Feasibility and Acceptability of Bright IDEAS-Young Adults: A Problem-Solving Skills Training Intervention
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Intervention
2.3. Procedures
2.4. Measures
2.4.1. Feasibility and Acceptability
2.4.2. Patient-Reported Outcomes
2.5. Analysis
3. Results
3.1. Feasibility
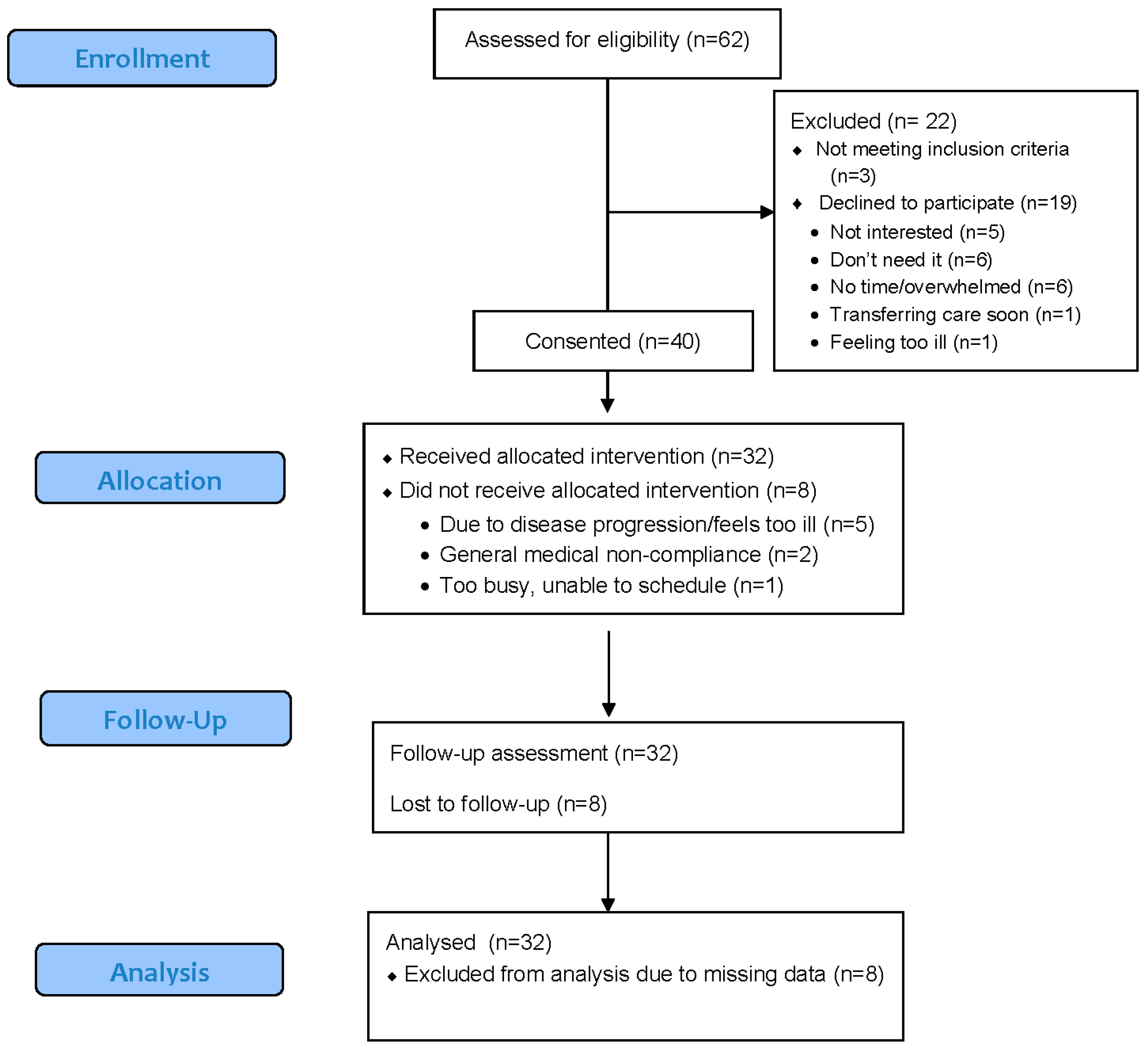
3.1.1. Enrollment and Retention
3.1.2. Participant Engagement and Satisfaction
3.2. Secondary Outcomes
3.2.1. Problem-Solving Skills
3.2.2. Anxiety
3.2.3. Depression
3.2.4. Quality of Life
3.2.5. Distress
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Zebrack, B.J.; Corbett, V.; Embry, L.; Aguilar, C.; Meeske, K.A.; Hayes-Lattin, B.; Block, R.; Zeman, D.T.; Cole, S. Psychological distress and unsatisfied need for psychosocial support in adolescent and young adult cancer patients during the first year following diagnosis. Psychooncology 2014, 23, 1267–1275. [Google Scholar] [CrossRef] [PubMed]
- Devins, G.M.; Bezjak, A.; Mah, K.; Loblaw, D.A.; Gotowiec, A.P. Context moderates illness-induced lifestyle disruptions across life domains: A test of the illness intrusiveness theoretical framework in six common cancers. Psychooncology 2006, 15, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.W.; Bellizzi, K.M.; Keegan, T.H.M.; Zebrack, B.; Chen, V.W.; Neale, A.V.; Hamilton, A.S.; Shnorhavorian, M.; Lynch, C.F. Health-related quality of life of adolescent and young adult patients with cancer in the United States: The Adolescent and Young Adult Health Outcomes and Patient Experience study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 2136–2145. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Wang, K.; Zebrack, B.; Tan, C.Y.; Walling, E.; Chugh, R. Psychosocial, behavioral, and supportive interventions for pediatric, adolescent, and young adult cancer survivors: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2021, 160, 103291. [Google Scholar] [CrossRef]
- Zebrack, B.J.; Block, R.; Hayes-Lattin, B.; Embry, L.; Aguilar, C.; Meeske, K.A.; Li, Y.; Butler, M.; Cole, S. Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer 2013, 119, 201–214. [Google Scholar] [CrossRef]
- Zebrack, B. Information and service needs for young adult cancer survivors. Supportive Care Cancer 2009, 17, 349–357. [Google Scholar] [CrossRef]
- Dyson, G.J.; Thompson, K.; Palmer, S.; Thomas, D.M.; Schofield, P. The relationship between unmet needs and distress amongst young people with cancer. Supportive Care Cancer 2012, 20, 75–85. [Google Scholar] [CrossRef]
- Keegan, T.H.M.; Lichtensztajn, D.Y.; Kato, I.; Kent, E.E.; Wu, X.-C.; West, M.M.; Hamilton, A.S.; Zebrack, B.; Bellizzi, K.M.; Smith, A.W.; et al. Unmet adolescent and young adult cancer survivors information and service needs: A population-based cancer registry study. J. Cancer Surviv. 2012, 6, 239–250. [Google Scholar] [CrossRef]
- Parsons, H.M.; Harlan, L.C.; Lynch, C.F.; Hamilton, A.S.; Wu, X.-C.; Kato, I.; Schwartz, S.M.; Smith, A.W.; Keel, G.; Keegan, T.H.M. Impact of cancer on work and education among adolescent and young adult cancer survivors. J. Clin. Oncol. 2012, 30, 2393–2400. [Google Scholar] [CrossRef]
