Effect of Treatment in a Specialized Pediatric Hemato-Oncology Setting on 5-Year Survival in Acute Lymphoblastic Leukemia: A Quasi-Experimental Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Variables
2.3. Design
2.4. Statistical Analysis
3. Results
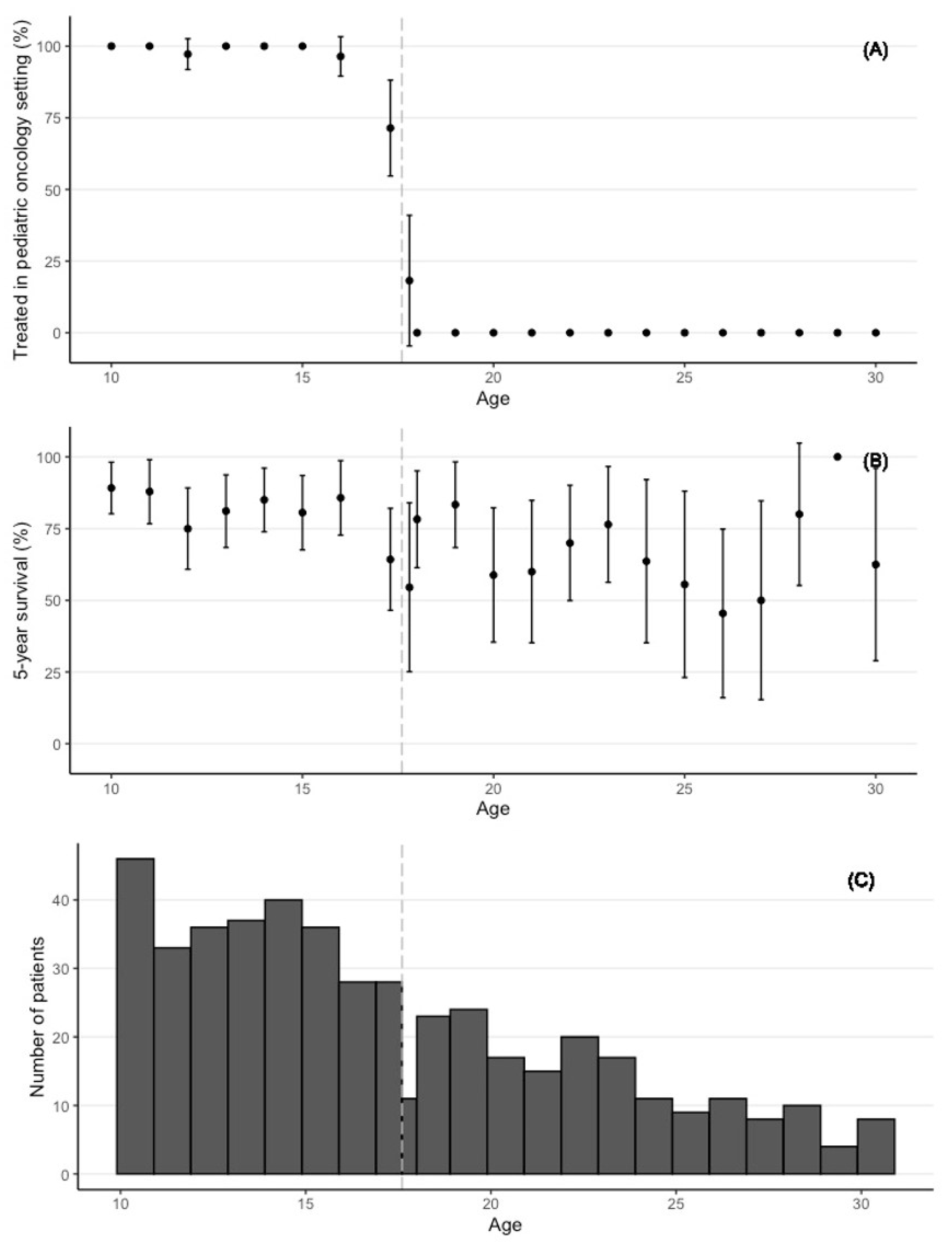
3.1. Descriptive Statistics of the Study Sample
3.2. Estimation Results
4. Discussion
4.1. Summary and Discussion of Main Findings
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hunger, S.P.; Mullighan, C.G. Acute Lymphoblastic Leukemia in Children. N. Engl. J. Med. 2015, 373, 1541–1552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reedijk, A.M.J.; Coebergh, J.W.W.; de Groot-Kruseman, H.A.; van der Sluis, I.M.; Kremer, L.C.; Karim-Kos, H.E.; Pieters, R. Progress against childhood and adolescent acute lymphoblastic leukaemia in the Netherlands, 1990–2015. Leukemia 2021, 35, 1001–1011. [Google Scholar] [CrossRef] [PubMed]
- Boissel, N.; Baruchel, A. Acute lymphoblastic leukemia in adolescent and young adults: Treat as adults or as children? Blood 2018, 132, 351–361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrison, C.J. Cytogenetics of paediatric and adolescent acute lymphoblastic leukaemia. Br. J. Haematol. 2009, 144, 147–156. [Google Scholar] [CrossRef]
- Trama, A.; Botta, L.; Foschi, R.; Ferrari, A.; Stiller, C.; Desandes, E.; Maule, M.M.; Merletti, F.; Gatta, G.; Group, E.-W. Survival of European adolescents and young adults diagnosed with cancer in 2000–07: Population-based data from EUROCARE-5. Lancet Oncol. 2016, 17, 896–906. [Google Scholar] [CrossRef] [Green Version]
- Keegan, T.H.; Ries, L.A.; Barr, R.D.; Geiger, A.M.; Dahlke, D.V.; Pollock, B.H.; Bleyer, W.A.; National Cancer Institute Next Steps for, A.; Young Adult Oncology Epidemiology Working, G. Comparison of cancer survival trends in the United States of adolescents and young adults with those in children and older adults. Cancer 2016, 122, 1009–1016. [Google Scholar] [CrossRef]
- Reedijk, A.M.J.; van der Heiden-van der Loo, M.; Visser, O.; Karim-Kos, H.E.; Lieverst, J.A.; de Ridder-Sluiter, J.G.; Coebergh, J.W.W.; Kremer, L.C.; Pieters, R. Site of childhood cancer care in the Netherlands. Eur. J. Cancer 2017, 87, 38–46. [Google Scholar] [CrossRef]
- Boissel, N.; Auclerc, M.F.; Lheritier, V.; Perel, Y.; Thomas, X.; Leblanc, T.; Rousselot, P.; Cayuela, J.M.; Gabert, J.; Fegueux, N.; et al. Should adolescents with acute lymphoblastic leukemia be treated as old children or young adults? Comparison of the French FRALLE-93 and LALA-94 trials. J. Clin. Oncol. 2003, 21, 774–780. [Google Scholar] [CrossRef]
- de Bont, J.M.; Holt, B.; Dekker, A.W.; van der Does-van den Berg, A.; Sonneveld, P.; Pieters, R. Significant difference in outcome for adolescents with acute lymphoblastic leukemia treated on pediatric vs. adult protocols in the Netherlands. Leukemia 2004, 18, 2032–2035. [Google Scholar] [CrossRef]
- Stock, W.; La, M.; Sanford, B.; Bloomfield, C.D.; Vardiman, J.W.; Gaynon, P.; Larson, R.A.; Nachman, J.; Children’s Cancer Group; Cancer and Leukemia Group B studies. What determines the outcomes for adolescents and young adults with acute lymphoblastic leukemia treated on cooperative group protocols? A comparison of Children’s Cancer Group and Cancer and Leukemia Group B studies. Blood 2008, 112, 1646–1654. [Google Scholar] [CrossRef] [Green Version]
