Potential Therapeutic and Prognostic Values of LSM Family Genes in Breast Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. UALCAN
2.2. DNA Methylation
2.3. Functional Enrichment Analysis
2.4. Survival Analysis
2.5. Analysis of Protein Expression in Clinical Specimen
2.6. TIMER Analysis
2.7. Differentially Expressed Genes (DEGs) Analysis
2.8. Statistical Analysis
3. Results
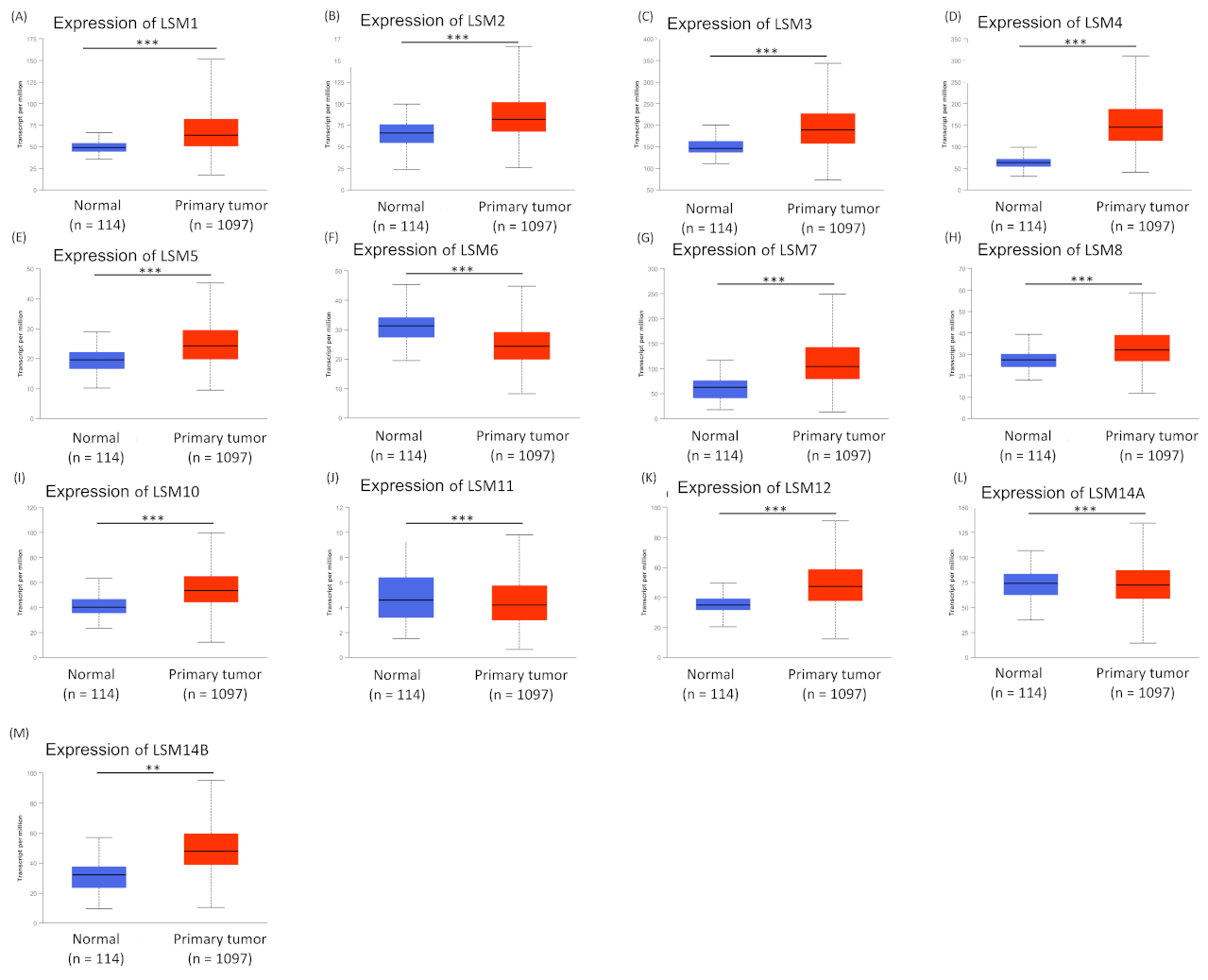
3.1. Analysis of Expression Profiles of LSM Family Members
3.2. Relationships between LSM Family Members and Stages of BRCA
3.3. Prognosis Value of DNA Methylation of LSM Family Gene
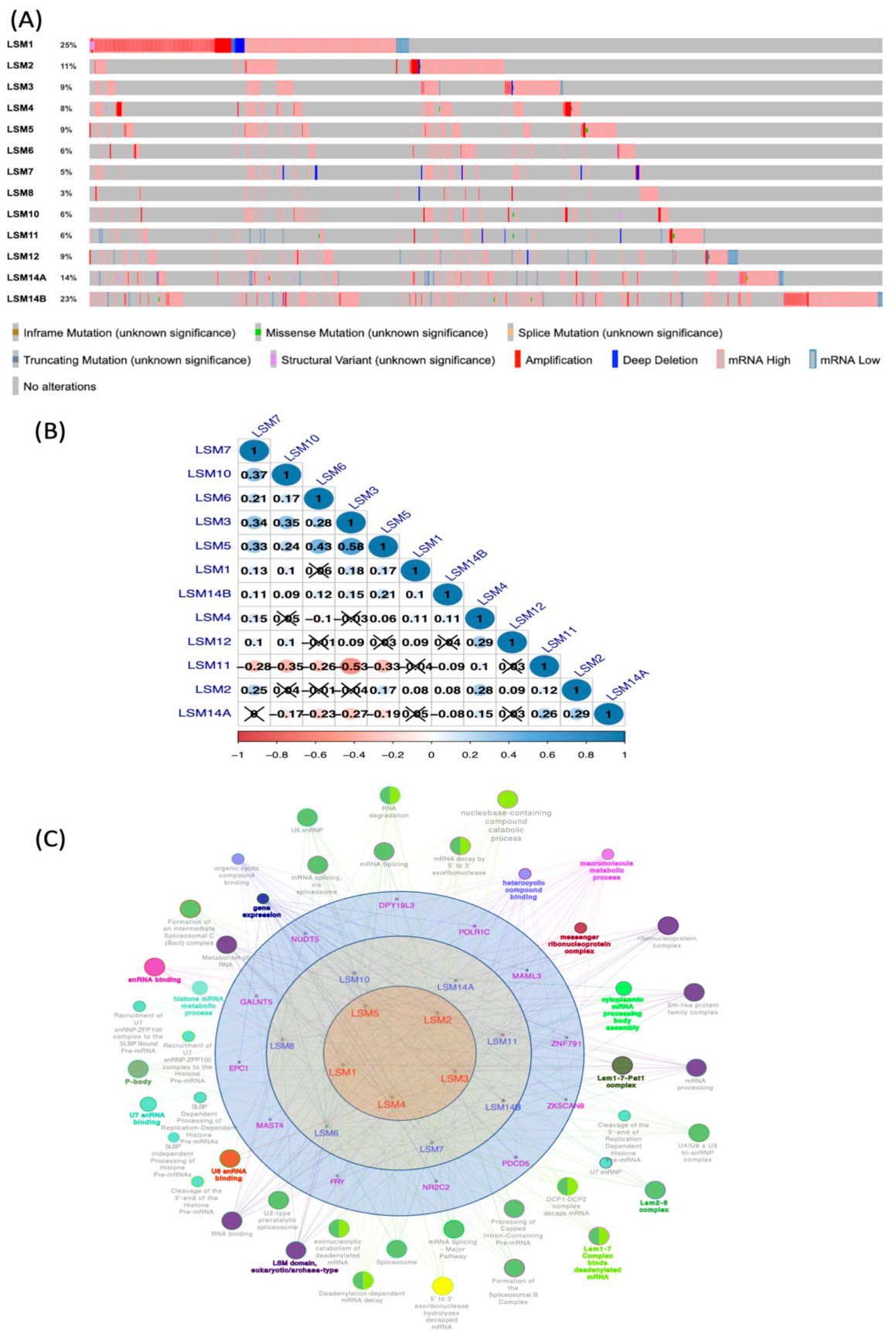
3.4. LSM Gene Mutations and Co-Expression Analysis
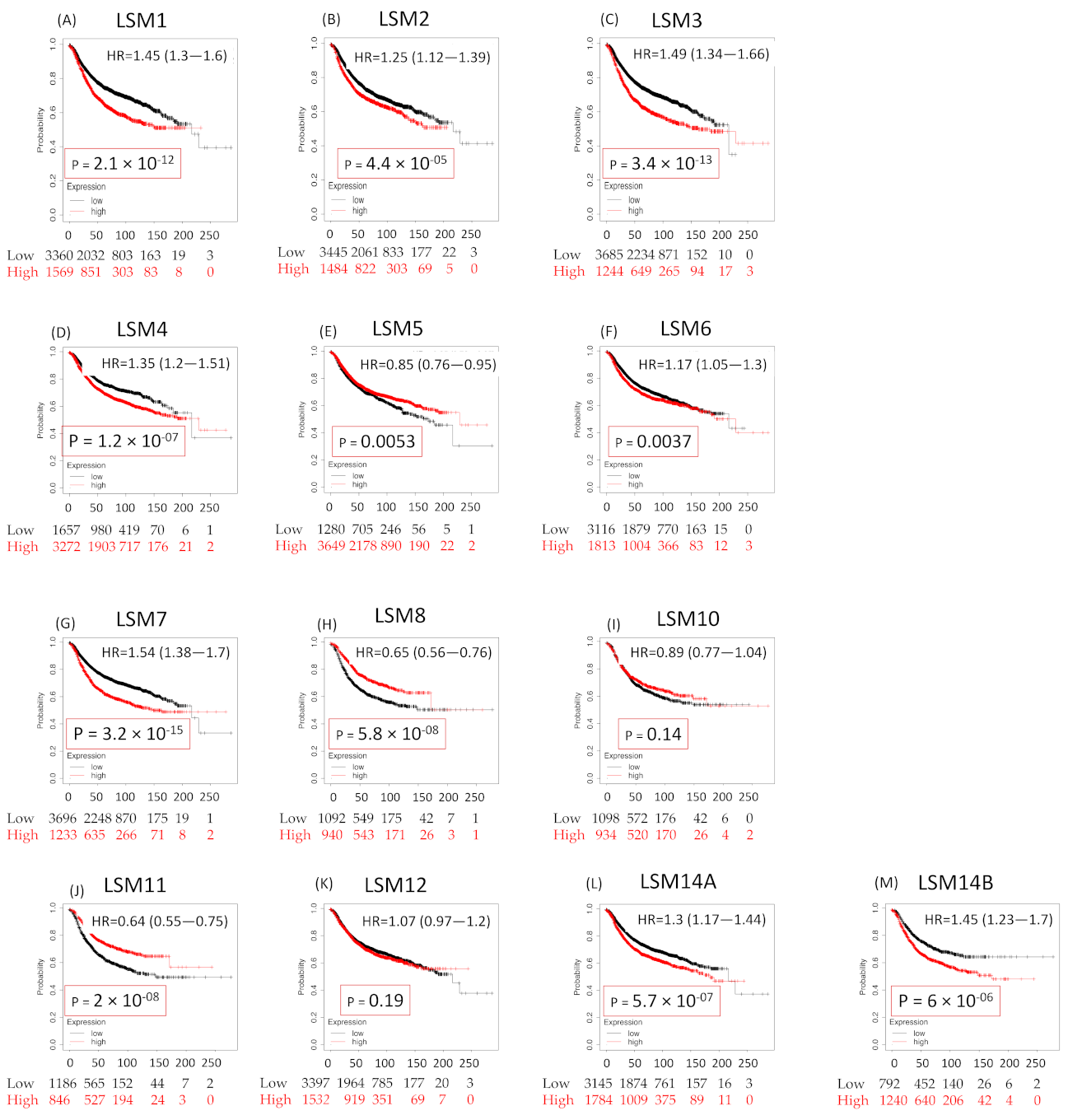
3.5. Survival Analysis of LSM Family Genes
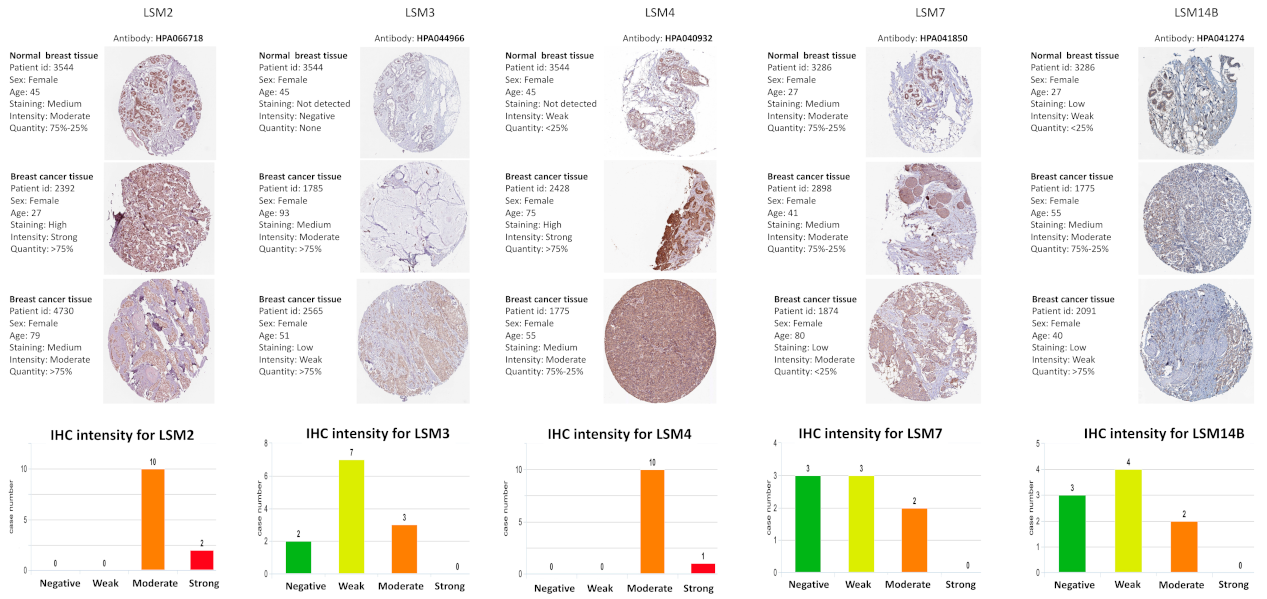
3.6. Protein Expressions of LSM Family Members
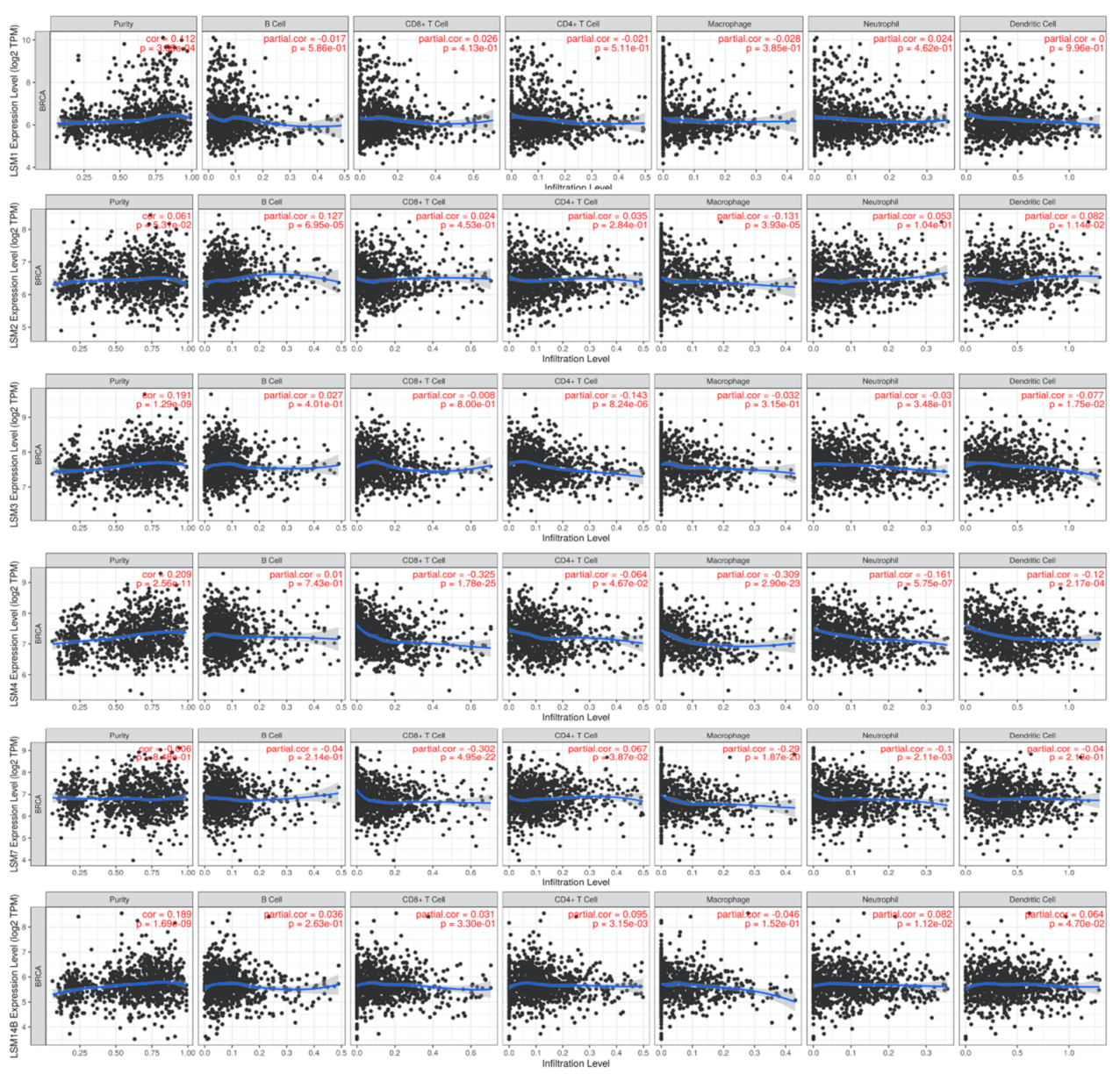
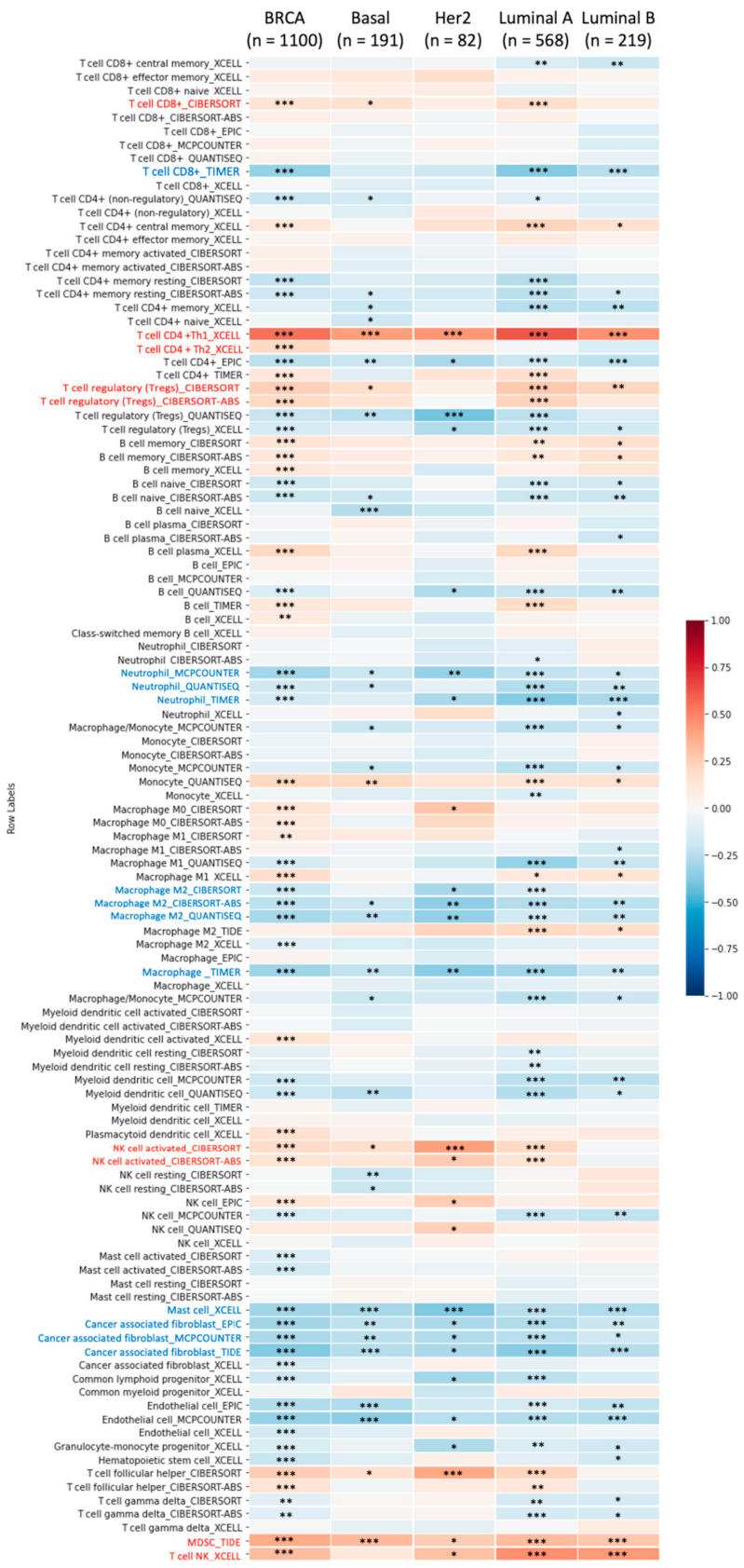
3.7. Relationship between LSMs Transcriptomic Expression Levels and Biomarkers of Different Immune Cells
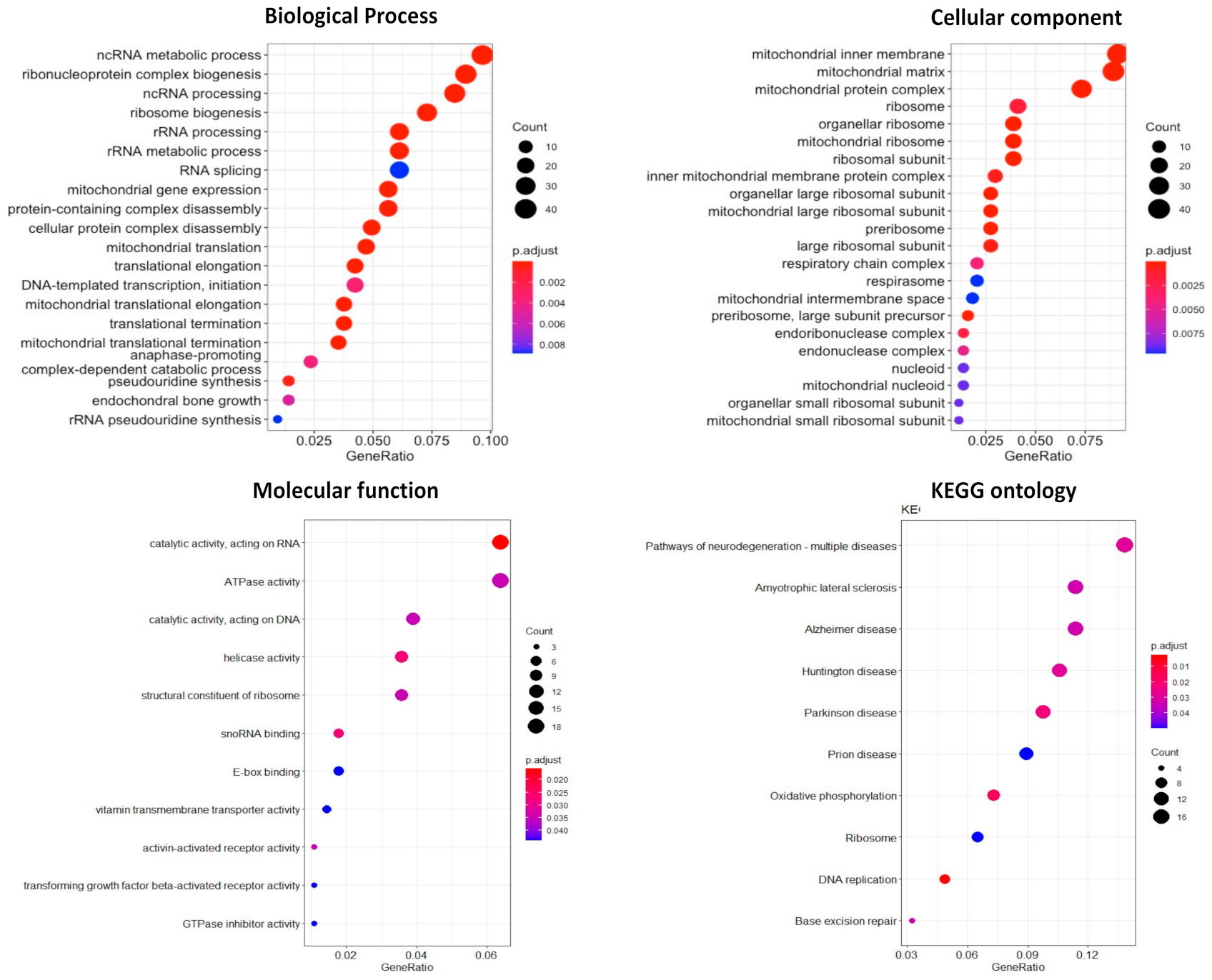