- Smith, A.; Parsons, H.; Kent, E.; Bellizzi, K.; Zebrack, B.; Keel, G.; Lynch, C.; Rubenstein, M.; Keegan, T. Unmet Support Service Needs and Health-Related Quality of Life among Adolescents and Young Adults with Cancer: The AYA HOPE Study. Front. Oncol. 2013, 3, 75. [Google Scholar] [CrossRef] [PubMed]
- Sender, A.; Friedrich, M.; Leuteritz, K.; Nowe, E.; Stöbel-Richter, Y.; Mehnert, A.; Geue, K. Unmet supportive care needs in young adult cancer patients: Associations and changes over time. Results from the AYA-Leipzig study. J. Cancer Surviv. 2019, 13, 611–619. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.C.; McNeil, R.; Drew, S.; Orme, L.; Sawyer, S.M. Information needs of adolescent and young adult cancer patients and their parent-carers. Supportive Care Cancer 2018, 26, 1655–1664. [Google Scholar] [CrossRef] [PubMed]
- Quinn, G.P.; Gonçalves, V.; Sehovic, I.; Bowman, M.L.; Reed, D.R. Quality of life in adolescent and young adult cancer patients: A systematic review of the literature. Patient Relat. Outcome Meas 2015, 6, 19–51. [Google Scholar] [CrossRef]
- Barnett, M.; McDonnell, G.; DeRosa, A.; Schuler, T.; Philip, E.; Peterson, L.; Touza, K.; Jhanwar, S.; Atkinson, T.M.; Ford, J.S. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): A systematic review. J. Cancer Surviv. 2016, 10, 814–831. [Google Scholar] [CrossRef]
- Thornton, C.P.; Ruble, K.; Kozachik, S. Psychosocial Interventions for Adolescents and Young Adults with Cancer: An Integrative Review. J. Pediatric Oncol. Nurs. 2020, 37, 408–422. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, A.R.; Bradford, M.C.; McCauley, E.; Curtis, J.R.; Wolfe, J.; Baker, K.S.; Yi-Frazier, J.P. Promoting resilience in adolescents and young adults with cancer: Results from the PRISM randomized controlled trial. Cancer 2018, 124, 3909–3917. [Google Scholar] [CrossRef]
- Rosenberg, A.R.; Bradford, M.C.; Barton, K.S.; Etsekson, N.; McCauley, E.; Curtis, J.R.; Wolfe, J.; Baker, K.S.; Yi-Frazier, J.P. Hope and benefit finding: Results from the PRISM randomized controlled trial. Pediatric Blood Cancer 2019, 66, e27485. [Google Scholar] [CrossRef]
- D’Zurilla, T.; Nezu, A. Problem-Solving Therapy: A Positive Approach to Clinical Intervention, 3rd ed.; Springer Publishing Company: New York, NY, USA, 2007. [Google Scholar]
- Sahler, O.J.Z.; Fairclough, D.L.; Phipps, S.; Mulhern, R.K.; Dolgin, M.J.; Noll, R.B.; Katz, E.R.; Varni, J.W.; Copeland, D.R.; Butler, R.W. Using Problem-Solving Skills Training to Reduce Negative Affectivity in Mothers of Children with Newly Diagnosed Cancer: Report of a Multisite Randomized Trial. J. Consult. Clin. Psychol. 2005, 73, 272–283. [Google Scholar] [CrossRef]
- Sahler, O.J.Z.; Varni, J.W.; Fairclough, D.L.; Butler, R.W.; Noll, R.B.; Dolgin, M.J.; Phipps, S.; Copeland, D.R.; Katz, E.R.; Mulhern, R.K. Problem-Solving Skills Training for Mothers of Children with Newly Diagnosed Cancer: A Randomized Trial. J. Dev. Behav. Pediatrics 2002, 23, 77–86. [Google Scholar] [CrossRef]
