Clinical Benefits of Conversion Surgery for Unresectable Pancreatic Ductal Adenocarcinoma: A Single-Institution, Retrospective Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Ethics Statements
2.2. Study Design and Patient Population
2.3. Therapy Method
2.4. Conversion Surgery
2.5. Adjuvant Chemotherapy
2.6. Assessment
2.7. Statistical Analysis
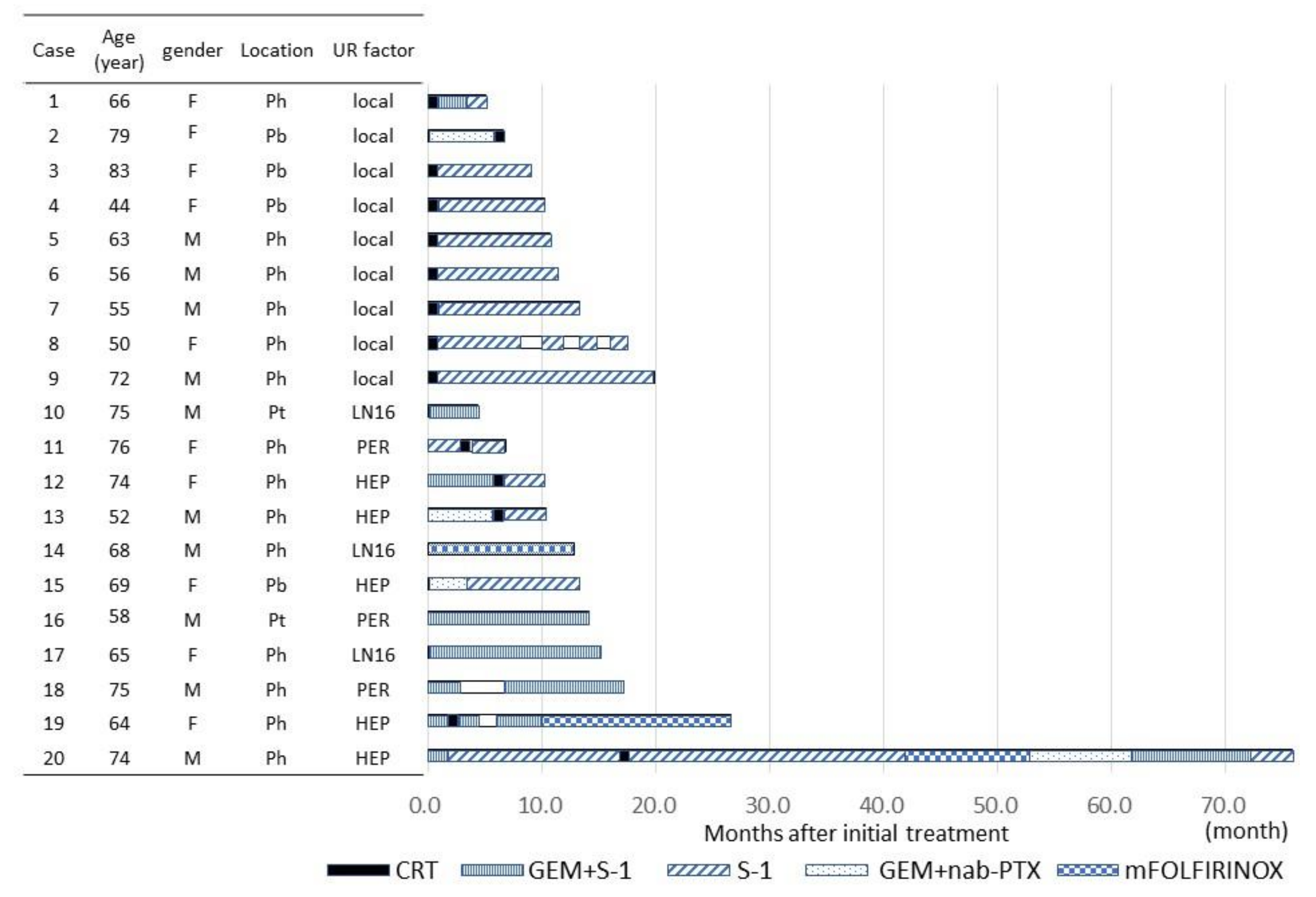
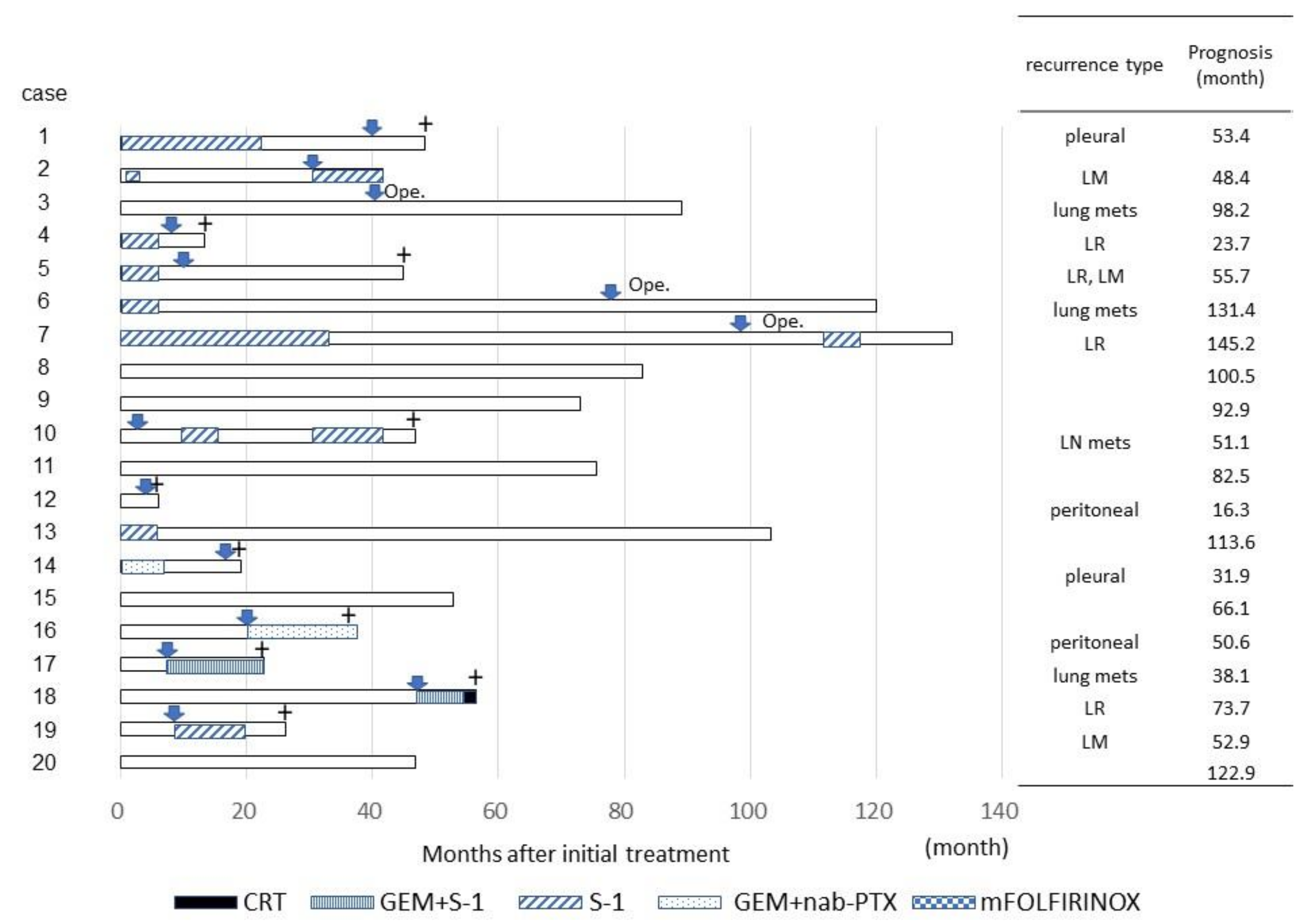
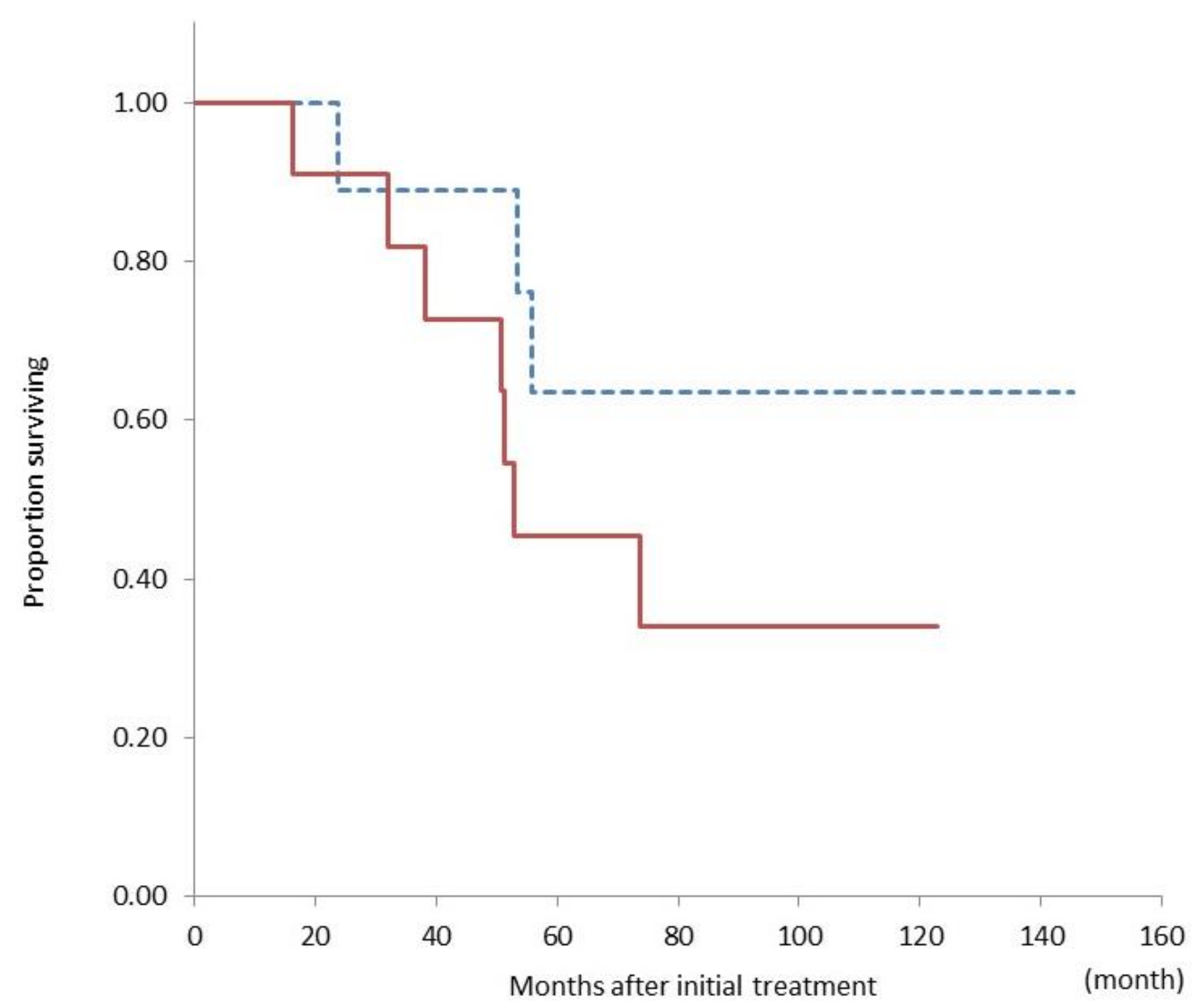
3. Results
3.1. Patient Characteristics
3.2. Adjuvant Chemotherapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- In Cancer Statistics in Japan-2019, Foundation for Promotion of Cancer Research (FPCR). Available online: https://www.fpcr.or.jp/data_files/view/41/mode:inline (accessed on 1 December 2020).
- Jonathan, D.M.; Rishi, S.; Juan, W.V.; Rachna, T.S. Pancreatic cancer. Lancet 2020, 395, 2008–2020. [Google Scholar]
- Vincent, A.; Herman, J.; Schulick, R.; Hruban, R.H.; Goggins, M. Pancreatic cancer. Lancet 2011, 378, 607–620. [Google Scholar] [CrossRef]
- NCCN. Clinical Practice Guidelines in Oncology (NCCN Guidelines): NCCN, Pancreatic Adenocarcinoma, Version 1. 2020. Available online: https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf (accessed on 17 January 2021).
- Japan Pancreas Society. General Rules for the Study of Pancreatic Cancer, 7th ed.; Kanehara Shuppan: Tokyo, Japan, 2016. [Google Scholar]
- Imamura, M.; Doi, R.; Imaizumi, T.; Funakoshi, A.; Wakasugi, H.; Sunamura, M.; Ogata, Y.; Hishinuma, S.; Asano, T.; Aikou, T.; et al. A randomized multicenter trial comparing resection and radiochemotherapy for resectable locally invasive pancreatic cancer. Surgery 2004, 136, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Hackert, T.; Sachsenmaier, M.; Hinz, U.; Schneider, L.; Michalski, C.W.; Springfeld, C.; Strobel, O.; Jäger, D.; Ulrich, A.; Büchler, M.W. Locally advanced pancreatic cancer: Neoadjuvant therapy with FOLFIRINOX results in resectability in 60% of the patients. Ann. Surg. 2016, 264, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Sui, K.; Okabayashi, T.; Shima, Y.; Morita, S.; Iwata, J.; Sumiyoshi, T.; Saisaka, Y.; Yasuhiro, H.; Yoshihiro, N.; Matsumoto, M.; et al. Clinical effects of chemoradiotherapy in pursuit of optimal treatment of locally advanced unresectable pancreatic cancer. Br. J. Radiol. 2017, 90, 20170165. [Google Scholar] [CrossRef]