- Dinmohamed, A.G.; Szabo, A.; van der Mark, M.; Visser, O.; Sonneveld, P.; Cornelissen, J.J.; Jongen-Lavrencic, M.; Rijneveld, A.W. Improved survival in adult patients with acute lymphoblastic leukemia in the Netherlands: A population-based study on treatment, trial participation and survival. Leukemia 2016, 30, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Norgaard, M.; Ehrenstein, V.; Vandenbroucke, J.P. Confounding in observational studies based on large health care databases: Problems and potential solutions—A primer for the clinician. Clin. Epidemiol. 2017, 9, 185–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hilton Boon, M.; Craig, P.; Thomson, H.; Campbell, M.; Moore, L. Regression Discontinuity Designs in Health: A Systematic Review. Epidemiology 2021, 32, 87–93. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; le Cessie, S. Commentary: Regression discontinuity design: Let’s give it a try to evaluate medical and public health interventions. Epidemiology 2014, 25, 738–741. [Google Scholar] [CrossRef] [PubMed]
- Venkataramani, A.S.; Bor, J.; Jena, A.B. Regression discontinuity designs in healthcare research. BMJ 2016, 352, i1216. [Google Scholar] [CrossRef] [Green Version]
- Normand, S.L.; McNeil, B.J. What is evidence? Stat. Med. 2010, 29, 1985–1988, discussion 1996–1987. [Google Scholar] [CrossRef]
- Basch, E.; Aronson, N.; Berg, A.; Flum, D.; Gabriel, S.; Goodman, S.N.; Helfand, M.; Ioannidis, J.P.A.; Lauer, M.; Meltzer, D.; et al. Methodological standards and patient-centeredness in comparative effectiveness research: The PCORI perspective. JAMA 2012, 307, 1636–1640. [Google Scholar] [CrossRef]
- van der Meer, D.J.; Karim-Kos, H.E.; van der Mark, M.; Aben, K.K.H.; Bijlsma, R.M.; Rijneveld, A.W.; van der Graaf, W.T.A.; Husson, O. Incidence, Survival, and Mortality Trends of Cancers Diagnosed in Adolescents and Young Adults (15–39 Years): A Population-Based Study in The Netherlands 1990–2016. Cancers 2020, 12, 3421. [Google Scholar] [CrossRef]
- Kyriacou, D.N.; Lewis, R.J. Confounding by Indication in Clinical Research. JAMA 2016, 316, 1818–1819. [Google Scholar] [CrossRef]
- Been, J.V.; Burgos Ochoa, L.; Bertens, L.C.M.; Schoenmakers, S.; Steegers, E.A.P.; Reiss, I.K.M. Impact of COVID-19 mitigation measures on the incidence of preterm birth: A national quasi-experimental study. Lancet Public Health 2020, 5, e604–e611. [Google Scholar] [CrossRef]
- Bor, J.; Ahmed, S.; Fox, M.P.; Rosen, S.; Meyer-Rath, G.; Katz, I.T.; Tanser, F.; Pillay, D.; Barnighausen, T. Effect of eliminating CD4-count thresholds on HIV treatment initiation in South Africa: An empirical modeling study. PLoS ONE 2017, 12, e0178249. [Google Scholar] [CrossRef] [Green Version]
