Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
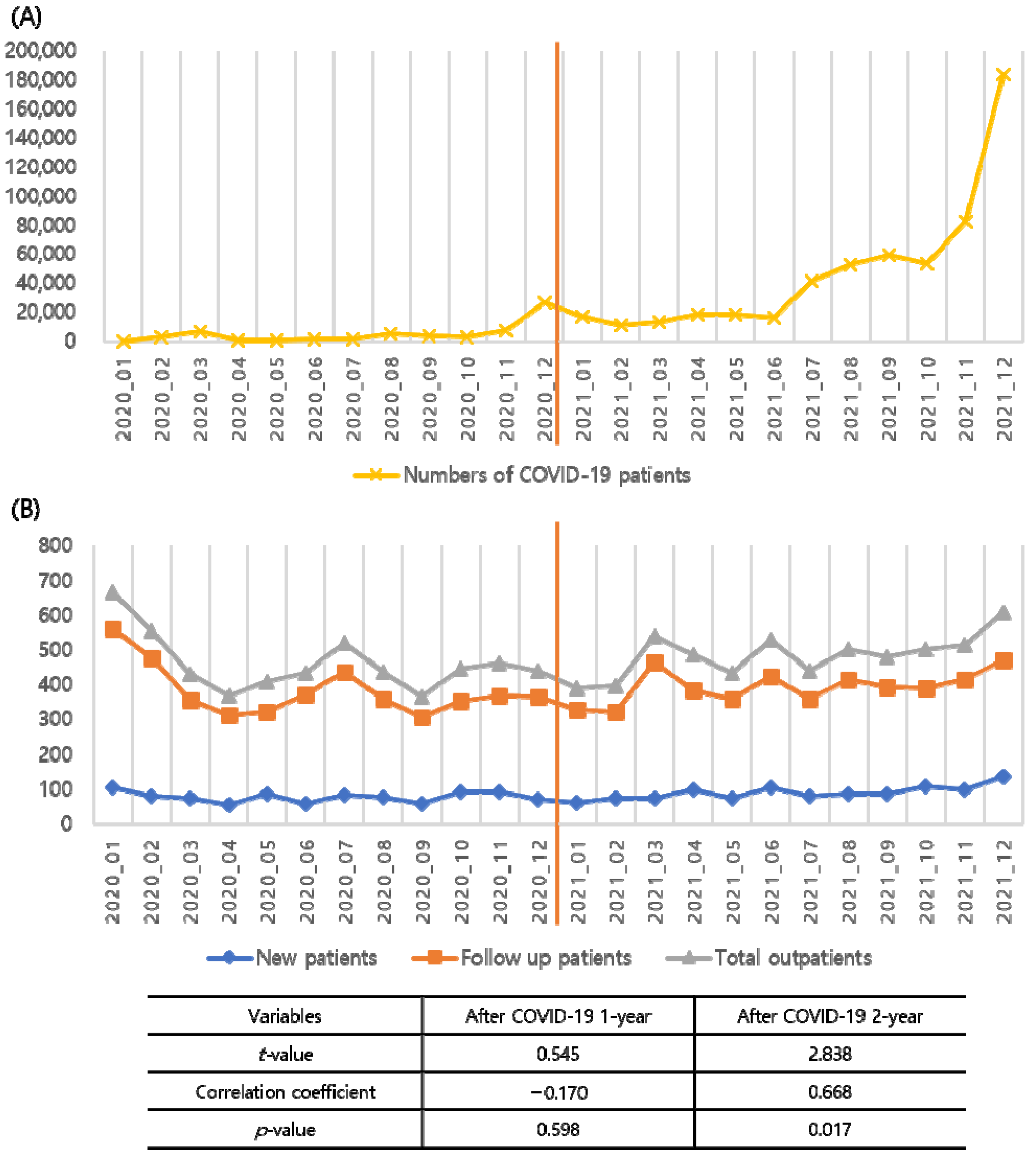
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Onyeaka, H.; Anumudu, C.K.; Al-Sharify, Z.T.; Egele-Godswill, E.; Mbaegbu, P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci. Prog. 2021, 104, 368504211019854. [Google Scholar] [CrossRef] [PubMed]
- Al-Jabir, A.; Kerwan, A.; Nicola, M.; Alsafi, Z.; Khan, M.; Sohrabi, C.; O’Neill, N.; Iosifidis, C.; Griffin, M.; Mathew, G.; et al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice—Part 1. Int. J. Surg. 2020, 79, 168–179. [Google Scholar] [CrossRef]
- Brindle, M.E.; Gawande, A. Managing COVID-19 in Surgical Systems. Ann. Surg. 2020, 272, e1–e2. [Google Scholar] [CrossRef]
- Diaz, A.; Sarac, B.A.; Schoenbrunner, A.R.; Janis, J.E.; Pawlik, T.M. Elective surgery in the time of COVID-19. Am. J. Surg. 2020, 219, 900–902. [Google Scholar] [CrossRef]
- Gambardella, C.; Pagliuca, R.; Pomilla, G.; Gambardella, A. COVID-19 risk contagion: Organization and procedures in a South Italy geriatric oncology ward. J. Geriatr. Oncol. 2020, 11, 1187–1188. [Google Scholar] [CrossRef]
- Pizzato, M.; Li, M.; Vignat, J.; Laversanne, M.; Singh, D.; La Vecchia, C.; Vaccarella, S. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 2022, 10, 264–272. [Google Scholar] [CrossRef]
- Vigliar, E.; Cepurnaite, R.; Alcaraz-Mateos, E.; Ali, S.Z.; Baloch, Z.W.; Bellevicine, C.; Bongiovanni, M.; Botsun, P.; Bruzzese, D.; Bubendorf, L.; et al. Global impact of the COVID-19 pandemic on cytopathology practice: Results from an international survey of laboratories in 23 countries. Cancer Cytopathol. 2020, 128, 885–894. [Google Scholar] [CrossRef]
- Vigliar, E.; Cepurnaite, R.; Iaccarino, A.; Pisapia, P.; De Luca, C.; Malapelle, U.; Bellevicine, C.; Troncone, G. Cytopathology practice during the COVID-19 postlockdown: An Italian experience. Cancer Cytopathol. 2021, 129, 548–554. [Google Scholar] [CrossRef]
- Tsang, V.H.M.; Gild, M.; Glover, A.; Clifton-Bligh, R.; Robinson, B.G. Thyroid cancer in the age of COVID-19. Endocr. Relat. Cancer 2020, 27, R407–R416. [Google Scholar] [CrossRef] [PubMed]
- Giannoula, E.; Iakovou, I.; Giovanella, L.; Vrachimis, A. Updated clinical management guidance during the COVID-19 pandemic: Thyroid nodules and cancer. Eur. J. Endocrinol. 2022, 186, G1–G7. [Google Scholar] [CrossRef] [PubMed]
