Patients with Metachronous Peritoneal Metastatic Mucinous Colorectal Adenocarcinoma Benefit More from Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) than Their Synchronous Counterparts
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Details of CRS + HIPEC
2.3. Clinical Characteristics
2.4. Statistical Analysis
3. Results
3.1. Comparisions between the Synchronous and Metachronous Metastasis Groups
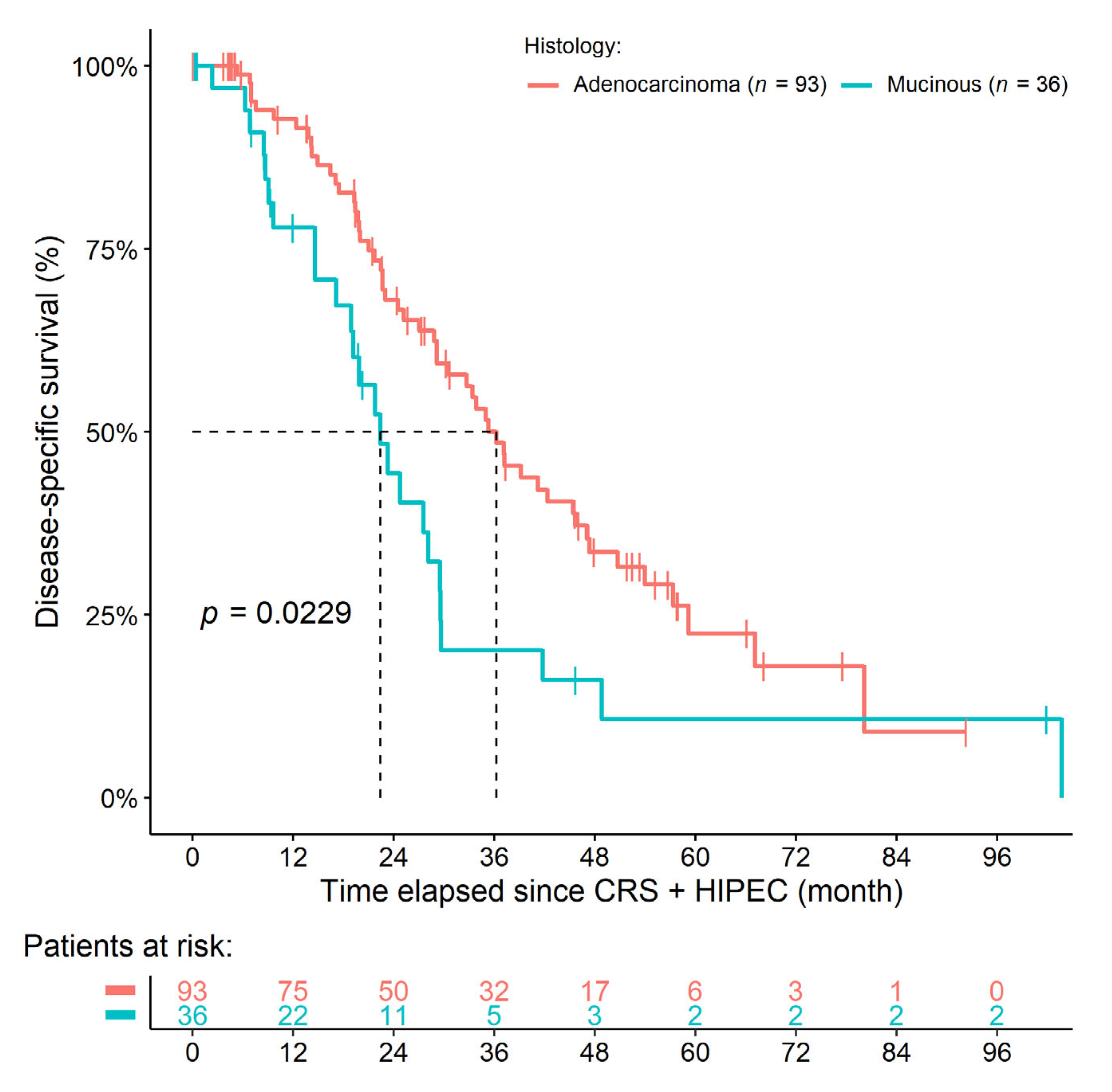
3.2. Comparisions of AC and MAC Histology within the Synchronous Metastasis Group
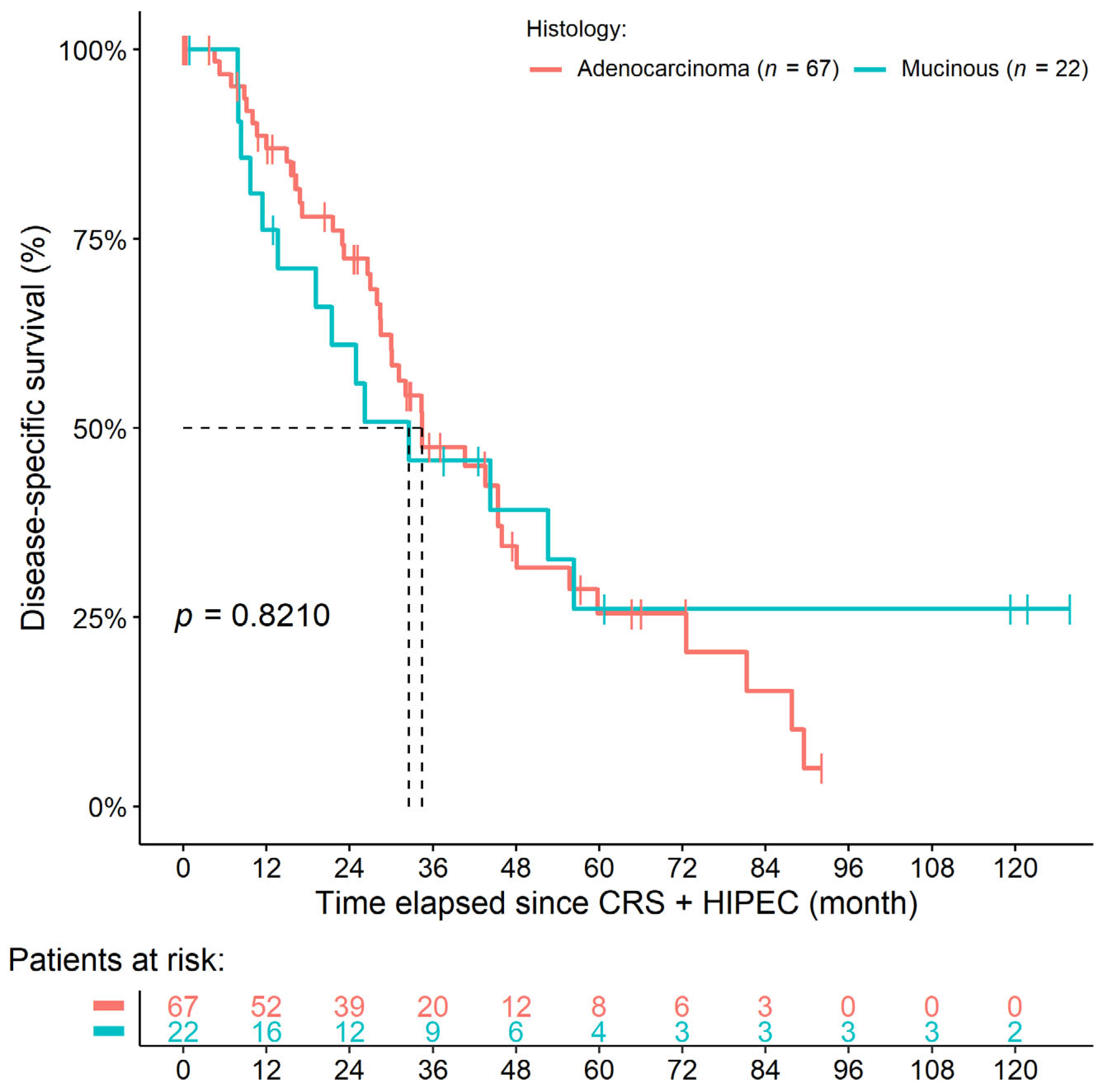
3.3. Comparisions of AC and MAC Histology within the Metachronous Metastasis Group
3.4. Comparisons of All Four Study Groups
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kim, C.H. Treatment for Peritoneal Metastasis of Patients with Colorectal Cancer. Ann. Coloproctol. 2021, 37, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Breuer, E.; Hebeisen, M.; Schneider, M.A.; Roth, L.; Pauli, C.; Frischer-Ordu, K.; Eden, J.; Pache, B.; Steffen, T.; Hübner, M.; et al. Site of Recurrence and Survival After Surgery for Colorectal Peritoneal Metastasis. JNCI J. Natl. Cancer Inst. 2021, 113, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- Glehen, O.; Kwiatkowski, F.; Sugarbaker, P.; Elias, D.; Levine, E.; De Simone, M.; Barone, R.; Yonemura, Y.; Cavaliere, F.; Quenet, F.; et al. Cytoreductive Surgery Combined with Perioperative Intraperitoneal Chemotherapy for the Management of Peritoneal Carcinomatosis from Colorectal Cancer: A Multi-Institutional Study. J. Clin. Oncol. 2004, 22, 3284–3292. [Google Scholar] [CrossRef] [PubMed]
- Goéré, D.; Malka, D.; Tzanis, D.; Gava, V.; Boige, V.; Eveno, C.; Maggiori, L.; Dumont, F.; Ducreux, M.; Elias, D. Is There a Possibility of a Cure in Patients with Colorectal Peritoneal Carcinomatosis Amenable to Complete Cytoreductive Surgery and Intraperitoneal Chemotherapy? Ann. Surg. 2013, 257, 1065–1071. [Google Scholar] [CrossRef]
- Verwaal, V.J.; van Ruth, S.; de Bree, E.; van Sloothen, G.W.; van Tinteren, H.; Boot, H.; Zoetmulder, F.A. Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol 2003, 21, 3737–3743. [Google Scholar] [CrossRef]
- Elias, D.; Delpero, J.R.; Sideris, L.; Benhamou, E.; Pocard, M.; Baton, O.; Giovannini, M.; Lasser, P. Treatment of Peritoneal Carcinomatosis From Colorectal Cancer: Impact of Complete Cytoreductive Surgery and Difficulties in Conducting Randomized Trials. Ann. Surg. Oncol. 2004, 11, 518–521. [Google Scholar] [CrossRef]
- Cashin, P.; Mahteme, H.; Spång, N.; Syk, I.; Frödin, J.; Torkzad, M.; Glimelius, B.; Graf, W. Cytoreductive surgery and intraperitoneal chemotherapy versus systemic chemotherapy for colorectal peritoneal metastases: A randomised trial. Eur. J. Cancer 2016, 53, 155–162. [Google Scholar] [CrossRef]
