Management of Patients with Treatment of Pheochromocytoma: A Critical Appraisal
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
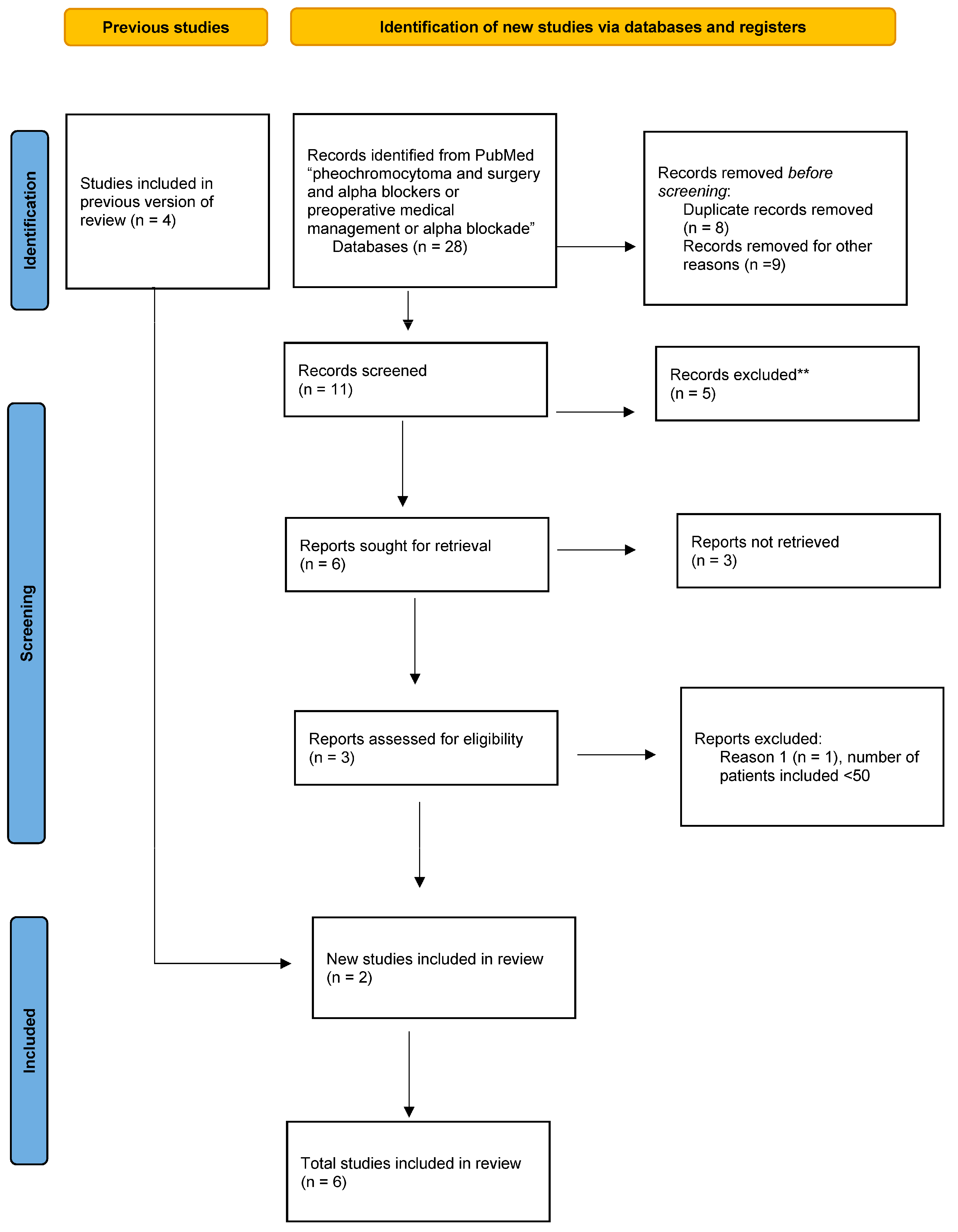
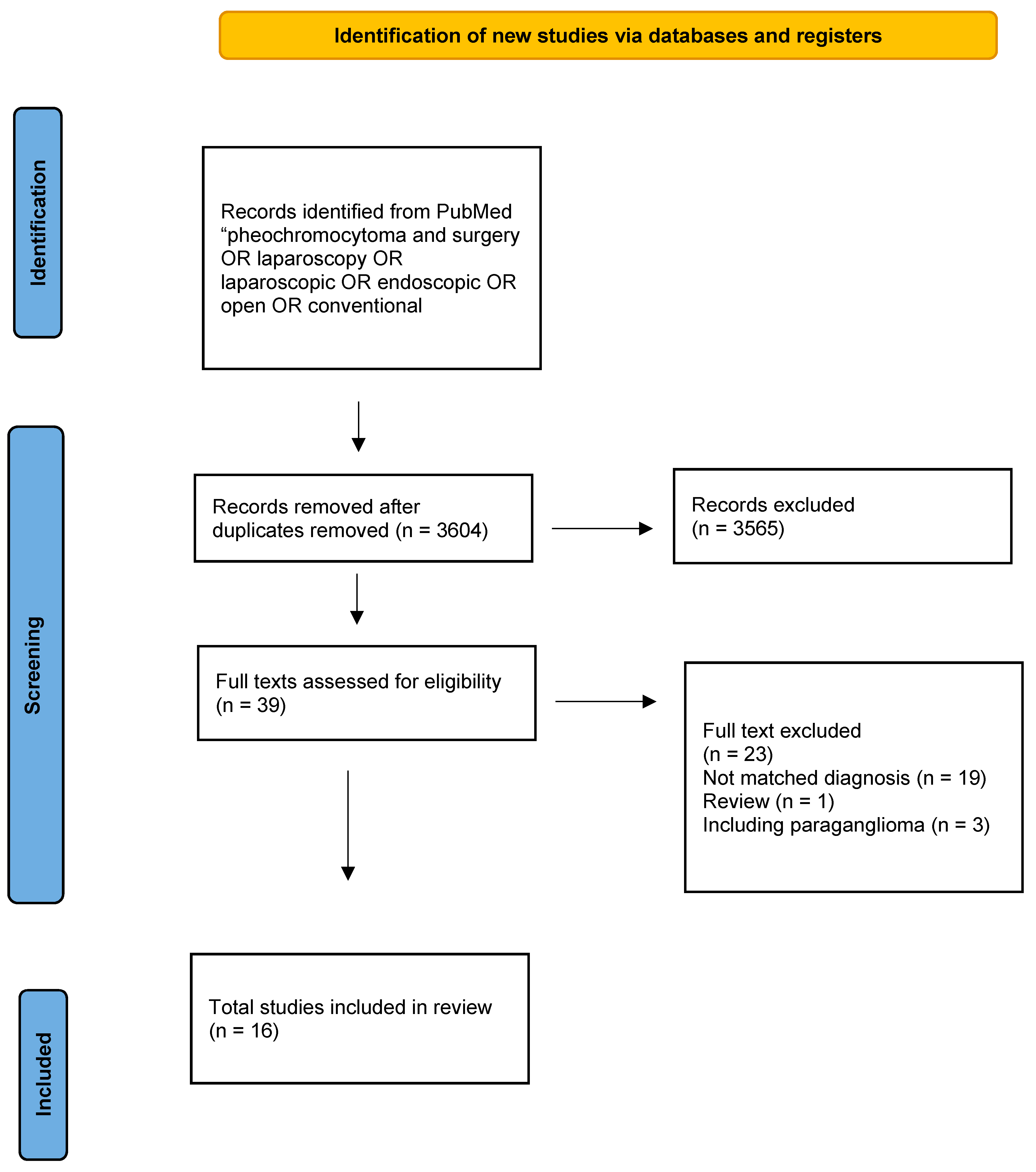
2.1. Systematic Literature Search
2.2. Study Selection
2.3. Data Extraction
3. Results
3.1. Surgical Treatment for Pheochromocytoma
3.2. The Concept of Preoperative Medical Preparation (PMP) to Avoid Intraoperative Hemodynamic Instability
3.3. Medications Used for Preoperative Medical Preparation (PMP)
3.4. Is There a Relationship between Preoperative Blood Pressure Control after Preparation and Perioperative Hemodynamic Events?