- Saito, T.; Ishido, K.; Kudo, D.; Kimura, N.; Wakiya, T.; Nakayama, Y.; Hakamada, K. Combination therapy with gemcitabine and nab-paclitaxel for locally advanced unresectable pancreatic cancer. Mol. Clin. Oncol. 2017, 6, 963–967. [Google Scholar] [CrossRef]
- Uesaka, K.; Boku, N.; Fukutomi, A.; Okamura, Y.; Konishi, M.; Matsumoto, I.; Kaneoka, Y.; Shimizu, Y.; Nakamori, S.; Sakamoto, H.; et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: A phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 2016, 16, 248–257. [Google Scholar] [CrossRef]
- Ferrone, C.R.; Marchegiani, G.; Hong, T.S.; Ryan, D.P.; Deshpande, V.; McDonnell, E.I.; Sabbatino, F.; Santos, D.D.; Allen, J.N.; Blaszkowsky, L.S.; et al. Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann. Surg. 2015, 261, 12–17. [Google Scholar] [CrossRef]
- Klaiber, U.; Hackert, T. Conversion surgery for pancreatic cancer—The impact of neoadjuvant treatment. Front Oncol. 2020, 14, 1501. [Google Scholar] [CrossRef]
- Satoi, S.; Yamaue, H.; Kato, K.; Takahashi, S.; Hirono, S.; Takeda, S.; Eguchi, H.; Sho, M.; Wada, K.; Shinchi, H.; et al. Role of adjuvant surgery for patients with initially unresectable pancreatic cancer with a long-term favorable response to non-surgical anti-cancer treatments: Results of a project study for pancreatic surgery by the Japanese society of hepato-biliary-pan. J. HepatoBiliary-Pancreat. Sci. 2013, 20, 590–600. [Google Scholar] [CrossRef]
- Gillen, S.; Schuster, T.; Büschenfelde, C.M.Z.; Friess, H.; Kleeff, J. Preoperative/neoadjuvant therapy in pancreatic cancer: A systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010, 7, e1000267. [Google Scholar] [CrossRef]
- Yoshitomi, H.; Takano, S.; Furukawa, K.; Takayashiki, T.; Kuboki, S.; Ohtsuka, M. Conversion surgery for initially unresectable pancreatic cancer: Current status and unsolved issues. Surg. Today 2019, 49, 894–906. [Google Scholar] [CrossRef] [PubMed]
- Natsume, S.; Shimizu, Y.; Senda, Y.; Hijioka, S.; Matsuo, K.; Ito, S.; Komori, K.; Abe, T.; Hara, K. Conversion surgery only for highly selected patients with unresectable pancreatic cancer: A satisfactory outcome in exchange for a lower resection rate. Surg. Today 2019, 49, 670–677. [Google Scholar] [CrossRef] [PubMed]
- Furuse, J.; Shibahara, J.; Sugiyama, M. Development of chemotherapy and significance of conversion surgery after chemotherapy in unresectable pancreatic cancer. J. Hepato Biliary Pancreat. Sci. 2018, 25, 261–268. [Google Scholar] [CrossRef]