- Quenet, F.; Elias, D.; Roca, L.; Goere, D.; Ghouti, L.; Pocard, M.; Facy, O.; Arvieux, C.; Lorimier, G.; Pezet, D.; et al. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy versus cytoreductive surgery alone for colorectal peritoneal metastases (PRODIGE 7): A multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 2021, 22, 256–266. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network (NCCN). NCCN Guidelines: Colon cancer (Version 1.2022). Available online: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1428 (accessed on 15 July 2022).
- National Comprehensive Cancer Network (NCCN). NCCN Guidelines: Rectal Cancer (Version 1.2022). Available online: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1461 (accessed on 15 July 2022).
- Leopoldo, S.; Lorena, B.; Cinzia, A.; Gabriella, D.C.; Angela Luciana, B.; Renato, C.; Antonio, M.; Carlo, S.; Cristina, P.; Stefano, C.; et al. Two Subtypes of Mucinous Adenocarcinoma of The Colorectum: Clinicopathological and Genetic Features. Ann. Surg. Oncol. 2008, 15, 1429–1439. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- van Eden, W.; Kok, N.; Woensdregt, K.; Huitema, A.; Boot, H.; Aalbers, A. Safety of intraperitoneal Mitomycin C versus intraperitoneal oxaliplatin in patients with peritoneal carcinomatosis of colorectal cancer undergoing cytoreductive surgery and HIPEC. Eur. J. Surg. Oncol. EJSO 2018, 44, 220–227. [Google Scholar] [CrossRef]
- Jessup, J.; Goldberg, R.; Asare, E.; Benson, A.; Brierley, J.; Chang, G.; Chen, V.; Compton, C.; De Nardi, P.; Goodman, K.; et al. Colon and Rectum. In AJCC Cancer Staging Manual, 8th ed.; Amin, M., Edge, S., Greene, F., Byrd, D., Brookland, R., Washington, M., Gershenwald, J., Compton, C., Hess, K., Sullivan, D., et al., Eds.; Springer International Publishing: Chicago, IL, USA, 2018; pp. 251–274. [Google Scholar]
- Weiser, M.R. AJCC 8th Edition: Colorectal Cancer. Ann Surg Oncol 2018, 25, 1454–1455. [Google Scholar] [CrossRef] [PubMed]
- Baran, B.; Mert Ozupek, N.; Yerli Tetik, N.; Acar, E.; Bekcioglu, O.; Baskin, Y. Difference between Left-Sided and Right-Sided Colorectal Cancer: A Focused Review of Literature. Gastroenterol. Res. 2018, 11, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Paschke, S.; Jafarov, S.; Staib, L.; Kreuser, E.-D.; Maulbecker-Armstrong, C.; Roitman, M.; Holm, T.; Harris, C.C.; Link, K.-H.; Kornmann, M. Are Colon and Rectal Cancer Two Different Tumor Entities? A Proposal to Abandon the Term Colorectal Cancer. Int. J. Mol. Sci. 2018, 19, 2577. [Google Scholar] [CrossRef] [PubMed]