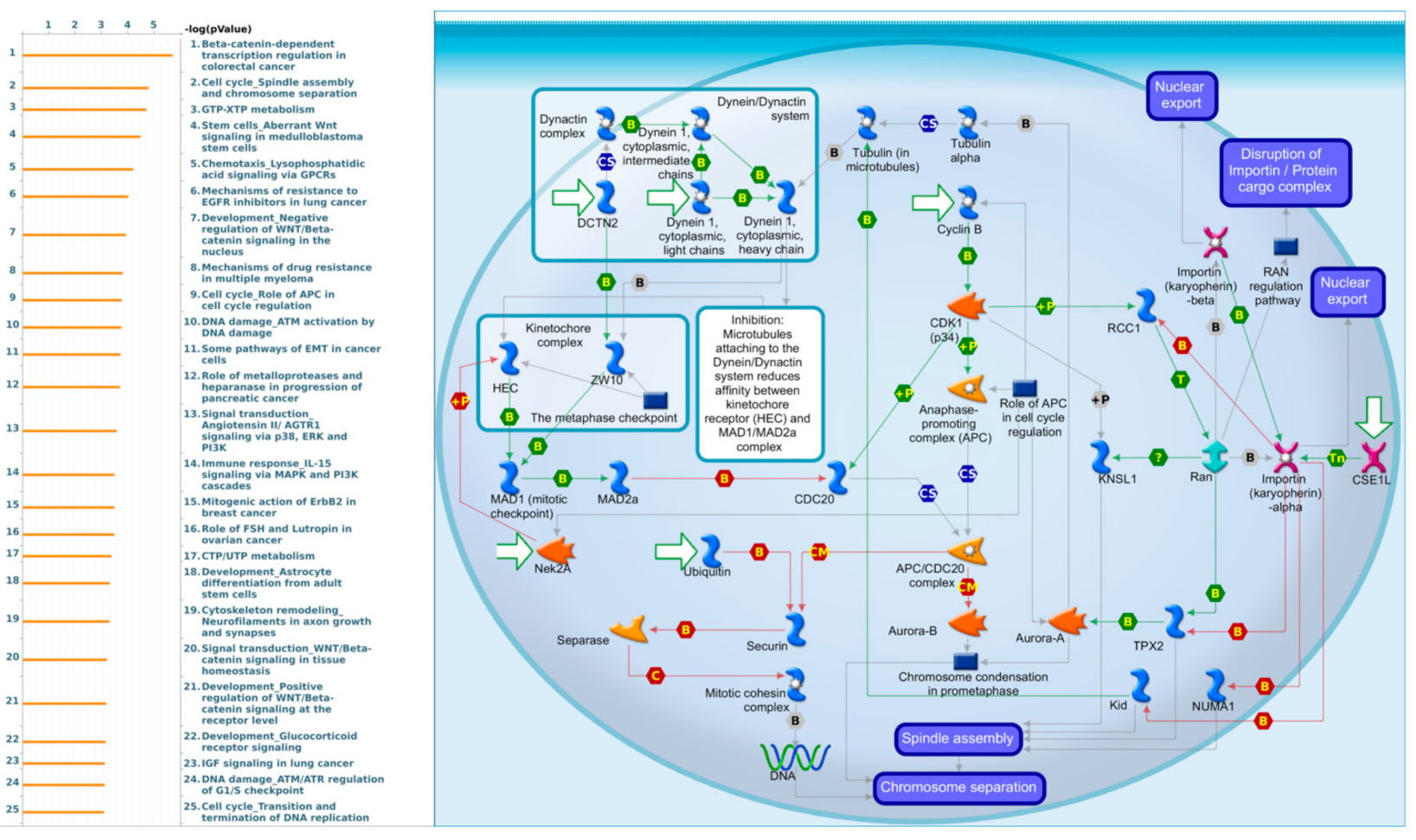
3.8. Comprehensive Results of LSM4 in Functional Enrichment Analysis
3.8.1. Gene Ontology Enrichment Analysis
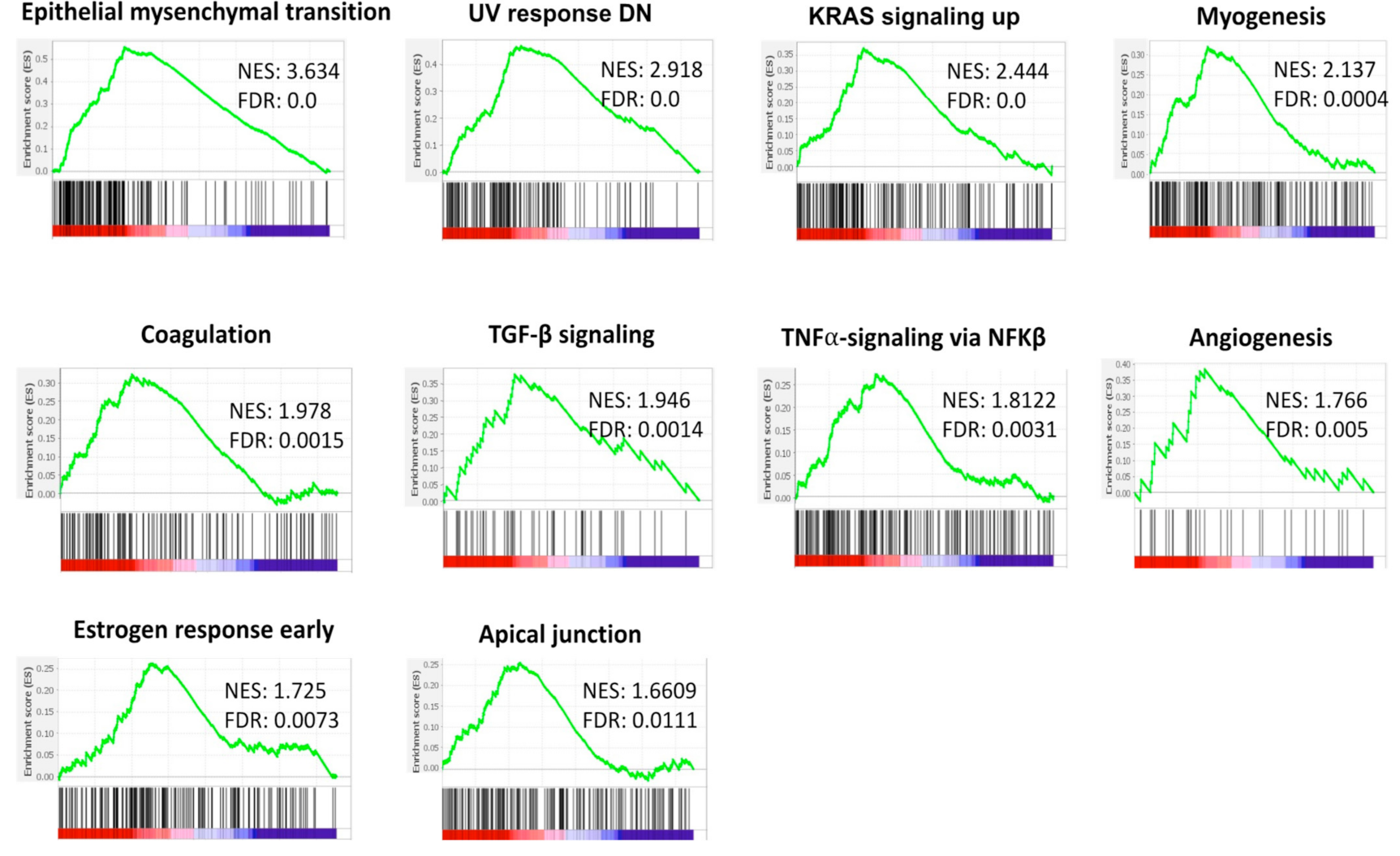
3.8.2. High Expression of LSM4 Is Related to Epithelial-Mesenchymal Transition (EMT) and Pro-Cancerous Related Gene Sets in Breast Cancer
3.8.3. Identification of Differentially Expressed Genes (DEGs) in BRCA Patients
3.8.4. LSM4 Not Only Plays Roles in BRCA Development but Is Also Involved in Various Cancer Types
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Breast Cancer; WHO: Geneva, Switzerland, 2021.
- Azubuike, S.O.; Muirhead, C.; Hayes, L.; McNally, R. Rising global burden of breast cancer: The case of sub-Saharan Africa (with emphasis on Nigeria) and implications for regional development: A review. World J. Surg. Oncol. 2018, 16, 63. [Google Scholar] [CrossRef] [PubMed]
- Ginsburg, O.; Bray, F.; Coleman, M.P.; Vanderpuye, V.; Eniu, A.; Kotha, S.R.; Sarker, M.; Huong, T.T.; Allemani, C.; Dvaladze, A.; et al. The global burden of women’s cancers: A grand challenge in global health. Lancet 2017, 389, 847–860. [Google Scholar] [CrossRef]