- Sahler, O.J.Z.; Dolgin, M.J.; Phipps, S.; Fairclough, D.L.; Askins, M.A.; Katz, E.R.; Noll, R.B.; Butler, R.W. Specificity of problem-solving skills training in mothers of children newly diagnosed with cancer: Results of a multisite randomized clinical trial. J. Clin. Oncol. 2013, 31, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Young, M.; Voll, M.; Noll, R.B.; Fairclough, D.L.; Flanagan-Priore, C. Bright IDEAS problem-solving skills training for caregivers of children with sickle cell disease: A two-site pilot feasibility trial. Pediatric Blood Cancer 2021, 68, e28822. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.T.; Fairclough, D.L.; Noll, R.B. Problem-solving skills training for mothers of children recently diagnosed with autism spectrum disorder: A pilot feasibility study. Autism 2016, 20, 55–64. [Google Scholar] [CrossRef]
- Noyes, K.; Zapf, A.L.; Depner, R.M.; Flores, T.; Huston, A.; Rashid, H.H.; McNeal, D.; Constine, L.S.; Fleming, F.J.; Wilding, G.E.; et al. Problem-solving skills training in adult cancer survivors: Bright IDEAS-AC pilot study. Cancer Treat. Res. Commun. 2022, 31, 100552. [Google Scholar] [CrossRef] [PubMed]
- Orsmond, G.I.; Cohn, E.S. The distinctive features of a feasibility study: Objectives and guiding questions. OTJR Occup. Particip. Health 2015, 35, 169–177. [Google Scholar] [CrossRef]
- Phipps, S.; Fairclough, D.L.; Noll, R.B.; Devine, K.A.; Dolgin, M.J.; Schepers, S.A.; Askins, M.A.; Schneider, N.M.; Ingman, K.; Voll, M.; et al. In-person vs. web-based administration of a problem-solving skills intervention for parents of children with cancer: Report of a randomized noninferiority trial. EClinicalMedicine 2020, 24, 100428. [Google Scholar] [CrossRef]
- Sidani, S.; Epstein, D.R.; Fox, M. Psychometric evaluation of a multi-dimensional measure of satisfaction with behavioral interventions. Res. Nurs. Health 2017, 40, 459–469. [Google Scholar] [CrossRef]
- Hawkins, D.; Sofronoff, K.; Sheffield, J. Psychometric Properties of the Social Problem Solving Inventory-Revised Short-Form: Is the Short Form a Valid and Reliable Measure for Young Adults? Cogn. Ther. Res. 2009, 33, 462–470. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Distress management. Clinical practice guidelines. J. Natl. Compr. Cancer Netw. 2003, 1, 344–374. [Google Scholar] [CrossRef]
- Patterson, P.; McDonald, F.; Anazodo, A.; Dsj, C.; Wakefield, C.; White, K.; Thompson, K.; Osborn, M. Validation of the distress thermometer for use among adolescents and young adults with cancer in Australia: A multicenter study protocol. Clin. Oncol. Adolesc. Young Adults 2015, 5, 51–62. [Google Scholar] [CrossRef]
- Pilkonis, P.A.; Choi, S.W.; Reise, S.P.; Stover, A.M.; Riley, W.T.; Cella, D. Item Banks for Measuring Emotional Distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, Anxiety, and Anger. Assessment 2011, 18, 263–283. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Seid, M.; Kurtin, P.S. PedsQL™ 4.0: Reliability and Validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Limbers, C.A. The PedsQL™ 4.0 Generic Core Scales Young Adult Version: Feasibility, Reliability and Validity in a University Student Population. J. Health Psychol. 