- Jacquet, P.; Sugarbaker, P.H. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. In Peritoneal Carcinomatosis: Principles of Management; Sugarbaker, P.H., Ed.; Springer US: Boston, MA, USA, 1996; Volume 82, pp. 359–374. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Luo, C.; Cen, S.; Ding, G.; Wu, W. Mucinous colorectal adenocarcinoma: Clinical pathology and treatment options. Cancer Commun. 2019, 39, 13. [Google Scholar] [CrossRef]
- Hugen, N.; van Beek, J.; De Wilt, J.H.W.; Nagtegaal, I. Insight into Mucinous Colorectal Carcinoma: Clues from Etiology. Ann. Surg. Oncol. 2014, 21, 2963–2970. [Google Scholar] [CrossRef]
- Huang, A.; Yang, Y.; Shi, J.-Y.; Li, Y.-K.; Xu, J.-X.; Cheng, Y.; Gu, J. Mucinous adenocarcinoma: A unique clinicopathological subtype in colorectal cancer. World J. Gastrointest. Surg. 2021, 13, 1567–1583. [Google Scholar] [CrossRef]
- Reynolds, I.S.; O’Connell, E.; Fichtner, M.; McNamara, D.A.; Kay, E.W.; Prehn, J.H.M.; Furney, S.J.; Burke, J.P. Mucinous adenocarcinoma is a pharmacogenomically distinct subtype of colorectal cancer. Pharm. J. 2019, 20, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Byrd, J.C.; Bresalier, R. Mucins and mucin binding proteins in colorectal cancer. Cancer Metastasis Rev. 2004, 23, 77–99. [Google Scholar] [CrossRef]
- Bresalier, R.; Niv, Y.; Byrd, J.C.; Duh, Q.Y.; Toribara, N.W.; Rockwell, R.W.; Dahiya, R.; Kim, Y.S. Mucin production by human colonic carcinoma cells correlates with their metastatic potential in animal models of colon cancer metastasis. J. Clin. Investig. 1991, 87, 1037–1045. [Google Scholar] [CrossRef]
- Reynolds, I.S.; Fichtner, M.; McNamara, D.A.; Kay, E.W.; Prehn, J.H.; Burke, J.P. Mucin glycoproteins block apoptosis; promote invasion, proliferation, and migration; and cause chemoresistance through diverse pathways in epithelial cancers. Cancer Metastasis Rev. 2019, 38, 237–257. [Google Scholar] [CrossRef]
- Song, W.; Wu, S.-J.; He, Y.-L.; Cai, S.-R.; Zhang, C.-H.; Zhang, X.-H.; Zhan, W.-H. Clinicopathologic features and survival of patients with colorectal mucinous, signet-ring cell or non-mucinous adenocarcinoma: Experience at an institution in southern China. Chin. Med J. 2009, 122, 1486–1491. [Google Scholar] [PubMed]
- Nozoe, T.; Anai, H.; Nasu, S.; Sugimachi, K. Clinicopathological characteristics of mucinous carcinoma of the colon and rectum. J. Surg. Oncol. 2000, 75, 103–107. [Google Scholar] [CrossRef]
- Reynolds, I.S.; Furney, S.J.; Kay, E.W.; McNamara, D.A.; Prehn, J.H.M.; Burke, J.P. Meta-analysis of the molecular associations of mucinous colorectal cancer. Br. J. Surg. 2019, 106, 682–691. [Google Scholar] [CrossRef] [PubMed]
