Surgical Principles of Primary Retroperitoneal Sarcoma in the Era of Personalized Treatment: A Review of the Frontline Extended Surgery
Abstract
Simple Summary
Abstract
1. Introduction
2. Frontline Extended Surgery: Background and Bases
3. International Collaboration in RPS Care
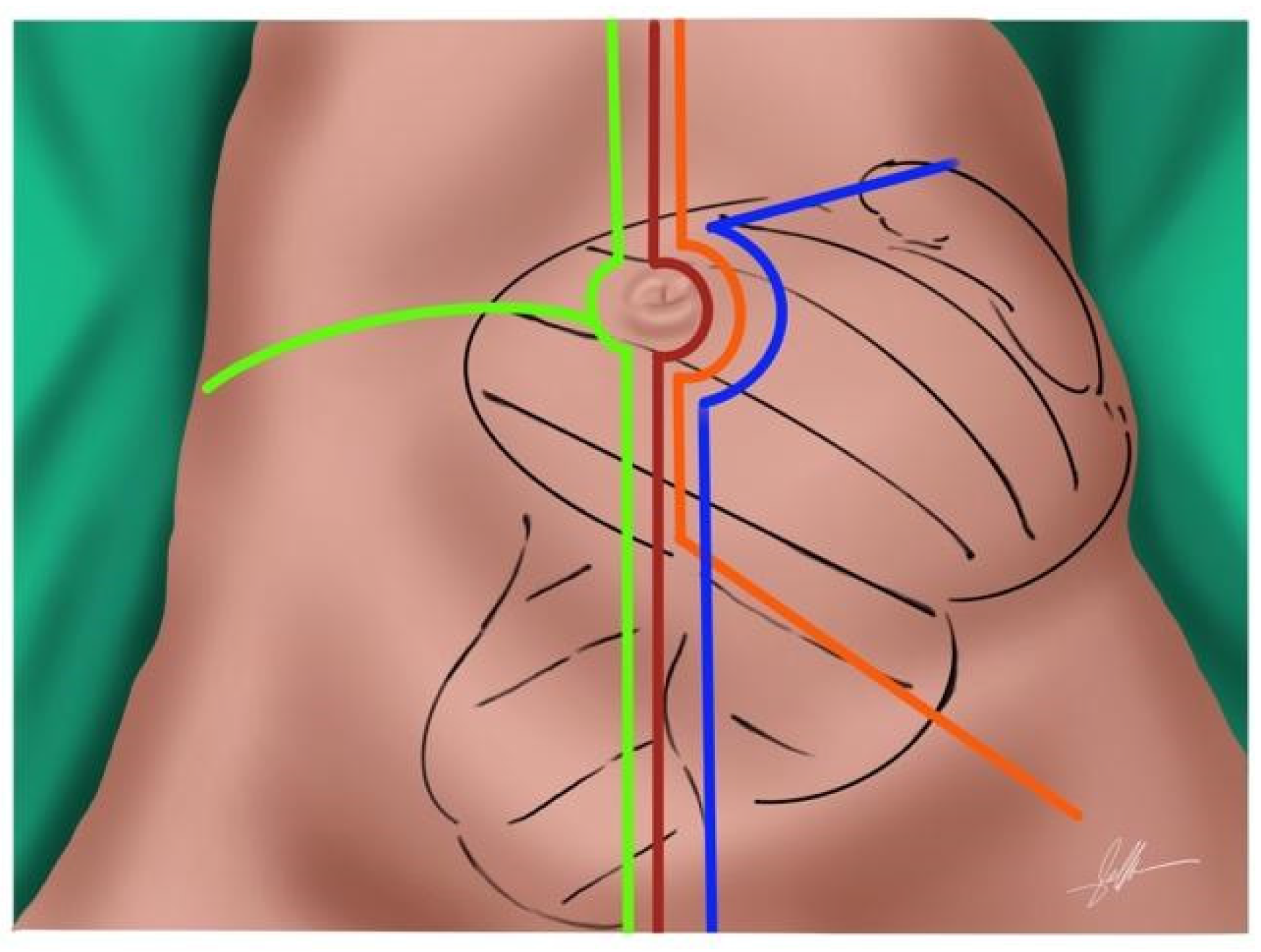
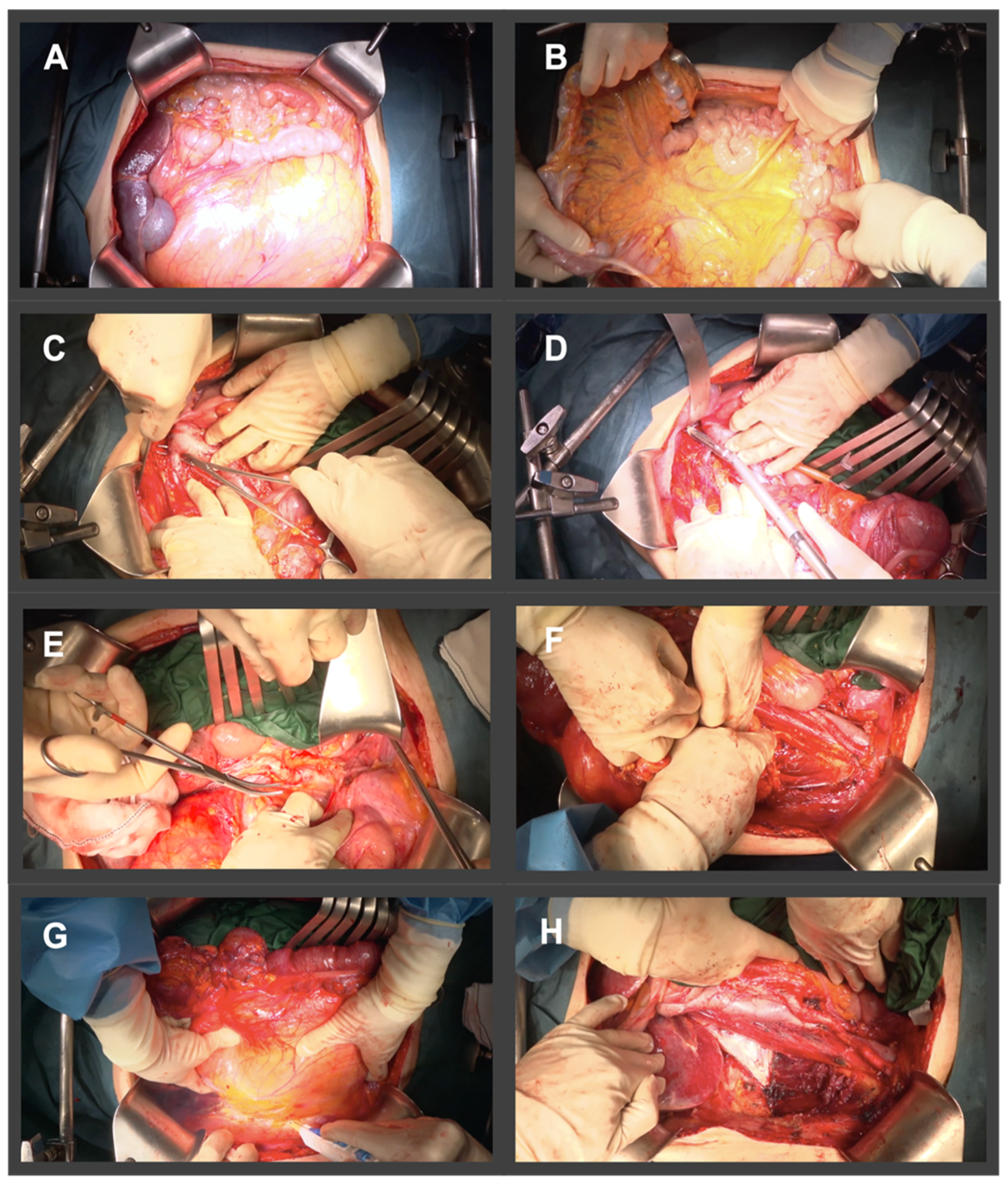
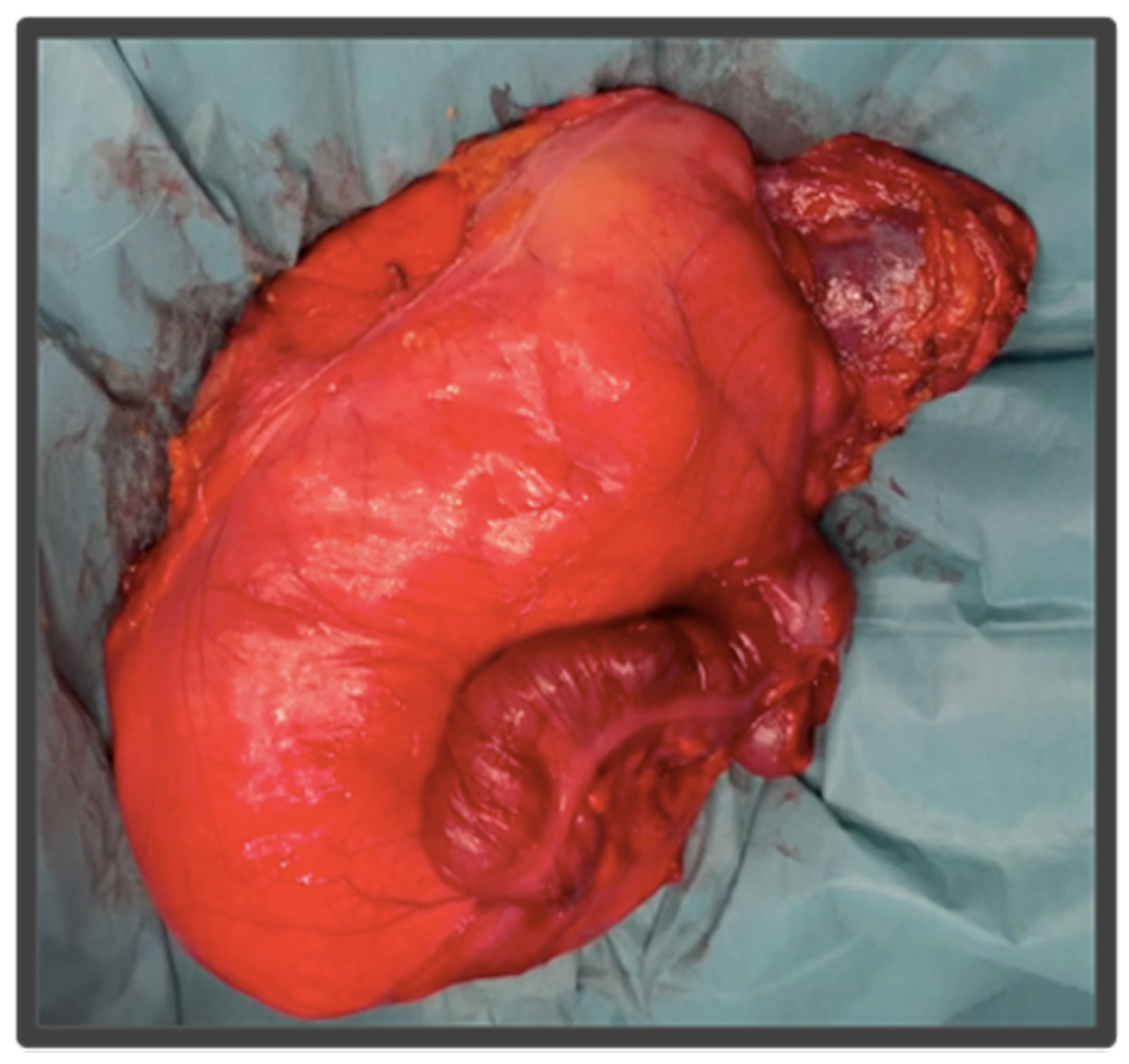
4. Standardized Surgical Technique of the Frontline Extended Approach
- Right side: right LPS may require a right medial visceral rotation en bloc with the tumor, to assess involvement of the IVC. A wide Kocher maneuver allows both duodenal retraction and access to the full extension of the infrahepatic cava vein. This approach will allow for the preservation of the duodenum and the head of the pancreas. The resection of the duodenum-pancreas does not improve disease-free survival and is in fact associated with the highest complication rates, therefore the aim of the surgery at this point is to pass through the tumor pseudocapsule (i.e., marginal dissection) releasing it from these organs. However, partial resection should be considered when the pancreatoduodenal junction dissection from the tumor leads to duodenal perforation due to a wall thinned by tumor compression or invasion. In extremely rare cases, duodenopancreatectomy is required.
- Left side: In left LPS a wide release of Treitz angle without injuring the duodenum is important. When there is a clear infiltration of the 3rd duodenal portion, we should add its resection with a reconstruction through a duodeno-jejunostomy. In left upper quadrant tumors, a distal spleno-pancreatectomy or even diaphragm resection is required [19,20].
5. Personalizing Surgery in Primary RPS
5.1. Histology
5.2. Localization
Localization and Technical Unresectability
5.3. Patient
6. Morbidity and Complications after Radical Resection of RPS
7. Role of Systemic Treatment and Radiotherapy in RPS
7.1. Systemic Therapy
7.2. Radiation Therapy
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Porter, G.A.; Baxter, N.N.; Pisters, P.W.T. Retroperitoneal sarcoma: A population-based analysis of epidemiology, surgery, and radiotherapy. Cancer 2006, 106, 1610–1616. [Google Scholar] [CrossRef] [PubMed]
- Storm, F.K.; Mahvi, D.M. Diagnosis and Management of Retroperitoneal Soft-tissue Sarcoma. Ann. Surg. 1991, 214, 2. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.J.; Leung, D.; Woodruff, J.M.; Brennan, M.F. Retroperitoneal Soft-Tissue Sarcoma Analysis of 500 Patients Treated and Followed at a Single Institution. Ann. Surg. 1998, 228, 355–365. [Google Scholar] [CrossRef]
