Perioperative Management of Complex Hepatectomy for Colorectal Liver Metastases: The Alliance between the Surgeon and the Anesthetist
Abstract
Simple Summary
Abstract
1. Introduction
2. Preoperative Considerations
3. General Anesthesia Management and Intraoperative Hemodynamics
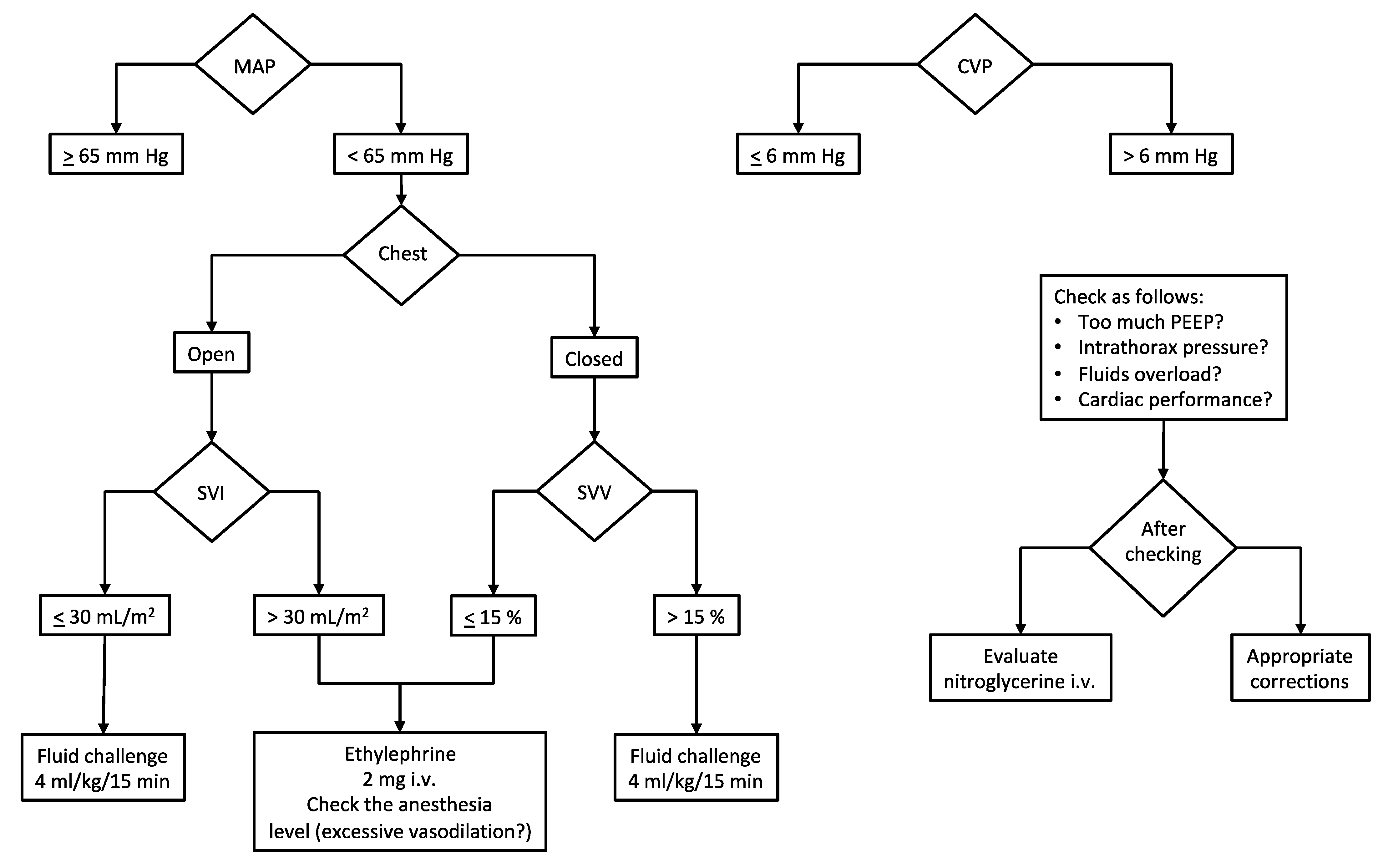
3.1. How Much Fluid Does a Patient Need?
3.2. How to Manage CVP?
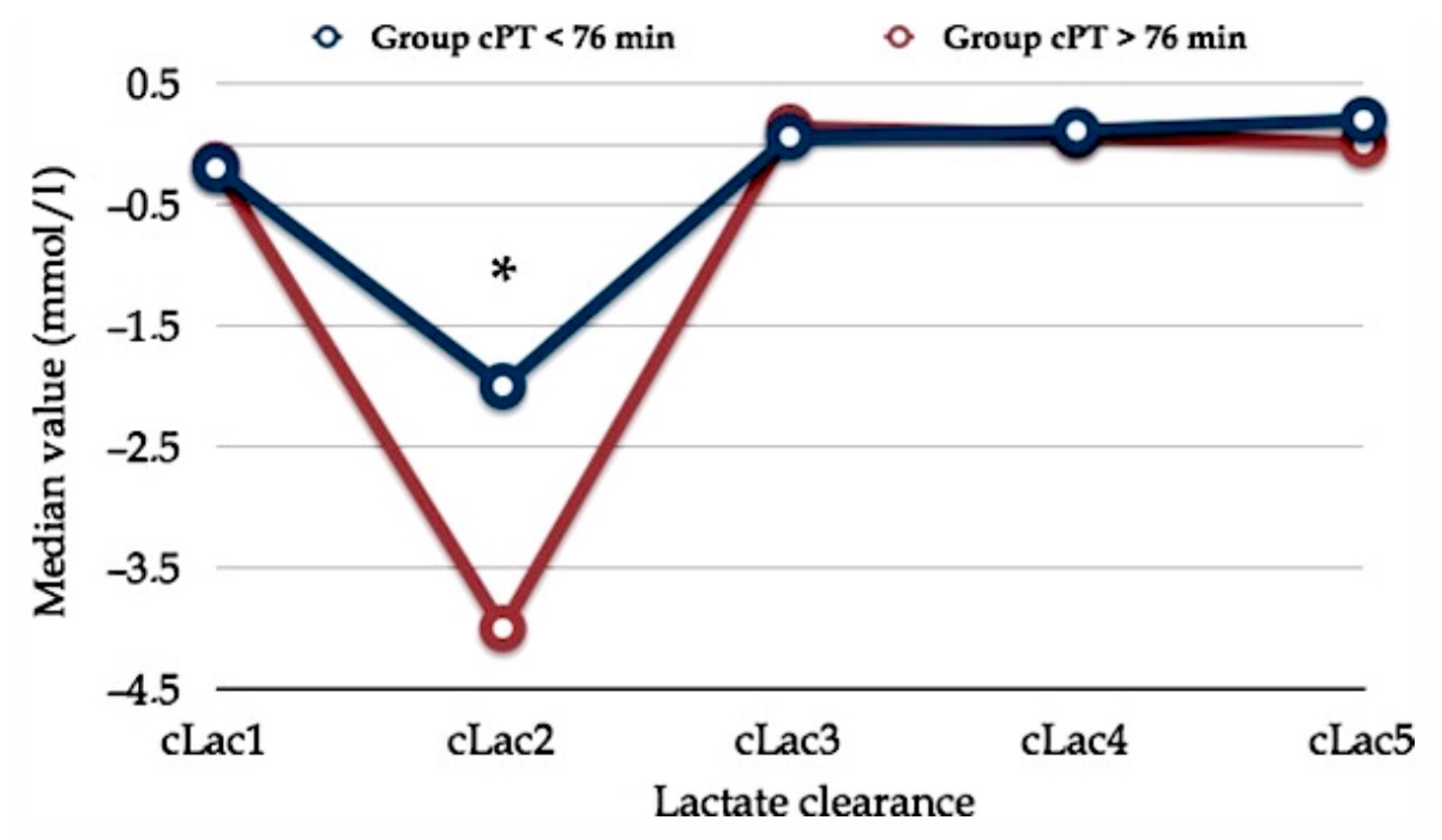
4. Intraoperative Acid–Base Balance and Metabolic Issues
5. Blood-Derivative Products
6. Postoperative Analgesia
7. Postoperative Complications
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hartog, A.; Mills, G. Anesthesia for hepatic resection surgery. Contin. Educ. Anaesth. Crit. Care Pain 2009, 9, 1–5. [Google Scholar] [CrossRef]
- Valderrama-Treviño, A.I.; Barrera-Mera, B.; Ceballos-Villalva, J.C.; Montalvo-Javé, E.E. Hepatic Metastasis from Colorectal Cancer. Euroasian J. Hepatogastroenterol. 2017, 7, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H.; Wilmore, D.W. Fast-track surgery. Br. J. Surg. 2005, 92, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Melloul, E.; Hübner, M.; Scott, M.; Snowden, C.; Prentis, J.; Dejong, C.H.; Garden, O.J.; Farges, O.; Kokudo, N.; Vauthey, J.N.; et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J. Surg. 2016, 40, 2425–2440. [Google Scholar] [CrossRef]
- Wei, A.C.; Greig, P.D.; Grant, D.; Taylor, B.; Langer, B.; Gallinger, S. Survival after hepatic resection for colorectal metastases: A 10-year experience. Ann. Surg. Oncol. 2006, 13, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Belghiti, J.; Hiramatsu, K.; Benoist, S.; Massault, P.; Sauvanet, A.; Farges, O. Seven hundred forty-seven hepatectomies in the 1990s: An update to evaluate the actual risk of liver resection. J. Am. Coll. Surg. 2000, 191, 38–46. [Google Scholar] [CrossRef]
- Jarnagin, W.R.; Gonen, M.; Fong, Y.; DeMatteo, R.P.; Ben-Porat, L.; Little, S.; Corvera, C.; Weber, S.; Blumgart, L.H. Improvement in perioperative outcome after hepatic resection: Analysis of 1,803 consecutive cases over the past decade. Ann. Surg. 2002, 236, 397–406, discussion 406–407. [Google Scholar] [CrossRef] [PubMed]
- Sobol, J.B.; Wunsch, H. Triage of high-risk surgical patients for intensive care. Crit. Care 2011, 15, 217. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, S.D.; Knuuti, J.; Saraste, A.; Anker, S.; Bøtker, H.E.; Hert, S.D.; Ford, I.; Gonzalez-Juanatey, J.R.; Gorenek, B.; Heyndrickx, G.R.; et al. Authors/Task Force Members. 2014 ESC/ESA Guidelines on non-cardiac surgery: Cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: Cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur. Heart J. 2014, 35, 2383–2431. [Google Scholar] [CrossRef]
- Wijeysundera, D.N.; Pearse, R.M.; Shulman, M.A.; Abbott, T.E.F.; Torres, E.; Ambosta, A.; Croal, B.L.; Granton, J.T.; Thorpe, K.E.; Grocott, M.P.W.; et al. METS study investigators. Assessment of functional capacity before major non-cardiac surgery: An international, prospective cohort study. Lancet 2018, 391, 2631–2640. [Google Scholar] [CrossRef]
