Innovation for the Sake of Innovation? How Does Robotic Hepatectomy Compare to Laparoscopic or Open Resection for HCC—A Systematic Review and Meta-Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
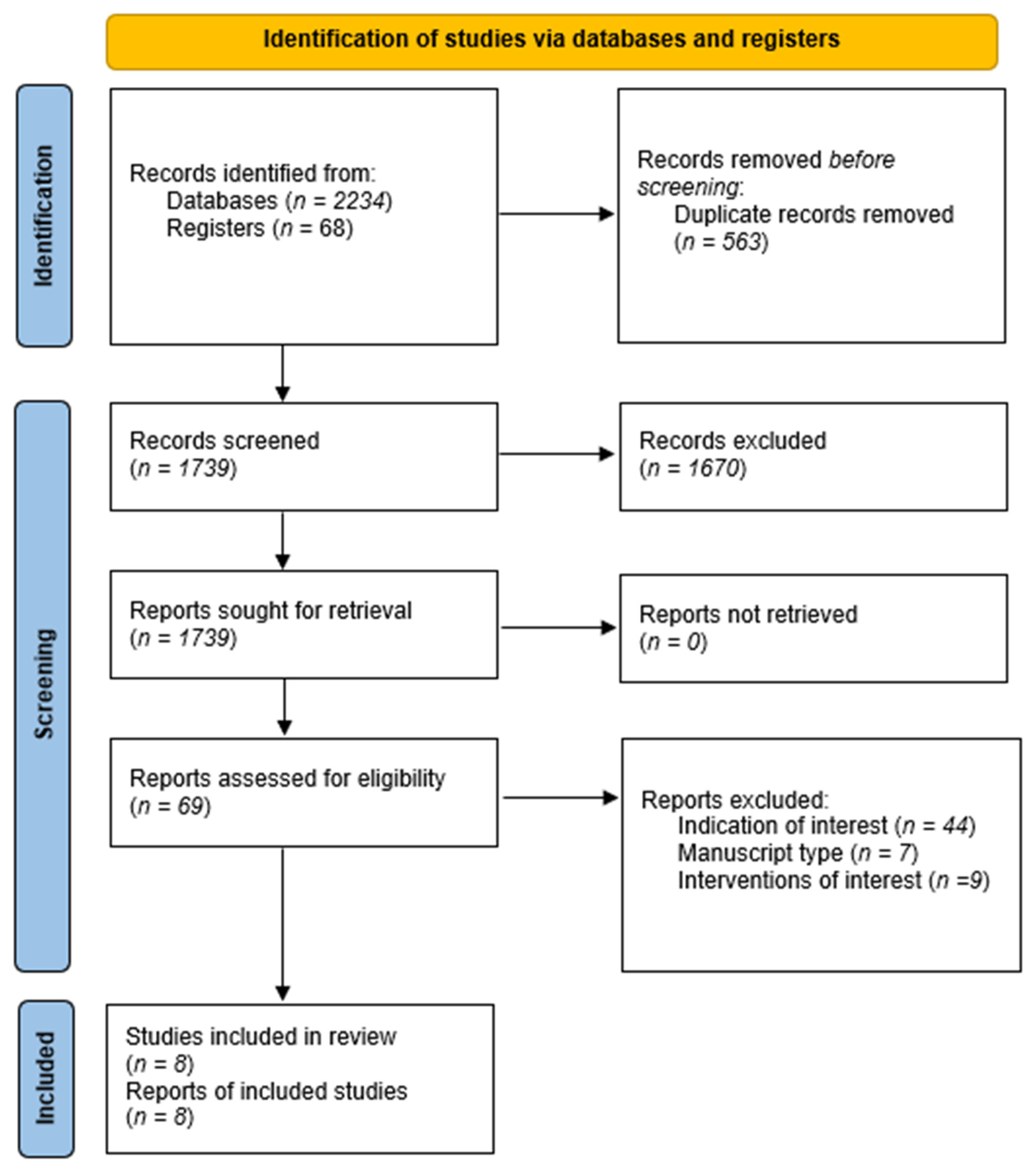
2. Materials and Methods
- Population: patients undergoing hepatectomy for HCC
- Intervention: Robot-assisted hepatectomy
- Comparison: Laparoscopic or open hepatectomy
- Outcomes: complications (overall, major, minor), PHLF, ascites, biliary leak, hemorrhage, infections, conversion rates, recurrence, overall survival, and recurrence free survival.
