Li, W. Identification of squalamine in the plasma membrane of white blood cells in the sea lamprey, Petromyzon marinus. J. Lipid Res. 2007, 48, 2579–2586. [Google Scholar] [CrossRef]
- Teicher, B.A.; Williams, J.I.; Takeuchi, H.; Ara, G.; Herbst, R.S.; Buxton, D. Potential of the aminosterol, squalamine in combination therapy in the rat 13,762 mammary carcinoma and the murine Lewis lung carcinoma. Anticancer Res. 1998, 18, 2567–2573. [Google Scholar]
- Eckhardt, S.G. Angiogenesis inhibitors as cancer therapy. Hosp. Pract. 1999, 34, 63–84. [Google Scholar] [CrossRef] [PubMed]
- Sills, A.K., Jr.; Williams, J.I.; Tyler, B.M.; Epstein, D.S.; Sipos, E.P.; Davis, J.D.; McLane, M.P.; Pitchford, S.; Cheshire, K.; Gannon, F.H.; et al. Squalamine inhibits angiogenesis and solid tumor growth in vivo and perturbs embryonic vasculature. Cancer Res. 1998, 58, 2784–2792. [Google Scholar] [PubMed]
- Moore, K.S.; Wehrli, S.; Roder, H.; Rogers, M.; Forrest, J.N., Jr.; McCrimmon, D.; Zasloff, M. Squalamine: An aminosterol antibiotic from the shark. Proc. Natl. Acad. Sci. USA 1993, 90, 1354–1358. [Google Scholar] [CrossRef] [PubMed]
- Higgins, R.D.; Sanders, R.J.; Yan, Y.; Zasloff, M.; Williams, J.I. Squalamine improves retinal neovascularization. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1507–1512. [Google Scholar]
- Genaidy, M.; Kazi, A.A.; Peyman, G.A.; Passos-Machado, E.; Farahat, H.G.; Williams, J.I.; Holroyd, K.J.; Blake, D.A. Effect of squalamine on iris neovascularization in monkeys. Retina 2002, 22, 772–778. [Google Scholar] [CrossRef]
- Wroblewski, J.J.; Hu, A.Y. Topical Squalamine 0.2% and Intravitreal Ranibizumab 0.5 mg as Combination Therapy for Macular Edema Due to Branch and Central Retinal Vein Occlusion: An Open-Label, Randomized Study. Ophthalmic. Surg. Lasers Imaging Retina 2016, 47, 914–923. [Google Scholar] [CrossRef]
- Akhter, S.; Nath, S.K.; Tse, C.M.; Williams, J.; Zasloff, M.; Donowitz, M. Squalamine, a novel cationic steroid, specifically inhibits the brush-border Na+/H+ exchanger isoform NHE3. Am. J. Physiol. 1999, 276, C136–C144. [Google Scholar] [CrossRef]
- Williams, J.I.; Weitman, S.; Gonzalez, C.M.; Jundt, C.H.; Marty, J.; Stringer, S.D.; Holroyd, K.J.; McLane, M.P.; Chen, Q.; Zasloff, M.; et al. Squalamine treatment of human tumors in nu/nu mice enhances platinum-based chemotherapies. Clin. Cancer Res. 2001, 7, 724–733. [Google Scholar]
- Herbst, R.S.; Hammond, L.A.; Carbone, D.P.; Tran, H.T.; Holroyd, K.J.; Desai, A.; Williams, J.I.; Bekele, B.N.; Hait, H.; Allgood, V.; et al. A phase I/IIA trial of continuous five-day infusion of squalamine lactate (MSI-1256F) plus carboplatin and paclitaxel in patients with advanced non-small cell lung cancer. Clin. Cancer Res. 2003, 9, 4108–4115. [Google Scholar]