- Gawande, A.A.; Kwaan, M.R.; Regenbogen, S.E.; Lipsitz, S.A.; Zinner, M.J. An Apgar score for surgery. J. Am. Coll. Surg. 2007, 204, 201–208. [Google Scholar] [CrossRef]
- Redai, I.; Emond, J.; Brentjens, T. Anesthetic considerations during liver surgery. Surg. Clin. N. Am. 2004, 84, 401–411. [Google Scholar] [CrossRef]
- Page, A.J.; Kooby, D.A. Perioperative management of hepatic resection. J. Gastrointest. Oncol. 2012, 3, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Genda, T.; Ichida, T.; Sakisaka, S.; Tanaka, E.; Mochida, S.; Ueno, Y.; Inui, A.; Egawa, H.; Umeshita, K.; Furukawa, H.; et al. Assessment Committee of Indication for Transplantation. Survival in patients with Child-Pugh class C cirrhosis: Analysis of the liver transplant registry in Japan. Hepatol. Res. 2017, 47, 1155–1164. [Google Scholar] [CrossRef]
- Torzilli, G.; Donadon, M.; Palmisano, A.; Del Fabbro, D.; Spinelli, A.; Makuuchi, M.; Montorsi, M. Back-flow bleeding control during resection of right-sided liver tumors by means of ultrasound-guided finger compression of the right hepatic vein at its caval confluence. Hepatogastroenterology 2007, 54, 1364–1367. [Google Scholar] [PubMed]
- Safirstein, R.; Andrade, L.; Vieira, J.M. Acetylcysteine and nephrotoxic effects of radiographic contrast agent—A new use for an old drug. N. Eng. J. Med. 2000, 343, 210–212. [Google Scholar] [CrossRef]
- Ho, K.M.; Morgan, D.J. Meta-analysis of N-acetylcysteine to prevent acute renal failure after major surgery. Am. J. Kidney Dis. 2009, 53, 33–40. [Google Scholar] [CrossRef]
- Pasupathy, S.; Tavella, R.; Grover, S.; Raman, B.; Procter, N.E.K.; Du, T.Y.; Mahadavan, G.; Stafford, I.; Heresztyn, T.; Holmes, A.; et al. Early Use of N-acetylcysteine With Nitrate Therapy in Patients Undergoing Primary Percutaneous Coronary Intervention for ST-Segment-Elevation Myocardial Infarction Reduces Myocardial Infarct Size (The NACIAM Trial [N-acetylcysteine in Acute Myocardial Infarction]). Circulation 2017, 136, 894–903. [Google Scholar]
- Weisbord, S.D.; Gallagher, M.; Jneid, H.; Garcia, S.; Cass, A.; Thwin, S.S.; Conner, T.A.; Chertow, G.M.; Bhatt, D.L.; Shunk, K.; et al. PRESERVE Trial Group. Outcomes After Angiography With Sodium Bicarbonate and Acetylcysteine. N. Eng. J. Med. 2018, 378, 603–614. [Google Scholar] [CrossRef]
- Lentschener, C.; Ozier, Y. Anaesthesia for elective liver resection: Some points should be revisited. Eur. J. Anaesthesiol. 2002, 19, 780–788. [Google Scholar] [CrossRef]
- Hofer, C.K.; Cannesson, M. Monitoring Fluid Responsiveness. Acta. Anesthesiol. Taiwanica 2011, 49, 59–65. [Google Scholar] [CrossRef]
- Magder, S. Volume and its relationship to Cardiac Output and Venous Return. Crit. Care 2016, 20, 271. [Google Scholar] [CrossRef] [PubMed]
- Levy, B. Lactate and shock state: The methabolic view. Curr. Opin. Crit. Care 2006, 12, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Kraut, J.A.; Madias, N.E. Lactic acidosis. N. Eng. J. Med. 2014, 371, 2309–2319. [Google Scholar] [CrossRef] [PubMed]