3. Results
3.1. Critical Appraisal of Included Studies
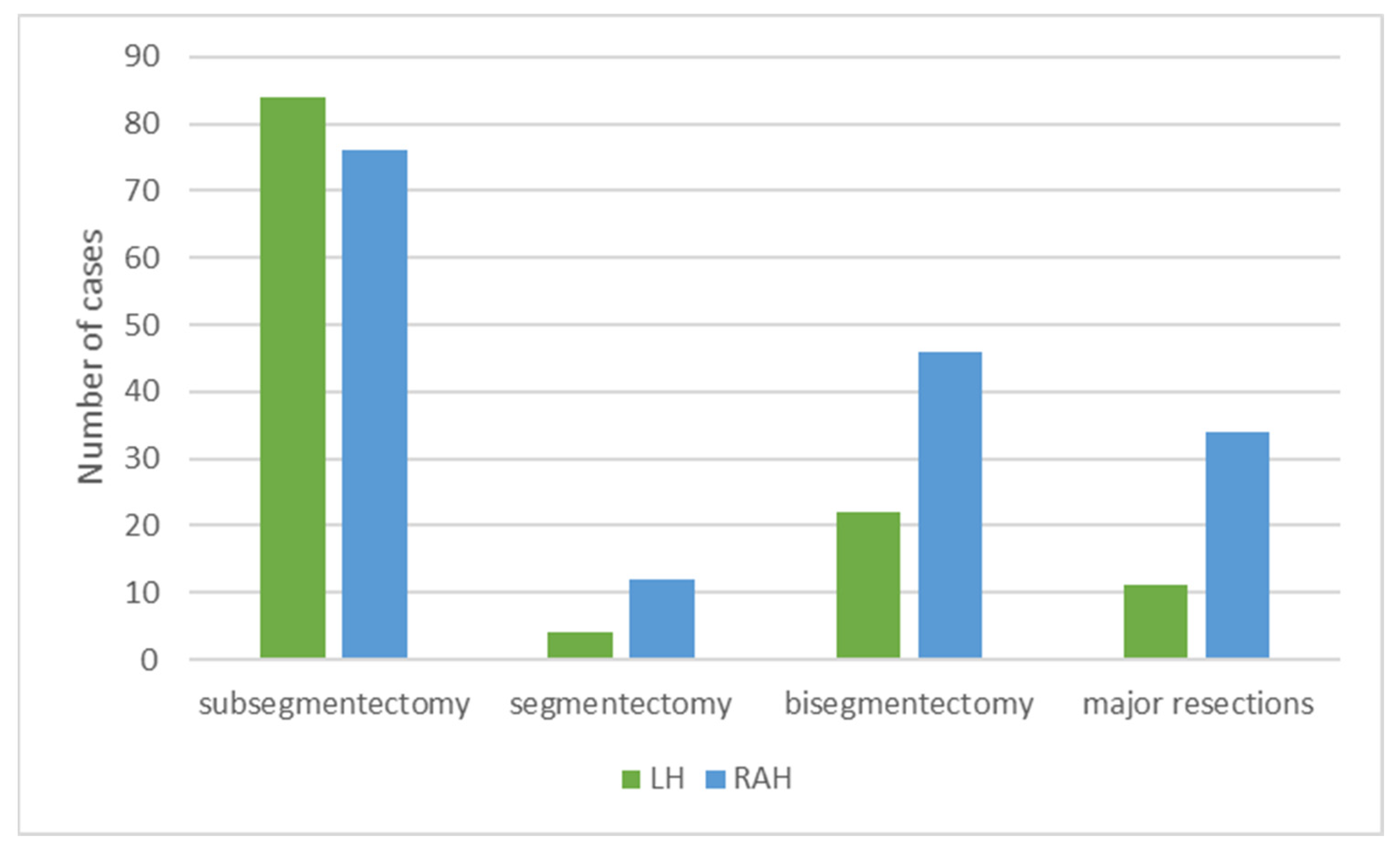
3.2. Characteristics of Included Studies and Patients in RAH and LH Comparisons
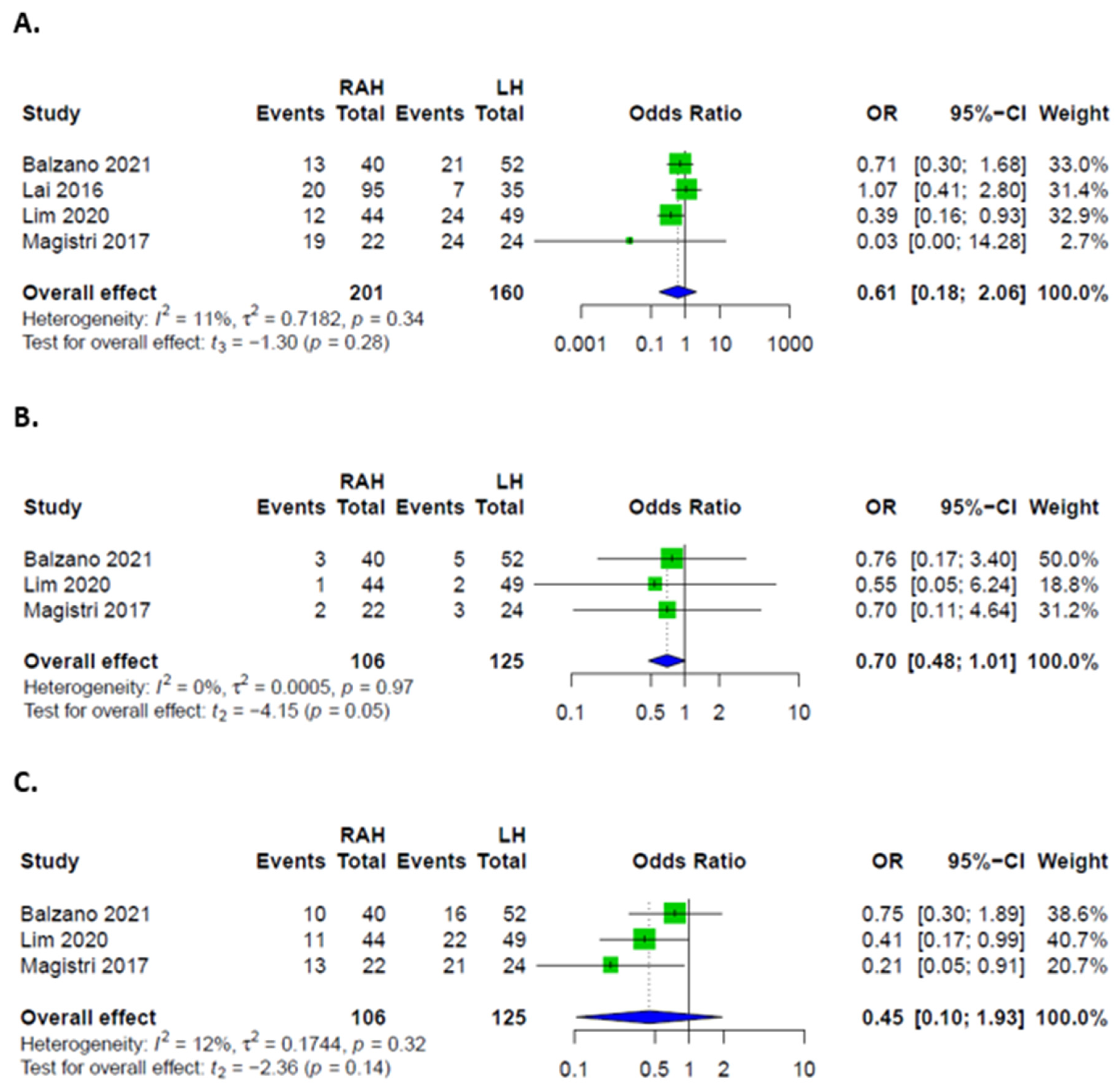
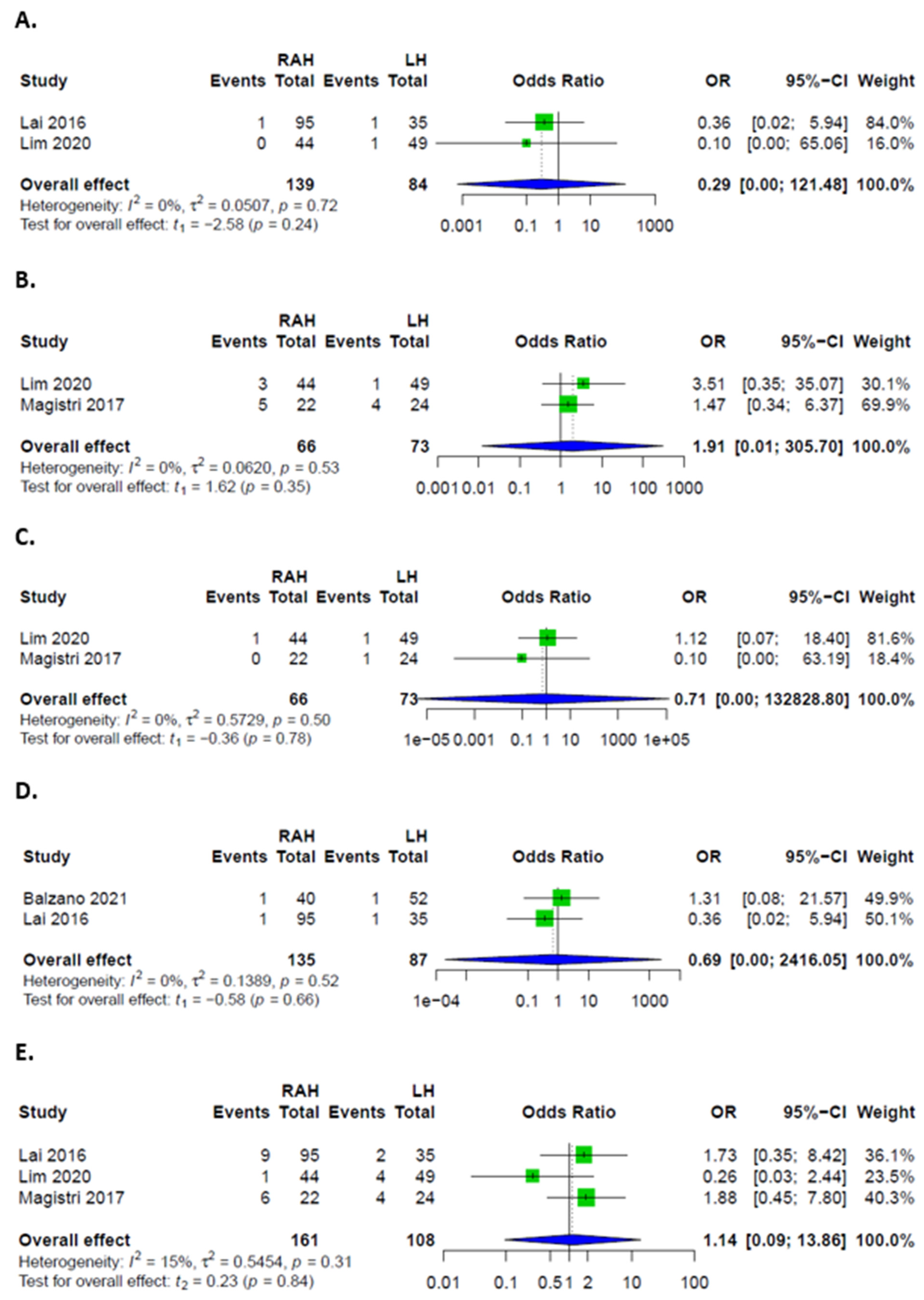
3.3. Comparison between RAH and LH
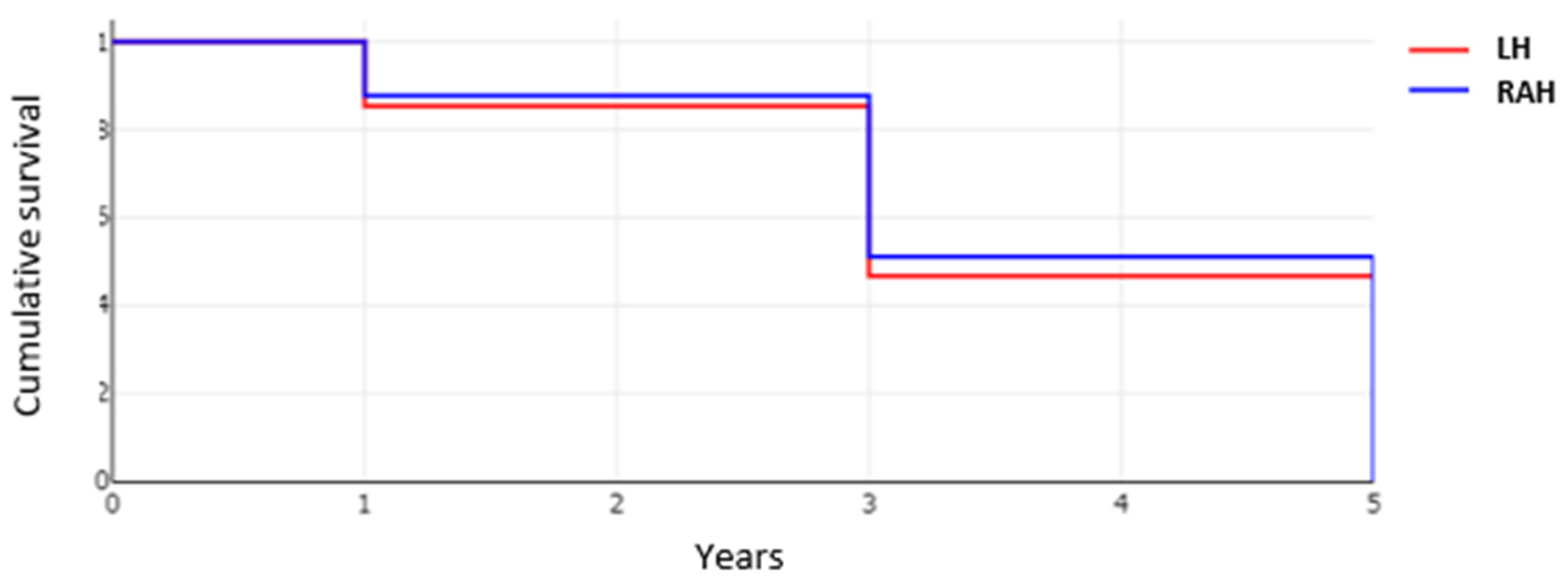
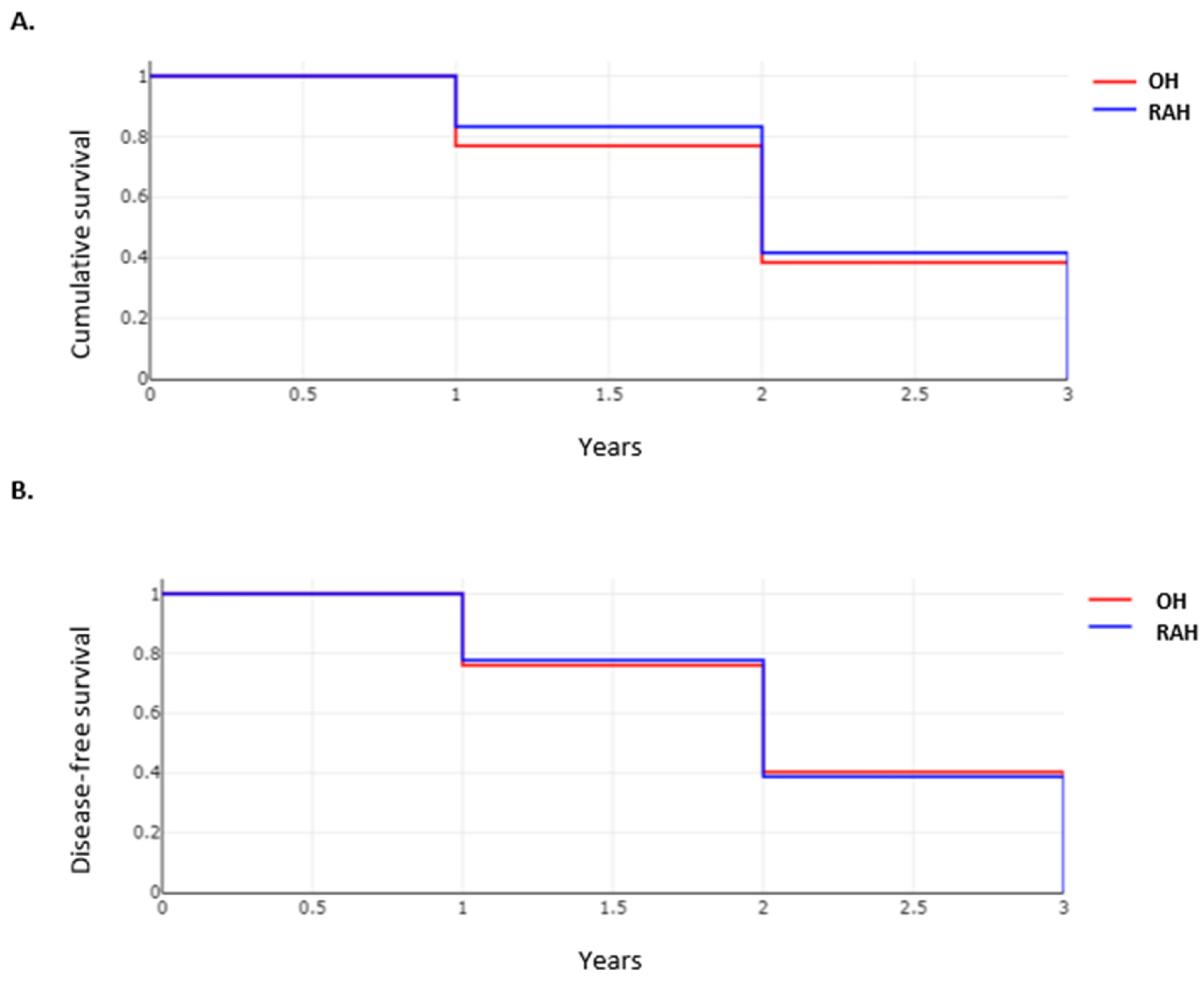
3.4. Oncological Outcome in Patients after RAH and LH Approaches
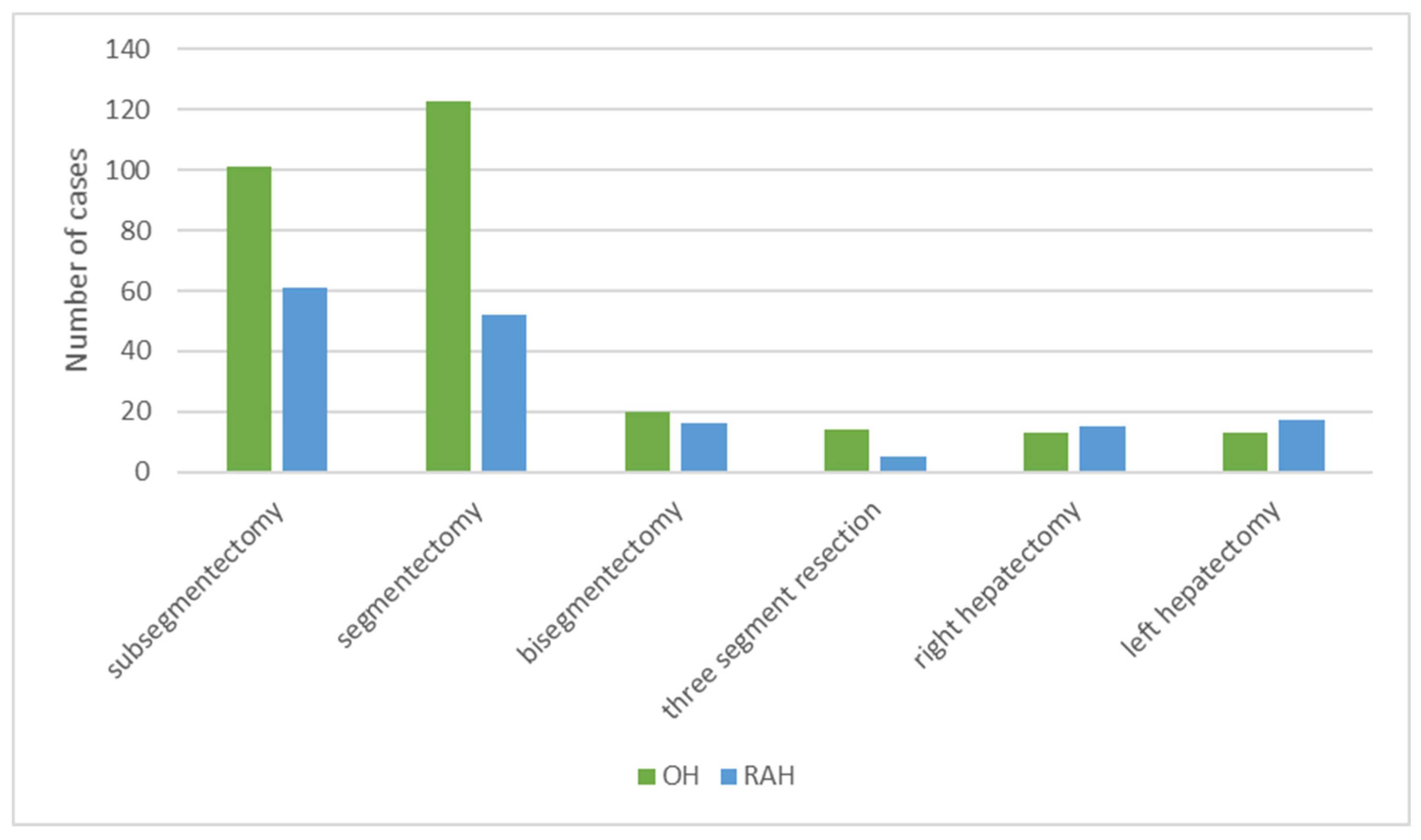
3.5. Characteristics of Included Studies and Patients in RAH and OH Comparisons
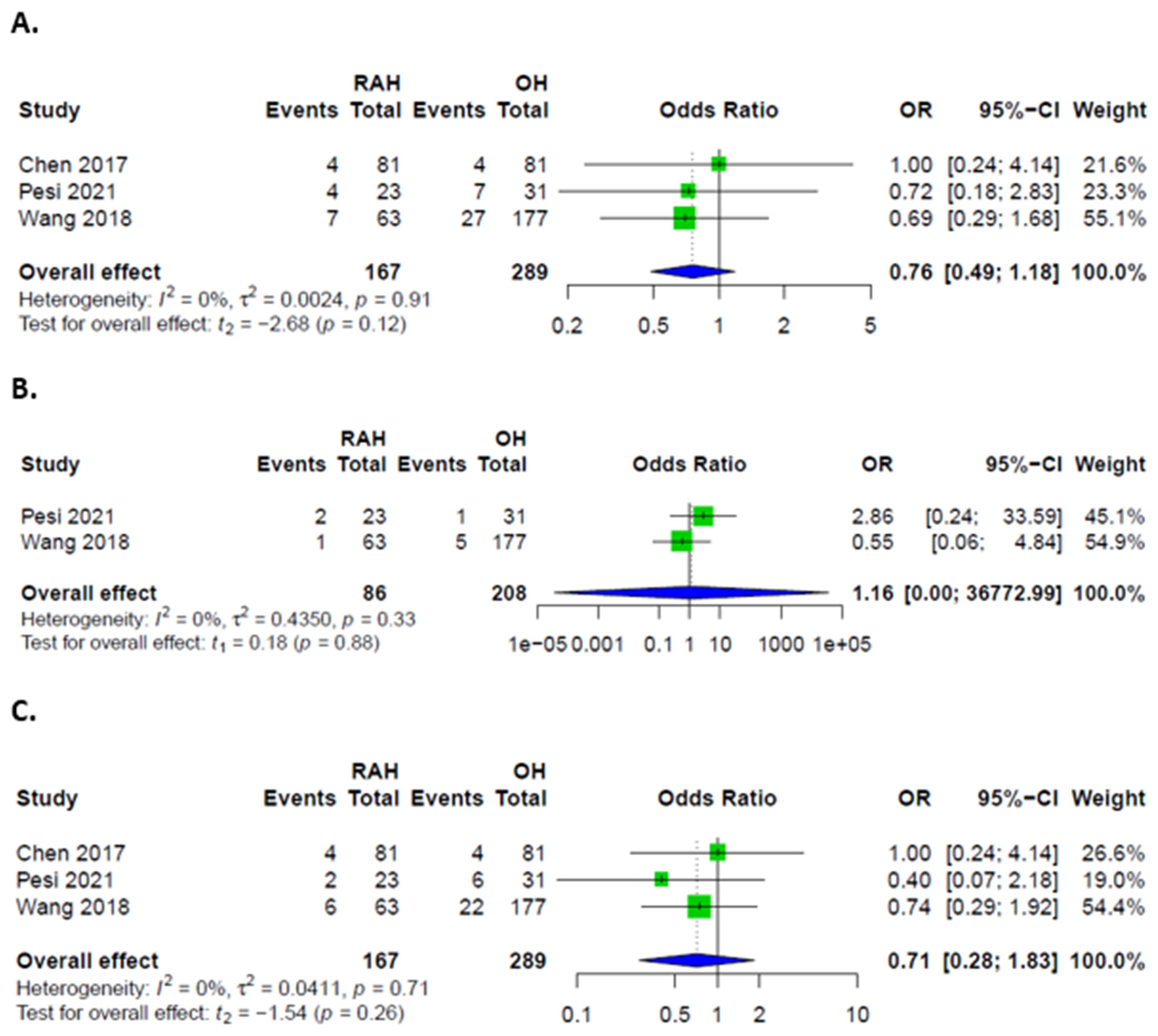
3.6. Comparison between RAH and OH
3.7. Oncological Outcome in Patients after RAH and OH Approaches
3.8. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- George, E.I.; Brand, T.C.; LaPorta, A.; Marescaux, J.; Satava, R.M. Origins of Robotic Surgery: From Skepticism to Standard of Care. JSLS J. Soc. Laparoendosc. Surg. 2018, 22, e2018.00039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulchandani, J.; Shetty, N.; Kulkarni, A.; Shetty, S.; Sadat, M.S.; Kudari, A. Short-term and pathologic outcomes of robotic versus open pancreatoduodenectomy for periampullary and pancreatic head malignancy: An early experience. J. Robot. Surg. 2021. [Google Scholar] [CrossRef]
- Ayabe, R.I.; Azimuddin, A.; Tran Cao, H.S. Robot-assisted liver resection: The real benefit so far. Langenbeck’s Arch. Surg. 2022. [Google Scholar] [CrossRef]
- Shugaba, A.; Lambert, J.E.; Bampouras, T.M.; Nuttall, H.E.; Gaffney, C.J.; Subar, D.A. Should All Minimal Access Surgery Be Robot-Assisted? A Systematic Review into the Musculoskeletal and Cognitive Demands of Laparoscopic and Robot-Assisted Laparoscopic Surgery. J. Gastrointest. Surg. 2022. [Google Scholar] [CrossRef]