- Vrachimis, A.; Iakovou, I.; Giannoula, E.; Giovanella, L. ENDOCRINOLOGY IN THE TIME OF COVID-19: Management of thyroid nodules and cancer. Eur. J. Endocrinol. 2020, 183, G41–G48. [Google Scholar] [CrossRef] [PubMed]
- Pramono, L.A. COVID-19 and Thyroid Diseases: How the Pandemic Situation Affects Thyroid Disease Patients. J. ASEAN Fed. Endocr. Soc. 2020, 35, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Shaha, A.R. Thyroid surgery during COVID-19 pandemic: Principles and philosophies. Head Neck 2020, 42, 1322–1324. [Google Scholar] [CrossRef]
- Medas, F.; Ansaldo, G.L.; Avenia, N.; Basili, G.; Boniardi, M.; Bononi, M.; Bove, A.; Carcoforo, P.; Casaril, A.; Cavallaro, G.; et al. The THYCOVIT (Thyroid Surgery during COVID-19 pandemic in Italy) study: Results from a nationwide, multicentric, case-controlled study. Updates Surg. 2021, 73, 1467–1475. [Google Scholar] [CrossRef]
- Tunca, F.; Iscan, Y.; Sormaz, I.C.; Aksakal, N.; Senyurek, Y. Impact of the Coronavirus Disease Pandemic on the Annual Thyroid, Parathyroid, and Adrenal Surgery Volume in a Tertiary Referral Endocrine Surgery Center in 2020. Med. Bull. Sisli Etfal Hosp. 2021, 55, 286–293. [Google Scholar] [CrossRef]
- Liu, H.; Zhan, L.; Guo, L.; Yu, X.; Li, L.; Feng, H.; Yang, D.; Xu, Z.; Tu, Y.; Chen, C.; et al. More Aggressive Cancer Behaviour in Thyroid Cancer Patients in the Post-COVID-19 Pandemic Era: A Retrospective Study. Int. J. Gen. Med. 2021, 14, 7197–7206. [Google Scholar] [CrossRef]
- COVID-19 National Emergency Response Center; Epidemiology Center; Epidemiology & and Case Management Team; Korea Centers for Disease Control and Prevention. Coronavirus Disease-19: The First 7755 Cases in the Republic of Korea. Osong. Public Health Res. Perspect. 2020, 11, 85–90. [Google Scholar] [CrossRef]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Lee, J.J.; Choe, Y.J.; Jeong, H.; Kim, M.; Kim, S.; Yoo, H.; Park, K.; Kim, C.; Choi, S.; Sim, J.; et al. Importation and Transmission of SARS-CoV-2 B.1.1.529 (Omicron) Variant of Concern in Korea, November 2021. J. Korean Med. Sci. 2021, 36, e346. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Oluyomi, A.; Woodard, L.; Raza, S.A.; Adel Fahmideh, M.; El-Mubasher, O.; Byun, J.; Han, Y.; Amos, C.I.; Badr, H. Individual-Level Determinants of Lifestyle Behavioral Changes during COVID-19 Lockdown in the United States: Results of an Online Survey. Int. J. Environ. Res. Public Health 2021, 18, 4364. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef]