- Chioléro, R.; Tappy, L.; Gillet, M.; Revelly, J.P.; Roth, H.; Cayeux, C.; Schneiter, P.; Leverve, X. Effect of major hepatectomy on glucose and lactate metabolism. Ann. Surg. 1999, 229, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Husain, F.A.; Martin, M.J.; Mullenix, P.S.; Steele, S.R.; Elliott, D.C. Serum lactate and base deficit as predictors of mortality and morbidity. Am. J. Surg. 2003, 185, 485–491. [Google Scholar] [CrossRef]
- Khosravani, H.; Shahpori, R.; Stelfox, H.T.; Kirkpatrick, A.W.; Laupland, K.B. Occurrence and adverse effect on outcome of hyper- lactatemia in the critically ill. Crit. Care. 2009, 13, R90. [Google Scholar] [CrossRef]
- Macquillan, G.C.; Seyam, M.S.; Nightingale, P.; Neuberger, J.M.; Murphy, N. Blood lactate but not serum phosphate levels can predict patient outcome in fulminant hepatic failure. Liver Transpl. 2005, 11, 1073–1079. [Google Scholar] [CrossRef]
- Bernardin, G.; Pradier, C.; Tiger, F.; Deloffre, P.; Mattei, M. Blood pressure and arterial lactate level are early indicators of short- term survival in human septic shock. Intensive Care Med. 1996, 22, 17–25. [Google Scholar] [CrossRef]
- Manikis, P.; Jankowski, S.; Zhang, H.; Kahn, R.J.; Vincent, J.L. Correlation of serial blood lactate levels to organ failure and mortality after trauma. Am. J. Emerg. Med. 1995, 13, 619–622. [Google Scholar] [CrossRef]
- Shapiro, N.I.; Howell, M.D.; Talmor, D.; Nathanson, L.A.; Lisbon, A.; Wolfe, R.E.; Weiss, J.W. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann. Emerg. Med. 2005, 45, 524–528. [Google Scholar] [CrossRef]
- Trzeciak, S.; Dellinger, R.P.; Chansky, M.E.; Arnold, R.C.; Schorr, C.; Milcarek, B.; Hollenberg, S.M.; Parrillo, J.E. Serum lactate as a predictor of mortality in patients with infection. Intensive Care Med. 2007, 33, 970–977. [Google Scholar] [CrossRef]
- Jones, A.C.; Shapiro, N.I.; Trzeciak, S.; Arnold, R.C.; Claremont, H.A.; Kline, J.A.; for the Emergency Medicine Shock Research Network (EMShockNet) Investigators. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: A randomized clinical trial. JAMA 2010, 303, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Ghneim, M.H.; Regner, J.L.; Jupiter, D.C.; Kang, F.; Bonner, G.L.; Bready, M.S.; Frazee, R.; Ciceri, D.; Davis, M.L. Goal directed fluid resuscitation decreases time for lactate clearance and facilitates early fascial closure in damage control surgery. Am. J. Surg. 2013, 206, 995–999. [Google Scholar] [CrossRef] [PubMed]
- Giustiniano, E.; Procopio, F.; Ruggieri, N.; Grimaldi, S.; Torzilli, G.; Raimondi, F. Impact of the FloTrac/VigileoTM monitoring on intraoperative fluid management and outcome after Liver resection. Dig. Surg. 2018, 35, 435–441. [Google Scholar] [CrossRef]
- Benes, J.; Chytra, I.; Altmann, P.; Hluchy, M.; Kasal, E.; Svitak, R.; Pradl, R.; Stepan, M. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: Results of prospective randomized study. Crit. Care 2010, 14, R118. [Google Scholar] [CrossRef]
- Gorcott, M.P.W.; Mythen, M.G.; Gan, T.J. Perioperative fluid management and clinical outcome in adult. Anesth. Analg. 2005, 100, 1093–1106. [Google Scholar] [CrossRef]
- NHS-Technology Adoption Centre (NTAC). Intraoperative Fluid Management Technologies (IOFMT). 2012. Available online: www.ntac.nhs.uk/ (accessed on 9 February 2021).
