What’s beyond BRCA Mutational Status in High Grade Serous Ovarian Cancer? The Impact of Hormone Receptor Expression in a Large BRCA-Profiled Ovarian Cancer Patient Series: A Retrospective Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Immunohistochemistry
2.3. Evaluation of Immunohistochemical Staining
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Features
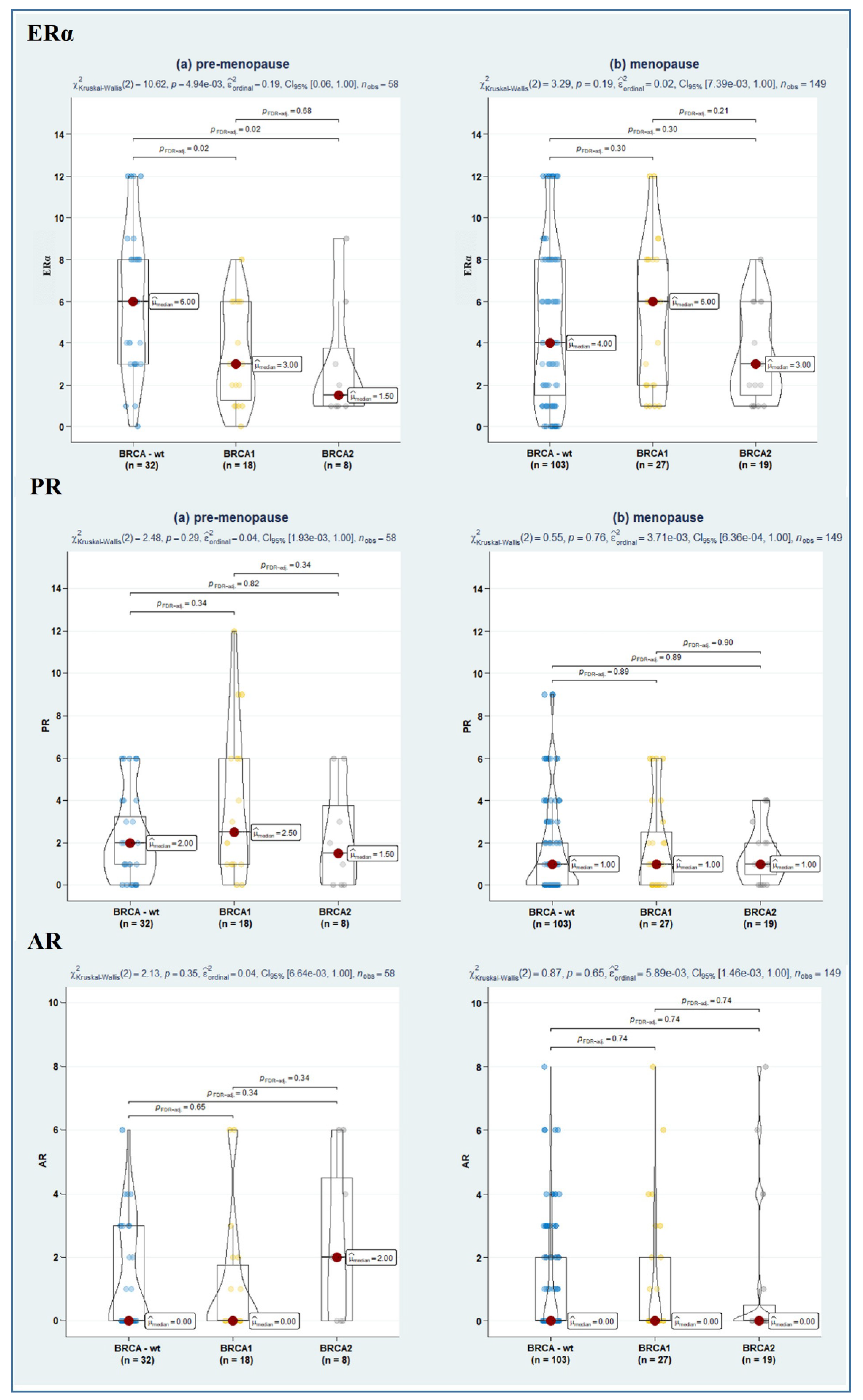
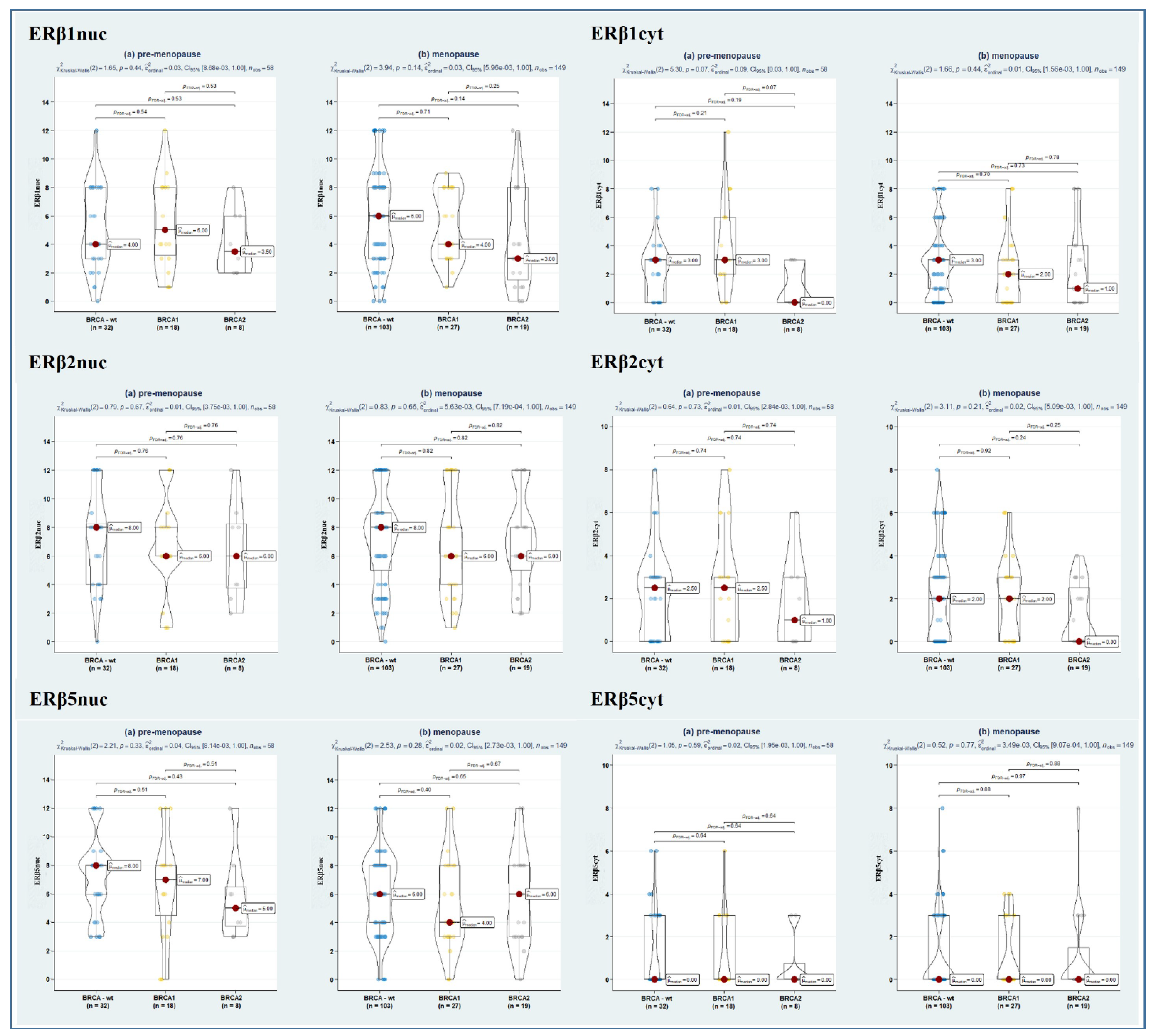
3.2. Hormone Receptor Status in HGSOC
3.3. Assessment of Potential Predictors of Overall Survival across BRCA Mutational Status
3.4. Assessment of Potential Predictors of Platinum Resistance across BRCA Mutational Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Additional Methods
Appendix A.1. Data Collection
Appendix A.2. Immunohistochemistry
Appendix A.3. Complete Statistical Analysis
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Park, E.Y.; Kim, O.; Schilder, J.M.; Coffey, D.M.; Cho, C.-H.; Bast, R.C., Jr. Cell Origins of High-Grade Serous Ovarian Cancer. Cancers 2018, 10, 433. [Google Scholar] [CrossRef]
- Torre, L.A.; Trabert, B.; DeSantis, C.E.; Miller, K.D.; Samimi, G.; Runowicz, C.D.; Gaudet, M.M.; Jemal, A.; Siegel, R.L. Ovarian cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 284–296. [Google Scholar] [CrossRef]
- Marchetti, C.; De Felice, F.; Romito, A.; Iacobelli, V.; Sassu, C.M.; Corrado, G.; Ricci, C.; Scambia, G.; Fagotti, A. Chemotherapy resistance in epithelial ovarian cancer: Mechanisms and emerging treatments. Semin. Cancer Biol. 2021, 77, 144–166. [Google Scholar] [CrossRef]
- Konstantinopoulos, P.A.; Matulonis, U.A. Targeting DNA Damage Response and Repair as a Therapeutic Strategy for Ovarian Cancer. Hematol. Oncol. Clin. N. Am. 2018, 32, 997–1010. [Google Scholar] [CrossRef]
