Low Prevalence of HPV Related Oropharyngeal Carcinogenesis in Northern Sardinia
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Histopathological Analysis
2.2. Molecular Analyses
2.3. Statistical Analysis
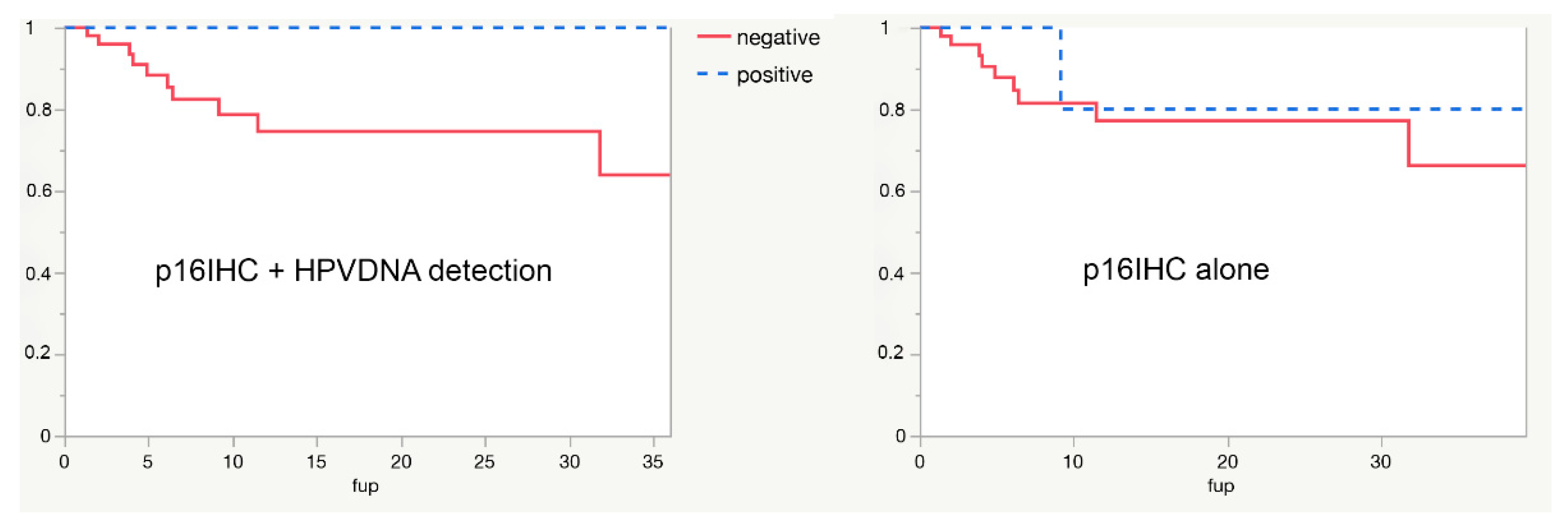
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- D’Souza, G.; Kreimer, A.R.; Viscidi, R.; Pawlita, M.; Fakhry, C.; Koch, W.M.; Westra, W.H.; Gillison, M.L. Case-control study of human papillomavirus and oropharyngeal cancer. N. Engl. J. Med. 2007, 356, 1944–1956. [Google Scholar] [CrossRef]
- Termine, N.; Panzarella, V.; Falaschini, S.; Russo, A.; Matranga, D.; Muzio, L.L.; Campisi, G. HPV in oral squamous cell carcinoma vs head and neck squamous cell carcinoma biopsies: A meta-analysis (1988–2007). Ann. Oncol. 2008, 19, 1681–1690. [Google Scholar] [CrossRef] [PubMed]
- Mariz, B.A.L.A.; Kowalski, L.P.; William, W.N., Jr.; de Castro, G., Jr.; Chaves, A.L.F.; Santos, M.; de Oliveira, T.B.; Araújo, A.L.D.; Normando, A.G.C.; Ribeiro, A.C.P.; et al. Global prevalence of human papillomavirus-driven oropharyngeal squamous cell carcinoma following the ASCO guidelines: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2020, 156, 103116. [Google Scholar] [CrossRef] [PubMed]
- Anantharaman, D.; Abedi-Ardekani, B.; Beachler, D.C.; Gheit, T.; Olshan, A.F.; Wisniewski, K.; Wunsch-Filho, V.; Toporcov, T.N.; Tajara, E.H.; Levi, J.E.; et al. Geographic heterogeneity in the prevalence of human papillomavirus in head and neck cancer. Int. J. Cancer 2017, 140, 1968–1975. [Google Scholar] [CrossRef]
- Carlander, A.; Jakobsen, K.; Bendtsen, S.; Garset-Zamani, M.; Lynggaard, C.; Jensen, J.; Grønhøj, C.; Buchwald, C. A Contemporary Systematic Review on Repartition of HPV-Positivity in Oropharyngeal Cancer Worldwide. Viruses 2021, 13, 1326. [Google Scholar] [CrossRef] [PubMed]
- Stein, A.P.; Saha, S.; Kraninger, J.L.; Swick, A.D.; Yu, M.; Lambertg, P.F.; Kimple, R. Prevalence of Human Papillomavirus in Oropharyngeal Cancer: A Systematic Review. Cancer J. 2015, 21, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Castellsagué, X.; Mena, M.; Alemany, L. Epidemiology of HPV-Positive Tumors in Europe and in the World. Recent Results Cancer Res. 2017, 6, 27–35. [Google Scholar]