3.5. Is There a Link between Perioperative Hemodynamic Episodes and Postoperative Complications?
3.6. Intraoperative Anesthetic Management
3.7. Clinical Guidelines: The Need for Evolution
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Reisch, N.; Peczkowska, M.; Januszewicz, A.; Neumann, H.P.H. Pheochromocytoma: Presentation, diagnosis and treatment. J. Hypertens. 2006, 24, 2331–2339. [Google Scholar]
- Omura, M.; Saito, J.; Yamaguchi, K.; Kakuta, Y.; Nishikawa, T. Prospective Study on the Prevalence of Secondary Hypertension among Hypertensive Patients Visiting a General Outpatient Clinic in Japan. Hypertens. Res. 2004, 27, 193–202. [Google Scholar]
- Naranjo, J.; Dodd, S.; Martin, Y.N. Perioperative Management of Pheochromocytoma. J. Cardiothorac. Vasc. Anesth. 2017, 31, 1427–1439. [Google Scholar]
- Y-Hassan, S.; Falhammar, H. Cardiovascular manifestations and complications of pheochromocytomas and paragangliomas. J. Clin. Med. 2020, 9, 2435. [Google Scholar]
- Lenders, J.W.M.; Eisenhofer, G. Update on modern management of pheochromocytoma and paraganglioma. Endocrinol. Metab. 2017, 32, 152–161. [Google Scholar]
- Farrugia, F.A.; Martikos, G.; Tzanetis, P.; Charalampopoulos, A.; Misiakos, E.; Zavras, N.; Sotiropoulos, D. Pheochromocytoma, diagnosis and treatment: Review of the literature. Endocr. Regul. 2017, 51, 168–181. [Google Scholar]
- Castinetti, F.; de Freminville, J.B.; Guerin, C.; Cornu, E.; Sarlon, G.; Amar, L. Controversies about the systematic preoperative pharmacological treatment before pheochromocytoma or paraganglioma surgery. Eur. J. Endocrinol. 2022, 168, D17–D24. [Google Scholar]
- Neumann, H.P.H.; Young, W.F.; Eng, C. Pheochromocytoma and Paraganglioma. N. Engl. J. Med. 2019, 381, 552–565. [Google Scholar]
- Young, W.F. Endocrine hypertension: Then and now. Endocr. Pract. 2010, 16, 888–902. [Google Scholar]
- Lenders, J.W.M.; Kerstens, M.N.; Amar, L.; Prejbisz, A.; Robledo, M.; Taieb, D.; Pacak, K.; Crona, J.; Zelinka, T.; Mannelli, M.; et al. Genetics, diagnosis, management and future directions of research of phaeochromocytoma and paraganglioma: A position statement and consensus of the Working Group on Endocrine Hypertension of the European Society of Hypertension. J. Hypertens. 2020, 38, 1443–1456. [Google Scholar]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar]
- Goossen, K.; Tenckhoff, S.; Probst, P.; Grummich, K.; Mihaljevic, A.L.; Büchler, M.W.; Diener, M.K. Optimal literature search for systematic reviews in surgery. Langenbeck’s Arch. Surg. 2018, 403, 119–129. [Google Scholar]
- Murphy, M.M.; Witkowski, E.R.; Ng, S.C.; McDade, T.P.; Hill, J.S.; Larkin, A.C.; Whalen, G.F.; Litwin, D.E.; Tseng, J.F. Trends in adrenalectomy: A recent national review. Surg. Endosc. 2010, 24, 2518–2526. [Google Scholar]
- Ross, E.J.; Prichard, B.N.; Kaufman, F.; Robertson, A.I.; Harries, B.J. Papers and Originals Preoperative and Operative Management of Patients with Phaeochromocytoma. BMJ 1967, 1, 191–198. [Google Scholar]