- Pearse, R.M.; Harrison, D.A.; MacDonald, N.; Gillies, M.A.; Blunt, M.; Ackland, G.; Grocott, M.P.; Ahern, A.; Griggs, K.; Scott, R.; et al. OPTIMISE Study Group. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery: A randomized clinical trial and systematic review. JAMA 2014, 311, 2181–2190. [Google Scholar] [CrossRef]
- Brandstrup, B.; Tønnesen, H.; Beier-Holgersen, R.; Hjortsø, E.; Ørding, H.; Lindorff-Larsen, K.; Rasmussen, M.S.; Lanng, C.; Wallin, L.; Iversen, L.H.; et al. Danish Study Group on Perioperative Fluid Therapy. Effects of intravenous fluid restriction on postoperative complications: Comparison of two perioperative fluid regimens: A randomized assessor-blinded multicenter trial. Ann. Surg. 2003, 238, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Pinsky, M.R.; Peyen, D. Functional Hemody-namic Monitoring. In Update in Intensive Care Medicine; Vincent, J.L., Ed.; Springer Verlag: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Giustiniano, E.; Procopio, F.; Morenghi, E.; Rocchi, L.; Fabbro, D.D.; Ruggieri, N.; Zito, P.C.; Donadon, M.; Torzilli, G.; Raimondi, F. Does Inferior-Vena-Cava Collapsibility Correlate with Fluid Regimen and Outcome in Patients Undergoing Liver Resection? J. Anesth. Clin. Res. 2015, 6, 577. [Google Scholar] [CrossRef]
- Wilks, J.A.; Hancher-Hodges, S.; Gottumukkala, V.N.R. Contemporary Perioperative Anesthetic Management of Hepatic Resection. Adv. Anesth. 2016, 34, 85–103. [Google Scholar] [CrossRef]
- Vitin, A.A.; Azamfirei, L.; Tomescu, D.; Lang, J.D. Perioperative Management of Lactic Acidosis in End-Stage Liver Disease Patient. J. Crit. Care Med. 2017, 3, 55–62. [Google Scholar] [CrossRef]
- Kraut, J.A.; Madias, N.E. Treatment of acute metabolic acidosis: A pathophysiologic approach. Nat. Rev. Nephrol. 2012, 8, 589–601. [Google Scholar] [CrossRef] [PubMed]
- Giustiniano, E.; Procopio, F.; Costa, G.; Rocchi, L.; Ruggieri, N.; Cantoni, S.; Zito, P.C.; Gollo, Y.; Torzilli, G.; Raimondi, F. Serum lactate in liver resection with intermittent Pringle maneuver: The “square-root” shape. J. Hepatobiliary Pancreat. Sci. 2017, 24, 627–636. [Google Scholar] [CrossRef] [PubMed]
- Vibert, E.; Boleslawski, E.; Cosse, C.; Adam, R.; Castaing, D.; Cherqui, D.; Naili, S.; Regimbeau, J.M.; Sa Cunha, A.; Truant, S.; et al. Arterial Lactate Concentration at the End of an Elective Hepatectomy Is an Early Predictor of the Postoperative Course and a Potential Surrogate of Intraoperative Events. Ann. Surg. 2015, 262, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Wiggans, M.G.; Starkie, T.; Shahtahmassebi, G.; Woolley, T.; Birt, D.; Erasmus, P.; Anderson, I.; Bowles, M.J.; Aroor, S.; Stell, D.A. Serum arterial lactate concentration predicts mortality and organ dysfunction following liver resection. Perioper. Med. 2013, 2, 21. [Google Scholar] [CrossRef]
- Kim, H.J.; Son, Y.K.; An, W.S. Effect of Sodium Bicarbonate Administration on Mortality in Patients with Lactic Acidosis: A Retrospective Analysis. PLoS ONE 2013, 8, e65283. [Google Scholar] [CrossRef]
- Müller, M.M.; Van Remoortel, H.; Meybohm, P.; Aranko, K.; Aubron, C.; Burger, R.; Carson, J.L.; Cichutek, K.; De Buck, E.; Devine, D.; et al. ICC PBM Frankfurt 2018 Group. Patient Blood Management: Recommendations from the 2018 Frankfurt Consensus Conference. JAMA 2019, 321, 983–997. [Google Scholar] [CrossRef]
- Hallet, J.; Jayaraman, S.; Martel, G.; Ouellet, J.B.; Lin, Y.; McCluskey, S.; Beyfuss, K.A.; Karanicolas, P.J. Canadian Hepato-Pancreatico-Biliary Association group. Patient blood management for liver resection: Consensus statements using Delphi methodology. HPB (Oxford) 2019, 21, 393–404. [Google Scholar] [CrossRef]
- Biancofiore, G.; Blasi, A.; De Boer, M.T.; Franchini, M.; Hartmann, M.; Lisman, T.; Liumbruno, G.M.; Porte, R.J.; Saner, F.; Senzolo, M.; et al. Perioperative hemostatic management in the cirrhotic patient: A position paper on behalf of the Liver Intensive Care Group of Europe (LICAGE). Minerva Anestesiol. 2019, 85, 782–798. [Google Scholar] [CrossRef]
- Makuuchi, M.; Takayama, T.; Gunven, P.; Kosuge, T.; Yamazaky, S.; Hasegawa, H. Restrictive versus liberal blood transfusion policy for hepatectomies in cirrhotic patients. World J. Surg. 1989, 13, 644–648. [Google Scholar] [CrossRef]
- Yamamoto, J.; Kosuge, T.; Takayama, T.; Shimada, K.; Yaamasaky, S.; Ozaki, H.; Yamaguchi, N.; Mizuno, s.; Makuuchi, M. Perioperatve blood transfusion promotes recurrence of patocellular carcinoma after hepatectomy. Surgery 1994, 115, 303–309. [Google Scholar] [PubMed]
