Clinical Utility of Prostate Health Index for Diagnosis of Prostate Cancer in Patients with PI-RADS 3 Lesions
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Laboratory Tests
2.3. mpMRI Protocol and Interpretation
2.4. Biopsy Protocol
2.5. Histopathological Analysis
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics
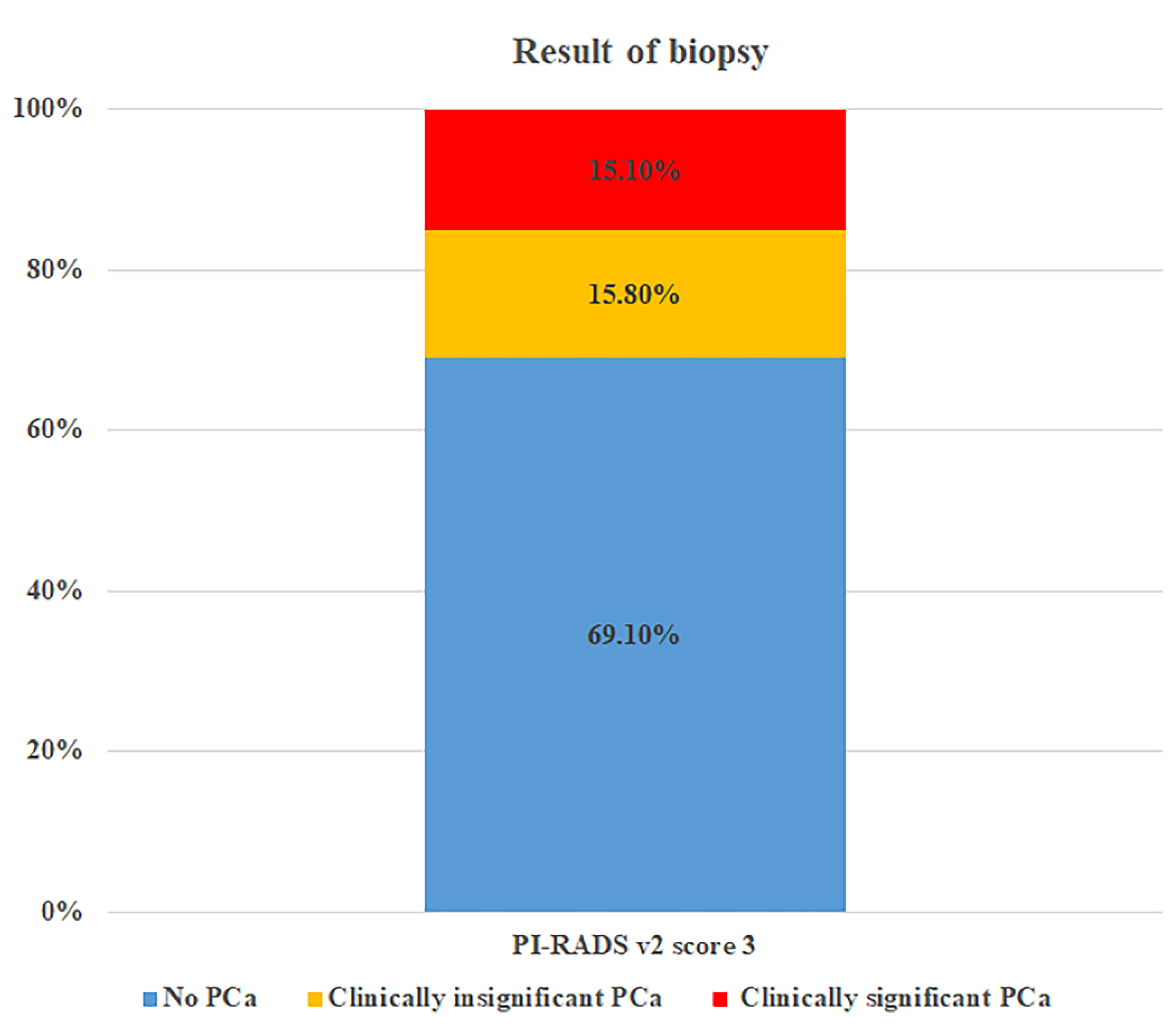
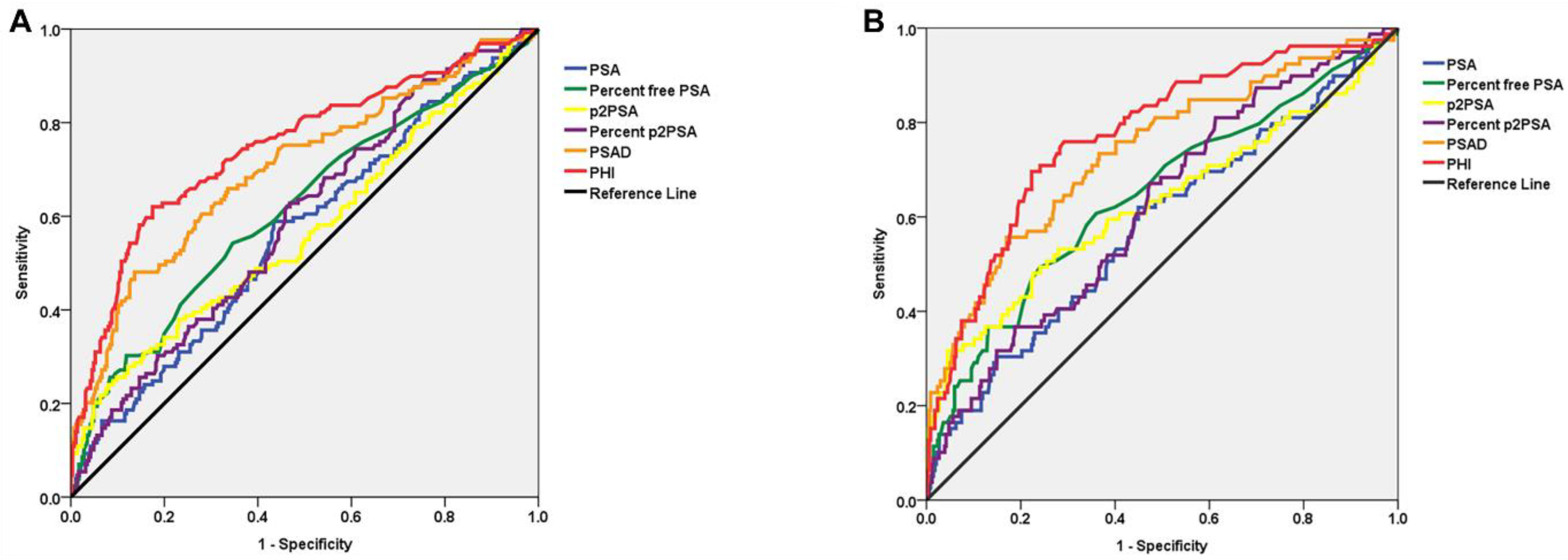
3.2. Biopsy Results and ROC Curve Analysis for PSA Derivatives
3.3. Diagnostic Performance According to Different PHI Cut-Offs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Culp, M.B.; Soerjomataram, I.; Efstathiou, J.A.; Bray, F.; Jemal, A. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur. Urol. 2020, 77, 38–52. [Google Scholar] [CrossRef] [PubMed]
- Duffy, M.J. Biomarkers for prostate cancer: Prostate-specific antigen and beyond. Clin. Chem. Lab. Med. 2020, 58, 326–339. [Google Scholar] [CrossRef] [PubMed]
- Stephan, C.; Vincendeau, S.; Houlgatte, A.; Cammann, H.; Jung, K.; Semjonow, A. Multicenter evaluation of [-2]proprostate-specific antigen and the prostate health index for detecting prostate cancer. Clin. Chem. 2013, 59, 306–314. [Google Scholar] [CrossRef]
- Lepor, A.; Catalona, W.J.; Loeb, S. The Prostate Health Index: Its Utility in Prostate Cancer Detection. Urol. Clin. North Am. 2016, 43, 1–6. [Google Scholar] [CrossRef]
- Dijkstra, S.; Mulders, P.F.; Schalken, J.A. Clinical use of novel urine and blood based prostate cancer biomarkers: A review. Clin. Biochem. 2014, 47, 889–896. [Google Scholar] [CrossRef]
- Catalona, W.J.; Partin, A.W.; Sanda, M.G.; Wei, J.T.; Klee, G.G.; Bangma, C.H.; Slawin, K.M.; Marks, L.S.; Loeb, S.; Broyles, D.L.; et al. A multicenter study of [-2]pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/ml prostate specific antigen range. J. Urol. 2011, 185, 1650–1655. [Google Scholar] [CrossRef]
- Tosoian, J.J.; Druskin, S.C.; Andreas, D.; Mullane, P.; Chappidi, M.; Joo, S.; Ghabili, K.; Agostino, J.; Macura, K.J.; Carter, H.B.; et al. Use of the Prostate Health Index for detection of prostate cancer: Results from a large academic practice. Prostate Cancer Prostatic Dis. 2017, 20, 228–233. [Google Scholar] [CrossRef]