- Melis, M.; Hernandez, J.; Siegel, E.M.; McLoughlin, J.M.; Ly, Q.P.; Nair, R.M.; Lewis, J.M.; Jensen, E.H.; Alvarado, M.D.; Coppola, D.; et al. Gene Expression Profiling of Colorectal Mucinous Adenocarcinomas. Dis. Colon Rectum 2010, 53, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, Y.; Huang, J.; Wu, X.; Tang, R.; Huang, Q.; Xu, Y.; Peng, X.; Fu, K.; Xiao, S. Mucinous histology is associated with poor prognosis in locally advanced colorectal adenocarcinoma treated with postoperative first-line adjuvant chemotherapy: A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Fields, A.C.; Lu, P.; Goldberg, J.; Irani, J.; Bleday, R.; Melnitchouk, N. The role of adjuvant chemotherapy in stage II and III mucinous colon cancer. J. Surg. Oncol. 2019, 120, 1190–1200. [Google Scholar] [CrossRef]
- Huang, Y.; Ge, K.; Fu, G.; Chu, J.; Wei, W. Mucinous Histology Might Be an Indicator for Enhanced Survival Benefit of Chemotherapy in Stage II Colon Cancer. Front. Med. 2020, 7, 205. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, R.; Alam, M.; Hasegawa, M.; Uchida, Y.; Al-Obaid, O.; Kharbanda, S.; Kufe, D. Targeting MUC1-C inhibits the AKT-S6K1-elF4A pathway regulating TIGAR translation in colorectal cancer. Mol Cancer 2017, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Le, D.T.; Uram, J.N.; Wang, H.; Bartlett, B.R.; Kemberling, H.; Eyring, A.D.; Skora, A.D.; Luber, B.S.; Azad, N.S.; Laheru, D.; et al. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N. Engl. J. Med. 2015, 372, 2509–2520. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Freeman, G.J. The microsatellite instable subset of colorectal cancer is a particularly good candidate for checkpoint blockade immunotherapy. Cancer Discov. 2015, 5, 16–18. [Google Scholar] [CrossRef]
- Kim, J.H.; Park, H.E.; Cho, N.Y.; Lee, H.S.; Kang, G.H. Characterisation of PD-L1-positive subsets of microsatellite-unstable colorectal cancers. Br. J. Cancer 2016, 115, 490–496. [Google Scholar] [CrossRef]
- Overman, M.J.; McDermott, R.; Leach, J.L.; Lonardi, S.; Lenz, H.-J.; Morse, M.A.; Desai, J.; Hill, A.; Axelson, M.; Moss, R.A.; et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): An open-label, multicentre, phase 2 study. Lancet Oncol. 2017, 18, 1182–1191. [Google Scholar] [CrossRef]
- Overman, M.J.; Lonardi, S.; Wong, K.Y.M.; Lenz, H.-J.; Gelsomino, F.; Aglietta, M.; Morse, M.A.; Van Cutsem, E.; McDermott, R.; Hill, A.; et al. Durable Clinical Benefit with Nivolumab Plus Ipilimumab in DNA Mismatch Repair–Deficient/Microsatellite Instability–High Metastatic Colorectal Cancer. J. Clin. Oncol. 2018, 36, 773–779. [Google Scholar] [CrossRef]
- Lipson, E.J.; Sharfman, W.H.; Drake, C.G.; Wollner, I.; Taube, J.M.; Anders, R.A.; Xu, H.; Yao, S.; Pons, A.; Chen, L.; et al. Durable Cancer Regression Off-Treatment and Effective Reinduction Therapy with an Anti-PD-1 Antibody. Clin. Cancer Res. 2013, 19, 462–468. [Google Scholar] [CrossRef]