- Martin, R.C.; Jamagin, W.R.; Fong, Y.; Biernacki, P.; Blumgart, L.H.; DeMatteo, R.P. The use of fresh frozen plasma after major hepatic resection for colorectal metastasis: Is there a standard for transfusion? J. Am. Coll. Surg. 2003, 196, 402–409. [Google Scholar] [CrossRef]
- Shiba, H.; Ishida, Y.; Haruki, K.; Furukawa, K.; Fujiwara, Y.; Iwase, R.; Ohkuma, M.; Ogawa, M.; Misawa, T.; Yanaga, K. Negative impact of fresh frozen plasma transfusion on prognosis after hepatic resection for liver metastases from colorectal cancer. Anticancer Res. 2013, 33, 2723–2728. [Google Scholar] [PubMed]
- Cannon, R.M.; Brown, R.E.; St Hill, C.R.; Dunki-Jacobs, E.; Martin, R.C.; McMasters, K.M.; Scoggins, C.R. Negative effects of transfused blood components after hepatectomy for metastatic colorectal cancer. Am. Surg. 2013, 79, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.W.; Zhang, W.Y.; Zhang, W.H.; Yang, L.; Deng, X.Q.; Ou, M.C.; Yang, Y.X.; Liu, H.B.; Zhu, T. Survival analysis of intraoperative blood salvage for patients with malignancy disease: A PRISMA-compliant systematic review and meta-analysis. Medicine 2019, 98, e16040. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Stanworth, S.; Hopewell, S.; Doree, C.; Murphy, M. Is fresh-frozen plasma clinically effective? An update of a systematic review of randomized controlled trials. Transfusion 2012, 52, 1673–1686. [Google Scholar] [CrossRef]
- Kaibori, M.; Saito, T.; Matsui, K.; Yamaoka, M.; Kamiyama, Y. Impact of fresh frozen plasma on hepatectomy for hepatocellular carcinoma. Anticancer Res. 2008, 28, 1749–1756. [Google Scholar]
- Bednarsch, J.; Czigany, Z.; Lurje, I.; Trautwein, C.; Lüdde, T.; Strnad, P.; Gaisa, N.T.; Barabasch, A.; Bruners, P.; Ulmer, T.; et al. Intraoperative Transfusion of Fresh Frozen Plasma Predicts Morbidity Following Partial Liver Resection for Hepatocellular Carcinoma. J. Gastrointest. Surg. 2020. [Google Scholar] [CrossRef]
- Tomimaru, Y.; Wada, H.; Marubashi, S.; Kobayashi, S.; Eguchi, H.; Takeda, Y.; Tanemura, M.; Noda, T.; Umeshita, K.; Doki, Y.; et al. Fresh frozen plasma transfusion does not affect outcomes following hepatic resection for hepatocellular carcinoma. World J. Gastroenterol. 2010, 16, 5603–5610. [Google Scholar] [CrossRef]
- Yamazaki, S.; Takayama, T.; Kimura, Y.; Moriguchi, M.; Higaki, T.; Nakayama, H.; Fujii, M.; Makuuchi, M. Transfusion criteria for fresh frozen plasma in liver resections: A 3+3 cohort expansion study. Arch. Surg. 2011, 146, 1293–1929. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zaw, A.S.; Bangalore Kantharajanna, S.; Kumar, N. Is Autologous Salvaged Blood a Viable Option for Patient Blood Management in Oncologic Surgery? Transfus. Med. Rev. 2017, 31, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Bolliger, D.; Seeberger, M.D.; Tanaka, K.A. Principles and practice of thromboelastography in clinical coagulation management and transfusion practice. Transfus. Med. Rev. 2012, 26, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Rigg, J.R.; Jamrozik, K.; Myles, P.S.; Silbert, B.S.; Peyton, P.J.; Parsons, R.W.; Collins, K.S. MASTER Anaethesia Trial Study Group. Epidural anaesthesia and analgesia and outcome of major surgery: A randomised trial. Lancet 2002, 359, 1276–1282. [Google Scholar] [CrossRef]
- Halpern, S.H.; Leighton, B.L.; Ohlsson, A.; Barrett, J.F.; Rice, A. Effect of epidural vs parenteral opioid analgesia on the progress of labor: A meta-analysis. JAMA 1998, 280, 2105–2110. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.D. Acute Postoperative Pain. In Miller’s Anesthesia, 6th ed.; Miller, R.D., Ed.; Elsevier: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Matot, I.; Scheinin, O.; Eid, A.; Jurim, O. Epidural anesthesia and analgesia in liver resection. Anesth. Analg. 2002, 95, 1179–1181. [Google Scholar] [CrossRef]
- Jacquenod, P.; Wallon, G.; Gazon, M.; Darnis, B.; Pradat, P.; Virlogeux, V.; Farges, O.; Aubrun, F. Incidence and Risk Factors of Coagulation Profile Derangement After Liver Surgery: Implications for the Use of Epidural Analgesia-A Retrospective Cohort Study. Anesth. Analg. 2018, 126, 1142–1147. [Google Scholar] [CrossRef] [PubMed]
- Tzimas, P.; Prout, J.; Papadopoulos, G.; Mallett, S.V. Epidural anaesthesia and analgesia for liver resection. Anaesthesia 2013, 68, 628–635. [Google Scholar] [CrossRef]
- Elterman, K.G.; Xiong, Z. Coagulation profile changes and safety of epidural analgesia after hepatectomy: A retrospective study. J. Anesth. 2015, 29, 367–372. [Google Scholar] [CrossRef]