- Smeets, S.J.; Hesselink, A.T.; Speel, E.-J.M.; Haesevoets, A.; Snijders, P.J.; Pawlita, M.; Meijer, C.J.; Braakhuis, B.J.; Leemans, C.R.; Brakenhoff, R.H. A novel algorithm for reliable detection of human papillomavirus in paraffin embedded head and neck cancer specimen. Int. J. Cancer 2007, 121, 2465–2472. [Google Scholar] [CrossRef]
- Amin, M.B.; Edge, S.; Greene, F.; Byrd, D.R.; Brookland, R.K.; Washington, M.K.; Gershenwald, J.E.; Compton, C.C.; Hess, K.R.; Sullivan, D.C.; et al. (Eds.) AJCC Cancer Staging Manual, 8th ed.; Springer International Publishing, American Joint Commission on Cancer: Chicago, IL, USA, 2017. [Google Scholar]
- Rietbergen, M.M.; Snijders, P.J.; Beekzada, D.; Braakhuis, B.J.; Brink, A.; Heideman, D.A.; Hesselink, A.T.; Witte, B.I.; Bloemena, E.; Baatenburg-De Jong, R.J. Molecular characterization of p16-immunopositive but HPV DNA-negative oropharyngeal carcinomas. Int. J. Cancer 2014, 134, 2366–2372. [Google Scholar] [CrossRef]
- Nauta, I.H.; Rietbergen, M.M.; Van Bokhoven, A.A.J.D.; Bloemena, E.; Lissenberg-Witte, B.I.; Heideman, D.A.M.; de Jong, R.B.; Brakenhoff, R.H.; Leemans, C.R. Evaluation of the eighth TNM classification on p16-positive oropharyngeal squamous cell carcinomas in the Netherlands and the importance of additional HPV DNA testing. Ann. Oncol. 2018, 29, 1273–1279. [Google Scholar] [CrossRef]
- Caudell, J.J.; Gillison, M.L.; Maghami, E.; Spencer, S.; Pfister, D.G.; Adkins, D.; Birkeland, A.C.; Brizel, D.M.; Busse, P.M.; Cmelak, A.J.; et al. NCCN Guidelines® Insights: Head and Neck Cancers, Version 1.2022: Featured Updates to the NCCN Guidelines. J. Natl. Compr. Cancer Netw. 2022, 20, 224–234. [Google Scholar] [CrossRef]
- CINtec®Histology (50-Test). Available online: http://reagent-catalog.roche.com/product/1875?type=2406 (accessed on 8 August 2022).
- DNA and RNA Purification Kit. Available online: https://www.qiagen.com/it/products/discovery-and-translational-research/dna-rna-purification/multianalyte-and-virus/allprep-dnarna-pe-kit/ (accessed on 8 August 2022).