2009, 14, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Ewing, J.E.; King, M.T.; Smith, N.F. Validation of modified forms of the PedsQL generic core scales and cancer module scales for adolescents and young adults (AYA) with cancer or a blood disorder. Qual. Life Res. 2009, 18, 231–244. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Nass, S.J.; Beaupin, L.K.; Demark-Wahnefried, W.; Fasciano, K.; Ganz, P.A.; Hayes-Lattin, B.; Hudson, M.M.; Nevidjon, B.; Oeffinger, K.C.; Rechis, R.; et al. Identifying and Addressing the Needs of Adolescents and Young Adults with Cancer: Summary of an Institute of Medicine Workshop. Oncologist 2015, 20, 186–195. [Google Scholar] [CrossRef]
- Bibby, H.; White, V.; Thompson, K.; Anazodo, A. What Are the Unmet Needs and Care Experiences of Adolescents and Young Adults with Cancer? A Systematic Review. J. Adolesc. Young Adult Oncol. 2017, 6, 6–30. [Google Scholar] [CrossRef]
- Michelson, D.; Malik, K.; Parikh, R.; Weiss, H.A.; Doyle, A.M.; Bhat, B.; Sahu, R.; Chilhate, B.; Mathur, S.; Krishna, M.; et al. Effectiveness of a brief lay counsellor-delivered, problem-solving intervention for adolescent mental health problems in urban, low-income schools in India: A randomised controlled trial. Lancet Child Adolesc. Health 2020, 4, 571–582. [Google Scholar] [CrossRef]
- Cuijpers, P.; de Wit, L.; Kleiboer, A.; Karyotaki, E.; Ebert, D.D. Problem-solving therapy for adult depression: An updated meta-analysis. Eur. Psychiatry 2018, 48, 27–37. [Google Scholar] [CrossRef]
- Ferrari, A.; Stark, D.; Peccatori, F.A.; Fern, L.; Laurence, V.; Gaspar, N.; Bozovic-Spasojevic, I.; Smith, O.; De Munter, J.; Derwich, K.; et al. Adolescents and young adults (AYA) with cancer: A position paper from the AYA Working Group of the European Society for Medical Oncology (ESMO) and the European Society for Paediatric Oncology (SIOPE). ESMO Open 2021, 6, 100096. [Google Scholar] [CrossRef]
- Rabin, C.; Horowitz, S.; Marcus, B. Recruiting Young Adult Cancer Survivors for Behavioral Research. J. Clin. Psychol. Med. Settings 2013, 20, 33–36. [Google Scholar] [CrossRef]
- Kent, E.E.; Smith, A.W.; Keegan, T.H.M.; Lynch, C.F.; Wu, X.-C.; Hamilton, A.S.; Kato, I.; Schwartz, S.M.; Harlan, L.C. Talking about Cancer and Meeting Peer Survivors: Social Information Needs of Adolescents and Young Adults Diagnosed with Cancer. J. Adolesc. Young Adult Oncol. 2013, 2, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Berkanish, P.; Pan, S.; Viola, A.; Rademaker, Q.; Devine, K.A. Technology-Based Peer Support Interventions for Adolescents with Chronic Illness: A Systematic Review. J. Clin. Psychol. Med. Settings 2022, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Kaal, S.E.; Husson, O.; van Dartel, F.; Hermans, K.; Jansen, R.; Manten-Horst, E.; Servaes, P.; van de Belt, T.H.; Engelen, L.J.; Prins, J.B. Online support community for adolescents and young adults (AYAs) with cancer: User statistics, evaluation, and content analysis. Patient Prefer. Adherence 2018, 12, 2615. [Google Scholar] [CrossRef] [PubMed]
- Hendricks-Ferguson, V.L.; Cherven, B.O.; Burns, D.S.; Docherty, S.L.; Phillips-Salimi, C.R.; Roll, L.; Stegenga, K.A.; Donovan Stickler, M.; Haase, J.E. Recruitment Strategies and Rates of a Multi-Site Behavioral Intervention for Adolescents and Young Adults With Cancer. J. Pediatric Health Care 2013, 27, 434–442. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Characteristic | M (SD) or n (%) |
