Effect of Autotransfusion in HCC Surgery on Survival and Recurrence: A Systematic Review and Meta-Analysis
Abstract
Simple Summary
Abstract
1. Introduction
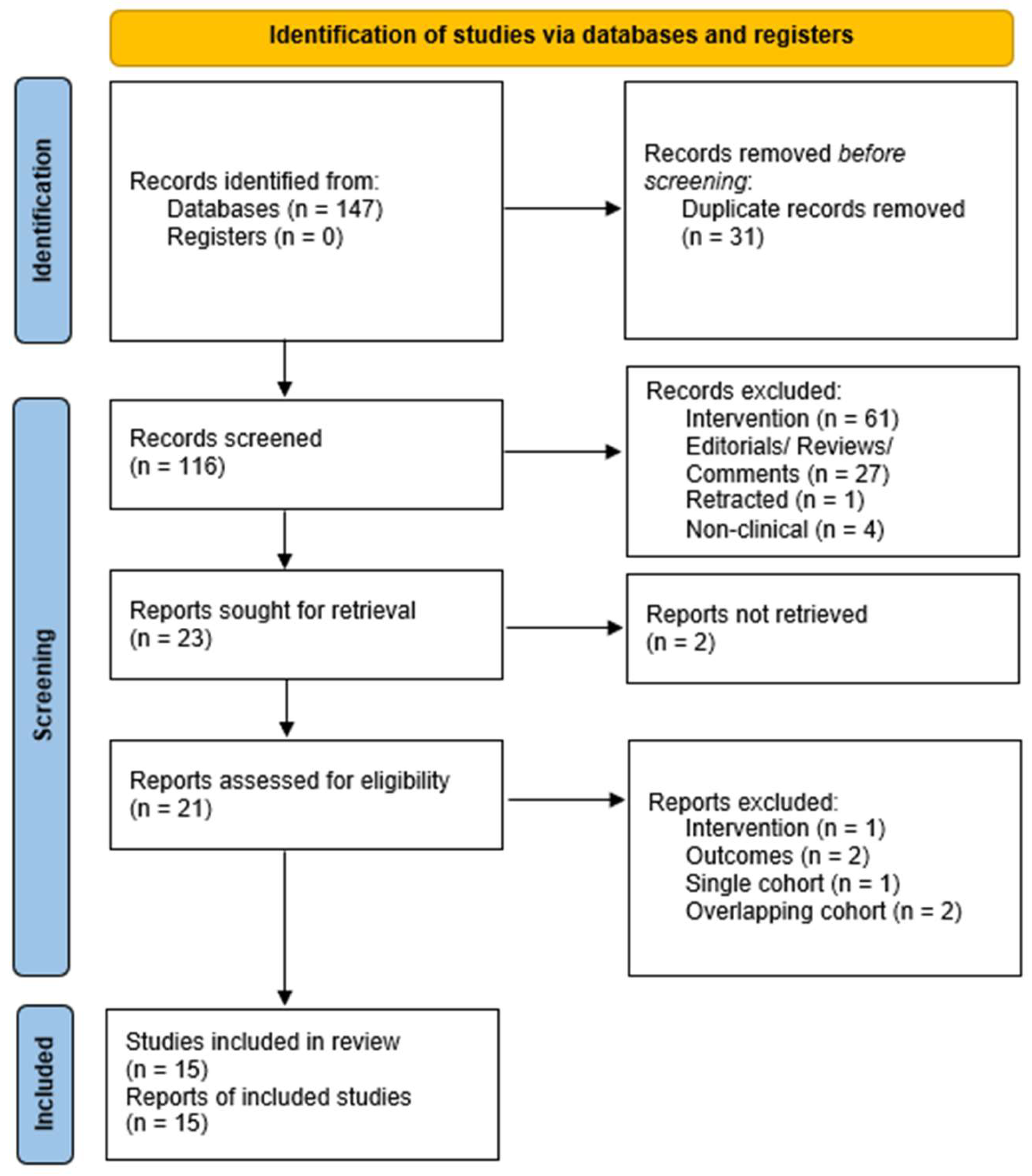
2. Materials and Methods
- Population: patients undergoing liver surgery for HCC
- Intervention: autologous transfusion (including intraoperative blood salvage)
- Comparison: no autologous transfusion
- Outcomes: recurrence, disease-free survival and overall survival
- Studies: comparative studies irrespective on methodology
3. Results
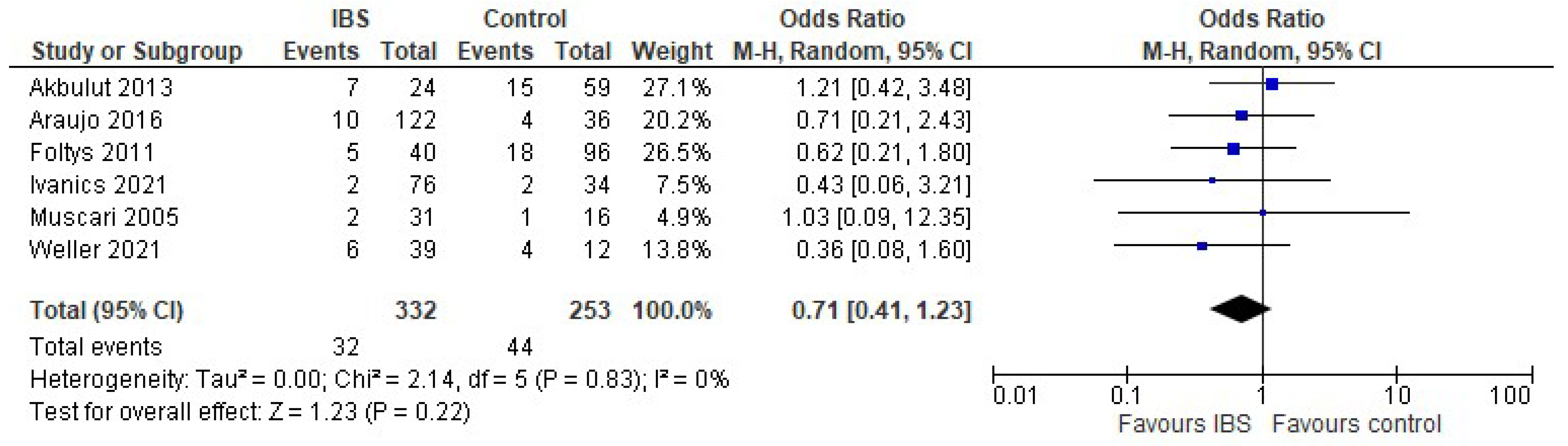
3.1. Autotransfusion in Liver Transplantation
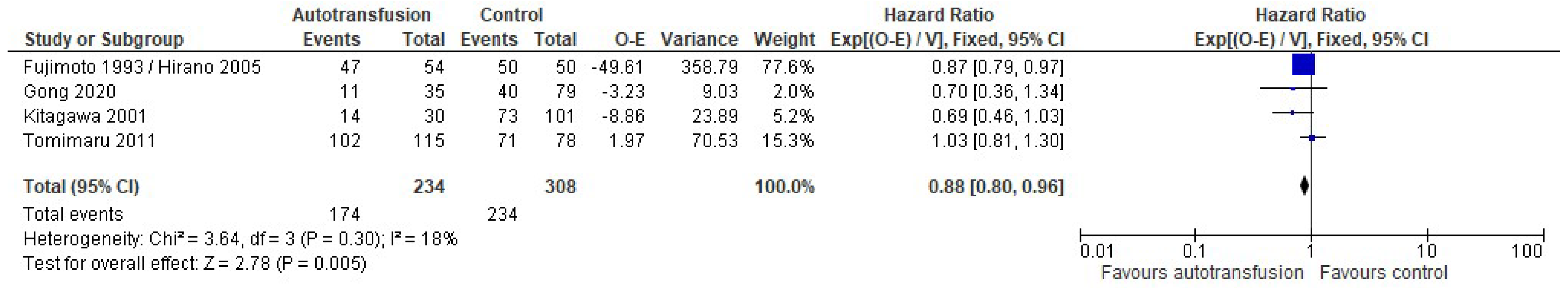
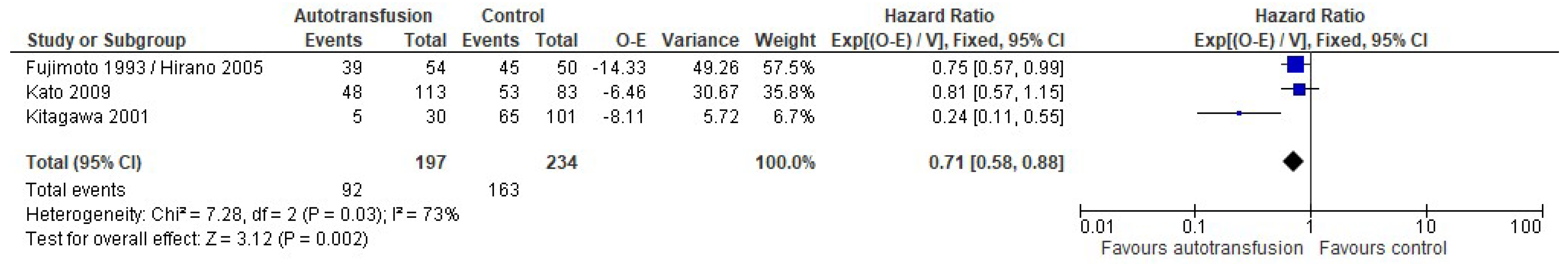
3.2. Autotransfusion in Hepatectomy
3.3. Risk of Bias and Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Llovet, J.M.; Kelley, R.K.; Villanueva, A.; Singal, A.G.; Pikarsky, E.; Roayaie, S.; Lencioni, R.; Koike, K.; Zucman-Rossi, J.; Finn, R.S. Hepatocellular carcinoma. Nat. Rev. Dis. Primers 2021, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Esteban, J.P.G.; Asgharpour, A. Evaluation of liver transplant candidates with non-alcoholic steatohepatitis. Transl. Gastroenterol. Hepatol. 2022, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Lai, E.C.; Lau, W.Y. The continuing challenge of hepatic cancer in Asia. Surgeon 2005, 3, 210–215. [Google Scholar] [CrossRef]
- Baumgartner, R.; Gilg, S.; Björnsson, B.; Hasselgren, K.; Ghorbani, P.; Sauter, C.; Stål, P.; Sandstöm, P.; Sparrelid, E.; Engstrand, J. Impact of post-hepatectomy liver failure on morbidity and short- and long-term survival after major hepatectomy. BJS Open 2022, 6, zrac097. [Google Scholar] [CrossRef]
- Pinto, M.A.; Grezzana-Filho, T.J.M.; Chedid, A.D.; Leipnitz, I.; Prediger, J.E.; Alvares-Da-Silva, M.R.; de Araújo, A.; Zahler, S.; Lopes, B.B.; Giampaoli, Z.D.; et al. Impact of intraoperative blood salvage and autologous transfusion during liver transplantation for hepatocellular carcinoma. Langenbecks Arch. Surg. 2021, 406, 67–74. [Google Scholar] [CrossRef]