- Di Benedetto, F.; Petrowsky, H.; Magistri, P.; Halazun, K.J. Robotic liver resection: Hurdles and beyond. Int. J. Surg. 2020, 82, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Murtha-Lemekhova, A.; Fuchs, J.; Feiler, S.; Schulz, E.; Teroerde, M.; Kalkum, E.; Klotz, R.; Billeter, A.; Probst, P.; Hoffmann, K. Is metabolic syndrome a risk factor in hepatectomy? A meta-analysis with subgroup analysis for histologically confirmed hepatic manifestations. BMC Med. 2022, 20, 47. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Su, C.W.; Wei, C.Y.; Chau, G.Y.; Chen, P.H.; Chao, Y.; Huang, Y.H.; Wu, J.C.; Yang, T.C.; Lee, P.C.; et al. Comparison of prognoses between cirrhotic and non-cirrhotic patients with hepatocellular carcinoma and esophageal varices undergo surgical resection. J. Chin. Med. Assoc. 2022, 85, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Cumpston, M.; Chandler, J.; Lasserson, T. Chapter III: Reporting the review. In Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2 (Updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: Chichester, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 10 June 2022).
- Kalkum, E.; Klotz, R.; Seide, S.; Hüttner, F.J.; Kowalewski, K.-F.; Nickel, F.; Khajeh, E.; Knebel, P.; Diener, M.K.; Probst, P. Systematic reviews in surgery—Recommendations from the Study Center of the German Society of Surgery. Langenbeck’s Arch. Surg. 2021, 406, 1723–1731. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- Foroutan, F.; Guyatt, G.; Zuk, V.; Vandvik, P.O.; Alba, A.C.; Mustafa, R.; Vernooij, R.; Arevalo-Rodriguez, I.; Munn, Z.; Roshanov, P.; et al. GRADE Guidelines 28: Use of GRADE for the assessment of evidence about prognostic factors: Rating certainty in identification of groups of patients with different absolute risks. J. Clin. Epidemiol. 2020, 121, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Balzano, E.; Bernardi, L.; Tincani, G.; Ghinolfi, D.; Melandro, F.; Bronzoni, J.; Meli, S.; Arenga, G.; Biancofiore, G.; Crocetti, L.; et al. Implementing a robotic liver resection program does not always require prior laparoscopic experience. Surg. Endosc. 2021, 36, 3317–3322. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.D.; Wu, C.Y.; Hu, R.H.; Chou, W.H.; Lai, H.S.; Liang, J.T.; Lee, P.H.; Wu, Y.M. Robotic Versus Open Hepatectomy for Hepatocellular Carcinoma: A Matched Comparison. Ann. Surg. Oncol. 2017, 24, 1021–1028. [Google Scholar] [CrossRef] [PubMed]
- Duong, L.M.; Cai, H.; Shrubsole, M.J.; Bailey, C.E.; Idrees, K.; Shu, X.O. Outcomes of robotic-assisted liver surgery versus laparoscopic liver surgery for treatment of stage I hepatocellular carcinoma. Cancer 2022, 128, 762–769. [Google Scholar] [CrossRef]
- Lai, E.C.; Tang, C.N. Long-term Survival Analysis of Robotic Versus Conventional Laparoscopic Hepatectomy for Hepatocellular Carcinoma: A Comparative Study. Surg. Laparosc. Endosc. Percutan. Tech. 2016, 26, 162–166. [Google Scholar] [CrossRef]
- Lim, C.; Goumard, C.; Salloum, C.; Tudisco, A.; Napoli, N.; Boggi, U.; Azoulay, D.; Scatton, O. Outcomes after 3D laparoscopic and robotic liver resection for hepatocellular carcinoma: A multicenter comparative study. Surg. Endosc. 2021, 35, 3258–3266. [Google Scholar] [CrossRef]