- Melamed, A.; Fink, G.; Wright, A.A.; Keating, N.L.; Gockley, A.A.; Del Carmen, M.G.; Schorge, J.O.; Rauh-Hain, J.A. Effect of adoption of neoadjuvant chemotherapy for advanced ovarian cancer on all cause mortality: Quasi-experimental study. BMJ 2018, 360, j5463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Sudharsanan, N.; Huang, F.; Liu, Y.; Geldsetzer, P.; Barnighausen, T. Impact of community based screening for hypertension on blood pressure after two years: Regression discontinuity analysis in a national cohort of older adults in China. BMJ 2019, 366, l4064. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goulden, R.; Rowe, B.H.; Abrahamowicz, M.; Strumpf, E.; Tamblyn, R. Association of Intravenous Radiocontrast with Kidney Function: A Regression Discontinuity Analysis. JAMA Intern. Med. 2021, 181, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Bor, J.; Moscoe, E.; Mutevedzi, P.; Newell, M.L.; Barnighausen, T. Regression discontinuity designs in epidemiology: Causal inference without randomized trials. Epidemiology 2014, 25, 729–737. [Google Scholar] [CrossRef] [Green Version]
- O’Keeffe, A.G.; Geneletti, S.; Baio, G.; Sharples, L.D.; Nazareth, I.; Petersen, I. Regression discontinuity designs: An approach to the evaluation of treatment efficacy in primary care using observational data. BMJ 2014, 349, g5293. [Google Scholar] [CrossRef] [Green Version]
- Oldenburg, C.E.; Moscoe, E.; Barnighausen, T. Regression Discontinuity for Causal Effect Estimation in Epidemiology. Curr. Epidemiol. Rep. 2016, 3, 233–241. [Google Scholar] [CrossRef] [Green Version]
- Boef, A.G.; Dekkers, O.M.; Vandenbroucke, J.P.; le Cessie, S. Sample size importantly limits the usefulness of instrumental variable methods, depending on instrument strength and level of confounding. J. Clin. Epidemiol. 2014, 67, 1258–1264. [Google Scholar] [CrossRef]
- Martens, E.P.; Pestman, W.R.; de Boer, A.; Belitser, S.V.; Klungel, O.H. Instrumental variables: Application and limitations. Epidemiology 2006, 17, 260–267. [Google Scholar] [CrossRef]
- Lousdal, M.L. An introduction to instrumental variable assumptions, validation and estimation. Emerg. Themes Epidemiol. 2018, 15, 1. [Google Scholar] [CrossRef] [Green Version]
- Bleyer, A.; Budd, T.; Montello, M. Adolescents and young adults with cancer: The scope of the problem and criticality of clinical trials. Cancer 2006, 107, 1645–1655. [Google Scholar] [CrossRef] [PubMed]
- Parsons, H.M.; Harlan, L.C.; Seibel, N.L.; Stevens, J.L.; Keegan, T.H. Clinical trial participation and time to treatment among adolescents and young adults with cancer: Does age at diagnosis or insurance make a difference? J. Clin. Oncol 2011, 29, 4045–4053. [Google Scholar] [CrossRef] [PubMed]
- Onciu, M. Acute lymphoblastic leukemia. Hematol. Oncol. Clin. North Am. 2009, 23, 655–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holowiecki, J.; Krawczyk-Kulis, M.; Giebel, S.; Jagoda, K.; Stella-Holowiecka, B.; Piatkowska-Jakubas, B.; Paluszewska, M.; Seferynska, I.; Lewandowski, K.; Kielbinski, M.; et al. Status of minimal residual disease after induction predicts outcome in both standard and high-risk Ph-negative adult acute lymphoblastic leukaemia. The Polish Adult Leukemia Group ALL 4-2002 MRD Study. Br. J. Haematol. 2008, 142, 227–237. [Google Scholar] [CrossRef]