- Kasivisvanathan, V.; Emberton, M.; Moore, C.M. MRI-Targeted Biopsy for Prostate-Cancer Diagnosis. N. Engl. J. Med. 2018, 379, 589–590. [Google Scholar] [CrossRef]
- Schoots, I.G.; Roobol, M.J.; Nieboer, D.; Bangma, C.H.; Steyerberg, E.W.; Hunink, M.G. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: A systematic review and meta-analysis. Eur. Urol. 2015, 68, 438–450. [Google Scholar] [CrossRef]
- Mottet, N.; van den Bergh, R.C.N.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S.; et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer—2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2021, 79, 243–262. [Google Scholar] [CrossRef]
- Sanda, M.G.; Cadeddu, J.A.; Kirkby, E.; Chen, R.C.; Crispino, T.; Fontanarosa, J.; Freedland, S.J.; Greene, K.; Klotz, L.H.; Makarov, D.V.; et al. Clinically Localized Prostate Cancer: AUA/ASTRO/SUO Guideline. Part I: Risk Stratification, Shared Decision Making, and Care Options. J. Urol. 2018, 199, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, J.C.; Barentsz, J.O.; Choyke, P.L.; Cornud, F.; Haider, M.A.; Macura, K.J.; Margolis, D.; Schnall, M.D.; Shtern, F.; Tempany, C.M.; et al. PI-RADS Prostate Imaging—Reporting and Data System: 2015, Version 2. Eur. Urol. 2016, 69, 16–40. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.U.; El-Shater Bosaily, A.; Brown, L.C.; Gabe, R.; Kaplan, R.; Parmar, M.K.; Collaco-Moraes, Y.; Ward, K.; Hindley, R.G.; Freeman, A.; et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): A paired validating confirmatory study. Lancet 2017, 389, 815–822. [Google Scholar] [CrossRef]
- Loeb, S.; Sanda, M.G.; Broyles, D.L.; Shin, S.S.; Bangma, C.H.; Wei, J.T.; Partin, A.W.; Klee, G.G.; Slawin, K.M.; Marks, L.S.; et al. The prostate health index selectively identifies clinically significant prostate cancer. J. Urol. 2015, 193, 1163–1169. [Google Scholar] [CrossRef]
- de la Calle, C.; Patil, D.; Wei, J.T.; Scherr, D.S.; Sokoll, L.; Chan, D.W.; Siddiqui, J.; Mosquera, J.M.; Rubin, M.A.; Sanda, M.G. Multicenter Evaluation of the Prostate Health Index to Detect Aggressive Prostate Cancer in Biopsy Naive Men. J. Urol. 2015, 194, 65–72. [Google Scholar] [CrossRef]