- Tripodi, A.; Mannucci, P.M. The coagulopathy of chronic liver disease. N. Eng. J. Med. 2011, 365, 147–156. [Google Scholar] [CrossRef]
- Tripodi, A. Hemostasis abnormalities in cirrhosis. Curr. Opin. Hematol. 2015, 22, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Stravitz, R.T. Potential applications of thromboelastography in patients with acute and chronic liver disease. Gastroenterol. Hepatol. (N. Y.) 2012, 8, 513–520. [Google Scholar]
- Mallett, S.V.; Sugavanam, A.; Krzanicki, D.A.; Patel, S.; Broomhead, R.H.; Davidson, B.R.; Riddell, A.; Gatt, A.; Chowdary, P. Alterations in coagulation following major liver resection. Anaesthesia 2016, 71, 657–668. [Google Scholar] [CrossRef] [PubMed]
- Nimmo, S.M. Benefit and outcome after epidural analgesia. Contin. Educ. Anaesth. Crit. Care Pain 2004, 4, 44–47. [Google Scholar] [CrossRef]
- Gu, C.Y.; Zhang, J.; Qian, Y.N.; Tang, Q.F. Effects of epidural anesthesia and postoperative epidural analgesia on immune function in esophageal carcinoma patients undergoing thoracic surgery. Mol. Clin. Oncol. 2015, 3, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Kambakamba, P.; Slankamenac, K.; Tschuor, C.; Kron, P.; Wirsching, A.; Maurer, K.; Petrowsky, H.; Clavien, P.A.; Lesurtel, M. Epidural analgesia and perioperative kidney function after major liver resection. Br. J. Surg. 2015, 102, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Siniscalchi, A.; Gamberini, L.; Bardi, T.; Laici, C.; Gamberini, E.; Francorsi, L.; Faenza, S. Role of epidural anesthesia in a fast track liver resection protocol for cirrhotic patients-results after three years of practice. World J. Hepatol. 2016, 8, 1097–1104. [Google Scholar] [CrossRef]
- Tomozawa, A.; Ishikawa, S.; Shiota, N.; Cholvisudhi, P.; Makita, K. Perioperative risk factors for acute kidney injury after liver resection surgery: An historical cohort study. Can. J. Anaesth. 2015, 62, 753–761. [Google Scholar] [CrossRef]
- Aloia, T.A.; Kim, B.J.; Segraves-Chun, Y.S.; Cata, J.P.; Truty, M.J.; Shi, Q.; Holmes, A.; Soliz, J.M.; Popat, K.U.; Rahlfs, T.F.; et al. A Randomized Controlled Trial of Postoperative Thoracic Epidural Analgesia Versus Intravenous Patient-controlled Analgesia After Major Hepatopancreatobiliary Surgery. Ann. Surg. 2017, 266, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Revie, E.J.; McKeown, D.W.; Wilson, J.A.; Garden, O.J.; Wigmore, S.J. Randomized clinical trial of local infiltration plus patient-controlled opiate analgesia vs. epidural analgesia following liver resection surgery. HPB (Oxford) 2012, 14, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Pourrahmat, M.M.; Vasilyeva, E.; Kim, P.T.; Osborn, J.; Wiseman, S.M. Efficacy and Safety of Patient-controlled Analgesia Compared With Epidural Analgesia After Open Hepatic Resection: A Systematic Review and Meta-analysis. Ann. Surg. 2019, 270, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Basu, S.; Tamijmarane, A.; Bulters, D.; Wells, J.K.; John, T.G.; Rees, M. An alternative method of wound pain control following hepatic resection: A preliminary study. HPB (Oxford) 2004, 6, 186–189. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hughes, M.J.; Harrison, E.M.; Peel, N.J.; Stutchfield, B.; McNally, S.; Beattie, C.; Wigmore, S.J. Randomized clinical trial of perioperative nerve block and continuous local anaesthetic infiltration via wound catheter versus epidural analgesia in open liver resection (LIVER 2 trial). BJS 2015. [Google Scholar] [CrossRef]
- Zhang, J.; Liu, T.; Zhou, H.; Fei, Y.; Yu, X. The Safety and Efficacy of Ultrasound-Guided Bilateral Dual Transversus Abdominis Plane (BD-TAP) Block in ERAS Program of Laparoscopic Hepatectomy: A Prospective, Randomized, Controlled, Blinded, Clinical Study. Drug Des. Devel. Ther. 2020, 14, 2889–2898. [Google Scholar] [CrossRef]
- Yassen, K.; Lotfy, M.; Miligi, A.; Sallam, A.; Hegazi, E.A.R.; Afifi, M. Patient-controlled analgesia with and without transverse abdominis plane and rectus sheath space block in cirrhotic patients undergoing liver resection. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, 58–64. [Google Scholar] [PubMed]
- Poon, R.T.; Fan, S.T.; Lo, C.M.; Liu, C.L.; Lam, C.M.; Yuen, W.K.; Yeung, C.; Wong, J. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: Analysis of 1222 consecutive patients from a prospective database. Ann. Surg. 2004, 240, 698–708. [Google Scholar] [CrossRef]