- Aguilar-Nascimento, J.E.; Zampieri-Filho, J.P.; Bordin, J.O. Implications of perioperative allogeneic red blood cell transfusion on the immune-inflammatory response. Hematol. Transfus. Cell. Ther. 2021, 43, 58–64. [Google Scholar] [CrossRef]
- Gammon, R.; Katz, L.M.; Strauss, D.; Rowe, K.; Menitove, J.; Benjamin, R.J.; Goel, R.; Borge, D.; Reichenberg, S.; Smith, R.; et al. Beyond COVID-19 and lessons learned in the United States. Transfus. Med. 2022, in press. [Google Scholar] [CrossRef]
- Han, S.; Kim, G.; Ko, J.S.; Sinn, D.H.; Yang, J.D.; Joh, J.-W.; Lee, S.-K.; Gwak, M.S. Safety of the Use of Blood Salvage and Autotransfusion During Liver Transplantation for Hepatocellular Carcinoma. Ann. Surg. 2016, 264, 339–343. [Google Scholar] [CrossRef]
- Gong, Y.; Tang, Y.; Xue, Y.; Chen, L. Impact of intraoperative allogenic and autologous transfusion on immune function and prognosis in patients with hepatocellular carcinoma. Medicine 2020, 99, e22568. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- Kalkum, E.; Klotz, R.; Seide, S.; Hüttner, F.J.; Kowalewski, K.-F.; Nickel, F.; Khajeh, E.; Knebel, P.; Diener, M.K.; Probst, P. Systematic Reviews in Surgery—Recommendations from the Study Center of the German Society of Surgery. Langenbeck’s Arch. Surg. 2021, 406, 1723–1731. [Google Scholar] [CrossRef] [PubMed]
- Tierney, J.F.; Stewart, L.A.; Ghersi, D.; Burdett, S.; Sydes, M.R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Foroutan, F.; Guyatt, G.; Zuk, V.; Vandvik, P.O.; Alba, A.C.; Mustafa, R.; Vernooij, R.; Arevalo-Rodriguez, I.; Munn, Z.; Roshanov, P.; et al. GRADE Guidelines 28: Use of GRADE for the assessment of evidence about prognostic factors: Rating certainty in identification of groups of patients with different absolute risks. J. Clin. Epidemiol. 2020, 121, 62–70. [Google Scholar] [CrossRef]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) Grade Handbook for Grading Quality of Evidence and Strength of Recommendations. Updated October 2013. The GRADE Working Group. 2013. Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 10 September 2022).