- Muresu, N.; Sotgiu, G.; Saderi, L.; Sechi, I.; Cossu, A.; Marras, V.; Meloni, M.; Martinelli, M.; Cocuzza, C.; Tanda, F.; et al. Distribution of HPV Genotypes in Patients with a Diagnosis of Anal Cancer in an Italian Region. Int. J. Environ. Res. Public Health 2020, 17, 4516. [Google Scholar] [CrossRef]
- Muresu, N.; Sotgiu, G.; Saderi, L.; Sechi, I.; Cossu, A.; Marras, V.; Meloni, M.; Martinelli, M.; Cocuzza, C.; Tanda, F.; et al. Italian observational study on HPV infection, E6, and p16 expression in men with penile cancer. Virol. J. 2020, 17, 161. [Google Scholar] [CrossRef]
- Bussu, F.; Sali, M.; Gallus, R.; Vellone, V.G.; Zannoni, G.F.; Autorino, R.; Dinapoli, N.; Santangelo, R.; Martucci, R.; Graziani, C.; et al. HPV infection in squamous cell carcinomas arising from different mucosal sites of the head and neck region. Is p16 immunohistochemistry a reliable surrogate marker? Br. J. Cancer 2013, 108, 1157–1162. [Google Scholar] [CrossRef]
- Bussu, F.; Sali, M.; Gallus, R.; Petrone, G.; Zannoni, G.F.; Autorino, R.; Dinapoli, N.; Santangelo, R.; Vellone, V.G.; Graziani, C.; et al. Human papillomavirus (HPV) infection in squamous cell carcinomas arising from the oropharynx: Detection of HPV DNA and p16 immunohistochemistry as diagnostic and prognostic indicators-a pilot study. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 1115–1120. [Google Scholar] [CrossRef]
- Bussu, F.; Ragin, C.; Boscolo-Rizzo, P.; Rizzo, D.; Gallus, R.; Delogu, G.; Morbini, P.; Tommasino, M. HPV as a marker for molecular characterization in head and neck oncology: Looking for a standardization of clinical use and of detection method(s) in clinical practice. Head Neck 2019, 41, 1104–1111. [Google Scholar] [CrossRef]
- Chiang, C.W.K.; Marcus, J.H.; Sidore, C.; Biddanda, A.; Al-Asadi, H.; Zoledziewska, M.; Pitzalis, M.; Busonero, F.; Maschio, A.; Pistis, G.; et al. Genomic history of the Sardinian population. Nat. Genet. 2018, 50, 1426–1434. [Google Scholar] [CrossRef]
- Melchers, L.J.; Mastik, M.F.; Samaniego Cameron, B.; Van Dijk, B.A.C.; De Bock, G.H.; Van Der Laan, B.F.A.M.; Van Der Vegt, B.; Speel, E.J.M.; Roodenburg, J.L.N.; Witjes, M.J.H.; et al. Detection of HPV-associated oropharyngeal tumours in a 16-year cohort: More than meets the eye. Br. J. Cancer 2015, 112, 1349–1357. [Google Scholar] [CrossRef]
- Carlander, A.L.F.; Larsen, C.G.; Jensen, D.H.; Garnæs, E.; Kiss, K.; Andersen, L.; Olsen, C.H.; Franzmann, M.; Høgdall, E.; Kjær, S.K.; et al. Continuing rise in oropharyngeal cancer in a high HPV prevalence area: A Danish population-based study from 2011 to 2014. Eur. J. Cancer 2017, 70, 75–82. [Google Scholar] [CrossRef]
- Zamani, M.; Grønhøj, C.; Jensen, D.H.; Carlander, A.F.; Agander, T.; Kiss, K.; Olsen, C.; Baandrup, L.; Nielsen, F.C.; Andersen, E.; et al. The current epidemic of HPV-associated oropharyngeal cancer: An 18-year Danish population-based study with 2169 patients. Eur. J. Cancer 2020, 134, 52–59. [Google Scholar] [CrossRef]