- Hallam, S.; Tyler, R.; Price, M.; Beggs, A.; Youssef, H. Meta-analysis of prognostic factors for patients with colorectal peritoneal metastasis undergoing cytoreductive surgery and heated intraperitoneal chemotherapy. BJS Open 2019, 3, 585–594. [Google Scholar] [CrossRef]
- Kwakman, R.; Schrama, A.M.; van Olmen, J.P.; Otten, R.H.; Klerk, E.S.D.L.-D.; de Cuba, E.M.; Kazemier, G.; Velde, E.A.T. Clinicopathological Parameters in Patient Selection for Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy for Colorectal Cancer Metastases. Ann. Surg. 2016, 263, 1102–1111. [Google Scholar] [CrossRef]
- Van Oudheusden, T.; Braam, H.; Nienhuijs, S.; Wiezer, M.; Van Ramshorst, B.; Luyer, P.; de Hingh, I. Poor outcome after cytoreductive surgery and HIPEC for colorectal peritoneal carcinomatosis with signet ring cell histology. J. Surg. Oncol. 2014, 111, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Dietz, M.V.; van Kooten, J.P.; Said, I.; Brandt-Kerkhof, A.R.M.; Verhoef, C.; Bremers, A.J.A.; de Wilt, J.H.W.; de Reuver, P.R.; Madsen, E.V.E. Survival Outcomes after Cytoreductive Surgery with Hyperthermic Intraperitoneal Chemotherapy in Patients with Synchronous versus Metachronous Onset of Peritoneal Metastases of Colorectal Carcinoma. Ann. Surg. Oncol. 2022. [Google Scholar] [CrossRef]
- Numata, M.; Shiozawa, M.; Watanabe, T.; Tamagawa, H.; Yamamoto, N.; Morinaga, S.; Watanabe, K.; Godai, T.; Oshima, T.; Fujii, S.; et al. The clinicopathological features of colorectal mucinous adenocarcinoma and a therapeutic strategy for the disease. World J. Surg. Oncol. 2012, 10, 109. [Google Scholar] [CrossRef] [PubMed]
- Du, W.; Mah, J.T.L.; Lee, J.; Sankila, R.; Sankaranarayanan, R.; Chia, K.S. Incidence and Survival of Mucinous Adenocarcinoma of the Colorectum: A Population-Based Study From an Asian Country. Dis. Colon Rectum 2004, 47, 78–85. [Google Scholar] [CrossRef]
- Xie, L.; Villeneuve, P.; Shaw, A. Survival of patients diagnosed with either colorectal mucinous or non-mucinous adenocarcinoma: A population-based study in Canada. Int. J. Oncol. 2009, 34, 1109–1115. [Google Scholar] [CrossRef]
- Huang, Y.; Alzahrani, N.A.; Liauw, W.; Arrowaili, A.; Morris, D.L. Survival difference between mucinous vs. non-mucinous colorectal cancer following cytoreductive surgery and intraperitoneal chemotherapy. Int. J. Hyperth. 2018, 35, 298–304. [Google Scholar] [CrossRef]
- Sugarbaker, P.H. Mucinous colorectal carcinoma. J. Surg. Oncol. 2001, 77, 282–283. [Google Scholar] [CrossRef]