- Riddell, D.H.; Schull, L.G.; Frist, T.F.; Baker, T.D. Experience with pheochromocytoma in 21 patients: Use of dichloroisoproterenol hydrochloride for cardiac arrhythmia. Ann. Surg. 1963, 157, 980–988. [Google Scholar]
- Assalia, A.; Gagner, M. Laparoscopic adrenalectomy. J. Br. Surg. 2004, 91, 1259–1274. [Google Scholar]
- Janetschek, G.; Finkenstedt, G.; Gasser, R.; Waibel, U.G.; Peschel, R.; Bartsch, G. Laparoscopic surgery for pheochromocytoma: Adrenalectomy, partial resection, excision of paragangliomas. J. Urol. 1998, 160, 330–334. [Google Scholar]
- Terachi, T.; Matsuda, T.; Terai, A.; Ogawa, O.; Kakehi, Y.; Wakita, M.K. Transperitoneal Laparoscopic Adrenalectomy: Experience in 100 Patients. J. Endourol. 1997, 11, 361–365. [Google Scholar]
- Lenders, J.W.M.; Duh, Q.Y.; Eisenhofer, G.; Gimenez-Roqueplo, A.P.; Grebe, S.K.G.; Murad, M.H. Pheochromocytoma and paraganglioma: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2014, 99, 1915–1942. [Google Scholar]
- Vargas, H.I.; Kavoussi, L.R.; Bartlett, D.L.; Wagner, J.R.; Venzon, D.J.; Fraker, D.L. Laparoscopic adrenalectomy; a new standard of care. Urology 1997, 49, 673–678. [Google Scholar]
- Schell, S.R.; Talamini, M.A.; Udelsman, R. Laparoscopic adrenalectomy for nonmalignant disease: Improved safety, morbidity, and cost-effectiveness. Surg. Endosc. 1999, 13, 30–34. [Google Scholar]
- Wang, W.; Li, P.; Wang, Y.; Wang, Y.; Ma, Z.; Wang, G. Effectiveness and safety of laparoscopic adrenalectomy of large pheochromocytoma: A prospective, nonrandomized, controlled study. Am. J. Surg. 2015, 210, 230–235. [Google Scholar]
- Li, J.; Wang, Y.; Chang, X.; Han, Z. Laparoscopic adrenalectomy (LA) vs open adrenalectomy (OA) for pheochromocytoma (PHEO): A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2020, 46, 991–998. [Google Scholar]
- Tanaka, M.; Tokuda, N.; Koga, H.; Kimoto, Y.; Naito, S. Laparoscopic Adrenalectomy for Pheochromocytoma: Comparison with Open Adrenalectomy and Comparison of Laparoscopic Surgery for Pheochromocytoma versus Other Adrenal Tumors Conclusions: Laparoscopic adrenalectomy does not increase the specific risks associated with surgery for pheochromocytoma. It is a minimally invasive alternative to conventional open adrenalectomy. J. Endourol. 2000, 14, 427–431. [Google Scholar]
- Toniato, A.; Boschin, I.M.; Opocher, G.; Guolo, A.; Pelizzo, M.; Mantero, F. Is the laparoscopic adrenalectomy for pheochromocytoma the best treatment? Surgery 2007, 141, 723–727. [Google Scholar]
- Bai, S.; Yao, Z.; Zhu, X.; Li, Z.; Jiang, Y.; Wang, R.; Wu, B. Comparison of transperitoneal laparoscopic versus open adrenalectomy for large pheochromocytoma: A retrospective propensity score-matched cohort study. Int. J. Surg. 2019, 61, 26–32. [Google Scholar]
- Tiberio, G.A.M.; Baiocchi, G.L.; Arru, L.; Rosei, C.A.; De Ponti, S.; Matheis, A.; Rizzoni, D.; Giulini, S.M. Prospective randomized comparison of laparoscopic versus open adrenalectomy for sporadic pheochromocytoma. Surg. Endosc. 2008, 22, 1435–1439. [Google Scholar]