- Cave, H.; van der Werff ten Bosch, J.; Suciu, S.; Guidal, C.; Waterkeyn, C.; Otten, J.; Bakkus, M.; Thielemans, K.; Grandchamp, B.; Vilmer, E.; et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia. European Organization for Research and Treatment of Cancer—Childhood Leukemia Cooperative Group. N. Engl. J. Med. 1998, 339, 591–598. [Google Scholar] [CrossRef]
- Giebel, S.; Marks, D.I.; Boissel, N.; Baron, F.; Chiaretti, S.; Ciceri, F.; Cornelissen, J.J.; Doubek, M.; Esteve, J.; Fielding, A.; et al. Hematopoietic stem cell transplantation for adults with Philadelphia chromosome-negative acute lymphoblastic leukemia in first remission: A position statement of the European Working Group for Adult Acute Lymphoblastic Leukemia (EWALL) and the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant. 2019, 54, 798–809. [Google Scholar] [CrossRef] [Green Version]
- Wieduwilt, M.J.; Stock, W.; Advani, A.; Luger, S.; Larson, R.A.; Tallman, M.; Appelbaum, F.; Zhang, M.J.; Bo-Subait, K.; Wang, H.L.; et al. Superior survival with pediatric-style chemotherapy compared to myeloablative allogeneic hematopoietic cell transplantation in older adolescents and young adults with Ph-negative acute lymphoblastic leukemia in first complete remission: Analysis from CALGB 10403 and the CIBMTR. Leukemia 2021, 35, 2076–2085. [Google Scholar] [CrossRef]
- Seftel, M.D.; Neuberg, D.; Zhang, M.J.; Wang, H.L.; Ballen, K.K.; Bergeron, J.; Couban, S.; Freytes, C.O.; Hamadani, M.; Kharfan-Dabaja, M.A.; et al. Pediatric-inspired therapy compared to allografting for Philadelphia chromosome-negative adult ALL in first complete remission. Am. J. Hematol. 2016, 91, 322–329. [Google Scholar] [CrossRef] [Green Version]
- Bhatia, S.; Landier, W.; Hageman, L.; Chen, Y.; Kim, H.; Sun, C.L.; Kornegay, N.; Evans, W.E.; Angiolillo, A.L.; Bostrom, B.; et al. Systemic Exposure to Thiopurines and Risk of Relapse in Children with Acute Lymphoblastic Leukemia: A Children’s Oncology Group Study. JAMA Oncol. 2015, 1, 287–295. [Google Scholar] [CrossRef]
- Bhatia, S.; Landier, W.; Shangguan, M.; Hageman, L.; Schaible, A.N.; Carter, A.R.; Hanby, C.L.; Leisenring, W.; Yasui, Y.; Kornegay, N.M.; et al. Nonadherence to oral mercaptopurine and risk of relapse in Hispanic and non-Hispanic white children with acute lymphoblastic leukemia: A report from the children’s oncology group. J. Clin. Oncol 2012, 30, 2094–2101. [Google Scholar] [CrossRef]
- Bleyer, A. Important factors improving outcome of young adults with acute lymphoblastic leukemia (ALL). Best Pract. Res. Clin. Haematol. 2021, 34, 101322. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, J.; Sun, C.L.; Wyatt, L.; Stock, W.; Bhatia, S. Adolescents and Young Adults with Acute Lymphoblastic Leukemia and Acute Myeloid Leukemia: Impact of Care at Specialized Cancer Centers on Survival Outcome. Cancer Epidemiol. Biomark. Prev. 2017, 26, 312–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hough, R.; Sandhu, S.; Khan, M.; Moran, A.; Feltbower, R.; Stiller, C.; Stevens, M.C.G.; Rowntree, C.; Vora, A.; McCabe, M.G. Are survival and mortality rates associated with recruitment to clinical trials in teenage and young adult patients with acute lymphoblastic leukaemia? A retrospective observational analysis in England. BMJ Open 2017, 7, e017052. [Google Scholar] [CrossRef] [PubMed]