- Marquez-Garban, D.C.; Gorrin-Rivas, M.; Chen, H.W.; Sterling, C., Jr.; Elashoff, D.; Hamilton, N.; Pietras, R.J. Squalamine blocks tumor-associated angiogenesis and growth of human breast cancer cells with or without HER-2/neu overexpression. Cancer Lett. 2019, 449, 66–75. [Google Scholar] [CrossRef]
- Kinney, W.A.; Zhang, X.; Williams, J.I.; Johnston, S.; Michalak, R.S.; Deshpande, M.; Dostal, L.; Rosazza, J.P. A short formal synthesis of squalamine from a microbial metabolite. Org. Lett. 2000, 2, 2921–2922. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.H.; Cai, F.; Zhou, X.D.; Zhou, W.S. A concise and stereoselective synthesis of squalamine. Org. Lett. 2003, 5, 3257–3259. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Zheng, Y.; Yang, B.; Zhong, J.; Shi, H. Study on synthesis of key squalamine intermediate 7alpha, 24R-dihydroxy-5alpha-cholestan-3-one. Steroids 2019, 151, 108472. [Google Scholar] [CrossRef]
- Limbocker, R.; Staats, R.; Chia, S.; Ruggeri, F.S.; Mannini, B.; Xu, C.K.; Perni, M.; Cascella, R.; Bigi, A.; Sasser, L.R.; et al. Squalamine and Its Derivatives Modulate the Aggregation of Amyloid-beta and alpha-Synuclein and Suppress the Toxicity of Their Oligomers. Front. Neurosci. 2021, 15, 680026. [Google Scholar] [CrossRef]
- Rao, M.N.; Shinnar, A.E.; Noecker, L.A.; Chao, T.L.; Feibush, B.; Snyder, B.; Sharkansky, I.; Sarkahian, A.; Zhang, X.; Jones, S.R.; et al. Aminosterols from the dogfish shark Squalus acanthias. J. Nat. Prod. 2000, 63, 631–635. [Google Scholar] [CrossRef]
- Williams, J. A New Angiostatic Steroid. In Antiangiogenic Agents in Cancer Therapy; Humana Press: Totowa, NJ, USA, 1999. [Google Scholar]
- Chen, Q.; Williams, J.; Anderson, M.; Kinney, W.; Zasloff, M. The angiostatic sterol squalamine is a calmodulin chaperone. Clin. Cancer Res. 1999, 5, 3768s. [Google Scholar]
- Schiller, J.H.; Bittner, G. Potentiation of platinum antitumor effects in human lung tumor xenografts by the angiogenesis inhibitor squalamine: Effects on tumor neovascularization. Clin. Cancer Res. 1999, 5, 4287–4294. [Google Scholar] [PubMed]
- Mauceri, H.J.; Hanna, N.N.; Beckett, M.A.; Gorski, D.H.; Staba, M.J.; Stellato, K.A.; Bigelow, K.; Heimann, R.; Gately, S.; Dhanabal, M.; et al. Combined effects of angiostatin and ionizing radiation in antitumour therapy. Nature 1998, 394, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Pietras, R.J.; Weinberg, O.K. Antiangiogenic Steroids in Human Cancer Therapy. Evid. Based Complement. Altern. Med. 2005, 2, 49–57. [Google Scholar] [CrossRef]