- Gharwan, H.; Bunch, K.P.; Annunziata, C.M. The role of reproductive hormones in epithelial ovarian carcinogenesis. Endocr.-Relat. Cancer 2015, 22, R339–R363. [Google Scholar] [CrossRef]
- Gallo, D.; De Stefano, I.; Grazia Prisco, M.; Scambia, G.; Ferrandina, M.G. Estrogen Receptor Beta in Cancer: An Attractive Target for Therapy. Curr. Pharm. Des. 2012, 18, 2734–2757. [Google Scholar] [CrossRef] [PubMed]
- Leung, Y.-K.; Mak, P.; Hassan, S.; Ho, S.-M. Estrogen receptor (ER)-β isoforms: A key to understanding ER-β signaling. Proc. Natl. Acad. Sci. USA 2006, 103, 13162–13167. [Google Scholar] [CrossRef] [PubMed]
- De Stefano, I.; Zannoni, G.F.; Prisco, M.G.; Fagotti, A.; Tortorella, L.; Vizzielli, G.; Mencaglia, L.; Scambia, G.; Gallo, D. Cytoplasmic expression of estrogen receptor beta (ERβ) predicts poor clinical outcome in advanced serous ovarian cancer. Gynecol. Oncol. 2011, 122, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Sieh, W.; Köbel, M.; Longacre, T.A.; Bowtell, D.D.; Defazio, A.; Goodman, M.T.; Høgdall, E.; Deen, S.; Wentzensen, N.; Moysich, K.B.; et al. Hormone-receptor expression and ovarian cancer survival: An Ovarian Tumor Tissue Analysis consortium study. Lancet Oncol. 2013, 14, 853–862. [Google Scholar] [CrossRef]
- Ciucci, A.; Zannoni, G.F.; Travaglia, D.; Petrillo, M.; Scambia, G.; Gallo, D. Prognostic significance of the estrogen receptor beta (ERβ) isoforms ERβ1, ERβ2, and ERβ5 in advanced serous ovarian cancer. Gynecol. Oncol. 2014, 132, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.K.L.; Siu, M.K.Y.; Jiang, Y.X.; Wang, J.J.; Wang, Y.; Leung, T.H.Y.; Liu, S.S.; Cheung, A.N.Y.; Ngan, H.Y.S. Differential expression of estrogen receptor subtypes and variants in ovarian cancer: Effects on cell invasion, proliferation and prognosis. BMC Cancer 2017, 17, 606. [Google Scholar] [CrossRef] [PubMed]