- Jansen, F.H.; van Schaik, R.H.; Kurstjens, J.; Horninger, W.; Klocker, H.; Bektic, J.; Wildhagen, M.F.; Roobol, M.J.; Bangma, C.H.; Bartsch, G. Prostate-specific antigen (PSA) isoform p2PSA in combination with total PSA and free PSA improves diagnostic accuracy in prostate cancer detection. Eur. Urol. 2010, 57, 921–927. [Google Scholar] [CrossRef]
- Barentsz, J.O.; Richenberg, J.; Clements, R.; Choyke, P.; Verma, S.; Villeirs, G.; Rouviere, O.; Logager, V.; Futterer, J.J.; European Society of Urogenital Radiology. ESUR prostate MR guidelines 2012. Eur. Radiol. 2012, 22, 746–757. [Google Scholar] [CrossRef]
- Park, S.Y.; Jung, D.C.; Oh, Y.T.; Cho, N.H.; Choi, Y.D.; Rha, K.H.; Hong, S.J.; Han, K. Prostate Cancer: PI-RADS Version 2 Helps Preoperatively Predict Clinically Significant Cancers. Radiology 2016, 280, 108–116. [Google Scholar] [CrossRef]
- Epstein, J.I.; Egevad, L.; Amin, M.B.; Delahunt, B.; Srigley, J.R.; Humphrey, P.A.; Grading Committee. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am. J. Surg. Pathol. 2016, 40, 244–252. [Google Scholar] [CrossRef]
- Hugosson, J.; Roobol, M.J.; Mansson, M.; Tammela, T.L.J.; Zappa, M.; Nelen, V.; Kwiatkowski, M.; Lujan, M.; Carlsson, S.V.; Talala, K.M.; et al. A 16-yr Follow-up of the European Randomized study of Screening for Prostate Cancer. Eur. Urol. 2019, 76, 43–51. [Google Scholar] [CrossRef] [Green Version]
- Tabayoyong, W.; Abouassaly, R. Prostate Cancer Screening and the Associated Controversy. Surg. Clin. N. Am. 2015, 95, 1023–1039. [Google Scholar] [CrossRef] [PubMed]
- Tosoian, J.J.; Trock, B.J.; Landis, P.; Feng, Z.; Epstein, J.I.; Partin, A.W.; Walsh, P.C.; Carter, H.B. Active surveillance program for prostate cancer: An update of the Johns Hopkins experience. J. Clin. Oncol. 2011, 29, 2185–2190. [Google Scholar] [CrossRef] [PubMed]
- Dall’Era, M.A.; Albertsen, P.C.; Bangma, C.; Carroll, P.R.; Carter, H.B.; Cooperberg, M.R.; Freedland, S.J.; Klotz, L.H.; Parker, C.; Soloway, M.S. Active surveillance for prostate cancer: A systematic review of the literature. Eur. Urol. 2012, 62, 976–983. [Google Scholar] [CrossRef] [PubMed]