- Yanagimoto, H.; Satoi, S.; Yamamoto, T.; Yamaki, S.; Hirooka, S.; Kotsuka, M.; Ryota, H.; Ishida, M.; Matsui, Y.; Sekimoto, M. Benefits of conversion surgery after multimodal treatment for unresectable pancreatic ductal adenocarcinoma. Cancers (Basel) 2020, 12, 1428. [Google Scholar] [CrossRef]
- Asano, T.; Hirano, S.; Nakamura, T.; Okamura, K.; Tsuchikawa, T.; Noji, T.; Nakanishi, Y.; Tanaka, K.; Shichinohe, T. Survival benefit of conversion surgery for patients with initially unresectable pancreatic cancer who responded favorably to nonsurgical treatment. J. Hepato-Biliary-Pancreat. Sci. 2018, 25, 342–350. [Google Scholar] [CrossRef]
- Kimura, Y.; Nakamura, T.; Hayashi, T.; Kuwatani, M.; Motoya, M.; Yoshida, M.; Imamura, M.; Nagayama, M.; Yamaguchi, H.; Yamakita, K.; et al. Clinical usefulness of conversion surgery for unresectable pancreatic cancer diagnosed on multidetector computed tomography imaging: Results from a multicenter observational cohort study by the Hokkaido Pancreatic Cancer Study Group (HOPS UR-01). Ann. Gastroenterol. Surg. 2019, 3, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, N.; Matsuyama, R.; Murakami, T.; Yabushita, Y.; Sawada, Y.; Kumamoto, T.; Endo, I. Role of conversion surgery for unresectable pancreatic cancer after long-term chemotherapy. World J. Surg. 2020, 44, 2752–2760. [Google Scholar] [CrossRef] [PubMed]
- Klaiber, U.; Schnaidt, E.S.; Hinz, U.; Gaida, M.M.; Heger, U.; Hank, U.; Strobel, O.; Neoptolemos, J.P.; Mihaljevic, A.L.; Büchler, M.W.; et al. Prognostic factors of survival after neoadjuvant treatment and resection for initially unresectable pancreatic cancer. Ann. Surg. 2021, 273, 154–162. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.B.; Rich, T.A.; Byrd, D.R.; Cleary, K.R.; Connelly, J.H.; Levin, B.; Charnsangavej, C.; Fenoglio, C.J.; Ames, F.C. Preoperative chemoradiation and pancreaticoduodenectomy for adenocarcinoma of the pancreas. Arch. Surg. 1992, 127, 1335–1339. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.-C.; Gromski, M.A.; Kim, H.W.; Kim, J.; Kim, J.; Hwang, J.-H. Clinical outcomes of FOLFIRINOX in locally advanced pancreatic cancer: A single center experience. Medicine (Baltimore) 2018, 97, e13592. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Kondo, S.; Hirano, S.; Tanaka, E.; Shichinohe, T.; Tsuchikawa, T.; Matsumoto, J. Adjuvant surgical therapy for patients with initially-unresectable pancreatic cancer with long-term favorable responses to chemotherapy. J. Hepato-Biliary-Pancreat. Sci. 2011, 18, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Wright, G.P.; Poruk, K.E.; Zenati, M.; Steve, J.; Bahary, N.; Hogg, M.E.; Zuriekat, A.H.; Wolfgang, C.L.; Zeh, H.J.; Weiss, M. Primary tumor resection following favorable response to systemic chemotherapy in stage IV pancreatic adenocarcinoma with synchronous metastases: A Bi-institutional analysis. J. Gastrointest. Surg. 2016, 20, 1830–1835. [Google Scholar] [CrossRef]
- Nitsche, U.; Wenzel, P.; Siveke, J.T.; Braren, R.; Holzapfel, K.; Schlitter, A.M.; Stöß, C.; Kong, B.; Esposito, I.; Erkan, M.; et al. Resectability after first-line FOLFIRINOX in initially unresectable locally advanced pancreatic cancer: A single-center experience. Ann. Surg. Oncol. 2015, 22, 1212–1220. [Google Scholar] [CrossRef] [PubMed]
- Opendro, S.S.; Satoi, S.; Yanagimoto, H.; Yamamoto, T.; Toyokawa, H.; Hirooka, S.; Yamaki, S.; Inoue, K.; Matsui, Y.; Kwon, A.-H. Role of adjuvant surgery in initially unresectable pancreatic cancer after long-term chemotherapy or chemoradiation therapy: Survival benefit? J. Hepato-Biliary-Pancreat. Sci. 2014, 21, 695–702. [Google Scholar] [CrossRef]
- Chad, A.B.; Ashley, N.K.; Mohammed, A.; Callisia, N.C.; Kathleen, K.C.; Abdul, H.K.; Bryan, C.H.; Paul, S.R.; Ben, G.; William, A.H.; et al. Is adjuvant therapy necessary for all patients with localized pancreatic cancer who have received neoadjuvant therapy? J. Gastrointest. Surg. 2017, 21, 1793–1803. [Google Scholar]
- Yoo, C.; Shin, S.H.; Kim, K.P.; Jeong, J.H.; Chang, H.M.; Kang, J.H.; Lee, S.S.; Park, D.H.; Song, T.J.; Seo, D.W.; et al. Clinical outcomes of conversion surgery after neoadjuvant chemotherapy in patients with borderline resectable and locally advanced unresectable pancreatic cancer: A single-center, retrospective analysis. Cancers 2019, 11, 278. [Google Scholar] [CrossRef] [PubMed]
- Michelakos, T.; Pergolini, I.; Castillo, C.F.-D.; Honselmann, K.C.; Cai, L.; Deshpande, V.; Wo, J.Y.; Ryan, D.P.; Allen, J.N.; Blaszkowsky, L.S.; et al. Predictors of resectability and survival in patients with borderline and locally advanced pancreatic cancer who underwent neoadjuvant treatment with FOLFIRINOX. Ann. Surg. 2019, 269, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Satoi, S.; Yamamoto, T.; Yamaki, S.; Sakaguchi, T.; Sekimoto, M. Surgical indication for and desirable outcomes of conversion surgery in patients with initially unresectable pancreatic ductal adenocarcinoma. Ann. Gastroenterol. Surg. 2019, 4, 6–13. [Google Scholar] [CrossRef]