- Mizushima, T.; Miyamoto, H. The Role of Androgen Receptor Signaling in Ovarian Cancer. Cells 2019, 8, 176. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Wentao, Y.; Bi, R.; Xiaojun, C.; Chen, X.; Yang, W.; Wu, X. A clinically applicable molecular classification for high-grade serous ovarian cancer based on hormone receptor expression. Sci. Rep. 2016, 6, 25408. [Google Scholar] [CrossRef]
- Diep, C.H.; Daniel, A.R.; Mauro, L.J.; Knutson, T.P.; Lange, C.A. Progesterone action in breast, uterine, and ovarian cancers. J. Mol. Endocrinol. 2015, 54, R31–R53. [Google Scholar] [CrossRef]
- Widschwendter, M.; Rosenthal, A.N.; Philpott, S.; Rizzuto, I.; Fraser, L.; Hayward, J.; Intermaggio, M.P.; Edlund, C.K.; Ramus, S.J.; Gayther, S.A.; et al. The sex hormone system in carriers of BRCA1/2 mutations: A case-control study. Lancet Oncol. 2013, 14, 1226–1232. [Google Scholar] [CrossRef]
- Rosen, E.M.; Fan, S.; Isaacs, C. BRCA1 in hormonal carcinogenesis: Basic and clinical research. Endocr.-Relat. Cancer 2005, 12, 533–548. [Google Scholar] [CrossRef]
- Aghmesheh, M.; Edwards, L.; Clarke, C.L.; Byth, K.; Katzenellenbogen, B.S.; Russell, P.J.; Friedlander, M.; Tucker, K.M.; de Fazio, A. Expression of steroid hormone receptors in BRCA1-associated ovarian carcinomas. Gynecol. Oncol. 2005, 97, 16–25. [Google Scholar] [CrossRef]
- Ciucci, A.; Ferrandina, G.; Mascilini, F.; Filippetti, F.; Scambia, G.; Zannoni, G.F.; Gallo, D. Estrogen receptor β: Potential target for therapy in adult granulosa cell tumors? Gynecol. Oncol. 2018, 150, 158–165. [Google Scholar] [CrossRef]
- NCSS. PASS 2021 Power Analysis and Sample Size Software; NCSS LLC: Kaysville, UT, USA, 2021. [Google Scholar]
- Feng, L.; Moritz, S.; Nowak, G.; Welsh, A.H.; O’Neill, T.J. imputeR: A General Multivariate Imputation Framework. R package version 2.2. 2020. Available online: https://CRAN.R-project.org/package=imputeR (accessed on 16 June 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 28 August 2022).