- Porten, S.P.; Whitson, J.M.; Cowan, J.E.; Cooperberg, M.R.; Shinohara, K.; Perez, N.; Greene, K.L.; Meng, M.V.; Carroll, P.R. Changes in prostate cancer grade on serial biopsy in men undergoing active surveillance. J. Clin. Oncol. 2011, 29, 2795–2800. [Google Scholar] [CrossRef]
- Kretschmer, A.; Tilki, D. Biomarkers in prostate cancer—Current clinical utility and future perspectives. Crit. Rev. Oncol. Hematol. 2017, 120, 180–193. [Google Scholar] [CrossRef]
- Tosoian, J.J.; Druskin, S.C.; Andreas, D.; Mullane, P.; Chappidi, M.; Joo, S.; Ghabili, K.; Mamawala, M.; Agostino, J.; Carter, H.B.; et al. Prostate Health Index density improves detection of clinically significant prostate cancer. BJU Int. 2017, 120, 793–798. [Google Scholar] [CrossRef]
- Fan, Y.H.; Pan, P.H.; Cheng, W.M.; Wang, H.K.; Shen, S.H.; Liu, H.T.; Cheng, H.M.; Chen, W.R.; Huang, T.H.; Wei, T.C.; et al. The Prostate Health Index aids multi-parametric MRI in diagnosing significant prostate cancer. Sci. Rep. 2021, 11, 1286. [Google Scholar] [CrossRef]
- Hsieh, P.F.; Li, W.J.; Lin, W.C.; Chang, H.; Chang, C.H.; Huang, C.P.; Yang, C.R.; Chen, W.C.; Chang, Y.H.; Wu, H.C. Combining prostate health index and multiparametric magnetic resonance imaging in the diagnosis of clinically significant prostate cancer in an Asian population. World J. Urol. 2020, 38, 1207–1214. [Google Scholar] [CrossRef]
- Druskin, S.C.; Tosoian, J.J.; Young, A.; Collica, S.; Srivastava, A.; Ghabili, K.; Macura, K.J.; Carter, H.B.; Partin, A.W.; Sokoll, L.J.; et al. Combining Prostate Health Index density, magnetic resonance imaging and prior negative biopsy status to improve the detection of clinically significant prostate cancer. BJU Int. 2018, 121, 619–626. [Google Scholar] [CrossRef]
- Friedl, A.; Stangl, K.; Bauer, W.; Kivaranovic, D.; Schneeweiss, J.; Susani, M.; Hruby, S.; Lusuardi, L.; Lomoschitz, F.; Eisenhuber-Stadler, E.; et al. Prostate-specific Antigen Parameters and Prostate Health Index Enhance Prostate Cancer Prediction with the In-bore 3-T Magnetic Resonance Imaging-guided Transrectal Targeted Prostate Biopsy After Negative 12-Core Biopsy. Urology 2017, 110, 148–153. [Google Scholar] [CrossRef]