- Williams, J.; Mangold, G.; Zasloff, M.; von Hoff, D. Evaluation of the natural aminosterol squalamine as adjunctive chemotherapy in the MX-1 breast cancer xenograft model. Breast Cancer Res. Treat. 1997, 46, 40. [Google Scholar]
- Pegram, M.D.; Konecny, G.E.; O’Callaghan, C.; Beryt, M.; Pietras, R.; Slamon, D.J. Rational combinations of trastuzumab with chemotherapeutic drugs used in the treatment of breast cancer. J. Natl. Cancer Inst. 2004, 96, 739–749. [Google Scholar] [CrossRef] [PubMed]
- Pietras, R.J.; Pegram, M.D.; Finn, R.S.; Maneval, D.A.; Slamon, D.J. Remission of human breast cancer xenografts on therapy with humanized monoclonal antibody to HER-2 receptor and DNA-reactive drugs. Oncogene 1998, 17, 2235–2249. [Google Scholar] [CrossRef] [PubMed]
- DeVita, V.; Lawrence, T.; Rosenberg, S. Cancer: Principles and Practice of Oncology Vols 1 and 2; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- DiSaia, P.J.; Bloss, J.D. Treatment of ovarian cancer: New strategies. Gynecol. Oncol. 2003, 90, S24–S32. [Google Scholar] [CrossRef]
- Ozols, R.F. Paclitaxel plus carboplatin in the treatment of ovarian cancer. Semin. Oncol. 1999, 26, 84–89. [Google Scholar] [PubMed]
- Stiff, P. The challenge of treating advanced ovarian cancer. Cancer Mgmt. 1997, 2, 5. [Google Scholar]
- Keck, P.J.; Hauser, S.D.; Krivi, G.; Sanzo, K.; Warren, T.; Feder, J.; Connolly, D.T. Vascular permeability factor, an endothelial cell mitogen related to PDGF. Science 1989, 246, 1309–1312. [Google Scholar] [CrossRef]
- Lewis, G.D.; Figari, I.; Fendly, B.; Wong, W.L.; Carter, P.; Gorman, C.; Shepard, H.M. Differential responses of human tumor cell lines to anti-p185HER2 monoclonal antibodies. Cancer Immunol. Immunother. 1993, 37, 255–263. [Google Scholar] [CrossRef]
- Zebrowski, B.K.; Liu, W.; Ramirez, K.; Akagi, Y.; Mills, G.B.; Ellis, L.M. Markedly elevated levels of vascular endothelial growth factor in malignant ascites. Ann. Surg. Oncol. 1999, 6, 373–378. [Google Scholar] [CrossRef]
- Pietras, R.J.; Gorrin-Rivas, M.; Chen, H.W. Squalamine blocks tumorassociated angiogenesis and growth of ovarian cancer. Int. J. Obstet. Gynecol. 2003, 83, 59–60. [Google Scholar]
- Joseph, I.B.; Isaacs, J.T. Potentiation of the antiangiogenic ability of linomide by androgen ablation involves down-regulation of vascular endothelial growth factor in human androgen-responsive prostatic cancers. Cancer Res. 1997, 57, 1054–1057. [Google Scholar]
- Sokoloff, M.H.; Rinker-Schaeffer, C.W.; Chung, L.W.; Brendler, C.B. Adjunctive therapy for men with high risk localized and locally advanced prostate cancer: Targeting disseminated tumor cells. J. Urol. 2004, 172, 2539–2544. [Google Scholar] [CrossRef] [PubMed]