- Sotoca Covaleda, A.M.; Van den Berg, H.; Vervoort, J.; van der Saag, P.; Ström, A.; Gustafsson, J.-Å.; Rietjens, I.; Murk, A.J. Influence of Cellular ERα/ERβ Ratio on the ERα-Agonist Induced Proliferation of Human T47D Breast Cancer Cells. Toxicol. Sci. 2008, 105, 303–311. [Google Scholar] [CrossRef]
- Schüler-Toprak, S.; Weber, F.; Skrzypczak, M.; Ortmann, O.; Treeck, O. Estrogen receptor β is associated with expression of cancer associated genes and survival in ovarian cancer. BMC Cancer 2018, 18, 981. [Google Scholar] [CrossRef] [PubMed]
- Lakhani, S.R.; van de Vijver, M.J.; Jacquemier, J.; Anderson, T.J.; Osin, P.P.; McGuffog, L.; Easton, D.F. The Pathology of Familial Breast Cancer: Predictive Value of Immunohistochemical Markers Estrogen Receptor, Progesterone Receptor, HER-2, and p53 in Patients With Mutations in BRCA1 and BRCA2. J. Clin. Oncol. 2002, 20, 2310–2318. [Google Scholar] [CrossRef] [PubMed]
- Gorski, J.J.; Kennedy, R.D.; Hosey, A.M.; Harkin, D.P. The Complex Relationship between BRCA1 and ERα in Hereditary Breast Cancer. Clin. Cancer Res. 2009, 15, 1514–1518. [Google Scholar] [CrossRef] [PubMed]
- Russell, P.A.; Pharoah, P.D.; De Foy, K.; Ramus, S.J.; Symmonds, I.; Wilson, A.; Scott, I.; Ponder, B.A.J.; Gayther, S.A. Frequent loss of BRCA1 mRNA and protein expression in sporadic ovarian cancers. Int. J. Cancer 2000, 87, 317–321. [Google Scholar] [CrossRef]
- Fan, S.; Wang, J.-A.; Yuan, R.; Ma, Y.; Meng, Q.; Erdos, M.R.; Pestell, R.G.; Yuan, F.; Auborn, K.J.; Goldberg, I.D.; et al. BRCA1 Inhibition of Estrogen Receptor Signaling in Transfected Cells. Science 1999, 284, 1354–1356. [Google Scholar] [CrossRef]
- Mungenast, F.; Thalhammer, T. Estrogen Biosynthesis and Action in Ovarian Cancer. Front. Endocrinol. 2014, 5, 192. [Google Scholar] [CrossRef]
- Gjorgoska, M.; Rižner, T.L. Estrogens and the Schrödinger’s Cat in the Ovarian Tumor Microenvironment. Cancers 2021, 13, 5011. [Google Scholar] [CrossRef]
- Poola, I. Molecular Assays to Profile 10 Estrogen Receptor Beta Isoform mRNA Copy Numbers in Ovary, Breast, Uterus, and Bone Tissues. Endocrine 2003, 22, 101–112. [Google Scholar] [CrossRef]
- Poola, I.; Abraham, J.; Baldwin, K.; Saunders, A.; Bhatnagar, R. Estrogen Receptors Beta4 and Beta5 Are Full Length Functionally Distinct ERβ Isoforms: Cloning from Human Ovary and Functional Characterization. Endocrine 2005, 27, 227–238. [Google Scholar] [CrossRef]
- Collins, F.; Itani, N.; Esnal-Zufiaurre, A.; Gibson, D.A.; Fitzgerald, C.; Saunders, P.T.K. The ERβ5 splice variant increases oestrogen responsiveness of ERαpos Ishikawa cells. Endocr.-Relat. Cancer 2020, 27, 55–66. [Google Scholar] [CrossRef]
- Peng, B.; Lu, B.; Leygue, E.; Murphy, L.C. Putative functional characteristics of human estrogen receptor-beta isoforms. J. Mol. Endocrinol. 2003, 30, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Langdon, S.P.; Herrington, C.S.; Hollis, R.L.; Gourley, C. Estrogen Signaling and Its Potential as a Target for Therapy in Ovarian Cancer. Cancers 2020, 12, 1647. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Song, C.; Wang, D.; Hu, Y.; Liu, D.; Ma, D.; Gao, Q. Expression of hormone receptors predicts survival and platinum sensitivity of high-grade serous ovarian cancer. Biosci. Rep. 2021, 41, BSR20210478. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Luo, H.; Li, S.; Sheng, B.; Zhao, M.; Zhu, H.; Zhu, X. Correlation between estrogen receptor expression and prognosis in epithelial ovarian cancer: A meta-analysis. Oncotarget 2017, 8, 62400–62413. [Google Scholar] [CrossRef]