- Gronchi, A.; Miceli, R.; Allard, M.A.; Callegaro, D.; Le Péchoux, C.; Fiore, M.; Honoré, C.; Sanfilippo, R.; Coppola, S.; Stacchiotti, S.; et al. Personalizing the Approach to Retroperitoneal Soft Tissue Sarcoma: Histology-specific Patterns of Failure and Postrelapse Outcome after Primary Extended Resection. Ann. Surg. Oncol. 2014, 22, 1447–1454. [Google Scholar] [CrossRef] [PubMed]
- Gronchi, A.; Vullo, S.L.; Fiore, M.; Mussi, C.; Stacchiotti, S.; Collini, P.; Lozza, L.; Pennacchioli, E.; Mariani, L.; Casali, P.G. Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients. J. Clin. Oncol. 2009, 27, 24–30. [Google Scholar] [CrossRef]
- Bonvalot, S.; Rivoire, M.; Castaing, M.; Stoeckle, E.; Le Cesne, A.; Blay, J.Y.; Laplanche, A. Primary Retroperitoneal Sarcomas: A Multivariate Analysis of Surgical Factors Associated with Local Control. J. Clin. Oncol. 2009, 27, 31–37. [Google Scholar] [CrossRef]
- Asencio Pascual, J.M.; Fernandez Hernandez, J.A.; Blanco Fernandez, G.; Muñoz Casares, C.; Álvarez Álvarez, R.; Fox Anzorena, B.; Lozano Borbalas, A.; Rodriguez Blanco, M.; Cantin Blázquez, S. Update in pelvic and retroperitoneal sarcoma management: The role of compartment surgery. Cir. Esp. 2019, 97, 480–488. [Google Scholar] [CrossRef]
- Karakousis, C.P.; Kontzogiou, K.; Driscoll, D.L. Resectability of retroperitoneal sarcomas: A matter of surgical technique? Eur. J. Surg. Oncol. 1995, 21, 617–622. [Google Scholar] [CrossRef]
- Swallow, C.J.; Strauss, D.C.; Bonvalot, S.; Rutkowski, P.; Desai, A.; Gladdy, R.A.; Gonzalez, R.; Gyorki, D.E.; Fairweather, M.; van Houdt, W.J.; et al. Management of Primary Retroperitoneal Sarcoma (RPS) in the Adult: An Updated Consensus Approach from the Transatlantic Australasian RPS Working Group. Ann. Surg. Oncol. 2021, 28, 7873–7888. [Google Scholar] [CrossRef]
- Callegaro, D.; Fiore, M.; Gronchi, A. Personalizing surgical margins in retroperitoneal sarcomas. Expert Rev. Anticancer. Ther. 2015, 15, 553–567. [Google Scholar] [CrossRef]
- Dangoor, A.; Seddon, B.; Gerrand, C.; Grimer, R.; Whelan, J.; Judson, I. UK guidelines for the management of soft tissue sarcomas. Clin. Sarcoma Res. 2016, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Gronchi, A.; Pollock, R. Surgery in retroperitoneal soft tissue sarcoma: A call for a consensus between Europe and North America. Ann. Surg. Oncol. 2011, 18, 2107–2110. [Google Scholar] [CrossRef] [PubMed]
- Raut, C.P.; Swallow, C.J. Editorial: Are radical compartmental resections for retroperitoneal sarcomas justified? Ann. Surg. Oncol. 2010, 17, 1481–1484. [Google Scholar] [CrossRef]