- Akbulut, S. Effect of autotransfusion system on tumor recurrence and survival in hepatocellular carcinoma patients. World J. Gastroenterol. 2013, 19, 1625–1631. [Google Scholar] [CrossRef]
- Araujo, R.L.; Pantanali, C.A.; Haddad, L.; Rocha Filho, J.A.; D’Albuquerque, L.A.C.; Andraus, W. Does autologous blood transfusion during liver transplantation for hepatocellular carcinoma increase risk of recurrence? World J. Gastrointest. Surg. 2016, 8, 161–168. [Google Scholar] [CrossRef]
- Foltys, D.; Zimmermann, T.; Heise, M.; Kaths, M.; Lautem, A.; Wisser, G.; Weiler, N.; Hoppe-Lotichius, M.; Hansen, T.; Otto, G. Liver Transplantation for Hepatocellular Carcinoma—Is There a Risk of Recurrence Caused by Intraoperative Blood Salvage Autotransfusion? Eur. Surg. Res. 2011, 47, 182–187. [Google Scholar] [CrossRef]
- Fujimoto, J.; Okamoto, E.; Yamanaka, N.; Oriyama, T.; Furukawa, K.; Kawamura, E.; Tanaka, T.; Tomoda, F. Efficacy of autotransfusion in hepatectomy for hepatocellular carcinoma. Arch. Surg. 1993, 128, 1065–1069. [Google Scholar] [CrossRef]
- Hirano, T.; Yamanaka, J.; Iimuro, Y.; Fujimoto, J. Long-term safety of autotransfusion during hepatectomy for hepatocellular carcinoma. Surg. Today 2005, 35, 1042–1046. [Google Scholar] [CrossRef]
- Ivanics, T.; Shubert, C.R.; Muaddi, H.; Claasen, M.P.A.W.; Yoon, P.; Hansen, B.E.; McCluskey, S.A.; Sapisochin, G. Blood Cell Salvage and Autotransfusion Does Not Worsen Oncologic Outcomes Following Liver Transplantation with Incidental Hepatocellular Carcinoma: A Propensity Score-Matched Analysis. Ann. Surg. Oncol. 2021, 28, 6816–6825. [Google Scholar] [CrossRef]
- Kato, K.; Nomoto, S.; Sugimoto, H.; Kanazumi, N.; Takeda, S.; Nakao, A. Autologous blood storage before hepatectomy for hepatocellular carcinoma. Hepatogastroenterology 2009, 56, 802–807. [Google Scholar]