- Parsons, H.M.; Penn, D.C.; Li, Q.; Cress, R.D.; Pollock, B.H.; Malogolowkin, M.H.; Wun, T.; Keegan, T.H.M. Increased clinical trial enrollment among adolescent and young adult cancer patients between 2006 and 2012–2013 in the United States. Pediatr. Blood Cancer 2019, 66, e27426. [Google Scholar] [CrossRef]
- van der Sanden, G.A.; Coebergh, J.W.; Schouten, L.J.; Visser, O.; van Leeuwen, F.E. Cancer incidence in The Netherlands in 1989 and 1990: First results of the nationwide Netherlands cancer registry. Coordinating Committee for Regional Cancer Registries. Eur. J. Cancer 1995, 31A, 1822–1829. [Google Scholar] [CrossRef]
- Graubert, T.A. A call to action for acute lymphoblastic leukemia. N. Engl. J. Med. 2014, 371, 1064–1066. [Google Scholar] [CrossRef]
- Leeuwen, N.V. Design and Analysis of Randomized and Non-randomized Studies: Improving Validity and Reliability; Erasmus University Rotterdam: Rotterdam, The Netherlands, 2019. [Google Scholar]
| Total | 10 Years–17 Years and 7 Months (Treatment Group) | 17 Years and 7 Months–30 Years (Control Group) | |
|---|---|---|---|
| N (%) | 472 (100) | 284 (100) | 188 (100) |
| Treatment setting | |||
| Pediatric hemato-oncology [N (%)] | 276 (58.5) | 274 (96.5) | 2 (1.1) |
| Adult hemato-oncology [N (%)] | 196 (41.5) | 10 (3.5) | 186 (98.9) |
| Alive 5 years after diagnosis [N (%)] | 360 (76.3) | 232 (81.7) | 128 (68.1) |
| Age at diagnosis (years) | |||
| Median (interquartile range) | 16 (13–20) | 13 (11–15) | 22 (19–25) |
| Sex | |||
| Male [N (%)] | 296 (62.7) | 180 (63.4) | 116 (61.7) |
| Female [N (%)] | 176 (37.3) | 104 (36.6) | 72 (38.3) |
| Immunophenotype * | |||
| BCP-ALL [N (%)] | 346 (73.3) | 211 (74.3) | 135 (71.8) |
| T-cell ALL [N (%)] | 126 (26.7) | 73 (25.7) | 53 (28.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Linde, M.; van Leeuwen, N.; Eijkenaar, F.; Rijneveld, A.W.; Pieters, R.; Karim-Kos, H.E. Effect of Treatment in a Specialized Pediatric Hemato-Oncology Setting on 5-Year Survival in Acute Lymphoblastic Leukemia: A Quasi-Experimental Study. Cancers 2022, 14, 2451. https://doi.org/10.3390/cancers14102451
van der Linde M, van Leeuwen N, Eijkenaar F, Rijneveld AW, Pieters R, Karim-Kos HE. Effect of Treatment in a Specialized Pediatric Hemato-Oncology Setting on 5-Year Survival in Acute Lymphoblastic Leukemia: A Quasi-Experimental Study. Cancers. 2022; 14(10):2451. https://doi.org/10.3390/cancers14102451
Chicago/Turabian Stylevan der Linde, Margrietha, Nikki van Leeuwen, Frank Eijkenaar, Anita W. Rijneveld, Rob Pieters, and Henrike E. Karim-Kos. 2022. "Effect of Treatment in a Specialized Pediatric Hemato-Oncology Setting on 5-Year Survival in Acute Lymphoblastic Leukemia: A Quasi-Experimental Study" Cancers 14, no. 10: 2451. https://doi.org/10.3390/cancers14102451
APA Stylevan der Linde, M., van Leeuwen, N., Eijkenaar, F., Rijneveld, A. W., Pieters, R., & Karim-Kos, H. E. (2022). Effect of Treatment in a Specialized Pediatric Hemato-Oncology Setting on 5-Year Survival in Acute Lymphoblastic Leukemia: A Quasi-Experimental Study. Cancers, 14(10), 2451. https://doi.org/10.3390/cancers14102451