- Strauss, D.C.; Renne, S.L.; Gronchi, A. Adjacent, Adherent, Invaded: A Spectrum of Biologic Aggressiveness Rather Than a Rationale for Selecting Organ Resection in Surgery of Primary Retroperitoneal Sarcomas. Ann. Surg. Oncol. 2018, 25, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Fairweather, M.; Wang, J.; Jo, V.Y.; Baldini, E.H.; Bertagnolli, M.M.; Raut, C.P. Surgical Management of Primary Retroperitoneal Sarcomas: Rationale for Selective Organ Resection. Ann. Surg. Oncol. 2018, 25, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Fairweather, M.; Wang, J.; Jo, V.Y.; Baldini, E.H.; Bertagnolli, M.M.; Raut, C.P. Incidence and Adverse Prognostic Implications of Histopathologic Organ Invasion in Primary Retroperitoneal Sarcoma. J. Am. Coll. Surg. 2017, 224, 876–883. [Google Scholar] [CrossRef]
- Bonvalot, S.; Miceli, R.; Berselli, M.; Causeret, S.; Colombo, C.; Mariani, L.; Bouzaiene, H.; Le Péchoux, C.; Casali, P.G.; Le Cesne, A.; et al. Aggressive surgery in retroperitoneal soft tissue sarcoma carried out at high-volume centers is safe and is associated with improved local control. Ann. Surg. Oncol. 2010, 17, 1507–1514. [Google Scholar] [CrossRef]
- MacNeill, A.J.; Gronchi, A.; Miceli, R.; Bonvalot, S.; Swallow, C.J.; Hohenberger, P.; van Coevorden, F.; Rutkowski, P.; Callegaro, D.; Hayes, A.J.; et al. Postoperative Morbidity after Radical Resection of Primary Retroperitoneal Sarcoma. Ann. Surg. 2018, 267, 959–964. [Google Scholar] [CrossRef]
- Callegaro, D.; Raut, C.P.; Ng, D.; Strauss, D.C.; Honoré, C.; Stoeckle, E.; Bonvalot, S.; Haas, R.L.; Vassos, N.; Conti, L.; et al. Has the Outcome for Patients Who Undergo Resection of Primary Retroperitoneal Sarcoma Changed Over Time? A Study of Time Trends during the Past 15 years. Ann. Surg. 2021, 28, 1700–1709. [Google Scholar] [CrossRef]
- MacNeill, A.J.; Fiore, M. Surgical morbidity in retroperitoneal sarcoma resection. J. Surg. Oncol. 2018, 117, 56–61. [Google Scholar] [CrossRef]
- Pisters, P.W.T. Resection of some-but not all-clinically uninvolved adjacent viscera as part of surgery for retroperitoneal soft tissue sarcomas. J. Clin. Oncol. 2009, 27, 6–8. [Google Scholar] [CrossRef] [PubMed]
- Fairweather, M.; Gonzalez, R.J.; Strauss, D.; Raut, C.P. Current principles of surgery for retroperitoneal sarcomas. J. Surg. Oncol. 2018, 117, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Gronchi, A.; Miah, A.B.; Dei Tos, A.P.; Abecassis, N.; Bajpai, J.; Bauer, S.; Bonvalot, S.; Boukovinas, I.; Bovee, J.V.M.G.; Boye, K.; et al. Soft tissue and visceral sarcomas: ESMO–EURACAN–GENTURIS Clinical Practice Guidelines for diagnosis, treatment and follow-up☆. Ann. Oncol. 2021, 32, 1348–1365. [Google Scholar] [CrossRef] [PubMed]
- Bonvalot, S.; Raut, C.P.; Pollock, R.E.; Rutkowski, P.; Strauss, D.C.; Hayes, A.J.; Van Coevorden, F.; Fiore, M.; Stoeckle, E.; Hohenberger, P.; et al. Technical considerations in surgery for retroperitoneal sarcomas: Position paper from E-Surge, a master class in sarcoma surgery, and EORTC-STBSG. Ann. Surg. Oncol. 2012, 19, 2981–2991. [Google Scholar] [CrossRef] [PubMed]