- Magistri, P.; Tarantino, G.; Guidetti, C.; Assirati, G.; Olivieri, T.; Ballarin, R.; Coratti, A.; Di Benedetto, F. Laparoscopic versus robotic surgery for hepatocellular carcinoma: The first 46 consecutive cases. J. Surg. Res. 2017, 217, 92–99. [Google Scholar] [CrossRef]
- Pesi, B.; Bencini, L.; Moraldi, L.; Tofani, F.; Batignani, G.; Bechi, P.; Farsi, M.; Annecchiarico, M.; Coratti, A. Robotic Versus Open Liver Resection in Hepatocarcinoma: Surgical and Oncological Outcomes. Surg. Laparosc. Endosc. Percutan. Tech. 2021, 31, 468–474. [Google Scholar] [CrossRef]
- Wang, W.H.; Kuo, K.K.; Wang, S.N.; Lee, K.T. Oncological and surgical result of hepatoma after robot surgery. Surg. Endosc. 2018, 32, 3918–3924. [Google Scholar] [CrossRef]
- Mohan, A.; Wara, U.U.; Arshad Shaikh, M.T.; Rahman, R.M.; Zaidi, Z.A. Telesurgery and Robotics: An Improved and Efficient Era. Cureus 2021, 13, e14124. [Google Scholar] [CrossRef]
- Rana, R.; Gaur, P.; Agarwal, V.; Parthasarathy, H. Tremor Estimation and Removal in Robot-Assisted Surgery Using Lie Groups and EKF. Robotica 2019, 37, 1904–1921. [Google Scholar] [CrossRef]
- Kim, M.J.; Park, S.C.; Park, J.W.; Chang, H.J.; Kim, D.Y.; Nam, B.H.; Sohn, D.K.; Oh, J.H. Robot-assisted Versus Laparoscopic Surgery for Rectal Cancer: A Phase II Open Label Prospective Randomized Controlled Trial. Ann. Surg. 2018, 267, 243–251. [Google Scholar] [CrossRef] [PubMed]


| Publication | Population | Design | n (RAH) | n (LH) | n (OH) |
|---|---|---|---|---|---|