- Matsushima, H.; Goto, T.; Hosaka, Y.; Kitamura, T.; Kawabe, K. Correlation between proliferation, apoptosis, and angiogenesis in prostate carcinoma and their relation to androgen ablation. Cancer 1999, 85, 1822–1827. [Google Scholar] [CrossRef]
- Sokoloff, M.H.; Bradley, M.J.m.; Zhau, H.E.; Simons, J.W.; Chung, L.W. VEGF inhibits human prostate cancer growth and potentiates anti-angiogenesis therapy. J. Urol. 1999, 161, 53. [Google Scholar] [CrossRef]
- Shibuya, M. Vascular endothelial growth factor receptor-1 (VEGFR-1/Flt-1): A dual regulator for angiogenesis. Angiogenesis 2006, 9, 225–230, discussion 231. [Google Scholar] [CrossRef]
- Sokoloff, M.H.; Bradley, M.J.m.; Zhau, H.E.; Williams, J.; Chung, L.W. Squalamine downregulates integrin alpha gamma beta 3 expression and obliterates advanced human prostate cancer: A preclinical study. J. Urol. 1999, 161, 298. [Google Scholar] [CrossRef]
- Pietras, R.J. Biologic basis of sequential and combination therapies for hormone-responsive breast cancer. Oncologist 2006, 11, 704–717. [Google Scholar] [CrossRef] [PubMed]
- Carmona, S.; Brunel, J.M.; Bonier, R.; Sbarra, V.; Robert, S.; Borentain, P.; Lombardo, D.; Mas, E.; Gerolami, R. A squalamine derivative, NV669, as a novel PTP1B inhibitor: In vitro and in vivo effects on pancreatic and hepatic tumor growth. Oncotarget 2019, 10, 6651–6667. [Google Scholar] [CrossRef]
- Shu, Y.; Jones, S.R.; Kinney, W.A.; Selinsky, B.S. The synthesis of spermine analogs of the shark aminosterol squalamine. Steroids 2002, 67, 291–304. [Google Scholar] [CrossRef]
- Brunel, J.M.; Salmi, C.; Loncle, C.; Vidal, N.; Letourneux, Y. Squalamine: A polyvalent drug of the future? Curr. Cancer Drug Targets 2005, 5, 267–272. [Google Scholar] [CrossRef]
- Bhargava, P.; Marshall, J.L.; Dahut, W.; Rizvi, N.; Trocky, N.; Williams, J.I.; Hait, H.; Song, S.; Holroyd, K.J.; Hawkins, M.J. A phase I and pharmacokinetic study of squalamine, a novel antiangiogenic agent, in patients with advanced cancers. Clin. Cancer Res. 2001, 7, 3912–3919. [Google Scholar]
- Hao, D.; Hammond, L.A.; Eckhardt, S.G.; Patnaik, A.; Takimoto, C.H.; Schwartz, G.H.; Goetz, A.D.; Tolcher, A.W.; McCreery, H.A.; Mamun, K.; et al. A Phase I and pharmacokinetic study of squalamine, an aminosterol angiogenesis inhibitor. Clin. Cancer Res. 2003, 9, 2465–2471. [Google Scholar] [PubMed]
- Johnson, D.H.; Paul, D.M.; Hande, K.R.; DeVore, R. Paclitaxel plus carboplatin in the treatment of patients with advanced lung cancer: A Vanderbilt University Cancer Center phase II trial (LUN-46). Semin. Oncol. 1996, 23, 42–46. [Google Scholar] [PubMed]
