Differences in Stakeholders’ Perception of the Impact of COVID-19 on Clinical Care and Decision-Making
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Questionnaire
2.2. Participants
2.3. Variables
2.4. Data Analysis
3. Results
3.1. Questionnaire Response and Cohort Description
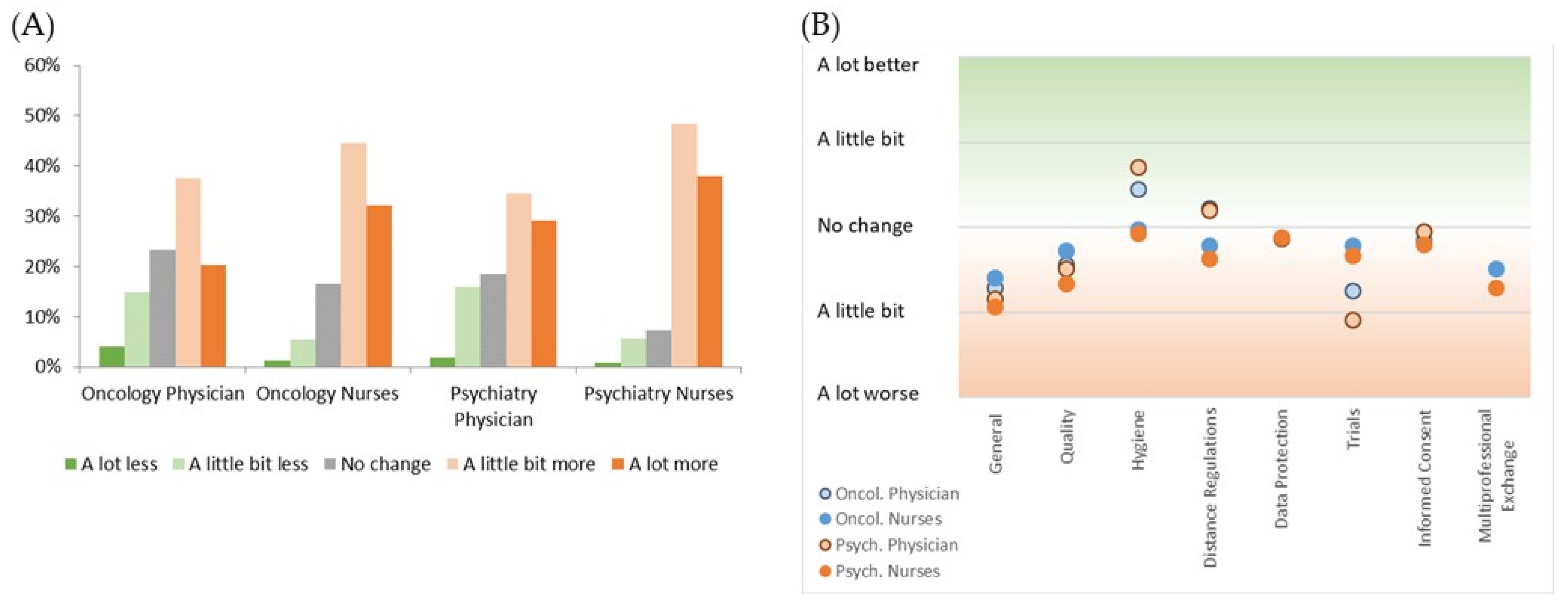
3.2. Perception of Workload and Clinical Management by Professionals
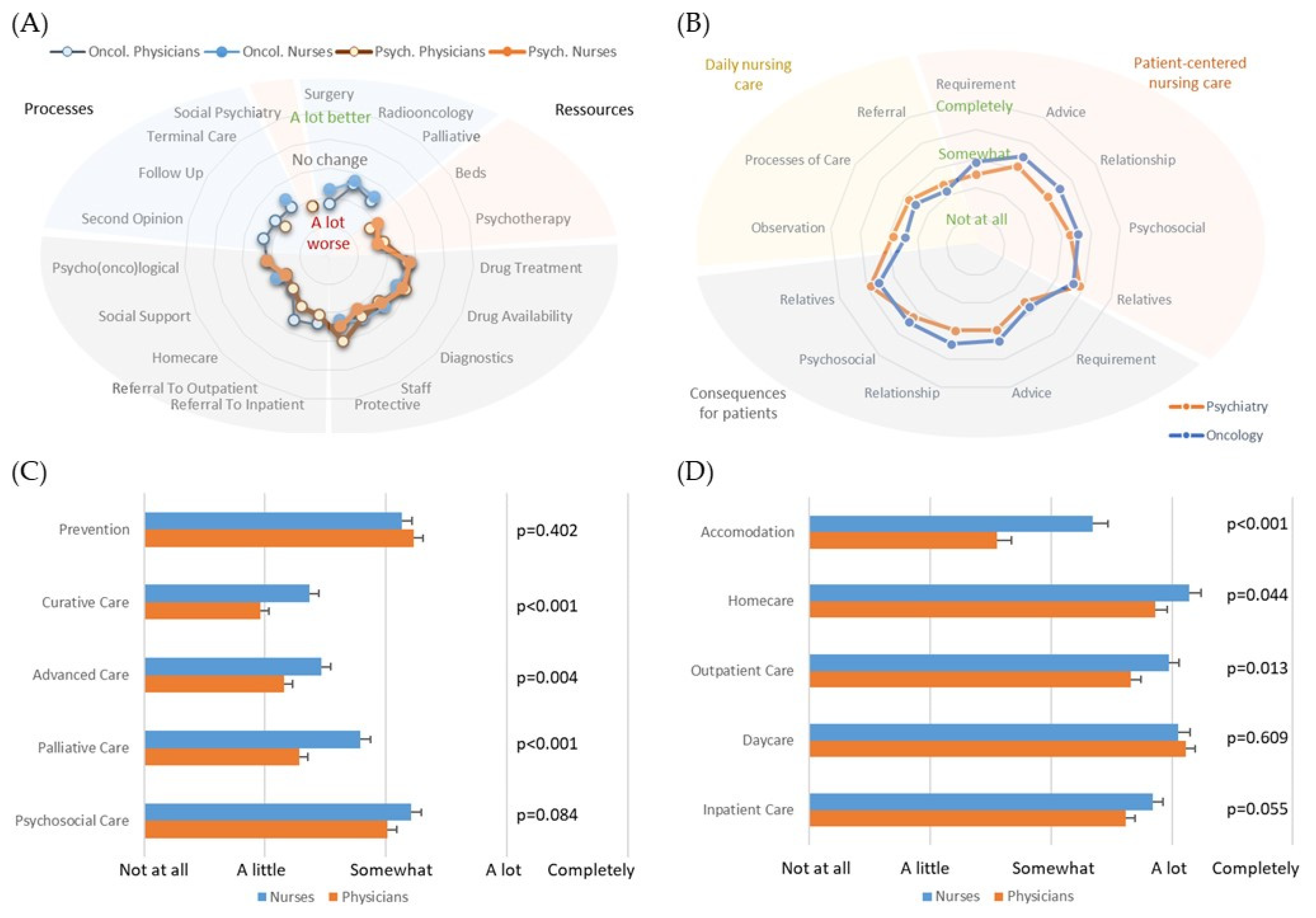
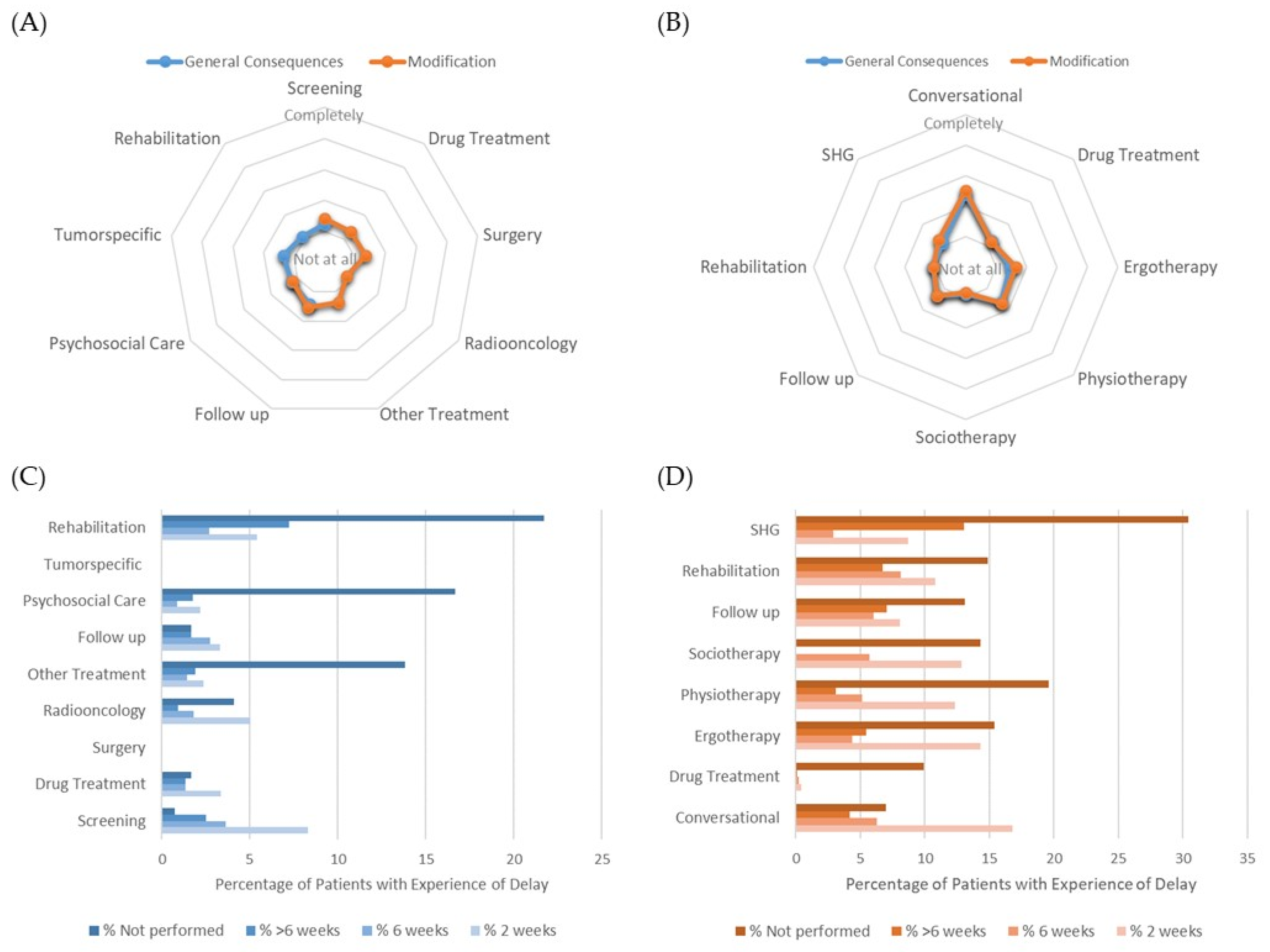
3.3. Perception of Modified Clinical Care and Consequences
3.4. Decisional Conflicts and Burden
3.5. Discrimination Analysis of Impact Perception
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dermody, S.M.; Shuman, A.G. Psychosocial Implications of COVID-19 on Head and Neck Cancer. Curr. Oncol. 2022, 29, 90. [Google Scholar] [CrossRef] [PubMed]
- Menculini, G.; Tortorella, A.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’Osso, B.; Luciano, M.; Nanni, M.G.; Pompili, M.; et al. Access to Mental Health Care during the First Wave of the COVID-19 Pandemic in Italy: Results from the COMET Multicentric Study. Brain Sci. 2021, 11, 1413. [Google Scholar] [CrossRef] [PubMed]
- Al-Quteimat, O.M.; Amer, A.M. The Impact of the COVID-19 Pandemic on Cancer Patients. Am. J. Clin. Oncol. 2020, 43, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Rashid, S.; Reeder, C.; Sahu, S.; Rashid, S. Psychological distress and moral injury to oncologists and their patients during COVID-19 pandemic. Curr. Psychol. 2021, 1–6. [Google Scholar] [CrossRef]
- Haier, J.; Beller, J.; Adorjan, K.; Bleich, S.; De Greck, M.; Griesinger, F.; Hein, A.; Hurlemann, R.; Mees, S.T.; Philipsen, A.; et al. Decision Conflicts in Clinical Care during COVID-19: A Patient Perspective. Healthcare 2022, 10, 1019. [Google Scholar] [CrossRef] [PubMed]