- Inabnet, W.B.; Pitre, J.; Bernard, D.; Chapuis, Y. Comparison of the hemodynamic parameters of open and laparoscopic adrenalectomy for pheochromocytoma. World J. Surg. 2000, 24, 574–578. [Google Scholar]
- Möbius, E.; Nies, C.; Rothmund, M. Surgical treatment of pheochromocytomas Laparoscopic or conventional ? Surg. Endosc. 1999, 13, 35–39. [Google Scholar]
- Kasahara, T.; Nishiyama, T.; Takahashi, K. Laparoscopic adrenalectomy for pheochromocytoma: Evaluation of experience and strategy at a single institute. BJU Int. 2009, 103, 218–222. [Google Scholar]
- Kazaryan, A.M.; Kuznetsov, N.S.; Shulutko, A.M.; Beltsevich, D.G.; Edwin, B. Evaluation of endoscopic and traditional open approaches to pheochromocytoma. Surg. Endosc 2004, 18, 937–941. [Google Scholar]
- Agarwal, G.; Sadacharan, D.; Aggarwal, V.; Chand, G.; Mishra, A.; Agarwal, A. Surgical management of organ-contained unilateral pheochromocytoma: Comparative outcomes of laparoscopic and conventional open surgical procedures in a large single-institution series. Langenbeck′s Arch. Surg. 2012, 397, 1109–1116. [Google Scholar]
- Sprung, J.; O’hara, J.F.; Gill, I.S.; Abdelmalak, B.; Sarnaik, A.; Bravo, E.L. Anesthetic aspects of laparoscopic and open adrenalectomy for pheochromocytoma. Urology 2000, 55, 339–343. [Google Scholar]
- Ichikawa, T.; Mikami, K.; Suzuki, H.; Imamoto, T.; Yamazaki, T.; Naya, Y. Adrenal: Laparoscopic adrenalectomy for pheochromocytoma. Biomed. Pharmacother. 2002, 56 (Suppl. S1), 149–153. [Google Scholar]
- Fang, F.; Ding, L.; He, Q.; Liu, M. Preoperative Management of Pheochromocytoma and Paraganglioma. Front. Endocrinol. 2020, 11, 586795. [Google Scholar]
- Kim, H.H.; Han Kim, G.; Tak Sung, G. Laparoscopic Adrenalectomy for Pheochromocytoma: Comparison with Conventional Open Adrenalectomy. J. Endourol. 2004, 18, 251–255. [Google Scholar]
- Brunaud, L.; Nguyen-Thi, P.L.; Mirallie, E.; Raffaelli, M.; Vriens, M.; Theveniaud, P.E. Predictive factors for postoperative morbidity after laparoscopic adrenalectomy for pheochromocytoma: A multicenter retrospective analysis in 225 patients. Surg. Endosc. 2016, 30, 1051–1059. [Google Scholar]
- Groeben, H.; Walz, M.K.; Nottebaum, B.J.; Alesina, P.F.; Greenwald, A.; Schumann, R. International multicentre review of perioperative management and outcome for catecholamine-producing tumours. Br. J. Surg. 2020, 107, e170–e178. [Google Scholar]
- Buitenwerf, E.; Osinga, T.E.; Timmers, H.J.; Lenders, J.W.; Feelders, R.A.; Eekhoff, E.M. Efficacy of α-blockers on hemodynamic control during pheochromocytoma resection-a randomized controlled trial. J. Clin. Endocrinol. Metab. 2020, 105, 2381–2391. [Google Scholar]
- Goldstein, R.E.; O’neill, J.A.; Holcomb Iii, G.W.; Iii, W.M.M.; Neblett Iii, W.W.; Oates, J.A. Clinical Experience Over 48 Years With Pheochromocytoma. Ann. Surg. 1999, 229, 755–764. [Google Scholar]