| Balzano 2021 [13] | Italy | Retrospective | 40 | 52 | |
| Chen 2017 [14] | Taiwan | Retrospective, PSM | 81 | 81 | |
| Duong 2021 [15] | USA | Retrospective, PSM | 123 | 369 | |
| Lai 2016 [16] | China | Retrospective | 95 | 35 | |
| Lim 2020 [17] | France | Retrospective | 44 | 49 (3D) | |
| Magistri 2017 [18] | Italy | Retrospective | 22 | 24 | |
| Pesi 2021 [19] | Italy | Retrospective | 23 | 31 | |
| Wang 2018 [20] | Taiwan | Retrospective | 63 | 177 |
| Bias Due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Results | Overall | |
|---|---|---|---|---|---|---|---|---|
| Balzano 2022 [13] | H | L | L | L | L | L | L | L |
| Chen 2017 [14] | L | L | L | L | L | L | L | L |
| Duong 2021 [15] | L | L | L | L | M | L | M | L |
| Lai 2016 [16] | L | L | L | L | L | L | L | L |
| Lim 2020 [17] | L | M | L | L | M | L | L | L |
| Magistri 2017 [18] | L | L | L | L | L | L | M | L |
| Pesi 2021 [19] | L | L | L | L | L | L | M | L |
| Wang 2018 [20] | L | M | L | L | L | L | L | L |
| Characteristics | RAH | LH | p |
|---|---|---|---|
| n = 324 | n = 613 | ||
| Sex | |||
| 233 (71.9%) | 380 (62.0%) | 0.98 |
| 91 (28.1%) | 233 (38.0%) | ||
| Age | |||
| 62.5 ± 0.21 | 63.05 ± 11.44 | 0.54 |
| 46–83 | 34–86 | ||
| Liver disease | |||
| 13 (4.0%) | 13 (2.1%) | 0.16 |
| 126 (38.9%) | 75 (12.2%) | ||
| 9 (2.8%) | 12 (2.0%) | ||
| 5 (1.5%) | 6 (1.0%) | ||
| 171 (52.8%) | 507 (82.7) | ||
| Cirrhosis | |||
| 161 (49.7%) | 137 (22.3%) | 0.27 |
| 40 (12.3%) | 107 (17.5%) | ||
| 123 (38.0%) | 369 (60.2%) | ||
| Primary surgery | |||
| 130 (40.1%) | 79 (12.9%) | 0.96 |
| 9 (2.8%) | 89 (14.5%) | ||
| 185 (57.1%) | 445 (72.6%) | ||