- Libard, S.; Cerjan, D.; Alafuzoff, I. Characteristics of the tissue section that influence the staining outcome in immunohistochemistry. Histochem. Cell Biol. 2019, 151, 91–96. [Google Scholar] [CrossRef]
- Erhard, F. Estimating pseudocounts and fold changes for digital expression measurements. Bioinformatics 2018, 34, 4054–4063. [Google Scholar] [CrossRef]
- Edmondson, R.; Monaghan, J.M.; Davies, B.R. The human ovarian surface epithelium is an androgen responsive tissue. Br. J. Cancer 2002, 86, 879–885. [Google Scholar] [CrossRef]
- Collins, F.; MacPherson, S.; Brown, P.; Bombail, V.; Williams, A.R.; Anderson, R.A.; Jabbour, H.N.; Saunders, P.T. Expression of oestrogen receptors, ERα, ERβ, and ERβ variants, in endometrial cancers and evidence that prostaglandin F may play a role in regulating expression of ERα. BMC Cancer 2009, 9, 330. [Google Scholar] [CrossRef]
- Troxell, M.L.; Long, T.; Hornick, J.L.; Ambaye, A.B.; Jensen, K.C. Comparison of Estrogen and Progesterone Receptor Antibody Reagents Using Proficiency Testing Data. Arch. Pathol. Lab. Med. 2017, 141, 1402–1412. [Google Scholar] [CrossRef]
- Kassambara, A. ggpubr: ‘ggplot2′ Based Publication Ready Plots. R Package version 0.4.0. 2020. Available online: https://CRAN.R-project.org/package=ggpubr (accessed on 28 August 2022).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Patil, I. Visualizations with statistical details: The ‘ggstatsplot’ approach. J. Open Source Softw. 2021, 6, 3167. [Google Scholar] [CrossRef]
- Schemper, M. Cox Analysis of Survival Data with Non-Proportional Hazard Functions. J. R. Stat. Soc. Ser. D 1992, 41, 455–465. [Google Scholar] [CrossRef]
- Schemper, M.; Wakounig, S.; Heinze, G. The estimation of average hazard ratios by weighted Cox regression. Stat. Med. 2009, 28, 2473–2489. [Google Scholar] [CrossRef] [PubMed]
- Harrell, F.E., Jr. HMISC: Harrell Miscellaneous. R Package Version 4.6-0. 2021. Available online: http://CRAN.R-project.org/package=Hmisc (accessed on 28 August 2022).
- Therneau, T.M. A Package for Survival Analysis in R. R Package Version 3.3-1. 2022. Available online: http://CRAN.R-project.org/package=survival (accessed on 28 August 2022).
- Therneau, T.; Grambsch, P. Modeling Survival Data: Extending the Cox Model; Springer: New York, NY, USA, 2000. [Google Scholar]
- Kassambara, A.; Kosinski, M.; Biecek, P.; Scheipl, F. Survminer: Drawing Survival Curves Using ‘ggplot2′. R package version 0.4.9. 2019. Available online: https://CRAN.R-project.org/package=survminer (accessed on 28 August 2022).
- Dunkler, D.; Ploner, M.; Schemper, M.; Heinze, G. Weighted Cox Regression Using the R Package coxphw. J. Stat. Softw. 2018, 84, 1–26. [Google Scholar] [CrossRef]


| BRCA Mutation | ||||
|---|---|---|---|---|
| Overall (n = 207) | wt-BRCA (n = 135) | BRCA1/2 (n = 72) | p ** | |
| Age (yrs.) | 59.1 (11.4) | 60.6 (11.5) | 56.4 (10.8) | 0.011 |
| Baseline BMI (kg/m2) | 24 (21.6–27.7) | 24.1 (21.9–27.7) | 24.0 (20.6–27.8) | 0.532 |
| Menopause, No. (%) | 149 (72.0) | 103 (76.3) | 46 (63.9) | 0.058 |
| Ca125 at diagnosis | 880.2 (318–2136.1) | 1003 (341.5–2237.8) | 601 (285–1762) | 0.080 |