- Yamada, S.; Kobayashi, A.; Nakamori, S.; Baba, H.; Yamamoto, M.; Yamaue, H.; Fujii, T. Resection for recurrent pancreatic cancer in the remnant pancreas after pancreatectomy is clinically promising: Results of a project study for pancreatic surgery by the Japanese society of hepato-biliary-pancreatic surgery. Surgery 2018, 164, 1049–1056. [Google Scholar] [CrossRef]
- Kurahara, H.; Maemura, K.; Mataki, Y.; Tanoue, K.; Iino, S.; Kawasaki, Y.; Idichi, T.; Arigami, T.; Mori, S.; Shinden, Y.; et al. Lung recurrence and its therapeutic strategy in patients with pancreatic cancer. Pancreatology 2020, 20, 89–94. [Google Scholar] [CrossRef] [PubMed]
- White, R.R.; Xie, H.B.; Gottfried, M.R.; Czito, B.G.; Hurwitz, H.I.; Morse, M.A.; Blobe, G.C.; Paulson, E.K.; Baillie, J.; Branch, M.S.; et al. Significance of histological response to preoperative chemoradiotherapy for pancreatic cancer. Ann. Surg. Oncol. 2005, 12, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Heckler, M.; Mihaljevic, A.; Sun, H.; Klaiber, U.; Heger, U.; Büchler, M.W.; Hackert, T. CT response of primary tumor and CA19-9 predict resectability of metastasized pancreatic cancer after FOLFIRINOX. Eur. J. Surg. Oncol. 2019, 45, 1453–1459. [Google Scholar] [CrossRef]
- Moutardier, V.; Magnin, V.; Turrini, O.; Viret, F.; Hennekinne-Mucci, S.; Gonçalves, A.; Pésenti, C.; Guiramand, J.; Lelong, B.; Giovannini, M.; et al. Assessment of pathologic response after preoperative chemoradiotherapy and surgery in pancreatic adenocarcinoma. Int. J. Radiat. Oncol. 2004, 60, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, D.; Katz, M.H.; Rashid, A.; Varadhachary, G.R.; Wolff, R.A.; Wang, H.; Lee, J.E.; Pisters, P.W.T.; Vauthey, J.-N.; Crane, C.; et al. Histologic grading of the extent of residual carcinoma following neoadjuvant chemoradiation in pancreatic ductal adenocarcinoma: A predictor for patient outcome. Cancer 2012, 118, 3182–3190. [Google Scholar] [CrossRef] [PubMed]
- Shinchi, H.; Maemura, K.; Mataki, Y.; Kurahara, H.; Sakoda, M.; Ueno, S.; Hiraki, Y.; Nakajo, M.; Natsugoe, S.; Takao, S. A phase II study of oral S-1 with concurrent radiotherapy followed by chemotherapy with S-1 alone for locally advanced pancreatic cancer. J. Hepato Biliary Pancreat. Sci. 2012, 19, 152–158. [Google Scholar] [CrossRef]