- Kitagawa, K.; Taniguchi, H.; Mugitani, T.; Koh, T.; Obayashi, T.; Kunishima, S.; Yamaguchi, A.; Yamagishi, H. Safety and advantage of perioperative autologous blood transfusion in hepatic resection for hepatocellular carcinoma. Anticancer Res. 2001, 21, 3663–3667. [Google Scholar]
- Muscari, F.; Suc, B.; Vigouroux, D.; Duffas, J.P.; Migueres, I.; Mathieu, A.; Lavayssiere, L.; Rostaing, L.; Fourtanier, G. Blood salvage autotransfusion during transplantation for hepatocarcinoma: Does it increase the risk of neoplastic recurrence? Transpl. Int. 2005, 18, 1236–1239. [Google Scholar] [CrossRef]
- Nutu, O.A.; Sneiders, D.; Mirza, D.; Isaac, J.; Perera, M.T.P.; Hartog, H. Safety of intra-operative blood salvage during liver transplantation in patients with hepatocellular carcinoma, a propensity score-matched survival analysis. Transpl. Int. 2021, 34, 2887–2894. [Google Scholar] [CrossRef]
- Tomimaru, Y.; Eguchi, H.; Marubashi, S.; Wada, H.; Kobayashi, S.; Tanemura, M.; Umeshita, K.; Doki, Y.; Mori, M.; Nagano, H. Advantage of autologous blood transfusion in surgery for hepatocellular carcinoma. World J. Gastroenterol. 2011, 17, 3709–3715. [Google Scholar] [CrossRef]
- Weller, A.; Seyfried, T.; Ahrens, N.; Baier-Kleinhenz, L.; Schlitt, H.-J.; Peschel, G.; Graf, B.M.; Sinner, B. Cell Salvage During Liver Transplantation for Hepatocellular Carcinoma: A Retrospective Analysis of Tumor Recurrence Following Irradiation of the Salvaged Blood. Transplant. Proc. 2021, 53, 1639–1644. [Google Scholar] [CrossRef]
- Hao, S.; Chen, S.; Tu, C.; Huang, T. Anterior Approach to Improve the Prognosis in HCC Patients Via Decreasing Dissemination of EpCAM(+) Circulating Tumor Cells. J. Gastrointest. Surg. 2017, 21, 1112–1120. [Google Scholar] [CrossRef]
- Sasaki, S.; Nomura, Y.; Sudo, T.; Sakai, H.; Hisaka, T.; Akiba, J.; Nakashima, O.; Yano, H.; Kage, M.; Akagi, Y. Hematogenous Dissemination of Tumor Cells in Hepatocellular Carcinoma: Comparing Anterior and Non-anterior Approach Hepatectomy. Anticancer Res. 2022, 42, 4129–4137. [Google Scholar] [CrossRef]