- MacNeill, A.J.; Miceli, R.; Strauss, D.C.; Bonvalot, S.; Hohenberger, P.; Van Coevorden, F.; Rutkowski, P.; Callegaro, D.; Hayes, A.J.; Honoré, C.; et al. Post-relapse outcomes after primary extended resection of retroperitoneal sarcoma: A report from the Trans-Atlantic RPS Working Group. Cancer 2017, 123, 1971–1978. [Google Scholar] [CrossRef]
- Dingley, B.; Fiore, M.; Gronchi, A. Personalizing surgical margins in retroperitoneal sarcomas: An update. Expert Rev. Anticancer Ther. 2019, 19, 613–631. [Google Scholar] [CrossRef]
- Carbone, F.; Pizzolorusso, A.; di Lorenzo, G.; di Marzo, M.; Cannella, L.; Barretta, M.L.; Delrio, P.; Tafuto, S. Multidisciplinary management of retroperitoneal sarcoma: Diagnosis, prognostic factors and treatment. Cancers 2021, 13, 4016. [Google Scholar] [CrossRef]
- Gronchi, A.; Miceli, R.; Shurell, E.; Eilber, F.C.; Eilber, F.R.; Anaya, D.A.; Kattan, M.; Honoré, C.; Lev, D.C.; Colombo, C.; et al. Outcome prediction in primary resected retroperitoneal soft tissue sarcoma: Histology-specific overall survival and disease-free survival nomograms built on major sarcoma center data sets. J. Clin. Oncol. 2013, 31, 1649–1655. [Google Scholar] [CrossRef]
- Bonvalot, S.; Gronchi, A.; Hohenberger, P.; Litiere, S.; Pollock, R.E.; Raut, C.P. Management of Primary Retroperitoneal Sarcoma (RPS) in the Adult: A Consensus Approach from the Trans-Atlantic RPS Working Group. Ann. Surg. Oncol. 2015, 22, 256–263. [Google Scholar]
- Cates, J.M.M. The AJCC 8th edition staging system for soft tissue sarcoma of the extremities or trunk: A Cohort study of the SEER database. JNCCN J. Natl. Compr. Cancer Netw. 2018, 16, 144–152. [Google Scholar] [CrossRef]
- Watson, S.; Gruel, N.; le Loarer, F. New developments in the pathology and molecular biology of retroperitoneal sarcomas. Eur. J. Surg. Oncol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Renne, S.L.; Iwenofu, O.H. Pathology of retroperitoneal sarcomas: A brief review. J. Surg. Oncol. 2018, 117, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Anaya, D.A.; Lahat, G.; Wang, X.; Xiao, L.; Pisters, P.W.; Cormier, J.N.; Hunt, K.K.; Feig, B.W.; Lev, D.C.; Pollock, R.E. Postoperative nomogram for survival of patients with retroperitoneal sarcoma treated with curative intent. Ann. Oncol. 2010, 21, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Raut, C.P.; Miceli, R.; Strauss, D.C.; Swallow, C.J.; Hohenberger, P.; van Coevorden, F.; Rutkowski, P.; Fiore, M.; Callegaro, D.; Casali, P.G.; et al. External validation of a multi-institutional retroperitoneal sarcoma nomogram. Cancer 2016, 122, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Mastoraki, A.; Toska, F.; Tsiverdis, I.; Kyriazi, M.; Tsagkas, A.; Danias, N.; Smyrniotis, V.; Arkadopoulos, N. Retroperitoneal schwannomas: Dilemmas in diagnostic approach and therapeutic management. J. Gastrointest. Cancer 2013, 44, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.C.B.; Brennan, M.; Kuk, D.; Agaram, N.P.; Antonescu, C.R.; Qin, L.