| Tumor size | |||
| 35.6 ± 21.3 | 31.9 ± 18.5 | 0.14 |
| 12–65 | Nov-58 | ||
| Surgery time | |||
| 204.4 ± 101.8 | 212.4 ± 80.4 | 0.49 |
| 95–390 | 80–256 | ||
| Pringle time | |||
| 34 ± 20.6 | 38.8 ± 23.6 | 0.11 |
| Hospital stay | |||
| 6.9 ± 4.9 | 6.7 ± 2.6 | 0.77 |
| Characteristics | RAH | OH | p |
|---|---|---|---|
| n = 167 | n = 289 | ||
| Sex | |||
| 61 (36.5%) | 146 (50.5%) | 0.9 |
| 25 (15.0%) | 62 (21.5%) | ||
| 81 (48.5%) | 81 (28.0%) | ||
| Liver disease | |||
| 2 (1.2%) | 3 (1.0%) | 0.7 |
| 68 (40.7%) | 155 (53.6%) | ||
| 3 (1.8%) | 0 | ||
| 0 | 0 | ||
| 94 (56.3%) | 131 (45.3%) | ||
| Cirrhosis | |||
| 54 (32.3%) | 64 (22.1%) | 0.4 |
| 50 (29.9%) | 48 (16.6%) | ||
| 63 (37.7%) | 177 (61.2%) | ||
| Child-Pugh Grade | |||
| 81 (48.5%) | 199 (68.8%) | 0.8 |
| 2 (1.2%) | 4 (1.4%) | ||
| 0 | 0 | ||
| 84 (50.3%) | 86 (29.8%) | ||
| Primary surgery | |||
| 63 (37.7%) | 177 (61.2%) | NA |
| 0 | 0 | ||
| 104 (62.3%) | 112 (38.8%) | ||
| TNM | |||
| 98 (58.7%) | 162 (56.1%) | 0.03 |
| 42 (25.1%) | 70 (24.2%) | ||
| 4 (2.4%) | 26 (9.0%) | ||
| 23 (13.8%) | 31 (10.7%) | ||
| Vascular invasion | |||
| 123 (73.7%) | 221 (76.5%) | 0.9 |
| 39 (23.3%) | 68 (23.5%) | ||
| 0 | 0 | ||
| 0 | 0 | ||
| Outcome | № of Included Studies | Certainty of the Evidence (GRADE) | Relative Effect (95% CI) |
|---|---|---|---|
| RAH versus LH Overall complications | 4 retrospective | Low | OR 0.61 [0.18; 2.06] |
| RAH versus OH Overall complications | 3 retrospective | Very Low | OR 0.76 [0.49; 1.18] |
| RAH versus LH Major complications | 3 retrospective | Very Low | OR 0.70 [0.48; 1.01] |