- Yang, S.; Guo, B.; Ao, L.; Yang, C.; Zhang, L.; Zhou, J.; Jia, P. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin. Obes. 2020, 10, e12416. [Google Scholar] [CrossRef] [PubMed]
- Mogharab, V.; Ostovar, M.; Ruszkowski, J.; Hussain, S.Z.M.; Shrestha, R.; Yaqoob, U.; Aryanpoor, P.; Nikkhoo, A.M.; Heidari, P.; Jahromi, A.R.; et al. Global burden of the COVID-19 associated patient-related delay in emergency healthcare: A panel of systematic review and meta-analyses. Global Health 2022, 18, 58. [Google Scholar] [CrossRef]
- Carvalho, A.S.; Brito Fernandes, Ó.; de Lange, M.; Lingsma, H.; Klazinga, N.; Kringos, D. Changes in the quality of cancer care as assessed through performance indicators during the first wave of the COVID-19 pandemic in 2020: A scoping review. BMC Health Serv. Res. 2022, 22, 786. [Google Scholar] [CrossRef]
- Garcia, D.; Siegel, J.B.; Mahvi, D.A.; Zhang, B.; Mahvi, D.M.; Camp, E.R.; Graybill, W.; Savage, S.J.; Giordano, A.; Giordano, S.; et al. What is Elective Oncologic Surgery in the Time of COVID-19? A Literature Review of the Impact of Surgical Delays on Outcomes in Patients with Cancer. Clin. Oncol. Res. 2020, 3, 1–11. [Google Scholar] [CrossRef]
- Lee, J.; Park, J.H.; Lee, C.R.; Chung, W.Y.; Park, C.S. Long-term outcomes of total thyroidectomy versus thyroid lobectomy for papillary thyroid microcarcinoma: Comparative analysis after propensity score matching. Thyroid 2013, 23, 1408–1415. [Google Scholar] [CrossRef]
- Jeon, Y.W.; Gwak, H.G.; Lim, S.T.; Schneider, J.; Suh, Y.J. Long-Term Prognosis of Unilateral and Multifocal Papillary Thyroid Microcarcinoma After Unilateral Lobectomy Versus Total Thyroidectomy. Ann. Surg. Oncol. 2019, 26, 2952–2958. [Google Scholar] [CrossRef]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, S.H.; Choi-Kwon, S. Changes in quality of life and related factors in thyroid cancer patients with radioactive iodine remnant ablation. J. Korean Acad. Nurs. 2013, 43, 801–811. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.W.; Choi, Y.M.; Kim, H.S.; Kim, D.J.; Jo, H.J.; O’Donnell, B.F.; Jang, E.K.; Kim, T.Y.; Shong, Y.K.; Hong, J.P.; et al. Diminished Quality of Life and Increased Brain Functional Connectivity in Patients with Hypothyroidism After Total Thyroidectomy. Thyroid 2016, 26, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Gambardella, C.; Patrone, R.; Di Capua, F.; Offi, C.; Mauriello, C.; Clarizia, G.; Andretta, C.; Polistena, A.; Sanguinetti, A.; Calò, P. The role of prophylactic central compartment lymph node dissection in elderly patients with differentiated thyroid cancer: A multicentric study. BMC Surg. 2019, 18, 110. [Google Scholar] [CrossRef]
- Bakkar, S.; Al-Omar, K.; Aljarrah, Q.; Al-Dabbas, M.; Al-Dabbas, N.; Samara, S.; Miccoli, P. Impact of COVID-19 on thyroid cancer surgery and adjunct therapy. Updates Surg. 2020, 72, 867–869. [Google Scholar] [CrossRef]
- Nickel, B.; Miller, J.A.; Cvejic, E.; Gild, M.L.; Cope, D.; Dodd, R.; McCaffery, K.; Glover, A. Thyroid cancer clinicians’ views and experiences of delayed treatment during the COVID-19 pandemic: An international cross-sectional survey. ANZ J. Surg. 2021, 91, 2562–2564. [Google Scholar] [CrossRef] [PubMed]
- Murugan, A.K.; Alzahrani, A.S. SARS-CoV-2: Emerging role in the pathogenesis of various thyroid diseases. J. Inflamm. Res. 2021, 14, 6191. [Google Scholar] [CrossRef]
- Facchiano, A.; Facchiano, F.; Facchiano, A. An investigation into the molecular basis of cancer comorbidities in coronavirus infection. FEBS Open Bio. 2020, 10, 2363–2374. [Google Scholar] [CrossRef]
- Chen, W.; Tian, Y.; Li, Z.; Zhu, J.; Wei, T.; Lei, J. Potential interaction between SARS-CoV-2 and thyroid: A review. Endocrinology 2021, 162, bqab004. [Google Scholar] [CrossRef]
- Naguib, R. Potential relationships between COVID-19 and the thyroid gland: An update. J. Int. Med. Res. 2022, 50, 3000605221082898. [Google Scholar] [CrossRef]
- Scappaticcio, L.; Pitoia, F.; Esposito, K.; Piccardo, A.; Trimboli, P. Impact of COVID-19 on the thyroid gland: An update. Rev. Endocr. Metab. Disord. 2021, 22, 803–815. [Google Scholar] [CrossRef]
- Lisco, G.; De Tullio, A.; Jirillo, E.; Giagulli, V.A.; De Pergola, G.; Guastamacchia, E.; Triggiani, V. Thyroid and COVID-19: A review on pathophysiological, clinical and organizational aspects. J. Endocrinol. Investig. 2021, 44, 1801–1814. [Google Scholar] [CrossRef] [PubMed]
- Center Disease Control Headquarters in Korea. Available online: http://ncov.mohw.go.kr/index.jsp (accessed on 1 May 2022).