- Rovers, K.P.; Bakkers, C.; Simkens, G.; Burger, J.W.A.; Nienhuijs, S.W.; Creemers, G.M.; Thijs, A.M.J.; Brandt-Kerkhof, A.R.M.; Madsen, E.V.E.; Ayez, N.; et al. Perioperative systemic therapy and cytoreductive surgery with HIPEC versus upfront cytoreductive surgery with HIPEC alone for isolated resectable colorectal peritoneal metastases: Protocol of a multicentre, open-label, parallel-group, phase II-III, randomised, superiority study (CAIRO6). BMC Cancer 2019, 19, 1–15. [Google Scholar] [CrossRef]

| Clinical Characteristics | Synchronous PM (n = 129) | sAC (n = 93) | sMAC (n = 36) | Crude p-Value | Adjusted p-Value |
|---|---|---|---|---|---|
| Stage T (size of tumor) 1 | 0.0518 | 1.0000 | |||
| 1–2 | 3 (2.3%) | 3 (3.2%) | 0 (0%) | ||
| 3 | 31 (24.0%) | 27 (29.0%) | 4 (11.1%) | ||
| 4 | 93 (72.1%) | 62 (66.7%) | 31 (86.1%) | ||
| Stage N (lymph node metastases) 1 | 0.0343 | 1.0000 | |||
| 0 | 23 (17.8%) | 14 (15.1%) | 9 (25.0%) | ||
| 1 | 33 (25.6%) | 29 (31.2%) | 4 (11.1%) | ||
| 2–3 | 71 (55.0%) | 48 (51.6%) | 23 (63.9%) | ||
| Lineage of chemotherapy | 0.0201 | 1.0000 | |||
| First line | 90 (69.8%) | 70 (75.3%) | 20 (55.6%) | ||
| Second line | 8 (6.2%) | 7 (7.5%) | 1 (2.8%) | ||
| Third line | 3 (2.3%) | 1 (1.1%) | 2 (5.6%) | ||
| Previous partial peritonectomy 2 | 30 (23.3%) | 27 (29.0%) | 3 (8.3%) | 0.0114 | 0.6959 |
| Peritoneal carcinomatosis index | 7.67 ± 6.63 | 6.69 ± 5.83 | 10.22 ± 7.89 | 0.0080 | 0.4983 |
| Surgical procedures: | |||||
| Perit.: omental bursa | 10 (7.8%) | 4 (4.3%) | 6 (16.7%) | 0.0281 | 1.0000 |
| Perit.: right-upper quadrant | 38 (29.5%) | 23 (24.7%) | 15 (41.7%) | 0.0840 | 1.0000 |
| Perit.: left-upper quadrant | 21 (16.3%) | 9 (9.7%) | 12 (33.3%) | 0.0025 | 0.1585 |
| Splenectomy | 9 (7.0%) | 3 (3.2%) | 6 (16.7%) | 0.0142 | 0.8531 |
| Median overall survival (month) | 29.17 (22.97–35.32) | 34.99 (28.84–45.67) | 19.88 (14.59–28.16) | – | 0.0028 3 |
| Median DSS (month) | 29.67 (25.20–37.19) | 36.27 (29.17–47.08) | 22.41 (18.92–29.60) | – | 0.0229 3 |
| Clinical Characteristics | DSS | OS | ||
|---|---|---|---|---|
| Univariate p-Value | Multivariate p-Value | Univariate p-Value | Multivariate p-Value | |
| Age (years) | 0.3060 | 0.0068 | 0.1460 | 0.2324 |
| Body mass index (kg/m2) | 0.7610 | 0.6984 | 0.8330 | 0.9951 |
| Sex (female (ref.) vs. male) | 0.2220 | 0.0005 | 0.0535 | 0.0084 |
| ASA score (I-II (ref.) vs. III-IV) | 0.9260 | 0.0850 | 0.2970 | 0.4688 |
| CC score | ||||
| CC-0 (ref.) vs. CC-1 | 0.0002 | 0.8930 | 0.0008 | 0.4297 |
| CC-0 (ref.) vs. CC-2 | <0.0001 | <0.0001 | 0.0002 | 0.4779 |
| Peritoneal carcinomatosis index | <0.0001 | <0.0001 | <0.0001 | 0.0284 |
| Histopathology (Normal adenocarcinoma (ref.) vs. mucinous) | 0.0229 | 0.6695 | 0.0028 | 0.3049 |
| Duration of HIPEC | ||||
| 30 min (ref.) vs. 60 min | <0.0001 | 0.0036 | 0.0058 | 0.4879 |