- Susini, T.; Saccardin, G.; Renda, I.; Giani, M.; Tartarotti, E.; Nori, J.; Vanzi, E.; Pasqualini, E.; Bianchi, S. Immunohistochemical evaluation of FGD3 expression: A new strong prognostic factor in invasive breast cancer. Cancers 2021, 13, 3824. [Google Scholar] [CrossRef] [PubMed]
- Renda, I.; Bianchi, S.; Vezzosi, V.; Nori, J.; Vanzi, E.; Tavella, K.; Susini, T. Expression of FGD3 gene as prognostic factor in young breast cancer patients. Sci. Rep. 2019, 9, 15204. [Google Scholar] [CrossRef]
- Susini, T.; Berti, B.; Carriero, C.; Tavella, K.; Nori, J.; Vanzi, E.; Molino, C.; Di Tommaso, M.; Santini, M.; Saladino, V.; et al. Topoisomerase II alpha and TLE3 as predictive markers of response to anthracycline and taxane-containing regimens for neoadjuvant chemotherapy in breast cancer. OncoTargets Ther. 2014, 7, 2111–2120. [Google Scholar] [CrossRef][Green Version]
- Thorat, M.A.; Balasubramanian, R. Breast cancer prevention in high-risk women. Best Pract. Res. Clin. Obstet. Gynaecol. 2020, 65, 18–31. [Google Scholar] [CrossRef]