- Ahn, D.W.; Shim, J.H.; Yoon, J.-H.; Kim, C.Y.; Lee, H.-S.; Kim, Y.T.; Kim, Y.J. Treatment and clinical outcome of needle-track seeding from hepatocellular carcinoma. Korean J. Hepatol. 2011, 17, 106–112. [Google Scholar] [CrossRef]
- Mu, X.M.; Wang, W.; Jiang, Y.-Y.; Feng, J. Patterns of Comorbidity in Hepatocellular Carcinoma: A Network Perspective. Int. J. Environ. Res. Public Health 2020, 17, 3108. [Google Scholar] [CrossRef]



| Study | Country | Population | Design | Intervention | Control |
|---|---|---|---|---|---|
| Akbulut 2013 [17] | Turkey | Liver transplantation Living and deceased donors | Retrospective | IBS | no IBS |
| Araujo 2016 [18] | Brazil | Liver transplantation | Retrospective | IBS | no IBS |
| Foltys 2011 [19] | Germany | Liver transplantation | Retrospective | IBS | no IBS |
| Han 2016 [8] | Korea | Liver transplantation Living donors | Retrospective, propensity score matched | IBS, leucocyte depletion | no IBS |
| Ivanics 2021 [22] | Canada | Liver transplantation Living and deceased donors | Retrospective | IBS | no IBS |
| Muscari 2005 [25] | France | Liver transplantation Deceased donor | Prospective | IBS | no IBS |
| Nutu 2021 [26] | UK | Liver transplantation Deceased donor | Retrospective, propensity score matched | IBS | no IBS |
| Pinto 2021 [5] | Brazil | Liver transplantation Deceased donor | Retrospective | IBS | no IBS |
| Weller 2021 [28] | Germany | Liver transplantation | Retrospective | IBS ± irradiation | no IBS |
| Fujimoto 1993/Hirano 2005 [20,21] | Japan | Hepatectomy | Prospective | Autotransfusion after preoperative phlebotomy + IBS | no IBS |
| Gong 2020 [9] | China | Hepatectomy | Prospective | Autotransfusion after preoperative phlebotomy | Allogeneic transfusions |
| Kato 2009 [23] | Japan | Hepatectomy | Prospective | Autotransfusion after preoperative phlebotomy + rh-EPO | no autotransfusion |
| Kitagawa 2001 [24] | Japan | Hepatectomy | Prospective | Autotransfusion after preoperative phlebotomy | no autotransfusion (allogeneic or no transfusion) |