| 30 min (ref.) vs. 90 min | 0.2390 | 0.3216 | 0.4234 | 0.3481 |
| Lineage of chemotherapy | ||||
| None (ref.) vs. first-line | 0.9550 | 0.3215 | 0.8024 | 0.3830 |
| None (ref.) vs. second-line | 0.1600 | <0.0001 | 0.1370 | 0.4480 |
| None (ref.) vs. third-line | <0.0001 | <0.0001 | 0.0025 | 0.0012 |
| Usage of biological agents | ||||
| None (ref.) vs. anti-VEGF | 0.2437 | 0.1874 | 0.0437 | 0.5559 |
| None (ref.) vs. anti-EGFR | 0.8621 | 0.0819 | 0.7991 | 0.3321 |
| Any incomplete tumor removal surgery prior to CRS + HIPEC | ||||
| None (ref.) vs. single | 0.4100 | 0.2237 | 0.3570 | 0.4283 |
| None (ref.) vs. multiple | 0.7150 | 0.0123 | 0.5670 | 0.3720 |
| Primary tumor resecated (Yes (ref.) vs. No) | 0.1840 | 0.0594 | 0.1490 | 0.4018 |
| Sidedness | ||||
| Left-sided (ref.) vs. right-sided | 0.0282 | <0.0001 | 0.1040 | 0.0070 |
| Left-sided (ref.) vs. rectum | 0.5587 | 0.8102 | 0.3590 | 0.6583 |
| T stage | ||||
| I-II (ref.) vs. III | 0.1930 | 0.0658 | 0.2250 | 0.4211 |
| I-II (ref.) vs. IV | 0.5270 | 0.0038 | 0.5300 | 0.6362 |
| Clinical Characteristics | Metachronous PM (n = 89) | mAC (n = 67) | mMAC (n = 22) | Crude p-Value | Adjusted p-Value |
|---|---|---|---|---|---|
| Sidedness | 0.0734 | 1.0000 | |||
| Left-sided | 45 (50.6%) | 33 (49.3%) | 7 (31.8%) | ||
| Right-sided | 29 (32.6%) | 22 (32.8%) | 12 (54.5%) | ||
| Rectum | 14 (15.7%) | 12 (17.9%) | 2 (9.1%) | ||
| Unknown primary location | 1 (1.1%) | 0 (0%) | 1 (4.5%) | ||
| Surgical procedures: | |||||
| Perit.: right-upper quadrant | 25 (28.1%) | 13 (19.4%) | 12 (54.5%) | 0.0026 | 0.1616 |
| Perit.: left-upper quadrant | 11 (12.4%) | 5 (7.5%) | 6 (27.3%) | 0.0238 | 1.0000 |
| Median overall survival (month) | 32.10 (26.97–45.40) | 32.10 (27.93–45.44) | 26.18 (19.12–NA) 1 | – | 0.8210 2 |
| Median DSS (month) | 34.43 (28.48–48.13) | 34.43 (29.96–48.13) | 32.56 (19.12–NA) 1 | – | 0.6490 2 |
| Clinical Characteristics | DSS | OS | ||
|---|---|---|---|---|
| Univariate p-Value | Multivariate p-Value | Univariate p-Value | Multivariate p-Value | |
| Age (years) | 0.9941 | 0.9141 | 0.4630 | 0.2623 |
| Body mass index (kg/m2) | 0.2740 | 0.4648 | 0.2010 | 0.4721 |
| Sex (female (ref.) vs. male) | 0.8615 | 0.5201 | 0.6160 | 0.1225 |
| ASA score (I-II (ref.) vs. III-IV) | 0.6940 | 0.2470 | 0.5690 | 0.2725 |
| CC score | ||||
| CC-0 (ref.) vs. CC-1 | 0.7410 | 0.3935 | 0.9980 | 0.5185 |
| CC-0 (ref.) vs. CC-2 | <0.0001 | 0.6079 | 0.3210 | 0.4917 |
| Peritoneal carcinomatosis index | 0.0606 | <0.0001 | 0.0564 | 0.0034 |
| Histopathology [normal adenocarcinoma (ref.) vs. mucinous] | 0.8210 | 0.1302 | 0.6490 | 0.5397 |
| Duration of HIPEC | ||||
| 30 min (ref.) vs. 60 min | 0.5760 | 0.2094 | 0.3310 | 0.1302 |
| 30 min (ref.) vs. 90 min | 0.1750 | 0.0617 | 0.2270 | 0.3711 |