- Ragin, C.; Liu, J.C.; Jones, G.; Shoyele, O.; Sowunmi, B.; Kennett, R.; Gibbs, D.; Blackman, E.; Esan, M.; Brandwein, M.S.; et al. Prevalence of HPV Infection in Racial-Ethnic Subgroups of Head and Neck Cancer Patients. Carcinogenesis 2017, 38, 218–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morbini, P.; Alberizzi, P.; Ferrario, G.; Capello, G.; De Silvestri, A.; Pedrazzoli, P.; Tinelli, C.; Benazzo, M. The evolving landscape of human papillomavirus-related oropharyngeal squamous cell carcinoma at a single institution in Northern Italy. Acta Otorhinolaryngol. Ital. 2019, 39, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Baboci, L.; Holzinger, D.; Boscolo-Rizzo, P.; Tirelli, G.; Spinato, R.; Lupato, V.; Fuson, R.; Schmitt, M.; Michel, A.; Halec, G.; et al. Low prevalence of HPV-driven head and neck squamous cell carcinoma in North-East Italy. Papillomavirus Res. 2016, 2, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Donà, M.G.; Rollo, F.; Pichi, B.; Spriano, G.; Moretto, S.; Covello, R.; Pellini, R.; Benevolo, M. Evolving Profile of HPV-Driven Oropharyngeal Squamous Cell Carcinoma in a National Cancer Institute in Italy: A 10-Year Retrospective Study. Microorganisms 2020, 8, 1498. [Google Scholar] [CrossRef]
- Del Mistro, A.; Frayle, H.; Menegaldo, A.; Favaretto, N.; Gori, S.; Nicolai, P.; Spinato, G.; Romeo, S.; Tirelli, G.; Da Mosto, M.C.; et al. Age-independent increasing prevalence of Human Papillomavirus-driven oropharyngeal carcinomas in North-East Italy. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Tagliabue, M.; Mena, M.; Maffini, F.; Gheit, T.; Blasco, B.Q.; Holzinger, D.; Tous, S.; Scelsi, D.; Riva, D.; Grosso, E.; et al. Role of Human Papillomavirus Infection in Head and Neck Cancer in Italy: The HPV-AHEAD Study. Cancers 2020, 12, 3567. [Google Scholar] [CrossRef]
- Braakhuis, B.J.; Brakenhoff, R.H.; Meijer, C.J.; Snijders, P.J.; Leemans, C.R. Human papilloma virus in head and neck cancer: The need for a standardised assay to assess the full clinical importance. Eur. J. Cancer 2009, 45, 2935–2939. [Google Scholar] [CrossRef]
- Gillison, M.L. HPV and prognosis for patients with oropharynx cancer. Eur. J. Cancer 2009, 45 (Suppl. S1), 383–385. [Google Scholar] [CrossRef]
- Cohen, M.A.; Basha, S.R.; Reichenbach, D.K.; Robertson, E.; Sewell, D.A. Increased viral load correlates with improved survival in HPV-16-associated tonsil carcinoma patients. Acta Otolaryngol. 2008, 128, 583–589. [Google Scholar] [CrossRef]
- Stephen, J.K.; Divine, G.; Chen, K.M.; Chitale, D.; Havard, S.; Worsham, M.J. Significance of p16 in Site-specific HPV Positive and HPV Negative Head and Neck Squamous Cell Carcinoma. Cancer Clin. Oncol. 2013, 2, 51–61. [Google Scholar]
- Miller, D.L.; Sharon Stack, M. Human Papillomavirus (HPV)-Associated Oropharyngeal Cancer; Springer: Berlin/Heidelberg, Germany, 2015; p. 314. [Google Scholar]
- Ang, K.K.; Harris, J.; Wheeler, R.; Weber, R.; Rosenthal, D.I.; Nguyen-Tân, P.F.; Westra, W.H.; Chung, C.H.; Jordan, R.C.; Lu, C.; et al. Human Papillomavirus and Survival of Patients with Oropharyngeal Cancer. N. Engl. J. Med. 2010, 363, 24–35. [Google Scholar] [CrossRef]
- Strohl, M.P.; Wai, K.C.; Ha, P.K. De-intensification strategies in HPV-related oropharyngeal squamous cell carcinoma—A narrative review. Ann. Transl. Med. 2020, 8, 1601. [Google Scholar] [CrossRef]