| Ascites, No. (%) | 0.445 | |||
| Yes | 111 (53.6) | 75 (55.6) | 36 (50.0) | |
| No | 96 (46.4) | 60 (44.4) | 36 (50.0) | |
| FIGO Stage, No. (%) | 0.519 | |||
| I–II | 4 (1.9) | 2 (1.5) | 2 (2.8) | |
| III–IV | 203 (98.1) | 133 (98.5) | 70 (97.2) | |
| Primary Treatment, No. (%) | 0.034 | |||
| PDS | 125 (60.4) | 82 (60.7) | 43 (59.7) | |
| IDS | 63 (30.4) | 36 (26.7) | 27 (37.5) | |
| Non cytoreduced | 19 (9.2) | 17 (12.6) | 2 (2.8) | |
| RT, No. (%) | 0.079 | |||
| 0 | 162 (78.3) | 104 (77.0) | 58 (80.6) | |
| 1–10 mm | 21 (10.1) | 11 (8.2) | 10 (13.9) | |
| >10 mm | 24 (11.6) | 20 (14.8) | 4 (5.6) | |
| Therapy, No. (%) | ||||
| PARP-i | 8 (3.9) | - | 8 (11.1) | <0.001 |
| Bevacizumab | 87 (42.0) | 52 (38.5) | 35 (48.6) | 0.184 |
| Outcomes | ||||
| Overall Survival, No. (%) | 135 (65.2) | 77 (57.0) | 58 (80.6) | 0.001 |
| OS follow-up (months) | 34 (22–43) | 33 (19–42) | 38 (32–44.5) | 0.001 |
| Relapse, No. (%) | 151 (73.0) | 105 (77.8) | 46 (63.9) | 0.048 |
| Platinum resistance, No. (%) | 61 (29.5) | 51 (37.8) | 10 (13.9) | <0.001 |
| BRCA Mutation | ||||
|---|---|---|---|---|
| Overall (n = 207) | wt-BRCA (n = 135) | BRCA1/2 (n = 72) | p ** | |
| AR score | 0 (0–2) | 0 (0–2) | 0 (0–2) | 0.711 |
| PR score | 1 (0–3) | 1 (0–3) | 1 (0–4) | 0.157 |
| ERα score | 4 (2–8) | 4 (2–8) | 3 (2–6) | 0.090 |
| Nucleus ERβ1 score | 4 (3–8) | 4 (3–8) | 4 (3–8) | 0.218 |
| Cytoplasm ERβ1 score | 3 (0–3) | 3 (1–3) | 2 (0–3) | 0.425 |
| Nucleus ERβ2 score | 8 (4–9) | 8 (4–9) | 6 (4–8) | 0.227 |
| Cytoplasm ERβ2 score | 2 (0–3) | 2 (0–3) | 2 (0–3) | 0.400 |
| Nucleus ERβ5 score | 6 (4–8) | 6 (4–8) | 6 (3–8) | 0.097 |
| Cytoplasm ERβ5 score | 0 (0–3) | 0 (0–3) | 0 (0–3) | 0.992 |
| ERα/ERβ1nuc ratio | 0.8 (0.4–2.0) | 1.0 (0.4–2.0) | 0.8 (0.4–1.8) | 0.603 |
| ERα/ERβ2nuc ratio | 0.7 (0.3–1.0) | 0.7 (0.3–1.1) | 0.5 (0.3–1.0) | 0.603 |
| ERα/ERβ5nuc ratio | 0.8 (0.3–1.3) | 0.8 (0.3–1.3) | 0.7 (0.3–1.4) | 0.892 |
| P53 Status | 0.763 | |||
| Wild-type | 11 (5.3) | 8 (5.9) | 3 (4.2) | |
| Mutated null-type | 55 (26.6) | 34 (25.2) | 21 (29.2) | |
| Mutated overexpressed | 141 (68.1) | 93 (68.9) | 48 (66.7) | |
| Ordinary Cox Model | Interaction Cox Model | ||
|---|---|---|---|
| Predictor Main Effect (with BRCA = 0 [wt]) | Predictor × BRCA Interaction | ||
| Death (Primary Outcome) | HR (95% CI); p | HR (95% CI); p | IHR (95% CI); p |
| BRCA (Ref. = wt) | 0.34 (0.18; 0.61); <0.001 | - | - |
| BMI at baseline | 1.01 (0.97; 1.06); 0.637 | 1.01 (0.95; 1.07); 0.855 | 0.98 (0.89; 1.07); 0.609 |
| Menopause | 2.32 (1.24; 4.31); 0.008 | 0.71 (0.29; 1.69); 0.438 | 2.34 (0.45; 12.23); 0.315 |
| Ca125 | 1.00 (1.00; 1.00); 0.201 | 1.00 (1.00; 1.00); 0.317 | 1.00 (0.99; 1.00); 0.660 |
| Ascites | 2.35 (1.42; 3.88); 0.001 | 1.73 (1.00; 2.98); 0.049 | 3.20 (0.65; 15.77); 0.152 |
| Primary treatment (Ref. Non cytoreduced) | |||
| PDS | 0.06 (0.03; 0.11); <0.001 | 0.09 (0.04; 0.18); <0.001 | 0.09 (0.02; 0.41); 0.002 |
| IDS | 0.10 (0.05; 0.20); <0.001 | 0.14 (0.06; 0.29); <0.001 | 0.32 (0.10; 1.03); 0.055 |
| RT (ref = 0) | |||
| 1–10 mm | 1.32 (0.60; 2.94); 0.488 | 1.86 (0.78; 4.42); 0.160 | 0.28 (0.03; 2.64); 0.268 |
| >10 mm | 7.50 (4.23; 13.28); <0.001 | 6.26 (3.31; 11.83); <0.001 | 0.88 (0.17; 4.51); 0.880 |
| Molecular markers | |||
| Nucleus AR score | 0.93 (0.82; 1.06); 0.303 | 0.90 (0.77; 1.06); 0.202 | 1.12 (0.84; 1.50); 0.433 |