- Davidson, S.; Chap, L.; Pietras, R.J.; Astrow, A.; Gajewski, W.; Brader, F.; Petrone, M.; Desai, A.; Solomon, S.; Holroyd, K.J. A phase IIA trial of continuous 5-day infusions of MSI-1256F (squalamine lactate) plus carboplatin for therapy of persistant or recurrent advanced ovarian cancer. Proc. Am. Soc. Clin. Oncol. 2002, 9, 2465–2471. [Google Scholar]
| * Development | Reference |
|---|---|
| Squalamine specifically inhibits cell surface sodium-proton transporter in fibroblast and ileum models in vitro | Akhter et al., 1999 [57] |
| (a) Squalamine disrupts F-actin filament organization and down-regulates expression of E-cadherin in preclinical models (b) Squalamine in combination with cisplatin increases response to chemotherapy in human lung tumors in nude mice. | Williams et al., 2001 [58] |
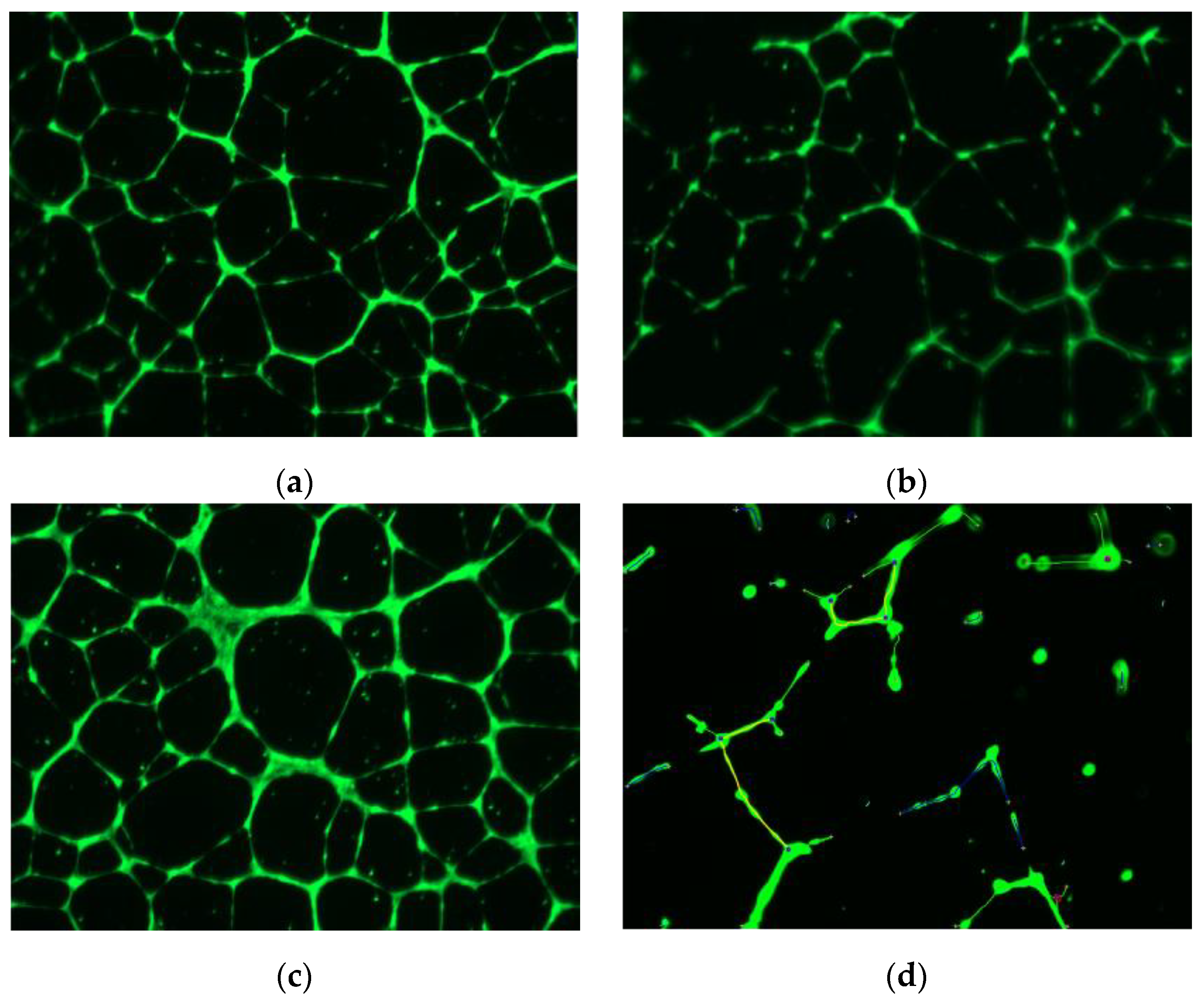
| (a) Squalamine inhibits VEGF-induced MAPK activation in HUVEC cells. (b) Combination of squalamine with cisplatin blocks growth of human ovarian cancer xenografts with or without HER-2 gene overexpression by inhibition of angiogenesis. | Li et al., 2002 [16] |
| Phase I/II clinical trial of 5-day infusion of squalamine lactate (MSI-1256F) in combination with paclitaxel and carboplatin in patients with advanced stage NSCLC, ORR was 28%, with stable disease in 19%. | Herbst et al., 2003 [59] |
| (a) Squalamine inhibits endothelial tube-like formation induced by VEGF in HUVEC cells that is mediated by FAK. (b) Squalamine blocks progression of human breast cancer xenografts with or without HER-2 overexpression by inhibiting angiogenesis. | Márquez-Garbán et al. 2019 [60] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sterling, C., Jr.; Márquez-Garbán, D.; Vadgama, J.V.; Pietras, R.J. Squalamines in Blockade of Tumor-Associated Angiogenesis and Cancer Progression. Cancers 2022, 14, 5154. https://doi.org/10.3390/cancers14205154
Sterling C Jr., Márquez-Garbán D, Vadgama JV, Pietras RJ. Squalamines in Blockade of Tumor-Associated Angiogenesis and Cancer Progression. Cancers. 2022; 14(20):5154. https://doi.org/10.3390/cancers14205154
Chicago/Turabian StyleSterling, Colin, Jr., Diana Márquez-Garbán, Jaydutt V. Vadgama, and Richard J. Pietras. 2022. "Squalamines in Blockade of Tumor-Associated Angiogenesis and Cancer Progression" Cancers 14, no. 20: 5154. https://doi.org/10.3390/cancers14205154
APA StyleSterling, C., Jr., Márquez-Garbán, D., Vadgama, J. V., & Pietras, R. J. (2022). Squalamines in Blockade of Tumor-Associated Angiogenesis and Cancer Progression. Cancers, 14(20), 5154. https://doi.org/10.3390/cancers14205154