- Khatri, V.P.; Petrelli, N.J.; Belghiti, J. Extending the frontiers of surgical therapy for hepatic colorectal metastases: Is there a limit? J. Clin. Oncol. 2005, 23, 8490–8499. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The clavien-dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- de Santibañes, E.; Ardiles, V.; Alvarez, F.A.; Busnelli, V.C.; de Santibañes, M. Increasing resectability in colorectal liver metastases. In Extreme Hepatic Surgery and Other Strategies, 1st ed.; Springer: Basel, Switzerland, 2017; pp. 1–383. [Google Scholar] [CrossRef]
- Lo, C.-M.; Fan, S.-T.; Liu, C.-L.; Lai, E.C.S.; Wong, J. Biliary Complications after Hepatic Resection. Arch. Surg. 1998, 133. [Google Scholar] [CrossRef]
- Yamashita, Y.; Hamatsu, T.; Rikimaru, T.; Tanaka, S.; Shirabe, K.; Shimada, M.; Sugimachi, K. Bile leakage after hepatic resection. Ann. Surg. 2001, 233, 45–50. [Google Scholar] [CrossRef]
- Kyoden, Y.; Imamura, H.; Sano, K.; Beck, Y.; Sugawara, Y.; Kokudo, N.; Makuuchi, M. Value of prophylactic abdominal drainage in 1269 consecutive cases of elective liver resection. J. Hepatobiliary Pancreat Sci. 2010, 17, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, S.; Takayama, T.; Moriguchi, M.; Mitsuka, Y.; Okada, S.; Midorikawa, Y.; Nakayama, H.; Higaki, T. Criteria for drain removal following liver resection. Br. J. Surg. 2012, 99, 1584–1590. [Google Scholar] [CrossRef]
- Spetzler, V.N.; Schepers, M.; Pinnschmidt, H.O.; Fischer, L.; Nashan, B.; Li, J. The incidence and severity of post-hepatectomy bile leaks is affected by surgical indications, preoperative chemotherapy, and surgical procedures. HepatoBiliary Surg. Nutr. 2019, 8, 101–110. [Google Scholar] [CrossRef]
- Guillaud, A.; Pery, C.; Campillo, B.; Lourdais, A.; Laurent, S.; Boudjema, K. Incidence and predictive factors of clinically relevant bile leakage in the modern era of liver resections. HPB (Oxford) 2013, 15, 224–229. [Google Scholar] [CrossRef]
- Karoui, M.; Penna, C.; Amin-Hashem, M.; Mitry, E.; Benoist, S.; Franc, B.; Rougier, P.; Nordlinger, B. Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann. Surg. 2006, 243, 1–7. [Google Scholar] [CrossRef]
- Capussotti, L. Bile Leakage and Liver Resection. Arch. Surg. 2006, 141, 690. [Google Scholar] [CrossRef] [PubMed]
- Donadon, M.; Costa, G.; Cimino, M.; Procopio, F.; Del Fabbro, D.; Palmisano, A.; Torzilli, G. Diagnosis and Management of Bile Leaks After Hepatectomy: Results of a Prospective Analysis of 475 Hepatectomies. World J. Surg. 2016, 40, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Garden, O.J.; Padbury, R.; Brooke-Smith, M.; Crawford, M.; Adam, R.; Koch, M.; Makuuchi, M.; Dematteo, R.P.; Christophi, C.; et al. Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011, 149, 713–724. [Google Scholar] [CrossRef] [PubMed]
- Hammond, J.S.; Guha, I.N.; Beckingham, I.J.; Lobo, D.N. Prediction, prevention and management of postresection liver failure. Br. J. Surg. 2011, 98, 1188–1200. [Google Scholar] [CrossRef]
- Sahajpal, A.; Vollmer CMJr Dixon, E.; Chan, E.K.; Wei, A.; Cattral, M.S.; Taylor, B.R.; Grant, D.R.; Greig, P.D.; Gallinger, S. Chemotherapy for colorectal cancer prior to liver resection for colorectal cancer hepatic metastases does not adversely affect peri-operative outcomes. J. Surg. Oncol. 2007, 95, 22–27. [Google Scholar] [CrossRef]
- Procopio, F.; Cimino, M.; Viganò, L.; Colombo, A.E.; Franchi, E.; Costa, G.; Donadon, M.; Del Fabbro, D.; Torzilli, G. Prediction of remnant liver volume using 3D simulation software in patients undergoing R1vasc parenchyma-sparing hepatectomy for multiple bilobar colorectal liver metastases: Reliability, clinical impact, and learning curve. HPB (Oxford) 2020, 19, S1365–182X(20)31231–4. [Google Scholar] [CrossRef]
- Rahbari, N.N.; Garden, O.J.; Padbury, R.; Maddern, G.; Koch, M.; Hugh, T.J.; Fan, S.T.; Nimura, Y.; Figueras, J.; Vauthey, J.N.; et al. Post-hepatectomy haemorrhage: A definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford) 2011, 13, 528–535. [Google Scholar] [CrossRef]
- Bellver Oliver, M.; Escrig-Sos, J.; Rotellar Sastre, F.; Moya-Herráiz, Á.; Sabater-Ortí, L. Outcome quality standards for surgery of colorectal liver metastasis. Langenbecks Arch. Surg. 2020, 405, 745–756. [Google Scholar] [CrossRef]
- Tsujita, E.; Yamashita, Y.; Takeishi, K.; Matsuyama, A.; Tsutsui, S.; Matsuda, H.; Taketomi, A.; Shirabe, K.; Ishida, T.; Maehara, Y. Subcuticular absorbable suture with subcutaneous drainage system prevents incisional SSI after hepatectomy for hepatocellular carcinoma. World J. Surg. 2012, 36, 1651–1656. [Google Scholar] [CrossRef]