-X.; Moraco, N.; Crago, A.M.; Singer, S. Histology-based classification predicts pattern of recurrence and improves risk stratification in primary retroperitoneal sarcoma. Ann. Surg. 2016, 263, 593–600. [Google Scholar] [CrossRef]
- Gronchi, A.; Strauss, D.C.; Miceli, R.; Bonvalot, S.; Swallow, C.J.; Hohenberger, P.; Van Coevorden, F.; Rutkowski, P.; Callegaro, D.; Hayes, A.; et al. Variability in patterns of recurrence after resection of primary retroperitoneal sarcoma (RPS). A report on 1007 patients from the multi-institutional collaborative RPS working group. Ann. Surg. 2016, 263, 1002–1009. [Google Scholar] [CrossRef]
- Lopez, J.A.G.; Raventós, V.A.; Blanco, M.R.; Lopez-Pousa, A.; Bagué, S.; Abellán, M.; Folch, M.T. Differences between En Bloc Resection and Enucleation of Retroperitoneal Sarcomas. Cir. Esp. 2014, 92, 525–531. [Google Scholar]
- Almond, L.M.; Gronchi, A.; Strauss, D.; Jafri, M.; Ford, S.; Desai, A. Neoadjuvant and adjuvant strategies in retroperitoneal sarcoma. Eur. J. Surg. Oncol. 2018, 44, 571–579. [Google Scholar] [CrossRef]
- Ng, D.; Swallow, C.J. Decision-making for palliative versus curative intent treatment of retroperitoneal sarcoma (RPS). Chin. Clin. Oncol. 2018, 7, 40. [Google Scholar] [CrossRef]
- Gronchi, A.; Pollock, R.E. Quality of local treatment or biology of the tumor: Which are the trump cards for loco-regional control of retroperitoneal sarcoma? Ann. Surg. Oncol. 2013, 20, 2111–2113. [Google Scholar] [CrossRef] [PubMed]
- Cranshaw, I.M.; Gikas, P.D.; Fisher, C.; Thway, K.; Thomas, J.M.; Hayes, A.J. Clinical outcomes of extra-thoracic solitary fibrous tumours. Eur. J. Surg. Oncol. 2009, 35, 994–998. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.; Coert, J.H.; Flucke, U.E.; Slooff, W.-B.M.; Ho, V.K.; van der Graaf, W.T.; van Dalen, T.; van de Sande, M.A.; van Houdt, W.J.; Grünhagen, D.J.; et al. A nationwide cohort study on treatment and survival in patients with malignant peripheral nerve sheath tumours. Eur. J. Cancer 2020, 124, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, E.; Nessim, C. Retroperitoneal Sarcoma Care in 2021. Cancers 2022, 14, 1293. [Google Scholar] [CrossRef] [PubMed]
- Daugaard, S. Current soft-tissue sarcoma classifications. Eur. J. Cancer 2004, 40, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Schwarzbach, M.H.; Hormann, Y.; Hinz, U.; Leowardi, C.; Böckler, D.; Mechtersheimer, G.; Friess, H.; Büchler, M.W.; Allenberg, J.-R. Clinical results of surgery for retroperitoneal sarcoma with major blood vessel involvement. J. Vasc. Surg. 2006, 44, 46–55. [Google Scholar] [CrossRef]