- Lin, C.Y.; Lee, C.H.; Chuang, Y.H.; Lee, J.Y.; Chiu, Y.Y.; Wu Lee, Y.H.; Jong, Y.J.; Hwang, J.K.; Huang, S.H.; Chen, L.C.; et al. Membrane protein-regulated networks across human cancers. Nat. Commun. 2019, 10, 3131. [Google Scholar] [CrossRef]
- Tsai, H.T.; Huang, C.S.; Tu, C.C.; Liu, C.Y.; Huang, C.J.; Ho, Y.S.; Tu, S.H.; Tseng, L.M.; Huang, C.C. Multi-gene signature of microcalcification and risk prediction among Taiwanese breast cancer. Sci. Rep. 2020, 10, 18276. [Google Scholar] [CrossRef]
- Nguyen, H.D.; Liao, Y.C.; Ho, Y.S.; Chen, L.C.; Chang, H.W.; Cheng, T.C.; Liu, D.; Lee, W.R.; Shen, S.C.; Wu, C.H.; et al. The α9 Nicotinic acetylcholine receptor mediates nicotine-induced PD-L1 expression and regulates melanoma cell proliferation and migration. Cancers 2019, 11, 1991. [Google Scholar] [CrossRef]
- Lee, K.L.; Kuo, Y.C.; Ho, Y.S.; Huang, Y.H. Triple-negative breast cancer: Current understanding and future therapeutic breakthrough targeting cancer stemness. Cancers 2019, 11, 1334. [Google Scholar] [CrossRef]