|---|---|
| Current Age in Years, M(SD) | 23.9 (3.3) |
| Range | 18–29 |
| Female, n (%) | 20 (50%) |
| Race, n (%) | |
| White | 18 (45.0%) |
| Black | 5 (12.5%) |
| Asian | 4 (10.0%) |
| More than one race | 1 (2.5%) |
| Other/Unknown/missing | 12 (30.0%) |
| Hispanic Ethnicity, n (%) | 17 (42.5%) |
| Single/Never Married, n (%) | 36 (90.0%) |
| Employment Status, n (%) | |
| Working Full-Time | 22 (55.0%) |
| Full-Time Student | 5 (12.5%) |
| Employed Part-Time/Student | 6 (15.0%) |
| Unemployed | 6 (15.0%) |
| Homemaker/Caregiver | 1 (2.5%) |
| Highest Grade Completed, n (%) | |
| Less than HS | 1 (2.5%) |
| High School/GED | 18 (45.0%) |
| 2-year College | 8 (20.0%) |
| 4-year Degree | 10 (25.0%) |
| Graduate Degree | 3 (7.5%) |
| Health Insurance, n (%) | |
| Public | 16 (35.0%) |
| Private | 19 (47.5%) |
| Charity care | 4 (10.0%) |
| I do not know | 1 (2.5%) |
| Cancer diagnosis, n (%) | |
| Blood cancers | 30 (75.0%) |
| Solid Tumors | 10 (25.0%) |
| Time since diagnosis in weeks, Md (min-max) | 7.0 (3–86) |
| Clinic type, n (%) | |
| Adult | 33 (82.5%) |
| Pediatric | 7 (17.5%) |
| N a | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree | Mean (SD) | |
|---|---|---|---|---|---|---|---|
| I can see myself using the Bright IDEAS system of problem-solving | 32 | 3.10% | 0% | 3.10% | 46.90% | 46.90% | 4.34 (0.83) |
| After I learned the Bright IDEAS system, I thought it might be useful for friends and family | 32 | 3.10% | 0% | 12.50% | 28.10% | 56.30% | 4.34 (0.94) |
| I have explained Bright IDEAS to another person | 32 | 3.10% | 6.30% | 21.90% | 37.50% | 31.30% | 3.87 (1.04) |
| I have solved a problem using Bright IDEAS | 32 | 0% | 0% | 3.10% | 34.40% | 62.50% | 4.59 (0.46) |
| The Bright IDEAS program was useful a | 22 | 0% | 0% | 0% | 40.90% | 59.10% | 4.59 (0.50) |
| The worksheets were helpful a | 22 | 0% | 4.50% | 13.60% | 36.40% | 45.50% | 4.23 (0.87) |
| The manual explaining the program was easy to understand a | 22 | 0% | 0% | 13.60% | 40.90% | 45.50% | 4.32 (0.72) |
| It was easy to talk with my trainer a | 22 | 0% | 0% | 0% | 9.10% | 90.90% | 4.91 (0.29) |
| Prompt | Theme | Definition | Illustrative Quotes |
|---|---|---|---|
| What did you like best? | Bright IDEAS approach | Learning ways to solve problems, worksheets, ease of use, motivation to act. | “…the best that I was able to learn how to approach my problems from systematic way…” “…it made my concerns seem more manageable and less overwhelming…” “Finding new solution whenever I gotten stuck on an issue…” “easy to use and effective” |
| Trainer | Someone to talk to, therapeutic | “I really enjoyed my long discussions with my trainer.” “…its like (having) a personal therapist!” “the person who listens to us…whatever we are experiencing right now.” | |
| What did you like least? | Scheduling | Treatment schedule makes difficult to complete; clinic setting is stressful | “The space between meetings due to my treatment regimen.” “Sometimes it was during treatment when I was stressed” |