- Davins, M.; Artigas, V.; López-Pousa, A.; Vela, S.; Latorre, J.; Escudero, J.R. Leiomyosarcoma of the Infrarenal Inferior Vena Cava: Management in Three Cases and a Review of the Literature. EJVES Extra 2007, 14, 19–21. [Google Scholar] [CrossRef][Green Version]
- Fiore, M.; Colombo, C.; Locati, P.; Berselli, M.; Radaelli, S.; Morosi, C.; Casali, P.G.; Gronchi, A. Surgical technique, morbidity, and outcome of primary retroperitoneal sarcoma involving inferior vena cava. Ann. Surg. Oncol. 2012, 19, 511–518. [Google Scholar] [CrossRef]
- Stucky, C.-C.H.; Johnson, K.N.; Gray, R.J.; Pockaj, B.A.; Ocal, I.T.; Rose, P.S.; Wasif, N. Malignant Peripheral Nerve Sheath Tumors (MPNST): The Mayo Clinic experience. Ann. Surg. Oncol. 2011, 19, 878–885. [Google Scholar] [CrossRef]
- Roeder, F.; Krempien, R. Intraoperative radiation therapy (IORT) in soft-tissue sarcoma. Radiat. Oncol. 2017, 12, 20. [Google Scholar] [CrossRef]
- Roeder, F.; Morillo, V.; Saleh-Ebrahimi, L.; Calvo, F.A.; Poortmans, P.; Albiach, C.F. Intraoperative radiation therapy (IORT) for soft tissue sarcoma—ESTRO IORT Task Force/ACROP recommendations. Radiother. Oncol. 2020, 150, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Mullen, J.T.; van Houdt, W. Soft tissue tumors of the pelvis: Technical and histological considerations. J. Surg. Oncol. 2018, 117, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, P.L.; Mullen, J.T. Management of the “Other” retroperitoneal sarcomas. J. Surg. Oncol. 2018, 117, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Abbott, A.M.; Habermann, E.B.; Parsons, H.M.; Tuttle, T.; Al-Refaie, W. Prognosis for primary retroperitoneal sarcoma survivors: A conditional survival analysis. Cancer 2012, 118, 3321–3329. [Google Scholar] [CrossRef] [PubMed]
- Penel, N.; Glabbeke, M.; Mathoulin-Pelissier, S.; Judson, I.; Sleijfer, S.; Bui, B.; Schoffski, P.; Ouali, M.; Marreaud, S.; Brouste, V.; et al. Performance status is the most powerful risk factor for early death among patients with advanced soft tissue sarcomaThe European Organisation for Research and Treatment of Cancer—Soft Tissue and Bone Sarcoma Group (STBSG) and French Sarcoma Group (FSG) study. Br. J. Cancer 2011, 104, 1544–1550. [Google Scholar]
- Raedkjaer, M.; Maretty-Kongstad, K.; Baad-Hansen, T.; Jørgensen, P.H.; Safwat, A.; Vedsted, P.; Petersen, M.M.; Hovgaard, T.; Nymark, T.; Keller, J. The impact of comorbidity on mortality in danish sarcoma patients from 2000–2013: A nationwide population-based multicentre study. PLoS ONE 2018, 13, e0198933. [Google Scholar] [CrossRef]
- West, H.; Jin, J.O. Performance status in patients with cancer. JAMA Oncol. 2015, 1, 998. [Google Scholar] [CrossRef]