- Iorio, G.C.; Arcadipane, F.; Martini, S.; Ricardi, U.; Franco, P. Decreasing treatment burden in HPV-related OPSCC: A systematic review of clinical trials. Crit. Rev. Oncol. Hematol. 2021, 160, 103243. [Google Scholar] [CrossRef]
- Shi, W.; Kato, H.; Perez-Ordonez, B.; Pintilie, M.; Huang, S.H.; Hui, A.; O’Sullivan, B.; Waldron, J.; Cummings, B.; Kim, J.; et al. Comparative Prognostic Value of HPV16 E6 mRNA Compared With In Situ Hybridization for Human Oropharyngeal Squamous Carcinoma. J. Clin. Oncol. 2009, 27, 6213–6221. [Google Scholar] [CrossRef]
- Saito, Y.; Yoshida, M.; Omura, G.; Kobayashi, K.; Fujimoto, C.; Ando, M.; Sakamoto, T.; Asakage, T.; Yamasoba, T. Prognostic value of p16 expression irrespective of human papillomavirus status in patients with oropharyngeal carcinoma. Jpn. J. Clin. Oncol. 2015, 45, 828–836. [Google Scholar] [CrossRef]
- Benzerdjeb, N.; Tantot, J.; Blanchet, C.; Philouze, P.; Mekki, Y.; Lopez, J.; Devouassoux-Shisheboran, M. Oropharyngeal squamous cell carcinoma: p16/p53 immunohistochemistry as a strong predictor of HPV tumour status. Histopathology 2021, 79, 381–390. [Google Scholar] [CrossRef]
- Schache, A.G.; Liloglou, T.; Risk, J.M.; Filia, A.; Jones, T.M.; Sheard, J.; Woolgar, J.A.; Helliwell, T.R.; Triantafyllou, A.; Robinson, M.; et al. Evaluation of human papilloma virus diagnostic testing in oropharyngeal squamous cell carcinoma: Sensitivity, specificity, and prognostic discrimination. Clin. Cancer Res. 2011, 17, 6262–6271. [Google Scholar] [CrossRef]
- Oliva, C.; Carrillo-Beltrán, D.; Boettiger, P.; Gallegos, I.; Aguayo, F. Human Papillomavirus Detected in Oropharyngeal Cancers from Chilean Subjects. Viruses 2022, 14, 1212. [Google Scholar] [CrossRef]
- Méndez-Matías, G.; Velázquez-Velázquez, C.; Castro-Oropeza, R.; Mantilla-Morales, A.; Ocampo-Sandoval, D.; Burgos-González, A.; Heredia-Gutiérrez, C.; Alvarado-Cabrero, I.; Sánchez-Sandoval, R.; Barco-Bazán, A.; et al. Prevalence of HPV in Mexican Patients with Head and Neck Squamous Carcinoma and Identification of Potential Prognostic Biomarkers. Cancers 2021, 13, 5602. [Google Scholar] [CrossRef]
- Linge, A.; Schötz, U.; Löck, S.; Lohaus, F.; von Neubeck, C.; Gudziol, V.; Nowak, A.; Tinhofer, I.; Budach, V.; Sak, A.; et al. Comparison of detection methods for HPV status as a prognostic marker for loco-regional control after radiochemotherapy in patients with HNSCC. Radiother. Oncol. 2018, 127, 27–35. [Google Scholar] [CrossRef]
- Prigge, E.S.; Toth, C.; Dyckhoff, G.; Wagner, S.; Müller, F.; Wittekindt, C.; Freier, K.; Plinkert, P.; Hoffmann, J.; Vinokurova, S.; et al. p16(INK4a) /Ki-67 co-expression specifically identifies transformed cells in the head and neck region. Int. J. Cancer 2015, 136, 1589–1599. [Google Scholar] [CrossRef] [PubMed]