- Roizen, M.F.; Hunt, T.K.; Beaupre, P.N.; Kremer, P.; Firmin, R.; Chang, C.N.; Alpert, R.A.; Thomas, C.J.; Tyrrell, J.B.; Cahalan, B.J. The effect of alpha-adrenergic blockade on cardiac performance and tissue oxygen delivery during excision of pheochromocytoma. Surgery 1983, 94, 941–945. [Google Scholar]
- Bruynzeel, H.; Feelders, R.A.; Groenland, T.H.N.; van den Meiracker, A.H.; van Eijck, C.H.J.; Lange, J.F. Risk factors for hemodynamic instability during surgery for pheochromocytoma. J. Clin. Endocrinol. Metab. 2010, 95, 678–685. [Google Scholar]
- Brunaud, L.; Boutami, M.; Nguyen-Thi, P.L.; Finnerty, B.; Germain, A.; Weryha, G. Both preoperative alpha and calcium channel blockade impact intraoperative hemodynamic stability similarly in the management of pheochromocytoma. Surgery 2014, 156, 1410–1418. [Google Scholar]
- Jaiswal, S.K.; Memon, S.S.; Lila, A.; Sarathi, V.; Goroshi, M.; Garg, R.; Barnabas, R.; Hemantkumar, I.; Patel, R.D.; Oak, S.; et al. Preoperative Amlodipine Is Efficacious in Preventing Intraoperative HDI in Pheochromocytoma: Pilot RCT. J. Clin. Endocrinol. Metab. 2021, 106, e2907–e2918. [Google Scholar]
- Dubé, L.; Granry, J.C. The therapeutic use of magnesium in anesthesiology, intensive care and emergency medicine: A review. Can. J. Anaesth. 2003, 50, 732–746. [Google Scholar]
- Urabe, F.; Kimura, S.; Iwatani, K.; Takahashi, K.; Ito, K.; Tashiro, K. Risk factors for perioperative hemodynamic instability in pheochromocytoma: A systematic review and meta-analysis. J. Clin. Med. 2021, 10, 4531. [Google Scholar]
- Lentschener, C.; Gaujoux, S.; Tesniere, A.; Dousset, B. Point of controversy: Perioperative care of patients undergoing pheochromocytoma removal-time for a reappraisal? Eur. J. Endocrinol. 2011, 165, 365–373. [Google Scholar]
- Namekawa, T.; Utsumi, T.; Kawamura, K.; Kamiya, N.; Imamoto, T.; Takiguchi, T. Clinical predictors of prolonged postresection hypotension after laparoscopic adrenalectomy for pheochromocytoma. Surgery 2016, 159, 763–770. [Google Scholar]
- Kiernan, C.M.; Du, L.; Chen, X.; Broome, J.T.; Shi, C.; Peters, M.F. Predictors of Hemodynamic Instability During Surgery for Pheochromocytoma. Ann. Surg. Oncol. 2014, 21, 3865–3871. [Google Scholar]
- Zawadzka, K.; Więckowski, K.; Małczak, P.; Wysocki, M.; Major, P.; Pędziwiatr, M. Selective vs non-selective alpha-blockade prior to adrenalectomy for pheochromocytoma: Systematic review and meta-analysis. Eur. J. Endocrinol. 2021, 184, 751–760. [Google Scholar]
- Schimmack, S.; Kaiser, J.; Probst, P.; Kalkum, E.; Diener, M.K.; Strobel, O. Meta-analysis of α-blockade versus no blockade before adrenalectomy for phaeochromocytoma. Br. J. Surg. 2020, 107, e102–e108. [Google Scholar]
- Groeben, H.; Nottebaum, B.J.; Alesina, P.F.; Traut, A.; Neumann, H.P.; Walz, M.K. Perioperative α-receptor blockade in phaeochromocytoma surgery: An observational case series. Br. J. Anaesth. 2017, 118, 182–189. [Google Scholar]
- Araujo-Castro, M.; Pascual-Corrales, E.; Nattero Chavez, L.; Martínez Lorca, A.; Alonso-Gordoa, T.; Molina-Cerrillo, J. Protocol for presurgical and anesthetic management of pheochromocytomas and sympathetic paragangliomas: A multidisciplinary approach. J. Endocrinol. Investig 2021, 44, 2545–2555. [Google Scholar]