| Variables | Before COVID-19 1-Year (n = 490) | After COVID-19 1-Year (n = 428) | After COVID-19 2 Year (n = 432) | p Value |
|---|---|---|---|---|
| Age (years, mean ± sd) | 49.0 ± 13.2 | 49.1 ± 13.8 | 49.2 ± 13.4 | 0.925 |
| Gender | 0.979 | |||
| Male | 105 (35.8%) | 93 (21.7%) | 95 (22.0%) | |
| Female | 385 (78.6%) | 335 (78.3%) | 337 (78.0%) | |
| BMI (kg/m2, mean ± sd) | 25.1 ± 4.2 | 25.4 ± 4.1 | 25.3 ± 4.0 | 0.652 |
| Postoperative hospital stay days (mean ± sd) | 3.4 ± 1.1 | 3.1 ± 1.0 | 3.0 ± 1.4 | <0.001 |
| Days to 1st visit and surgery (mean ± sd) | 42.0 ± 42.7 | 62.5 ± 113.1 | 57.1 ± 141.8 | 0.009 |
| Bethesda category | 0.062 | |||
| I | 3 (0.6%) | 5 (1.2%) | 1 (0.2%) | |
| II | 75 (15.3%) | 85 (19.9%) | 60 (13.9%) | |
| III | 33 (6.7%) | 30 (7.0%) | 34 (7.9%) | |
| IV | 37 (7.6%) | 16 (3.7%) | 30 (6.9%) | |
| V | 80 (16.3%) | 67 (15.7%) | 89 (20.6%) | |
| VI | 254 (51.8%) | 218 (50.9%) | 215 (49.8%) | |
| Completed surgery | 8 (1.6%) | 7 (1.6%) | 3 (0.7%) | |
| Surgery extent, thyroid | 0.098 | |||
| Lobectomy | 249 (52.0%) | 236 (56.1%) | 251 (59.1%) | |
| Total thyroidectomy | 230 (48.0%) | 185 (43.9%) | 174 (40.9%) | |
| Surgery extent, node dissection | 0.6 | |||
| Central | 323 (89.2%) | 288 (90.6%) | 289 (88.1%) | |
| Lateral | 39 (10.8%) | 30 (9.4%) | 39 (11.9%) | |
| Pathologic diagnosis | 0.141 | |||
| Papillary thyroid cancer | 346 (70.6%) | 310 (72.4%) | 321 (74.3%) | |
| Follicular tumors * | 125 (25.5%) | 105 (24.5%) | 104 (24.1%) | |
| Medullary thyroid cancer | 5 (1.0%) | 1 (0.2%) | 0 (0%) | |
| Completion surgery | 3 (0.6%) | 5 (1.2%) | 0 (0%) | |
| Metastatic neck node | 11 (2.2%) | 7 (1.6%) | 7 (1.6%) |
| Variables | Before COVID-19, 1-Year (n = 346) | After COVID-19, 1-Year (n = 310) | After COVID-19, 2-Year (n = 321) | p Value |
|---|---|---|---|---|
| Age (years, mean ± sd) | 47.4 ± 12.6 | 47.4 ± 13.4 | 47.9 ± 12.6 | 0.862 |
| Gender | 0.479 | |||
| Male | 70 (20.2%) | 73 (23.5%) | 76 (23.7%) | |
| Female | 276 (79.8%) | 237 (76.5%) | 245 (76.3%) | |
| BMI (kg/m2, mean ± sd) | 25.2 ± 4.1 | 25.3 ± 4.1 | 25.5 ± 4.3 | 0.757 |
| Postoperative hospital stay days (mean ± sd) | 3.5 ± 1.1 | 3.2 ± 1.0 | 3.1 ± 1.6 | <0.001 |
| Days to 1st visit and surgery (mean ± sd) | 38.3 ± 32.2 | 58.3 ± 105.2 | 47.8 ± 124.7 | 0.027 |
| Tumor size (cm, mean ± sd) | 1.0 ± 0.8 | 1.1 ± 1.0 | 1.0 ± 0.9 | 0.405 |
| ≤1 cm | 232 (67.1%) | 203 (65.5%) | 224 (69.8%) | 0.505 |
| >1 cm | 114 (32.9%) | 107 (34.5%) | 97 (30.2%) | |
| Multifocality | 0.853 | |||
| Single | 208 (60.1%) | 181 (58.4%) | 194 (60.4%) | |
| Multiple | 139 (39.9%) | 129 (41.6%) | 127 (39.6%) | |
| Extrathyroidal extension | <0.001 | |||
| No | 257 (74.2%) | 215 (69.4%) | 187 (58.3%) | |
| Yes | 89 (25.7%) | 95 (30.6%) | 134 (41.7%) | |
| Lymphatic invasion | 0.006 | |||
| Absent | 234 (67.8%) | 215 (69.6%) | 178 (56.7%) | |