- Liberati, E.; Richards, N.; Parker, J.; Willars, J.; Scott, D.; Boydell, N.; Pinfold, V.; Martin, G.; Jones, P.B.; Dixon-Woods, M. Qualitative study of candidacy and access to secondary mental health services during the COVID-19 pandemic. Soc. Sci. Med. 2022, 296, 114711. [Google Scholar] [CrossRef] [PubMed]
- Wamkpah, N.S.; Gerndt, S.P.; Kallogjeri, D.; Piccirillo, J.F.; Chi, J.J. Patients’ Views of Shared Decision-making and Decisional Conflict in Otolaryngologic Surgery During the COVID-19 Pandemic. JAMA Otolaryngol. Neck Surg. 2021, 147, 879. [Google Scholar] [CrossRef]
- Ho, A.; Huang, V. Unmasking the Ethics of Public Health Messaging in a Pandemic. J. Bioethical Inq. 2021, 18, 549–559. [Google Scholar] [CrossRef]
- Beller, J.; Schäfers, J.; Geyer, S.; Haier, J.; Epping, J. Patterns of Changes in Oncological Care due to COVID-19: Results of a Survey of Oncological Nurses and Physicians from the Region of Hanover, Germany. Healthcare 2021, 10, 15. [Google Scholar] [CrossRef]
- Globig, L.K.; Blain, B.; Sharot, T. Perceptions of personal and public risk: Dissociable effects on behavior and well-being. J. Risk Uncertain. 2022, 64, 213–234. [Google Scholar] [CrossRef]
- Beller, J.; Schäfers, J.; Haier, J.; Geyer, S.; Epping, J. Trust in Healthcare during COVID-19 in Europe: Vulnerable groups trust the least. J. Public Health 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Botzen, W.J.W.; Duijndam, S.J.; Robinson, P.J.; van Beukering, P. Behavioral biases and heuristics in perceptions of COVID-19 risks and prevention decisions. Risk Anal. 2022. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, B.M.; Eichinger, J.; Schönweitz, F.; Buyx, A. Face mask uptake in the absence of mandates during the COVID-19 pandemic: A qualitative interview study with Swiss residents. BMC Public Health 2021, 21, 2171. [Google Scholar] [CrossRef]