| PR score | 0.90 (0.80; 1.01); 0.067 | 0.95 (0.84; 1.08); 0.460 | 0.88 (0.64; 1.21); 0.441 |
| ERα score | 0.99 (0.93; 1.06); 0.840 | 0.95 (0.88; 1.02); 0.175 | 1.13 (0.93; 1.36); 0.211 |
| Nucleus ERβ1 score | 1.05 (0.98; 1.14); 0.177 | 1.02 (0.94; 1.11); 0.413 | 1.05 (0.86; 1.29); 0.497 |
| Cytoplasm ERβ1 score | 1.00 (0.91; 1.10); 0.935 | 0.97 (0.86; 1.09); 0.642 | 1.12 (0.91; 1.39); 0.289 |
| Nucleus ERβ2 score | 1.01 (0.94; 1.08); 0.832 | 0.97 (0.90; 1.06); 0.534 | 1.05 (0.88; 1.25); 0.587 |
| Cytoplasm ERβ2 score | 1.04 (0.94; 1.16); 0.441 | 1.02 (0.91; 1.15); 0.696 | 1.04 (0.78; 1.39); 0.762 |
| Nucleus ERβ5 score | 0.99 (0.92; 1.07); 0.794 | 0.99 (0.90; 1.08); 0.803 | 0.96 (0.78; 1.17); 0.669 |
| Cytoplasm ERβ5 score | 0.89 (0.77; 1.03); 0.129 | 0.94 (0.81; 1.10); 0.438 | 0.82 (0.50; 1.33); 0.418 |
| ERα/ERβ1nuc ratio | 0.91 (0.78; 1.06); 0.215 | 0.89 (0.74; 1.08); 0.239 | 1.02 (0.69; 1.49); 0.934 |
| ERα/ERβ2nuc ratio | 0.92 (0.75; 1.12); 0.396 | 0.85 (0.65; 1.12); 0.248 | 1.29 (0.79; 2.09); 0.306 |
| ERα/ERβ5nuc ratio | 0.97 (0.85; 1.11); 0.714 | 0.77 (0.61; 0.96); 0.019 | 1.41 (1.06; 1.87); 0.020 |
| P53 Status (Ref. wt) | |||
| Mutated null-type | 1.30 (0.39; 4.40); 0.667 | 1.68 (0.49; 5.77); 0.410 | Inf^ (0.00; Inf^); 0.996 |
| Mutated overexpressed | 1.26 (0.39; 4.01); 0.695 | 1.23 (0.38; 3.98); 0.733 | Inf^ (0.00; Inf^); 0.996 |
| Univariable Analysis | Interaction Multivariable Model | ||||
|---|---|---|---|---|---|
| Platinum Resistance | Predictor Main Effect (with BRCA = 0 [wt]) | Predictor x BRCA Interaction | |||
| Yes (n = 61) | No (n = 146) | OR (95% CI); p | OR (95% CI); p | IOR (95% CI); p | |
| Age | 63.2 (11.2) | 57.5 (11.1) | 1.05 (1.02; 1.08); 0.001 | - | - |
| BRCA mutated (Ref. = wt) | 10 (16.4) | 62 (42.5) | 0.27 (0.13; 0.56); 0.001 | - | - |
| BMI at baseline | 23.8 (21.2–27.2) | 24 (21.6–27.7) | 0.99 (0.93; 1.04); 0.632 | 0.96 (0.89; 1.04); 0.369 | 1.00 (0.89; 1.13); 0.978 |
| Menopause | 50 (82.0) | 99 (67.8) | 2.16 (1.03; 4.52); 0.041 | 0.75 (0.23; 2.37); 0.620 | 1.64 (0.25; 10.54); 0.602 |
| Ca125 | 938.4 (350.4–2132) | 858 (311–2135) | 1.00 (0.99; 1.00); 0.776 | 1.00 (1.00; 1.00); 0.752 | 1.00 (1.00; 1.00); 0.297 |
| Ascites | 42 (68.8) | 69 (47.3) | 2.47 (1.31; 4.64); 0.005 | 1.71 (0.82; 3.55); 0.149 | 5.84 (0.61; 55.75); 0.125 |
| Primary treatment (Ref. Non cytoreduced) | |||||
| Non cytoreduced | 18 (29.5) | 1 (0.7) | - | - | - |
| PDS | 23 (37.7) | 102 (69.9) | 0.01 (0.00; 0.10); <0.001 | 0.02 (0.00; 0.19); <0.001 | 0.00 (0.00; Inf^); 0.989 |
| IDS | 20 (32.8) | 43 (29.4) | 0.03 (0.00; 0.21); 0.001 | 0.04 (0.00; 0.36); 0.004 | 0.00 (0.00; Inf^); 0.990 |
| RT (ref = 0) | |||||
| 0 | 35 (57.4) | 127 (87.0) | - | - | - |
| 1–10 mm | 8 (13.1) | 13 (8.9) | 2.23 (0.86; 5.81); 0.099 | 3.24 (0.90; 11.74); 0.073 | 0.58 (0.06; 5.26); 0.627 |
| >10 mm | 18 (29.5) | 6 (4.1) | 10.88 (4.02; 29.50); <0.001 | 9.45 (2.86; 31.18); <0.001 | 0.71 (0.06; 8.43); 0.788 |
| Molecular markers | |||||
| Nucleus AR score | 0 (0–1) | 0 (0–2) | 1.00 (0.85; 1.17); 0.987 | 0.92 (0.75; 1.14); 0.455 | 1.25 (0.89; 1.77); 0.197 |
| PR score | 1 (0–2) | 1 (0–3) | 0.83 (0.71; 0.97); 0.019 | 0.87 (0.73; 1.04); 0.137 | 0.87 (0.55; 1.38); 0.556 |
| ERα score | 4 (2–8) | 4 (2–8) | 1.06 (0.97; 1.15); 0.230 | 1.01 (0.92; 1.12); 0.793 | 1.11 (0.87; 1.42); 0.401 |