- Tan, S.G.; Koay, C.K.; Chan, S.T. The Use of Vasopressin to Treat Catecholamine-resistant Hypotension After Phaeochromocytoma Removal. Anaesth. Intensive Care 2002, 30, 477–480. [Google Scholar]
- Boutros, A.R.; Bravo, E.L.; Zanettin, G.; Straffon, R.A. Perioperative management of 63 patients with pheochromocytoma. Clevel. Clin. J. Med. 1990, 57, 613–617. [Google Scholar]
| Author | Year | Design | LA/OA | LA Type | OT (min) | Blood Loss (mL) | Hospital Stay (Days) | CNS (n) | CONV (n) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LA | OA | LA | OA | LA | OA | LA | OA | LA to OA | |||||
| Vargas [20] | 1996 | RTP | 6/6 | Trans | 193 | 178 | 245 | 283 | 3.1 *** | 7.2 *** | NA | NA | 1 |
| Sprung [33] | 1999 | RTP | 14/20 | Trans | 177 | 196 | 100 *** | 400 *** | 3 *** | 7.5 *** | NA | NA | 1 |
| Schell [21] | 1997 | RTP | 4/7 | Trans | NA | NA | NA | NA | 1.7 *** | 7.8 *** | 0 | 3 | NA |
| Ichikawa [34] | 2001 | RTP | 7/11 | Trans Retro | 145 | 165 | 55 ** | 330 ** | 12 | 14 | 1 | 3 | 1 |
| Tanaka [24] | 1998 | RTP | 10/7 | Trans | 240 | 288 | 200 | 400 | 8 ** | 15 ** | 1 | 2 | 1 |
| Inabnet [28] | 1997 | RTP | 11/11 | Trans | 146 | 153 | NA | NA | 5.5 | 6.1 | 0 | 1 | 0 |
| Möbius [29] | 1997 | RTP | 9/9 | Trans | 243 ** | 100 ** | NA | NA | 6 ** | 10 ** | 1 | 4 | 2 |
| Kim [36] | 2002 | RTP | 15/9 | Trans | 171 | 200 | 189.5 * | 397.1 * | 5.6 *** | 12.4 *** | 0 | 4 | NA |
| Toniato [25] | 2005 | RTP | 40/24 | NA | 78 ** | 149 ** | 100 * | 200 * | 3.7 ** | 10.1 ** | 1 | 4 | NA |
| Kazaryan [31] | 2002 | RTP | 9/22 | Trans | 132 * | 129 * | 178 * | 420 * | 3.2 * | 9.2 * | 0 * | 3 * | NA |
| Tibierio [27] | 2006 | RCT | 13/9 | Trans | 158 | 180 | 48 * | 164 * | 5 * | 8 * | 0 | 0 | NA |
| Kasahara [30] | 2007 | RTP | 23/18 | Trans | 210 | 212 | 120 * | 400 * | 9 ** | 19 ** | 0 ** | 4 ** | 4 |
| Wang [23] | 2013 | RTP | 23/28 | Trans | 158 ** | 121 ** | 47 | 102 | 4.2 ** | 9.7 ** | 2 | 2 | 2 |
| Bai [26] | 2017 | RTP | 82/100 | Trans | 167 | 150 | 100** | 400** | 9.8 | 10 | 19 | 36 | NA |
| Fang [35] | 2017 | RTP | 89/26 | Trans | 157 * | 260 * | 134 * | 439 * | 3.7 * | 5.2 * | 6 | 5 | NA |
| Agarwal [32] | 2010 | RTP | 49/52 | Trans | 270 | 258 | 223 ** | 473 ** | 6.1 | 10.4 | 3 ** | 12 ** | 19 |
| Study | Year | Definitions of Intraoperative Hemodynamic Instability (IHI) |
|---|---|---|
| Inabnet [28] | 2000 | Highest MAP Highest BP |
| Bruynzeel [42] | 2010 | SBP > 160 mmHg MAP < 60 mmHg |
| Shao [46] | 2011 | Highest BP Minutes SBP > 30% preinduction baseline Minutes SBP > 200 mmHg Lowest BP Minutes SBP < 30% preinduction baseline HR > 110 bpm HR< 50 bpm |
| Brunaud [43] | 2014 | SBP > 160 mmHg MAP < 60 mmHg |
| Kiernan [40] | 2014 | SBP > 200 mmHg HR > 110 bpm |
| Gaujoux [46] | 2015 | SBP > 150 mmHg SBP < 90 mmHg HR > 110 bpm |
| Livingstone [46] | 2015 | 10 hypo/hypertensive episodes where the anesthesiologist had to respond with a vasoactive substance |