| Tomimaru 2011 [27] | Japan | Hepatectomy | Prospective | Autotransfusion after preoperative phlebotomy + rh-EPO | no transfusion |
| Characteristic | IBS (n = 803) | no IBS (n = 511) | Significance (p =) |
|---|---|---|---|
| Age (years) [mean ± SD] | 55.8 ± 6.6 | 55.7 ± 6.2 | 0.82 |
| Gender (m/f) | 535/141 | 311/71 | 0.38 |
| BMI [mean ± SD] | 28.0 ± 4.25 | 27.3 ± 3.67 | 0.02 |
| - Liver disease | 0.08 | ||
| - Alcohol-associated | 70 | 70 | |
| - Metabolic-associated | 30 | 14 | |
| - Hepatitis | 326 | 221 | |
| - Genetic | 2 | 3 | |
| - Child-Pugh-Turcott | <0.001 | ||
| - A | 37 | 78 | |
| - B | 50 | 70 | |
| - C | 84 | 56 | |
| MELD [mean ± SD] | 13.1 ± 5.3 | 12.6 ± 3.9 | 0.31 |
| HCC diameter | 3.8 ± 1.5 | 4.1 ± 1.5 | 0.07 |
| - Grading | 0.47 | ||
| - Well differentiated | 50 | 58 | |
| - Moderately differentiated | 134 | 123 | |
| - Poorly differentiated | 16 | 20 | |
| Vascular invasion | |||
| - Donor | 0.68 | ||
| - Diseased donors | 338 | 264 | |
| - Living donors | 201 | 166 |
| Characteristic | Autotransfusion (n = 347) | No Autotransfusion (n = 391) | Significance |
|---|---|---|---|
| Age (years) [mean ± SD] | 58.7 ± 5.5 | 57.8 ± 4.1 | 0.01 |
| Gender (m/f) | 234/48 | 167/44 | 0.28 |
| - Cirrhosis | 0.08 | ||
| - Present | 88 | 176 | |
| - Absent | 144 | 215 | |
| Child-Pugh-Turcott | <0.001 | ||
| - A | 199 | 142 | |
| - B/C | 64 | 97 | |
| HCC tumor | 0.14 | ||
| - Solitary | 154 | 120 | |
| - Multiple | 74 | 41 | |
| Vascular invasion | 134 | 132 | 0.36 |
| Intraoperative blood loss | 1212 ± 998 | 2056 ± 2123 | <0.001 |
| Bias Due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Results | Overall | |
|---|---|---|---|---|---|---|---|---|
| Akbulut 2013 [17] | ! | ? | + | + | ? | ? | + | + |
| Araujo 2016 [18] | + | ? | + | + | + | + | + | + |
| Foltys 2011 [19] | ! | ! | + | ? | + | + | + | ? |
| Han 2016 [8] | + | ? | + | + | + | + | + | + |
| Ivanics 2021 [22] | + | ! | + | + | + | + | + | + |
| Muscari 2005 [25] | ? | ? | + | + | ? | ? | + | ? |
| Nutu 2021 [26] | + | + | + | ? | + | + | + | + |
| Pinto 2021 [5] | ? | ? | + | + | + | + | + | + |