| Indeterminate | 35 (10.1%) | 33 (10.7%) | 50 (15.9%) | |
| Present | 76 (22.0%) | 61 (19.7%) | 86 (27.4%) | |
| Vascular invasion | 0.002 | |||
| Absent | 307 (89.0%) | 269 (87.9%) | 249 (79.8%) | |
| Indeterminate | 35 (10.1%) | 28 (9.2%) | 48 (15.4%) | |
| Present | 3 (0.9%) | 9 (2.9%) | 15 (4.8%) | |
| Node stage | 0.001 | |||
| N0, Nx | 205 (59.2%) | 154 (49.7%) | 132 (41.1%) | |
| N1a | 113 (32.7%) | 132 (42.6%) | 158 (49.2%) | |
| N1b | 28 (8.1%) | 24 (7.7%) | 31 (9.7%) | |
| BRAF mutation | 0.36 | |||
| Absent | 36 (11.3%) | 33 (11.2%) | 46 (14.5%) | |
| Present | 284 (88.8%) | 262 (88.8%) | 272 (85.5%) | |
| TERT promotor mutation | 0.957 | |||
| Absent | 241 (97.6%) | 248 (97.3%) | 288 (97.6%) | |
| Present | 6 (2.4%) | 7 (2.7%) | 7 (2.4%) | |
| Radioactive iodine therapy | 0.126 | |||
| No | 205 (59.2%) | 185 (59.7%) | 214 (66.7%) | |
| Yes | 141 (40.8%) | 125 (40.3%) | 107 (33.3%) |
| Variables | Before COVID-19, 1-Year (n = 125) | After COVID-19, 1-Year (n = 105) | After COVID-19, 2-Year (n = 104) | p Value |
|---|---|---|---|---|
| Age (years, mean ± sd) | 52.0 ± 14.1 | 53.8 ± 14.1 | 53.4 ± 15.0 | 0.62 |
| Gender | 0.582 | |||
| Male | 27 (21.6%) | 19 (18.1%) | 17 (16.3%) | |
| Female | 98 (78.4%) | 86 (81.9%) | 87 (83.7%) | |
| BMI (kg/m2, mean ± sd) | 25.0 ± 4.5 | 25.3 ± 3.9 | 24.9 ± 3.1 | 0.772 |
| Postoperative hospital stay days (mean ± sd) | 3.1 ± 1.0 | 2.8 ± 0.8 | 2.9 ± 0.9 | 0.019 |
| Days to 1st visit and surgery (mean ± sd) | 45.8 ± 48.3 | 63.1 ± 111.0 | 69.9 ± 154.9 | 0.23 |
| Tumor size (cm, mean ± sd) | 3.5 ± 2.2 | 4.0 ± 1.9 | 4.3 ± 2.3 | 0.022 |
| Multifocality | 0.235 | |||
| Single | 104 (83.2%) | 93 (88.6%) | 94 (90.4%) | |
| Multiple | 21 (16.8%) | 12 (11.4%) | 20 (9.6%) | |
| Pathologic diagnosis | n/a | |||
| Benign | 112 (89.6%) | 95 (90.5%) | 91 (87.5%) | |
| NIFTP | 11 (8.8%) | 6 (5.7%) | 6 (5.8%) | |
| Hurthle cell carcinoma | 0 | 0 | 5 (4.8%) | |
| Follicular thyroid carcinoma | 2 (1.6%) | 2 (1.9%) | 0 | |
| WDT-UMP | 0 | 2 (1.9%) | 1 (1.0%) | |
| Lymphoma | 0 | 0 | 1 (1.0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.H.; Min, E.; Hwang, Y.M.; Choi, Y.S.; Yi, J.W. Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea. Cancers 2022, 14, 4338. https://doi.org/10.3390/cancers14174338
Kim SH, Min E, Hwang YM, Choi YS, Yi JW. Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea. Cancers. 2022; 14(17):4338. https://doi.org/10.3390/cancers14174338
Chicago/Turabian StyleKim, Seong Hoon, Euna Min, Young Mi Hwang, Yun Suk Choi, and Jin Wook Yi. 2022. "Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea" Cancers 14, no. 17: 4338. https://doi.org/10.3390/cancers14174338
APA StyleKim, S. H., Min, E., Hwang, Y. M., Choi, Y. S., & Yi, J. W. (2022). Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea. Cancers, 14(17), 4338. https://doi.org/10.3390/cancers14174338