| Namekawa [48] | 2016 | SBP > 160 mmHg SBP < 90 mmHg Dose of catecholamine to maintain SBP > 90 mmHg |
| Brunaud [37] | 2016 | SBP > 160 mmHg SBP > 200 mmHg MAP < 60 mmHg SBP > 200 mmHg + MAP < 60 mmHg |
| Kwon [46] | 2016 | SBP > 160 mmHg HR > 100 bpm |
| Vorselaars [46] | 2017 | SBP > 160 mmHg SBP > 200 mmHg MAP < 60 mmHg SBP > 160 mmHg + MAP < 60 mmHg SBP > 200 mmHg + MAP < 60 mmHg Intravenous vasopressor + vasodilator. |
| Groeben [48] | 2017 | Highest BP SBP > 250 mmHg |
| Askasakal [46] | 2018 | SBP > 200 mhg SPB < 90 mmHg Use of vasoactive drugs |
| Buitenwerf [39] | 2019 | SBP > 160 mmHg MAP < 60 mmHg |
| Tian [46] | 2019 | SBP > 200 mmHg SPB < 80 mmHg HR > 120 bpm |
| Thompson [46] | 2019 | SBP > 200 mmHg SBP < 90 mmHg HR > 120 bpm HR < 50 bpm Use of vasopressors |
| Buisset [46] | 2021 | SBP > 160 mmHg SBP > 200 mmHg MAP < 60 mmHg SBP > 200 mmHg + MAP < 60 mmHg |
| Study | Year | Patients | Blockade | IHD | Intraoperative Hypotension | Mortality | Morbidity | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Bl. | No Bl. | Bl. | No Bl. | Bl. | No Bl. | Bl. | No Bl. | |||
| Groeben [38] | 2017 | 1860 | 1517 1108 (alpha) 348 (other) | 343 | Systolic BP > 250 mmHg | NA | NA | 8 | 1 | 90 | 3 | |
| 64 | 25 | |||||||||||
| Goldstein [40] | 1998 | 104 | 67 | 16 | 3 (4.5%) | 0 | 2 (3%) | 0 | 0 | 0 | NA | NA |
| Groeben [52] | 2016 | 303 | 110 98 (alpha) 23 (dox) | 1 | Systolic BP > 250 mmHg | 51% * | 38% * | NA | NA | NA | NA | |
| 11 | 16 | |||||||||||
| Brunaud [43] | 2012 | 155 | 151 41 (alpha) 110 (CCB) | 4 | Greatest SBP (mmHg) | Lowest SBP (mmHg) | 0 | 0 | Alpha 24% CCB 15% | NA | ||
| Alpha 169 ** CCB. 198 ** | 163 ** | Alpha 82CCB 82 | 94 | |||||||||
| Shao [46] | 2011 | 50 | 38 (dox) | 21 | Greatest SBP (mmHg) | Lowest SBP (mmHg) | NA | NA | NA | NA | ||
| 154 | 153 | 90 | 92 | |||||||||
| Ulchaker [46] | 1994 | 113 | 79 (alpha,CCB,dox,BB) | 34 | Greatest SBP (mmHg) | Lowest SBP (mmHg) | 0 | 0 | 6 | 0 | ||
| 192 | 198 | NA | NA | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bihain, F.; Nomine-Criqui, C.; Guerci, P.; Gasman, S.; Klein, M.; Brunaud, L. Management of Patients with Treatment of Pheochromocytoma: A Critical Appraisal. Cancers 2022, 14, 3845. https://doi.org/10.3390/cancers14163845
Bihain F, Nomine-Criqui C, Guerci P, Gasman S, Klein M, Brunaud L. Management of Patients with Treatment of Pheochromocytoma: A Critical Appraisal. Cancers. 2022; 14(16):3845. https://doi.org/10.3390/cancers14163845
Chicago/Turabian StyleBihain, Florence, Claire Nomine-Criqui, Philippe Guerci, Stephane Gasman, Marc Klein, and Laurent Brunaud. 2022. "Management of Patients with Treatment of Pheochromocytoma: A Critical Appraisal" Cancers 14, no. 16: 3845. https://doi.org/10.3390/cancers14163845
APA StyleBihain, F., Nomine-Criqui, C., Guerci, P., Gasman, S., Klein, M., & Brunaud, L. (2022). Management of Patients with Treatment of Pheochromocytoma: A Critical Appraisal. Cancers, 14(16), 3845. https://doi.org/10.3390/cancers14163845