| RAH versus LH Minor complications | 3 retrospective | Very Low | OR 0.45 [0.10; 1.93] |
| RAH versus OH Minor complications | 3 retrospective | Very Low | OR 0.71 [0.28; 1.83] |
| RAH versus LH Infections | 3 retrospective | Very Low | OR 1.14 [0.09; 13.86] |
| RAH versus LH Transfusions | 3 retrospective | Very Low | OR 1.28 [0.01; 110.72] |
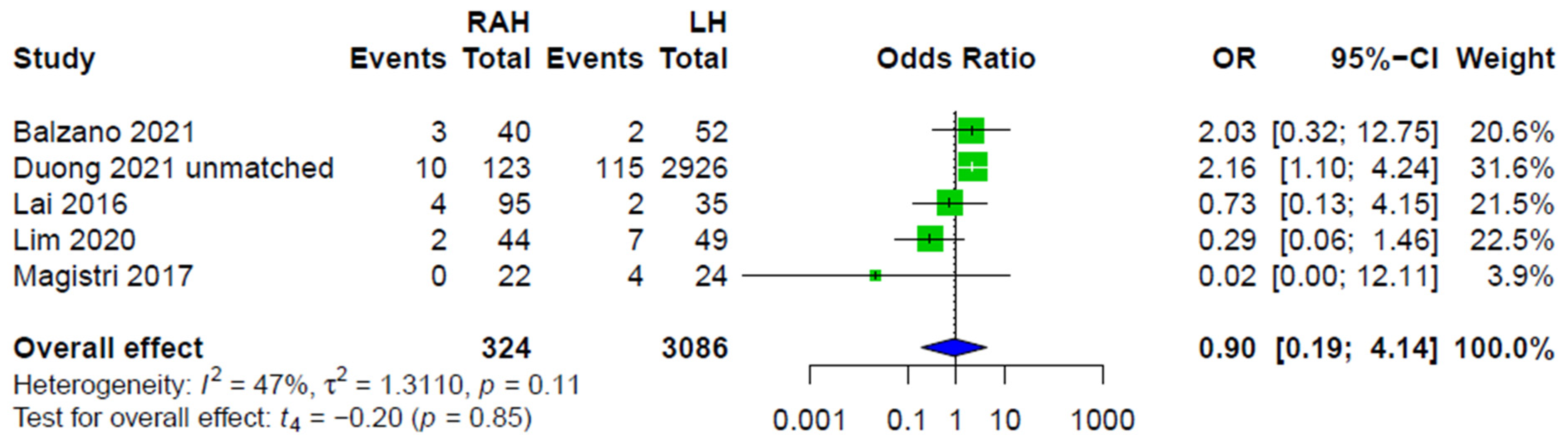
| RAH versus LH Conversions to OH | 5 retrospective | Low | OR 0.90 [0.19; 4.14] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murtha-Lemekhova, A.; Fuchs, J.; Hoffmann, K. Innovation for the Sake of Innovation? How Does Robotic Hepatectomy Compare to Laparoscopic or Open Resection for HCC—A Systematic Review and Meta-Analysis. Cancers 2022, 14, 3359. https://doi.org/10.3390/cancers14143359
Murtha-Lemekhova A, Fuchs J, Hoffmann K. Innovation for the Sake of Innovation? How Does Robotic Hepatectomy Compare to Laparoscopic or Open Resection for HCC—A Systematic Review and Meta-Analysis. Cancers. 2022; 14(14):3359. https://doi.org/10.3390/cancers14143359
Chicago/Turabian StyleMurtha-Lemekhova, Anastasia, Juri Fuchs, and Katrin Hoffmann. 2022. "Innovation for the Sake of Innovation? How Does Robotic Hepatectomy Compare to Laparoscopic or Open Resection for HCC—A Systematic Review and Meta-Analysis" Cancers 14, no. 14: 3359. https://doi.org/10.3390/cancers14143359
APA StyleMurtha-Lemekhova, A., Fuchs, J., & Hoffmann, K. (2022). Innovation for the Sake of Innovation? How Does Robotic Hepatectomy Compare to Laparoscopic or Open Resection for HCC—A Systematic Review and Meta-Analysis. Cancers, 14(14), 3359. https://doi.org/10.3390/cancers14143359