| Nucleus ERβ1 score | 4 (3–8) | 5 (3–8) | 0.98 (0.89; 1.09); 0.751 | 0.96 (0.86; 1.08); 0.512 | 0.96 (0.73; 1.25); 0.764 |
| Cytoplasm ERβ1 score | 2 (0–3) | 3 (0–4) | 0.94 (0.82; 1.07); 0.341 | 0.86 (0.72; 1.03); 0.096 | 1.22 (0.91; 1.65); 0.179 |
| Nucleus ERβ2 score | 6.7 (3.1) | 7.2 (3.3) | 0.95 (0.87; 1.04); 0.304 | 0.91 (0.82; 1.02); 0.111 | 1.08 (0.86; 1.36); 0.491 |
| Cytoplasm ERβ2 score | 2 (0–3) | 2 (0–3) | 0.93 (0.80; 1.08); 0.348 | 0.89 (0.75; 1.06); 0.197 | 1.15 (0.78; 1.70); 0.471 |
| Nucleus ERβ5 score | 6.2 (2.6) | 6.2 (3.1) | 1.00 (0.91; 1.11); 0.960 | 0.94 (0.83; 1.07); 0.356 | 1.24 (0.96; 1.59); 0.096 |
| Cytoplasm ERβ5 score | 0 (0–0) | 0 (0–3) | 0.88 (0.73; 1.06); 0.185 | 0.88 (0.71; 1.10); 0.264 | 1.10 (0.69; 1.74); 0.686 |
| ERα/ERβ1nuc ratio | 1 (0.4–2.2) | 0.8 (0.4–1.5) | 1.04 (0.91; 1.18); 0.591 | 0.99 (0.83; 1.17); 0.889 | 1.20 (0.89; 1.62); 0.227 |
| ERα/ERβ2nuc ratio | 0.8 (0.3–1.5) | 0.6 (0.3–1.0) | 1.06 (0.87; 1.29); 0.549 | 1.02 (0.82; 1.27); 0.853 | 1.27 (0.73; 2.21); 0.394 |
| ERα/ERβ5nuc ratio | 0.8 (0.3–1.3) | 0.8 (0.3–1.3) | 0.95 (0.80; 1.13); 0.533 | 0.93 (0.77; 1.13); 0.488 | 0.73 (0.31; 1.73); 0.472 |
| P53 Status (Ref. wt) | |||||
| Wt | 2 (3.3) | 9 (6.2) | - | - | - |
| Mutated null-type | 14 (23.0) | 41 (28.1) | 1.54 (0.30; 7.98); 0.609 | 1.80 (0.30; 10.68); 0.520 | Inf^ (0.00; Inf^); 0.987 |
| Mutated overexpressed | 45 (73.8) | 96 (65.7) | 2.11 (0.44; 10.16); 0.352 | 2.10 (0.39; 11.27); 0.391 | Inf^ (0.00; Inf^); 0.987 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perrone, E.; Tudisco, R.; Pafundi, P.C.; Guido, D.; Ciucci, A.; Martinelli, E.; Zannoni, G.F.; Piermattei, A.; Spadola, S.; Ferrante, G.; et al. What’s beyond BRCA Mutational Status in High Grade Serous Ovarian Cancer? The Impact of Hormone Receptor Expression in a Large BRCA-Profiled Ovarian Cancer Patient Series: A Retrospective Cohort Study. Cancers 2022, 14, 4588. https://doi.org/10.3390/cancers14194588
Perrone E, Tudisco R, Pafundi PC, Guido D, Ciucci A, Martinelli E, Zannoni GF, Piermattei A, Spadola S, Ferrante G, et al. What’s beyond BRCA Mutational Status in High Grade Serous Ovarian Cancer? The Impact of Hormone Receptor Expression in a Large BRCA-Profiled Ovarian Cancer Patient Series: A Retrospective Cohort Study. Cancers. 2022; 14(19):4588. https://doi.org/10.3390/cancers14194588
Chicago/Turabian StylePerrone, Emanuele, Riccardo Tudisco, Pia Clara Pafundi, Davide Guido, Alessandra Ciucci, Enrica Martinelli, Gian Franco Zannoni, Alessia Piermattei, Saveria Spadola, Giulia Ferrante, and et al. 2022. "What’s beyond BRCA Mutational Status in High Grade Serous Ovarian Cancer? The Impact of Hormone Receptor Expression in a Large BRCA-Profiled Ovarian Cancer Patient Series: A Retrospective Cohort Study" Cancers 14, no. 19: 4588. https://doi.org/10.3390/cancers14194588
APA StylePerrone, E., Tudisco, R., Pafundi, P. C., Guido, D., Ciucci, A., Martinelli, E., Zannoni, G. F., Piermattei, A., Spadola, S., Ferrante, G., Marchetti, C., Scambia, G., Fagotti, A., & Gallo, D. (2022). What’s beyond BRCA Mutational Status in High Grade Serous Ovarian Cancer? The Impact of Hormone Receptor Expression in a Large BRCA-Profiled Ovarian Cancer Patient Series: A Retrospective Cohort Study. Cancers, 14(19), 4588. https://doi.org/10.3390/cancers14194588