- Park, K.J.; Choi, S.H.; Lee, J.S.; Kim, J.K.; Kim, M.H.; Jeong, I.G. Risk Stratification of Prostate Cancer According to PI-RADS(R) Version 2 Categories: Meta-Analysis for Prospective Studies. J. Urol. 2020, 204, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Kruger-Stokke, B.; Bertilsson, H.; Langorgen, S.; Sjobakk, T.A.E.; Bathen, T.F.; Selnaes, K.M. Multiparametric Prostate MRI in Biopsy-Naive Men: A Prospective Evaluation of Performance and Biopsy Strategies. Front. Oncol. 2021, 11, 745657. [Google Scholar] [CrossRef] [PubMed]
- Natale, C.; Koller, C.R.; Greenberg, J.W.; Pincus, J.; Krane, L.S. Considering Predictive Factors in the Diagnosis of Clinically Significant Prostate Cancer in Patients with PI-RADS 3 Lesions. Life 2021, 11, 1432. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zeng, N.; Zhang, F.B.; Rui Huang, Y.X.; Tian, Y. Performing Precise Biopsy in Naive Patients with Equivocal PI-RADS, Version 2, Score 3, Lesions: An MRI-based Nomogram to Avoid Unnecessary Surgical Intervention. Clin. Genitourin. Cancer 2020, 18, 367–377. [Google Scholar] [CrossRef]
- Rico, L.; Blas, L.; Vitagliano, G.; Contreras, P.; Rios Pita, H.; Ameri, C. PI-RADS 3 lesions: Does the association of the lesion volume with the prostate-specific antigen density matter in the diagnosis of clinically significant prostate cancer? Urol. Oncol. 2021, 39, 431.e9–431.e13. [Google Scholar] [CrossRef]
- Yang, S.; Zhao, W.; Tan, S.; Zhang, Y.; Wei, C.; Chen, T.; Shen, J. Combining clinical and MRI data to manage PI-RADS 3 lesions and reduce excessive biopsy. Transl. Androl. Urol. 2020, 9, 1252–1261. [Google Scholar] [CrossRef]
- Al Awamlh, B.A.H.; Marks, L.S.; Sonn, G.A.; Natarajan, S.; Fan, R.E.; Gross, M.D.; Mauer, E.; Banerjee, S.; Hectors, S.; Carlsson, S.; et al. Multicenter analysis of clinical and MRI characteristics associated with detecting clinically significant prostate cancer in PI-RADS (v2.0) category 3 lesions. Urol. Oncol. 2020, 38, 637.e9–637.e15. [Google Scholar] [CrossRef]