| Worksheets | Homework was burdensome | “I didn’t always enjoy getting ‘homework’ assignments.” “Writing stuff down, it really did not help me. It might have helped other people. For me the worksheets and stuff was kind of juvenile. Just talking and going through it helped me.” | |
| What could we improve? | Format | Add group/peer community component; use videocall (instead of phone) | “being able to work in group sessions” “add a group session online. People can join the group and talk to each other’s story and experience.” “Facetime might be better [than phone], its more personable, it puts face to the voice, it kinda makes it more…human.” |
| Scheduling | Recruit closer to diagnosis; give more time to solve problems; add follow-up after treatment is over | “if you start it with other people, make sure they are at the beginning, because I think it will help in the beginning.” “probably given more time to solve the problems or experience them.” |
| Baseline M (SD) | Post-Intervention M (SD) | Mean Difference [95% CI] | p | d | |
|---|---|---|---|---|---|
| SPSI-R:S | 13.90 (2.79) | 15.18 (2.24) | 1.28 [0.43, 2.12] | <0.01 | 0.54 |
| PPO | 2.71(0.83) | 2.96 (0.76) | 0.25 [0.05, 0.45] | 0.02 | 0.44 |
| NPO | 2.84 (0.90) | 3.08 (0.61) | 0.24 [−0.02, 0.50] | 0.07 | 0.34 |
| RPS | 2.44 (0.99) | 2.91 (0.78) | 0.47 [0.21, 0.73] | <0.01 | 0.65 |
| ICS | 2.79 (0.59) | 2.86 (0.56) | 0.07 [−0.13, 0.27] | 0.50 | 0.12 |
| AS | 3.13 (0.71) | 3.38 (0.52) | 0.24 [−0.05, 0.54] | 0.10 | 0.30 |
| PROMIS—Anxiety T-score | 51.98 (11.03) | 49.52 (9.15) | −2.46 [−5.90, 0.99] | 0.16 | −0.26 |
| PROMIS—Depression T-score | 48.68 (9.62) | 45.50 (8.46) | −3.18 [−6.35, −0.002] | 0.05 | −0.36 |
| PedsQL Total | 70.75 (16.61) | 72.82 (14.81) | 2.07 [−2.48, 6.62] | 0.36 | 0.16 |
| Distress | 3.16 (2.81) | 2.06 (2.16) | −1.10 [−1.96, −0.23] | 0.02 | −0.47 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viola, A.S.; Kwok, G.; Levonyan-Radloff, K.; Manne, S.L.; Noll, R.B.; Phipps, S.; Sahler, O.J.Z.; Devine, K.A. Feasibility and Acceptability of Bright IDEAS-Young Adults: A Problem-Solving Skills Training Intervention. Cancers 2022, 14, 3124. https://doi.org/10.3390/cancers14133124
Viola AS, Kwok G, Levonyan-Radloff K, Manne SL, Noll RB, Phipps S, Sahler OJZ, Devine KA. Feasibility and Acceptability of Bright IDEAS-Young Adults: A Problem-Solving Skills Training Intervention. Cancers. 2022; 14(13):3124. https://doi.org/10.3390/cancers14133124
Chicago/Turabian StyleViola, Adrienne S., Gary Kwok, Kristine Levonyan-Radloff, Sharon L. Manne, Robert B. Noll, Sean Phipps, Olle Jane Z. Sahler, and Katie A. Devine. 2022. "Feasibility and Acceptability of Bright IDEAS-Young Adults: A Problem-Solving Skills Training Intervention" Cancers 14, no. 13: 3124. https://doi.org/10.3390/cancers14133124
APA StyleViola, A. S., Kwok, G., Levonyan-Radloff, K., Manne, S. L., Noll, R. B., Phipps, S., Sahler, O. J. Z., & Devine, K. A. (2022). Feasibility and Acceptability of Bright IDEAS-Young Adults: A Problem-Solving Skills Training Intervention. Cancers, 14(13), 3124. https://doi.org/10.3390/cancers14133124