| Weller 2021 [28] | ! | ! | + | + | ? | ? | + | ? |
| Fujimoto 1993/Hirano 2005 [20,21] | + | + | + | + | ? | + | ? | + |
| Gong 2020 [9] | + | + | + | + | ? | + | ? | + |
| Kato 2009 [23] | + | + | + | + | + | + | + | + |
| Kitagawa 2001 [24] | + | + | + | + | ? | ? | + | + |
| Tomimaru 2011 [27] | + | + | + | + | + | + | + | + |
| Outcome | № of Included Studies | Certainty of the Evidence (GRADE) | Relative Effect (95% CI) |
|---|---|---|---|
| DFS after IBS vs. no IBS in LTx | 8 | Very Low | HR 0.98 [0.76,1.24] |
| Recurrence after IBS vs. no IBS in LTx | 6 | Very Low | OR 0.71 CI [0.41, 1.23] |
| OS after IBS vs. no IBS in LTx | 6 | Very Low | HR 1.13. [0.89, 1.42] |
| DFS after autotransfusion vs. none in hepatectomy | 4 | Very Low | HR 0.88 [0.80, 0.96] |
| Recurrence after autotransfusion vs. none in hepatectomy | 2 | Very Low | OR 0.28 [0.04, 2.18] |
| OS after autotransfusion vs. none in hepatectomy | 3 | Very Low | HR 0.71 [0.58, 0.88] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murtha-Lemekhova, A.; Fuchs, J.; Ritscher, E.; Hoffmann, K. Effect of Autotransfusion in HCC Surgery on Survival and Recurrence: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 4837. https://doi.org/10.3390/cancers14194837
Murtha-Lemekhova A, Fuchs J, Ritscher E, Hoffmann K. Effect of Autotransfusion in HCC Surgery on Survival and Recurrence: A Systematic Review and Meta-Analysis. Cancers. 2022; 14(19):4837. https://doi.org/10.3390/cancers14194837
Chicago/Turabian StyleMurtha-Lemekhova, Anastasia, Juri Fuchs, Emil Ritscher, and Katrin Hoffmann. 2022. "Effect of Autotransfusion in HCC Surgery on Survival and Recurrence: A Systematic Review and Meta-Analysis" Cancers 14, no. 19: 4837. https://doi.org/10.3390/cancers14194837
APA StyleMurtha-Lemekhova, A., Fuchs, J., Ritscher, E., & Hoffmann, K. (2022). Effect of Autotransfusion in HCC Surgery on Survival and Recurrence: A Systematic Review and Meta-Analysis. Cancers, 14(19), 4837. https://doi.org/10.3390/cancers14194837