- Jang, J.Y.; Han, Y.; Lee, H.; Kim, S.W.; Kwon, W.; Lee, K.H.; Oh, D.Y.; Chie, E.K.; Lee, J.M.; Heo, J.S.; et al. Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: A prospective, randomized, open-label, multicenter phase 2/3 trial. Ann. Surg. 2018, 268, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Hammel, P.; Huguet, F.; van Laethem, J.L.; Goldstein, D.; Glimelius, B.; Artru, P.; Borbath, I.; Bouché, O.; Shannon, J.; André, T.; et al. Effect of chemoradiotherapy vs. chemotherapy on survival in patients with locally advanced pancreatic cancer controlled after 4 months of gemcitabine with or without erlotinib: The LAP07 randomized clinical trial. JAMA 2016, 315, 1844–1853. [Google Scholar] [CrossRef]
- Frigerio, I.; Regi, P.; Giardino, A.; Scopelliti, F.; Girelli, R.; Bassi, C.; Gobbo, S.; Martini, P.T.; Capelli, P.; D’Onofrio, M.; et al. Downstaging in stage IV pancreatic cancer: A new population eligible for surgery? Ann. Surg. Oncol. 2017, 24, 2397–2403. [Google Scholar] [CrossRef] [PubMed]

| Variables | Conversion Surgery | p-Value | |
|---|---|---|---|
| (+) (n = 20) | (−) (n = 378) | ||
| age (years), median (range) | 65 (44–83) | 69 (33–87) | 0.25 |
| gender (M/F), n | (10/10) | (207/171) | 0.656 |
| tumor location (Ph/Pb,Pt), n | (14/6) | (218/160) | 0.282 |
| unresectability status (UR-LA vs UR-M), n | (9/11) | (243/135) | 0.622 |
| CEA, median (range) (U/mL) | 3.4 (1.1–9.4) | 4.0(0.3–845) | 0.51 |
| CA19-9, median (range) (U/mL) | 2577 (0.6–1985) | 211(0.6–50,000) | 0.17 |
| tumor size, median (range) (mm) | 30 (18–50) | 35(8–116) | 0.323 |
| T(4/3), n | (16/4) | (332/46) | 0.385 |
| N(1/0), n | (7/13) | (136/252) | 0.917 |
| M(1/0), n | (11/9) | (197/181) | 0.829 |
| Case | CEA (U/mL, Before) | CEA (U/mL, After) | CA19-9 (U/mL, Before) | CA19-9 (U/mL, After) | Tumor Size (mm, Before) | Tumor Size (mm, After) | Treatment Effect (RECIST) | Operative Method | Operative Time (min) | Bleeding Volume (mL) | Hospital Stay (Day) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2.4 | 2 | 25.9 | 9.9 | 27 | 13 | PR | SSPPD | 678 | 295 | 32 |
| 2 | 2.6 | 3.3 | 55.9 | 39 | 33 | 13 | PR | DP | 403 | 160 | 22 |
| 3 | 8 | 10.3 | 2789 | 24.9 | 32 | 23 | PR | DP | 373 | 260 | 50 |
| 4 | 1.1 | 5.1 | 81.4 | 34 | 50 | 50 | SD | DP | 438 | 1150 | 9 |
| 5 | 2.9 | 3.1 | 5103 | 19.9 | 23 | 12 | PR | SSPPD + PVR | 509 | 1250 | 11 |
| 6 | 9.4 | 4.4 | 92 | 10.9 | 29 | 13 | PR | SSPPD | 575 | 1220 | 23 |