- Nuffiedtrust. Cancer Survival Rates; Elsevier: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Villasco, A.; Accomasso, F.; D’Alonzo, M.; Agnelli, F.; Sismondi, P.; Biglia, N. Evaluation of the ability of the Clinical Treatment Score at 5 years (CTS5) compared to other risk stratification methods to predict the response to an extended endocrine therapy in breast cancer patients. Breast Cancer 2021, 28, 1131–1140. [Google Scholar] [CrossRef]
- Villasco, A.; Agnelli, F.; D’Alonzo, M.; Accomasso, F.; Sismondi, P.; Biglia, N. Validation of CTS5 on a retrospective cohort of real-life pre- and postmenopausal patients diagnosed with estrogen receptor-positive breast cancers: Is it prognostic? Clin. Breast Cancer 2021, 21, e53–e62. [Google Scholar] [CrossRef]
- Modaffari, P.; Ponzone, R.; Ferrari, A.; Cipullo, I.; Liberale, V.; D’Alonzo, M.; Maggiorotto, F.; Biglia, N. Concerns and expectations of risk-reducing surgery in women with hereditary breast and ovarian cancer syndrome. J. Clin. Med. 2019, 8, 313. [Google Scholar] [CrossRef]
- Narrandes, S.; Xu, W. Gene expression detection assay for cancer clinical use. J. Cancer 2018, 9, 2249–2265. [Google Scholar] [CrossRef]