| Lineage of chemotherapy | ||||
| None (ref.) vs. first-line | 0.2782 | 0.7994 | 0.2787 | 0.3441 |
| None (ref.) vs. second-line | 0.0909 | 0.2421 | 0.0885 | 0.1340 |
| Usage of biological agents | ||||
| None (ref.) vs. anti-VEGF | 0.3177 | 0.2857 | 0.3720 | 0.2599 |
| None (ref.) vs. anti-EGFR | 0.0673 | 0.2533 | 0.2910 | 0.7365 |
| Any incomplete tumor removal surgery prior to CRS + HIPEC | ||||
| None (ref.) vs. single | 0.0634 | 0.0001 | 0.4550 | 0.3465 |
| None (ref.) vs. multiple | 0.3192 | <0.0001 | 0.6290 | 0.2752 |
| Primary tumor resecated (Yes (ref.) vs. No) | 0.3550 | <0.0001 | 0.3400 | 0.1621 |
| Sidedness | ||||
| Left-sided (ref.) vs. right-sided | 0.6200 | 0.0270 | 0.7080 | 0.4033 |
| Left-sided (ref.) vs. rectum | 0.7290 | 0.6344 | 0.5800 | 0.9616 |
| T stage | ||||
| I-II (ref.) vs. III | <0.0001 | <0.0001 | 0.8670 | 0.8323 |
| I-II (ref.) vs. IV | <0.0001 | <0.0001 | 0.9840 | 0.8258 |
| Histological Subtypes According Occurrence of Peritoneal Metastases | mAC | mMAC | sAC | sMAC |
|---|---|---|---|---|
| mAC | – | 0.7728 | 0.9686 | 0.302 |
| mMAC | 0.5966 | – | 0.7873 | 0.0782 |
| sAC | 0.6899 | 0.7861 | – | 0.0239 |
| sMAC | 0.118 | 0.0179 | 0.0031 | – |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herold, Z.; Acs, M.; Szasz, A.M.; Olasz, K.; Hussong, J.; Mayr, M.; Dank, M.; Piso, P. Patients with Metachronous Peritoneal Metastatic Mucinous Colorectal Adenocarcinoma Benefit More from Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) than Their Synchronous Counterparts. Cancers 2022, 14, 3978. https://doi.org/10.3390/cancers14163978
Herold Z, Acs M, Szasz AM, Olasz K, Hussong J, Mayr M, Dank M, Piso P. Patients with Metachronous Peritoneal Metastatic Mucinous Colorectal Adenocarcinoma Benefit More from Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) than Their Synchronous Counterparts. Cancers. 2022; 14(16):3978. https://doi.org/10.3390/cancers14163978
Chicago/Turabian StyleHerold, Zoltan, Miklos Acs, Attila Marcell Szasz, Katalin Olasz, Jana Hussong, Max Mayr, Magdolna Dank, and Pompiliu Piso. 2022. "Patients with Metachronous Peritoneal Metastatic Mucinous Colorectal Adenocarcinoma Benefit More from Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) than Their Synchronous Counterparts" Cancers 14, no. 16: 3978. https://doi.org/10.3390/cancers14163978
APA StyleHerold, Z., Acs, M., Szasz, A. M., Olasz, K., Hussong, J., Mayr, M., Dank, M., & Piso, P. (2022). Patients with Metachronous Peritoneal Metastatic Mucinous Colorectal Adenocarcinoma Benefit More from Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) than Their Synchronous Counterparts. Cancers, 14(16), 3978. https://doi.org/10.3390/cancers14163978