| 7 | 6.4 | 2.4 | 253.5 | 49.6 | 24 | 9 | PR | SSPPD + PVR | 738 | 3010 | 16 |
| 8 | 2 | 2.7 | 9.2 | 11.4 | 42 | 10 | PR | SSPPD | 464 | 1030 | 10 |
| 9 | 1.5 | 1.6 | 1559 | 11.2 | 41 | 9 | PR | SSPPD + PVR | 574 | 1665 | 13 |
| 10 | 2.3 | 2.2 | 67.4 | 9 | 21 | 10 | PR | DP | 408 | 1075 | 11 |
| 11 | 3.4 | 3 | 20.6 | 7.4 | 30 | 16 | PR | SSPPD + PVR | 643 | 1390 | 9 |
| 12 | 2.5 | 3.2 | 1985 | 48.2 | 24 | 12 | SD | SSPPD + HPR | 841 | 2340 | 11 |
| 13 | 3.8 | 4.2 | 270 | 38.1 | 29 | 8 | PR | SSPPD | 729 | 2470 | 16 |
| 14 | 4.6 | 8 | 1515 | 16.4 | 41 | 34 | PR | SSPPD + PVR | 919 | 3600 | 47 |
| 15 | 5.1 | 3 | 1846 | 13.3 | 35 | 0 | CR | DP | 391 | 240 | 23 |
| 16 | 3.4 | 3.4 | 5.2 | 10.4 | 21 | 19 | SD | DP | 352 | 90 | 8 |
| 17 | 8 | 8.4 | 0.6 | 0.6 | 18 | 13 | SD | SSPPD | 623 | 1040 | 13 |
| 18 | 3 | 4.6 | 1047 | 10.7 | 32 | 11 | PR | SSPPD | 550 | 1020 | 8 |
| 19 | 1.8 | 2.1 | 516 | 17.8 | 30 | 9 | PD | TP + PVR + HPR | 613 | 460 | 14 |
| 20 | 2.9 | 9.5 | 330 | 99 | 24 | 25 | SD | SSPPD + PVR | 641 | 1695 | 13 |
| Case | Stage (Before) | Stage (After) | p-Stage | Pathological | Evans |
|---|---|---|---|---|---|
| 1 | 3 | 3 | 2a | tub2 | IIb |
| 2 | 3 | 2a | 2a | tub1 | I |
| 3 | 3 | 3 | 2b | tub2 | III |
| 4 | 3 | 2b | 2a | muc | IIb |
| 5 | 3 | 2a | 2a | tub1 | IIb |
| 6 | 3 | 1a | 1 | por | III |
| 7 | 3 | 3 | 2b | tub1 | III |
| 8 | 3 | 3 | 2a | similar to NEN | IIb |
| 9 | 3 | 3 | 1 | tub2 | IIb |
| 10 | 4 | 3 | 0 | no neoplasm | IV |
| 11 | 4 | 2a | 2a | tub1 | III |
| 12 | 4 | 2a | 2a | tub2 | I |
| 13 | 4 | 2b | 1 | a few | III |
| 14 | 4 | 4 | 2a | tub2 | IIb |
| 15 | 4 | 0 | 0 | no neoplasm | IV |
| 16 | 4 | 2a | 2b | tub1 | I |
| 17 | 4 | 2a | 1 | tub1 | III |
| 18 | 4 | 3 | 2b | tub2 | III |
| 19 | 4 | 4 | 4 | tub2 | IIb |
| 20 | 4 | 3 | 2a | tub2 | I |
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95%CI | p-Value | HR | 95%CI | p-Value | |
| Age (per year) | 0.67 | - | 0.54 | - | - | - |
| Sex (male vs. female) | 0.75 | 0.19–2.39 | 0.65 | - | - | - |
| Location (Ph vs. Pb,Pt) | 1.47 | 0.22–2.61 | 0.59 | - | - | - |
| Tumor size (> 30 mm vs. <30 mm) | 0.64 | 0.37–5.80 | 0.49 | - | - | - |
| CEA (> 3 U/mL vs. <3 U/mL) | 0.32 | 0.18–2.27 | 0.32 | - | - | - |
| CA19-9 (> 100 U/mL vs. <100 U/mL) | 0.62 | 0.15–1.88 | 0.45 | - | - | - |
| UR-M vs. UR-LA | 2.38 | 0.18–2.16 | 0.21 | - | - | - |
| CRT ((+) vs.(−)) | 8.06 | 0.61–9.24 | 0.002 | 8.54 | 2.03–35.97 | 0.004 |