- Schiffman, J.D.; Fisher, P.G.; Gibbs, P. Early detection of cancer: Past, present, and future. Am. Soc. Clin. Oncol. Educ. Book 2015, 57–65. [Google Scholar] [CrossRef]
- Loud, J.T.; Murphy, J. Cancer screening and early detection in the 21(st) century. Semin. Oncol. Nurs. 2017, 33, 121–128. [Google Scholar] [CrossRef]
- Thomas, L.; Leiponen, A. Big data commercialization. IEEE Eng. Manag. Rev. 2016, 44. [Google Scholar] [CrossRef]
- Wilusz, C.J.; Wilusz, J. Lsm proteins and Hfq: Life at the 3′ end. RNA Biol. 2013, 10, 592–601. [Google Scholar] [CrossRef]
- Reeves, W.H.; Narain, S.; Satoh, M. Henry Kunkel, Stephanie Smith, clinical immunology, and split genes. Lupus 2003, 12, 213–217. [Google Scholar] [CrossRef]
- Li, W.; Li, X.; Gao, L.N.; You, C.G. Integrated analysis of the functions and prognostic values of RNA binding proteins in lung squamous cell carcinoma. Front Genet. 2020, 11, 185. [Google Scholar] [CrossRef]
- Streicher, K.L.; Yang, Z.Q.; Draghici, S.; Ethier, S.P. Transforming function of the LSM1 oncogene in human breast cancers with the 8p11–12 amplicon. Oncogene 2007, 26, 2104–2114. [Google Scholar] [CrossRef] [PubMed]