- Massanova, M.; Robertson, S.; Barone, B.; Dutto, L.; Caputo, V.F.; Bhatt, J.R.; Crocetto, F. The Comparison of Imaging and Clinical Methods to Estimate Prostate Volume: A Single-Centre Retrospective Study. Urol. Int. 2021, 105, 804–810. [Google Scholar] [CrossRef]

| Variables | Total | Detection of Prostate Cancer | p | |
|---|---|---|---|---|
| No | Yes | |||
| No. of Patients, n (%) | 392 (100.0) | 271 (69.1) | 121 (30.9) | |
| Age, years | 0.725 | |||
| Median (IQR) | 64.3 (60.0–69.3) | 64.0 (60.0–69.0) | 65.0 (60.0–70.0) | |
| Mean (SD) | 63.9 (8.2) | 63.7 (8.7) | 64.4 (7.3) | |
| Total PSA, ng/ml | 0.289 | |||
| Median (IQR) | 6.64 (4.05–9.54) | 6.56 (4.17–9.85) | 6.85 (4.31–10.18) | |
| Mean (SD) | 8.54 (8.96) | 8.21 (7.20) | 9.31 (9.21) | |
| Prostate volume, ml | <0.001 | |||
| Median (IQR) | 40.2 (28.5–50.5) | 42.6 (31.3–52.2) | 34.6 (23.9–44.1) | |
| Mean (SD) | 44.5 (21.6) | 47.8 (22.6) | 36.7 (18.0) | |
| PSAD | <0.001 | |||
| Median (IQR) | 0.16 (0.10–0.26) | 0.14 (0.11–0.28) | 0.20 (0.10–0.23) | |
| Mean (SD) | 0.19 (0.23) | 0.17 (0.24) | 0.25 (0.19) | |
| % fPSA | 0.013 | |||
| Median (IQR) | 16.8 (12.2–23.6) | 19.6 (13.9–24.8) | 11.5 (9.9–18.3) | |
| Mean (SD) | 17.9 (7.5) | 19.4 (8.6) | 14.1 (6.7) | |
| p2PSA, pg/ml | <0.001 | |||
| Median (IQR) | 18.35 (15.59–30.13) | 15.46 (11.28–22.25) | 24.24 (18.62–38.74) | |
| Mean (SD) | 19.69 (8.16) | 16.04 (8.46) | 27.62 (7.49) | |
| % p2PSA | <0.001 | |||
| Median (IQR) | 1.42 (1.27–2.01) | 1.25 (0.99–1.52) | 1.81 (1.49–2.23) | |
| Mean (SD) | 1.68 (1.56) | 1.35 (1.55) | 2.05 (1.55) | |
| PHI | <0.001 | |||
| Median (IQR) | 35.3 (28.6–48.3) | 30.5 (26.0–44.3) | 46.5 (35.0–62.1) | |
| Mean (SD) | 39.2 (17.3) | 36.5 (15.7) | 51.6 (19.5) | |
| Biopsy Gleason grade, n (%) | ||||
| 6 | 62 (51.2) | |||
| 7 (3 + 4) | 47 (38.9) | |||
| 8 | 12 (9.9) | |||
| Variables | Overall Prostate Cancer | Clinically Significant Prostate Cancer | ||||
|---|---|---|---|---|---|---|
| AUC | 95% CI | p | AUC | 95% CI | p | |
| Total PSA | 0.593 | 0.481–0.688 | Ref | 0.604 | 0.502–0.714 | Ref |