| Tumor size (> 30 mm vs. <30 mm) | 0.77 | 2.15–30.18 | 0.68 | - | - | - |
| CEA > 3 U/mL vs. <3 U/mL) | 1.23 | 0.22–2.69 | 0.76 | - | - | - |
| CA19-9 (> 100 U/mL vs. <100 U/mL) | 0.35 | 0.32–4.80 | 0.32 | - | - | - |
| Change of tumor size (> 0.5 v.s. <0.5) | 0.72 | 0.04–2.74 | 0.61 | - | - | - |
| Change of CEA | 1.5 | 0.20–2.55 | 0.56 | - | - | -- |
| Change of CA19-9 | 1 | 0.39–5.83 | 1 | - | - | - |
| RECIST (PD,SD vs. PR,CR) | 4.93 | 0.12–7.91 | 0.015 | 5.05 | 1.20-21.25 | 0.03 |
| Period until operation (> 12 m vs. <12 m) | 0.89 | 1.37–17.72 | 0.86 | - | - | |
| Operation time (> 600 min vs. <600 min) | 1.36 | 0.26–3.09 0.39–4.70 | 0.63 | - | - | - |
| Bleeding volume (> 1000 mL vs. <1000 mL) | 0.89 | 0.23–3.52 | 0.87 | - | - | - |
| Evans (I-IIa vs. IIb-V) | 0.57 | 0.12–2.76 | 0.49 | - | - | - |
| pT (1,2 vs.3,4) | 2.14 | 0.55–8.31 | 0.27 | - | - | - |
| LN mets ((+) vs.(−)) | 0.77 | 0.16–3.67 | 0.75 | - | - | - |
| Adjuvant chemo. ((−) vs(+)) | 2.07 | 0.53–8.10 | 0.29 | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mataki, Y.; Kurahara, H.; Idichi, T.; Tanoue, K.; Hozaka, Y.; Kawasaki, Y.; Iino, S.; Maemura, K.; Shinchi, H.; Ohtsuka, T. Clinical Benefits of Conversion Surgery for Unresectable Pancreatic Ductal Adenocarcinoma: A Single-Institution, Retrospective Analysis. Cancers 2021, 13, 1057. https://doi.org/10.3390/cancers13051057
Mataki Y, Kurahara H, Idichi T, Tanoue K, Hozaka Y, Kawasaki Y, Iino S, Maemura K, Shinchi H, Ohtsuka T. Clinical Benefits of Conversion Surgery for Unresectable Pancreatic Ductal Adenocarcinoma: A Single-Institution, Retrospective Analysis. Cancers. 2021; 13(5):1057. https://doi.org/10.3390/cancers13051057
Chicago/Turabian StyleMataki, Yuko, Hiroshi Kurahara, Tetsuya Idichi, Kiyonori Tanoue, Yuto Hozaka, Yota Kawasaki, Satoshi Iino, Kosei Maemura, Hiroyuki Shinchi, and Takao Ohtsuka. 2021. "Clinical Benefits of Conversion Surgery for Unresectable Pancreatic Ductal Adenocarcinoma: A Single-Institution, Retrospective Analysis" Cancers 13, no. 5: 1057. https://doi.org/10.3390/cancers13051057
APA StyleMataki, Y., Kurahara, H., Idichi, T., Tanoue, K., Hozaka, Y., Kawasaki, Y., Iino, S., Maemura, K., Shinchi, H., & Ohtsuka, T. (2021). Clinical Benefits of Conversion Surgery for Unresectable Pancreatic Ductal Adenocarcinoma: A Single-Institution, Retrospective Analysis. Cancers, 13(5), 1057. https://doi.org/10.3390/cancers13051057