- Rotnáglová, E.; Tachezy, R.; Saláková, M.; Procházka, B.; Košl’abová, E.; Veselá, E.; Ludvíková, V.; Hamšíková, E.; Klozar, J. HPV involvement in tonsillar cancer: Prognostic significance and clinically relevant markers. Int. J. Cancer 2011, 129, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Rietbergen, M.M.; Leemans, C.R.; Bloemena, E.; Heideman, D.A.M.; Braakhuis, B.J.M.; Hesselink, A.T.; Witte, B.I.; de Jong, R.J.B.; Meijer, C.J.L.M.; Snijders, P.J.F.; et al. Increasing prevalence rates of HPV attributable oropharyngeal squamous cell carcinomas in the Netherlands as assessed by a validated test algorithm. Int. J. Cancer 2013, 132, 1565–1571. [Google Scholar] [CrossRef] [PubMed]
| Male, n (%) | 54 (87.1) | |
| Mean age (SD), years | 64 (10.2) | |
| Anatomic site, n/N (%) | Tonsil/Lateral wall | 22/62 (35.5) |
| Base of Tongue (BOT) | 19/62 (30.7) | |
| Posterior wall | 11/62 (17.7) | |
| Soft palate | 10/62 (16.1) | |
| Tumor Stage, n/N (%) | I | 6/62 (9.7) |
| II | 10/62 (16.1) | |
| III | 6/62 (9.7) | |
| IV | 40/62 (64.5) | |
| Histopathological grading (AJCC), n/N (%) | not assessed | 24/62 (38.7) |
| G1 | 0/62 (0.0) | |
| G2 | 20/62 (32.3) | |
| G3 | 18/62 (29) | |
| HPV-DNA positivity, n/N (%) | 9/62 (14.5) | |
| HPV-16 | 6/9 (66.7) | |
| HPV-18 | 1/9 (11.1) | |
| HPV-35 | 2/9 (22.2) | |
| p-16 immunohistochemistry positivity, n/N (%) | 12/62 (19.4) | |
| Population | Rate of p16 Positive among HPV-Negative OPSCCs (FPR) | Rate of HPV-Induced OPSCC in the Population | Proportion of HPV-/p16+ OPSCC in the Population | Probability That Positive p16 Is HPV-(1-Specificity) |
|---|---|---|---|---|
| Nauta (Holland) | 5.6% | 28.2% | 4% | 12.3% |
| Bussu (North Sardinia) | 5.7% | 14.5% | 4.8% | 25% |
| Bussu (Central Italy) | 20.6% | 32% | 14% | 30.4% |
| Saito (Japan) | 9.8% | 32% | 6.7% | 17.2% |
| Benzerdjeb (France) | 13.6% | 46.4% | 7.2% | 13.6% |
| Schache (UK) | 11.3% | 36.1% | 7.2% | 18% |
| Ang * (US) | 18.8% | 63.8% | 6.8% | 10.3% |
| Rotnaglova (Czech Republic) | 5.3% | 60% | 2.2% | 3.7% |
| Linge (Germany) | 9.6% | 21.7% | 7.4% | 25.6% |
| Prigge (Germany) | 5.7% | 17.2% | 4.7% | 21.4% |
| Carolina Oliva (Chile) | 26.3% | 60.4% | 10.4% | 17.9% |
| Galo Méndez-Matías (Mexico) | 20% | 39.2% | 12.3% | 23.7% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bussu, F.; Muresu, N.; Crescio, C.; Gallus, R.; Rizzo, D.; Cossu, A.; Sechi, I.; Fedeli, M.; Cossu, A.; Delogu, G.; et al. Low Prevalence of HPV Related Oropharyngeal Carcinogenesis in Northern Sardinia. Cancers 2022, 14, 4205. https://doi.org/10.3390/cancers14174205
Bussu F, Muresu N, Crescio C, Gallus R, Rizzo D, Cossu A, Sechi I, Fedeli M, Cossu A, Delogu G, et al. Low Prevalence of HPV Related Oropharyngeal Carcinogenesis in Northern Sardinia. Cancers. 2022; 14(17):4205. https://doi.org/10.3390/cancers14174205
Chicago/Turabian StyleBussu, Francesco, Narcisa Muresu, Claudia Crescio, Roberto Gallus, Davide Rizzo, Andrea Cossu, Illari Sechi, Mariantonietta Fedeli, Antonio Cossu, Giovanni Delogu, and et al. 2022. "Low Prevalence of HPV Related Oropharyngeal Carcinogenesis in Northern Sardinia" Cancers 14, no. 17: 4205. https://doi.org/10.3390/cancers14174205
APA StyleBussu, F., Muresu, N., Crescio, C., Gallus, R., Rizzo, D., Cossu, A., Sechi, I., Fedeli, M., Cossu, A., Delogu, G., & Piana, A. (2022). Low Prevalence of HPV Related Oropharyngeal Carcinogenesis in Northern Sardinia. Cancers, 14(17), 4205. https://doi.org/10.3390/cancers14174205