- Joslyn, S.; Savelli, S.; Duarte, H.A.; Burgeno, J.; Qin, C.; Han, J.H.; Gulacsik, G. COVID-19: Risk perception, risk communication, and behavioral intentions. J. Exp. Psychol. Appl. 2021, 27, 599–620. [Google Scholar] [CrossRef]
- Armenia, S.; Arquitt, S.; Pedercini, M.; Pompei, A. Anticipating human resilience and vulnerability on the path to 2030: What can we learn from COVID-19? Futures 2022, 139, 102936. [Google Scholar] [CrossRef] [PubMed]
- Mielck, A.; Wild, V. Gesundheitliche Ungleichheit—Auf dem Weg von Daten zu Taten; Beltz Juventa: Weinheim, Germany; Basel, Switzerland, 2021; pp. 182–216. [Google Scholar]
- Rodriguez-Arrastia, M.; García-Martín, M.; Romero-López, A.; Ropero-Padilla, C.; Ruiz-Gonzalez, C.; Roman, P.; Sanchez-Labraca, N. Evolution of the Public-Health Response to COVID-19 Pandemic in Spain: A Descriptive Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 3824. [Google Scholar] [CrossRef]
- Wu, T. Perception Bias Effects on Healthcare Management in COVID-19 Pandemic: An Application of Cumulative Prospect Theory. Healthcare 2022, 10, 226. [Google Scholar] [CrossRef]
- Natale, A.; Concerto, C.; Rodolico, A.; Birgillito, A.; Bonelli, M.; Martinez, M.; Signorelli, M.S.; Petralia, A.; Infortuna, C.; Battaglia, F.; et al. Risk Perception among Psychiatric Patients during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2620. [Google Scholar] [CrossRef]
- Plate, R.C.; Jenkins, A.C. Anticipating Greater Impact of the COVID-19 Pandemic on Social Life Is Associated With Reduced Adherence to Disease-Mitigating Guidelines. Front. Psychol. 2022, 12, 756549. [Google Scholar] [CrossRef]
- Low, L.L.; Tong, S.F.; Ang, J.Y.; Abdullah, Z.; Hamid, M.A.; Risman, M.S.; Wong, Y.T.; Jamalul-Lail, N.I.; Chelladorai, K.; Tan, Y.P.; et al. Social responsibility perspective in public response to the COVID-19 pandemic: A grounded theory approach. BMC Public Health 2022, 22, 469. [Google Scholar] [CrossRef]