| PSAD | 0.712 | 0.611–0.813 | 0.016 | 0.760 | 0.652–0.866 | 0.014 |
| % fPSA | 0.661 | 0.566–0.772 | 0.231 | 0.682 | 0.589–0.772 | 0.248 |
| p2PSA | 0.613 | 0.521–0.704 | 0.304 | 0.662 | 0.554–0.756 | 0.326 |
| % p2PSA | 0.630 | 0.542–0.744 | 0.135 | 0.648 | 0.539–0.742 | 0.216 |
| PHI | 0.807 | 0.710–0.906 | 0.001 | 0.819 | 0.723–0.922 | <0.001 |
| Sensitivity | Specificity | PPV | NPV | Biopsy Criteria by PHI | ||
|---|---|---|---|---|---|---|
| % Biopsy Avoided | % PCa Missed | |||||
| PHI ≥ 27 | 95.0% | 33.9% | 39.1% | 93.9% | 25.0% | 5.0% |
| PHI ≥ 30 | 91.7% | 46.1% | 43.2% | 92.6% | 34.4% | 8.3% |
| PHI ≥ 33 | 86.0% | 56.5% | 46.8% | 90.0% | 43.4% | 14.0% |
| PHI ≥ 36 | 75.2% | 62.7% | 47.3% | 85.0% | 51.0% | 24.8% |
| PHI ≥ 40 | 66.1% | 70.1% | 49.7% | 82.3% | 58.7% | 33.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.-U.; Lee, S.-M.; Chung, J.-H.; Kang, M.; Sung, H.-H.; Jeon, H.-G.; Jeong, B.-C.; Seo, S.-I.; Jeon, S.-S.; Lee, H.-M.; et al. Clinical Utility of Prostate Health Index for Diagnosis of Prostate Cancer in Patients with PI-RADS 3 Lesions. Cancers 2022, 14, 4174. https://doi.org/10.3390/cancers14174174
Lee C-U, Lee S-M, Chung J-H, Kang M, Sung H-H, Jeon H-G, Jeong B-C, Seo S-I, Jeon S-S, Lee H-M, et al. Clinical Utility of Prostate Health Index for Diagnosis of Prostate Cancer in Patients with PI-RADS 3 Lesions. Cancers. 2022; 14(17):4174. https://doi.org/10.3390/cancers14174174
Chicago/Turabian StyleLee, Chung-Un, Sang-Min Lee, Jae-Hoon Chung, Minyong Kang, Hyun-Hwan Sung, Hwang-Gyun Jeon, Byong-Chang Jeong, Seong-Il Seo, Seong-Soo Jeon, Hyun-Moo Lee, and et al. 2022. "Clinical Utility of Prostate Health Index for Diagnosis of Prostate Cancer in Patients with PI-RADS 3 Lesions" Cancers 14, no. 17: 4174. https://doi.org/10.3390/cancers14174174
APA StyleLee, C.-U., Lee, S.-M., Chung, J.-H., Kang, M., Sung, H.-H., Jeon, H.-G., Jeong, B.-C., Seo, S.-I., Jeon, S.-S., Lee, H.-M., & Song, W. (2022). Clinical Utility of Prostate Health Index for Diagnosis of Prostate Cancer in Patients with PI-RADS 3 Lesions. Cancers, 14(17), 4174. https://doi.org/10.3390/cancers14174174