- Jin, S.; Fu, Q.; Wuyun, G.; Wuyun, T. Management of post-hepatectomy complications. World J. Gastroenterol. 2013, 19, 7983–7991. [Google Scholar] [CrossRef] [PubMed]
- Nobili, C.; Marzano, E.; Oussoultzoglou, E.; Rosso, E.; Addeo, P.; Bachellier, P.; Jaeck, D.; Pessaux, P. Multivariate analysis of risk factors for pulmonary complications after hepatic resection. Ann. Surg. 2012, 255, 540–550. [Google Scholar] [CrossRef]
- Del Fabbro, D.; Alloisio, M.; Procopio, F.; Cimino, M.; Donadon, M.; Palmisano, A.; Vigano, L.; Torzilli, G. Surgical treatment of synchronous colorectal liver and lung metastases: The usefulness of thoracophrenolaparotomy for single stage resection. Hepatobiliary Pancreat. Dis. Int. 2016, 15, 216–219. [Google Scholar] [CrossRef]
- Donadon, M.; Costa, G.; Gatti, A.; Torzilli, G. Thoracoabdominal approach in liver surgery: How, when, and why. Updates Surg. 2014, 66, 121–125. [Google Scholar] [CrossRef] [PubMed]
- O’Gara, B.; Talmor, D. Perioperative lung protective ventilation. BMJ 2018, 362, k3030. [Google Scholar] [CrossRef]
- Wiseman, J.T.; Guzman-Pruneda, F.; Xourafas, D.; Chun, Y.S.; Ejaz, A.; Tsung, A.; Pawlik, T.M.; Cloyd, J.M. Impact of Neoadjuvant Chemotherapy on the Postoperative Outcomes of Patients Undergoing Liver Resection for Colorectal Liver Metastases: A Population-Based Propensity-Matched Analysis. J. Am. Coll. Surg. 2019, 229, 69–77. [Google Scholar] [CrossRef]
- Zhao, J.; van Mierlo, K.M.C.; Gómez-Ramírez, J.; Kim, H.; Pilgrim, C.H.C.; Pessaux, P.; Rensen, S.S.; van der Stok, E.P.; Schaap, F.G.; Soubrane, O.; et al. Chemotherapy-Associated Liver Injury (CALI) consortium. Systematic review of the influence of chemotherapy-associated liver injury on outcome after partial hepatectomy for colorectal liver metastases. Br. J. Surg. 2017, 104, 990–1002. [Google Scholar] [CrossRef]
- Thasler, W.E.; Bein, T.; Jauch, K.W. Perioperative effects of hepatic resection surgery on hemodynamics, pulmonary fluid balance, and indocyanine green clearance. Langenbecks Arch. Surg. 2002, 387, 271–275. [Google Scholar] [CrossRef]
- Melendez, J.; Ferri, E.; Zwillman, M.; Fischer, M.; DeMatteo, R.; Leung, D.; Jarnagin, W.; Fong, Y.; Blumgart, L.H. Extended hepatic resection: A 6-year retrospective study of risk factors for perioperative mortality. J. Am. Coll. Surg. 2001, 192, 47–53. [Google Scholar] [CrossRef]
- Salem, R.R.; Tray, K. Hepatic resection-related hypophosphatemia is of renal origin as manifested by isolated hyperphosphaturia. Ann. Surg. 2005, 241, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Datta, H.K.; Malik, M.; Neely, R.D. Hepatic surgery-related hypophosphatemia. Clin. Chim. Acta. 2007, 380, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Wrighton, L.J.; O’Bosky, K.R.; Namm, J.P.; Senthil, M. Postoperative management after hepatic resection. J. Gastrointest. Oncol. 2012, 3, 41–47. [Google Scholar] [CrossRef]

| Parameter | Numerical Score | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Ascites | None | Slight | Moderate to severe |
| Encephalopathy | None | Slight to moderate | Moderate to severe |
| Bilirubin (mg/dL) | <2.0 | 2–3 | >3.0 |
| Albumin (g/dL) | >3.5 | 2.8–3.5 | <2.8 |
| Prothrombin time (s) | 1–3 | 4–6 | >6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giustiniano, E.; Nisi, F.; Rocchi, L.; Zito, P.C.; Ruggieri, N.; Cimino, M.M.; Torzilli, G.; Cecconi, M. Perioperative Management of Complex Hepatectomy for Colorectal Liver Metastases: The Alliance between the Surgeon and the Anesthetist. Cancers 2021, 13, 2203. https://doi.org/10.3390/cancers13092203
Giustiniano E, Nisi F, Rocchi L, Zito PC, Ruggieri N, Cimino MM, Torzilli G, Cecconi M. Perioperative Management of Complex Hepatectomy for Colorectal Liver Metastases: The Alliance between the Surgeon and the Anesthetist. Cancers. 2021; 13(9):2203. https://doi.org/10.3390/cancers13092203
Chicago/Turabian StyleGiustiniano, Enrico, Fulvio Nisi, Laura Rocchi, Paola C. Zito, Nadia Ruggieri, Matteo M. Cimino, Guido Torzilli, and Maurizio Cecconi. 2021. "Perioperative Management of Complex Hepatectomy for Colorectal Liver Metastases: The Alliance between the Surgeon and the Anesthetist" Cancers 13, no. 9: 2203. https://doi.org/10.3390/cancers13092203
APA StyleGiustiniano, E., Nisi, F., Rocchi, L., Zito, P. C., Ruggieri, N., Cimino, M. M., Torzilli, G., & Cecconi, M. (2021). Perioperative Management of Complex Hepatectomy for Colorectal Liver Metastases: The Alliance between the Surgeon and the Anesthetist. Cancers, 13(9), 2203. https://doi.org/10.3390/cancers13092203