- McCarthy, M.C.; Beamish, J.; Bauld, C.M.; Marks, I.R.; Williams, T.; Olsson, C.A.; De Luca, C.R. Parent perceptions of pediatric oncology care during the COVID-19 pandemic: An Australian study. Pediatr. Blood Cancer 2021, 69, e29400. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; An, S.; Comes, T. From warning messages to preparedness behavior: The role of risk perception and information interaction in the Covid-19 pandemic. Int. J. Disaster Risk Reduct. 2022, 73, 102871. [Google Scholar] [CrossRef] [PubMed]
- Shahrabani, S.; Bord, S.; Admi, H.; Halberthal, M. Physicians’ Compliance with COVID-19 Regulations: The Role of Emotions and Trust. Healthcare 2022, 10, 582. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Marotta, N.; Raimo, S.; Lippi, L.; Inzitari, M.T.; Tasselli, A.; Gimigliano, A.; Palermo, L.; Invernizzi, M.; Ammendolia, A. Psychological Distress and Work Environment Perception by Physical Therapists from Southern Italy during COVID-19 Pandemic: The C.A.L.A.B.R.I.A study. Int. J. Environ. Res. Public Health 2021, 18, 9676. [Google Scholar] [CrossRef]
- Begerow, A.; Gaidys, U. “Ich stehe jeden Dienst mit mir selbst im Konflikt”–“Moral distress” bei Altenpflegenden während der COVID-19-Pandemie. HeilberufeScience 2022, 13, 59–68. [Google Scholar] [CrossRef]

| Discrimination Function Coefficients | Wilks–Lambda | p Values | |
|---|---|---|---|
| (A) | |||
| Decision Support Social Environment | −0.191 | 0.888 | 0.000 |
| Decision Support Own Evaluation | −0.145 | 0.947 | 0.000 |
| Decision Criteria Symptoms | 0.022 | 0.986 | 0.018 |
| Burden Infection Risk | 0.667 | 0.973 | 0.001 |
| Age 3 groups | 0.554 | 0.720 | 0.000 |
| Factor Psychological Conditions | −0.754 | 0.755 | 0.000 |
| (B) | |||
| Burden Patients | −0.506 | 0.935 | 0.000 |
| Fulfillment Legal Obligation | 0.054 | 0.988 | 0.014 |