- Khorana, A.A.; Mangu, P.B.; Berlin, J.; Engebretson, A.; Hong, T.S.; Maitra, A.; Mohile, S.G.; Mumber, M.; Schulick, R.; Shapiro, M.; et al. Potentially curable pancreatic cancer: American society of clinical oncology clinical practice guideline. J. Clin. Oncol. 2016, 34, 2541–2556. [Google Scholar] [CrossRef]
- Previtali, P.; Fiore, M.; Colombo, J.; Arendar, I.; Fumagalli, L.; Pizzocri, M.; Colombo, C.; Rampello, N.N.; Mariani, L.; Gronchi, A.; et al. Malnutrition and Perioperative Nutritional Support in Retroperitoneal Sarcoma Patients: Results from a Prospective Study. Ann. Surg. Oncol. 2019, 27, 2025–2032. [Google Scholar] [CrossRef]
- Tseng, W.H.; Martinez, S.R.; Tamurian, R.M.; Chen, S.L.; Bold, R.J.; Canter, R.J. Contiguous organ resection is safe in patients with retroperitoneal sarcoma: An ACS-NSQIP analysis. J. Surg. Oncol. 2011, 103, 390–394. [Google Scholar] [CrossRef]
- Hull, M.A.; Niemierko, A.; Haynes, A.B.; Jacobson, A.; Chen, Y.L.; Delaney, T.F.; Mullen, J.T. Post-operative renal function following nephrectomy as part of en bloc resection of retroperitoneal sarcoma (RPS). J. Surg. Oncol. 2015, 112, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Callegaro, D.; Miceli, R.; Brunelli, C.; Colombo, C.; Sanfilippo, R.; Radaelli, S.; Casali, P.G.; Caraceni, A.; Gronchi, A.; Fiore, M. Long-term morbidity after multivisceral resection for retroperitoneal sarcoma. Br. J. Surg. 2015, 102, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Fiore, M.; Baia, M.; Conti, L.; Piccioni, F.; Mariani, L.; Pasquali, S.; Seregni, E.; Maltese, G.; Galizia, M.; Radaelli, S.; et al. Residual Adrenal Function After Multivisceral Resection With Adrenalectomy in Adult Patients. JAMA Surg. 2022, 157, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, R.; Eckert, F.; Gelfert, D.; Strohäker, J.; Beltzer, C.; Ladurner, R. Perioperative strategy and outcome in giant retroperitoneal dedifferentiated liposarcoma—results of a retrospective cohort study. World J. Surg. Oncol. 2020, 18, 296. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.J.; Oladeru, O.T.; Farrugia, M.K.; Shekher, R.; Iovoli, A.J.; Singh, A.K. Evaluation of Preoperative Chemotherapy or Radiation and Overall Survival in Patients with Nonmetastatic, Resectable Retroperitoneal Sarcoma. JAMA Netw. Open 2020, 3, e2025529. [Google Scholar] [CrossRef]
- Roeder, F.; Ulrich, A.; Habl, G.; Uhl, M.; Saleh-Ebrahimi, L.; E Huber, P.; Schulz-Ertner, D.; Nikoghosyan, A.V.; Alldinger, I.; Krempien, R.; et al. Clinical Phase I/II trial to Investigate Preoperative Dose-Escalated Intensity-Modulated Radiation Therapy (IMRT) and Intraoperative Radiation Therapy (IORT) in patients with retroperitoneal soft tissue sarcoma: Interim analysis. BMC Cancer 2014, 14, 617. [Google Scholar] [CrossRef]
- Cardona, K. The STRASS trial: An important step in the right direction. Lancet Oncol. 2020, 21, 1257–1258. [Google Scholar] [CrossRef]
- Bonvalot, S.; Gronchi, A.; Le Péchoux, C.; Swallow, C.J.; Strauss, D.; Meeus, P.; van Coevorden, F.; Stoldt, S.; Stoeckle, E.; Rutkowski, P.; et al. Preoperative radiotherapy plus surgery versus surgery alone for patients with primary retroperitoneal sarcoma (EORTC-62092: STRASS): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2020, 21, 1366–1377. [Google Scholar] [CrossRef]
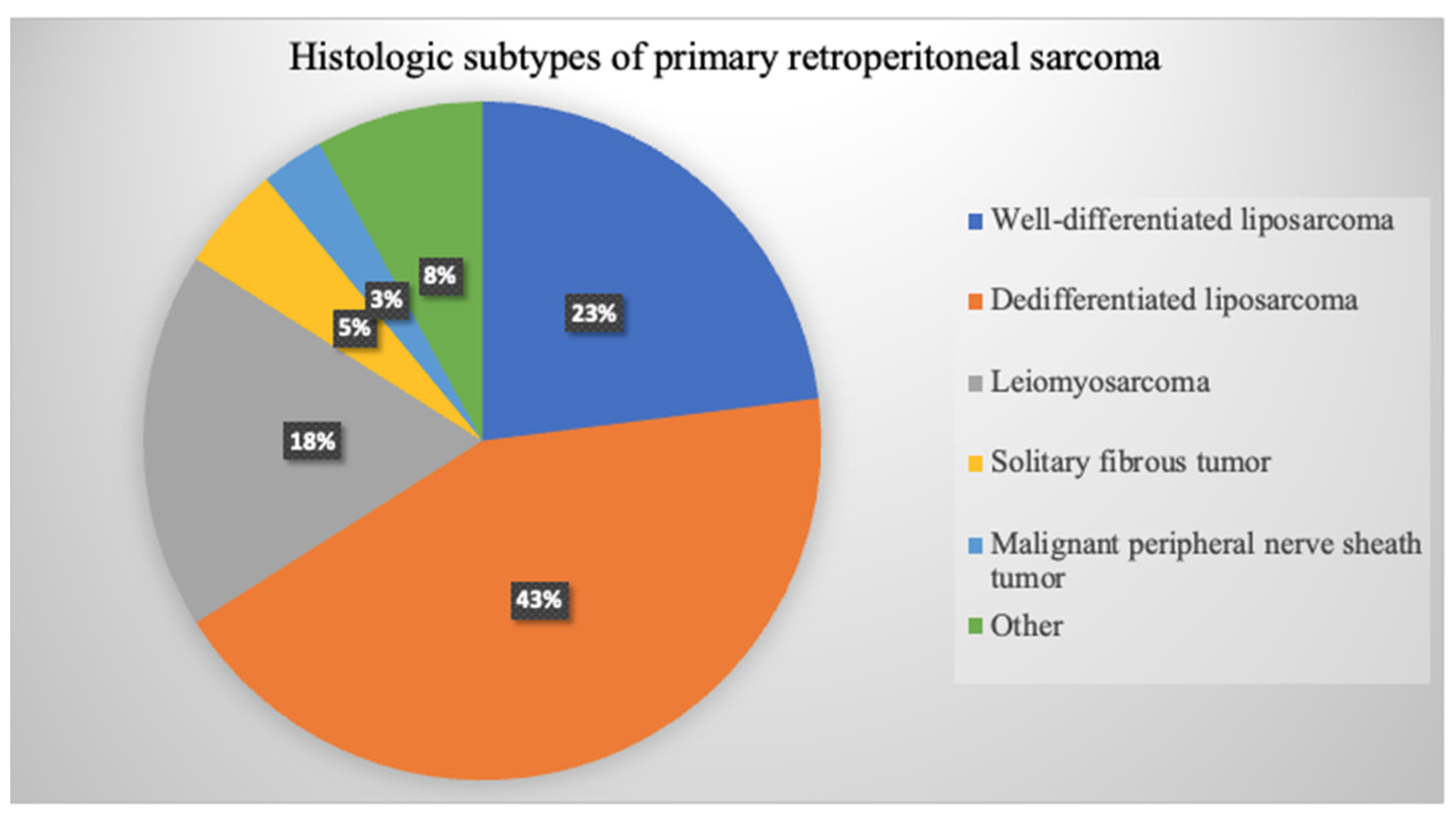
| RPS Histology | Pattern of Spread | Disease Failure 5-Year | Surgical Management |
|---|---|---|---|
| WDLPS | Adipose infiltration | LR (19–39%) >> DM (0%) | Extended en-bloc resection requiring ipsilateral retroperitoneal fat resection |
| Multilobulated | |||
| Indistinct borders | |||
| DDLPS | Adipose and visceral infiltration | G2: LR (44%) > DM (10%) G3: LR (33%) << DM (44%) | Extended en-bloc resection requiring ipsilateral retroperitoneal fat resection |
| Multilobulated | |||
| Indistinct borders | |||
| LMS | Distinct borders | LR (6–16%) << DM (55–56%) | En-bloc resection with vascular structures |
| May preserve adjacent critical structures | |||
| SFT | Distinct borders | LR (4–8%) < DM (17%) | En-bloc resection |
| Preservation of adjacent viscera and critical structures | |||
| MPNST | Distinct borders | LR (20–35%) > DM (12–13%) | Retroperitoneal approach |
| En-bloc resection with associated neurovascular structures | |||
| May preserve adjacent critical structures |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Munoz, P.; Bretcha-Boix, P.; Artigas, V.; Asencio, J.M. Surgical Principles of Primary Retroperitoneal Sarcoma in the Era of Personalized Treatment: A Review of the Frontline Extended Surgery. Cancers 2022, 14, 4091. https://doi.org/10.3390/cancers14174091
Munoz P, Bretcha-Boix P, Artigas V, Asencio JM. Surgical Principles of Primary Retroperitoneal Sarcoma in the Era of Personalized Treatment: A Review of the Frontline Extended Surgery. Cancers. 2022; 14(17):4091. https://doi.org/10.3390/cancers14174091
Chicago/Turabian StyleMunoz, Paula, Pedro Bretcha-Boix, Vicente Artigas, and José Manuel Asencio. 2022. "Surgical Principles of Primary Retroperitoneal Sarcoma in the Era of Personalized Treatment: A Review of the Frontline Extended Surgery" Cancers 14, no. 17: 4091. https://doi.org/10.3390/cancers14174091
APA StyleMunoz, P., Bretcha-Boix, P., Artigas, V., & Asencio, J. M. (2022). Surgical Principles of Primary Retroperitoneal Sarcoma in the Era of Personalized Treatment: A Review of the Frontline Extended Surgery. Cancers, 14(17), 4091. https://doi.org/10.3390/cancers14174091