| Management Hygiene | −0.358 | 0.941 | 0.000 |
| Resources Drug Treatment | 0.438 | 0.989 | 0.018 |
| Resources Drug Availability | −0.306 | 0.982 | 0.003 |
| Resources Diagnostics | 0.341 | 0.976 | 0.008 |
| Resources Protective Equipment | −0.142 | 0.976 | 0.001 |
| Burden Communication | 0.020 | 0.969 | 0.000 |
| Pandemic Workload | 0.414 | 0.944 | 0.000 |
| Burden Own Risk | 0.282 | 0.952 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haier, J.; Beller, J.; Adorjan, K.; Bleich, S.; de Greck, M.; Griesinger, F.; Heppt, M.V.; Hurlemann, R.; Mees, S.T.; Philipsen, A.; et al. Differences in Stakeholders’ Perception of the Impact of COVID-19 on Clinical Care and Decision-Making. Cancers 2022, 14, 4317. https://doi.org/10.3390/cancers14174317
Haier J, Beller J, Adorjan K, Bleich S, de Greck M, Griesinger F, Heppt MV, Hurlemann R, Mees ST, Philipsen A, et al. Differences in Stakeholders’ Perception of the Impact of COVID-19 on Clinical Care and Decision-Making. Cancers. 2022; 14(17):4317. https://doi.org/10.3390/cancers14174317
Chicago/Turabian StyleHaier, Joerg, Johannes Beller, Kristina Adorjan, Stefan Bleich, Moritz de Greck, Frank Griesinger, Markus V. Heppt, René Hurlemann, Soeren Torge Mees, Alexandra Philipsen, and et al. 2022. "Differences in Stakeholders’ Perception of the Impact of COVID-19 on Clinical Care and Decision-Making" Cancers 14, no. 17: 4317. https://doi.org/10.3390/cancers14174317
APA StyleHaier, J., Beller, J., Adorjan, K., Bleich, S., de Greck, M., Griesinger, F., Heppt, M. V., Hurlemann, R., Mees, S. T., Philipsen, A., Rohde, G., Schilling, G., Trautmann, K., Combs, S. E., Geyer, S., & Schaefers, J. (2022). Differences in Stakeholders’ Perception of the Impact of COVID-19 on Clinical Care and Decision-Making. Cancers, 14(17), 4317. https://doi.org/10.3390/cancers14174317