- Watson, P.M.; Miller, S.W.; Fraig, M.; Cole, D.J.; Watson, D.K.; Boylan, A.M. CaSm (LSm-1) overexpression in lung cancer and mesothelioma is required for transformed phenotypes. Am. J. Respir. Cell Mol. Biol. 2008, 38, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Luhtala, N.; Parker, R. LSM1 over-expression in Saccharomyces cerevisiae depletes U6 snRNA levels. Nucleic Acids Res. 2009, 37, 5529–5536. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tao, Y.; Han, Y.; Yu, L.; Wang, Q.; Leng, S.X.; Zhang, H. The predicted key molecules, functions, and pathways that bridge Mild Cognitive Impairment (MCI) and Alzheimer’s Disease (AD). Front Neurol. 2020, 11, 233. [Google Scholar] [CrossRef]
- Brčić, L.; Barić, A.; Gračan, S.; Torlak, V.; Brekalo, M.; Škrabić, V.; Zemunik, T.; Barbalić, M.; Punda, A.; Boraska Perica, V. Genome-wide association analysis suggests novel loci underlying thyroid antibodies in Hashimoto’s thyroiditis. Sci. Rep. 2019, 9, 5360. [Google Scholar] [CrossRef]
- Chong, W.; Shang, L.; Liu, J.; Fang, Z.; Du, F.; Wu, H.; Liu, Y.; Wang, Z.; Chen, Y.; Jia, S.; et al. A regulator-based methylation modification patterns characterized by distinct tumor microenvironment immune profiles in colon cancer. Theranostics 2021, 11, 2201–2217. [Google Scholar] [CrossRef]
- Shahjaman, M.; Manir Hossain Mollah, M.; Rezanur Rahman, M.; Islam, S.M.S.; Nurul Haque Mollah, M. Robust identification of differentially expressed genes from RNA-seq data. Genomics 2020, 112, 2000–2010. [Google Scholar] [CrossRef]
- Garcia-Reyero, N.; Griffitt, R.; Liu, L.; Kroll, K.; Farmerie, W.; Barber, D.; Denslow, N. Construction of a robust microarray from a non-model species largemouth bass, Micropterus salmoides (Lacèpede), using pyrosequencing technology. J. Fish Biol. 2008, 72, 2354–2376. [Google Scholar] [CrossRef]
- Llorens, F.; Hummel, M.; Pantano, L.; Pastor, X.; Vivancos, A.; Castillo, E.; Mattlin, H.; Ferrer, A.; Ingham, M.; Noguera, M.; et al. Microarray and deep sequencing cross-platform analysis of the mirRNome and isomiR variation in response to epidermal growth factor. BMC Genom. 2013, 14, 371. [Google Scholar] [CrossRef]
- Perez-Santángelo, S.; Mancini, E.; Francey, L.J.; Schlaen, R.G.; Chernomoretz, A.; Hogenesch, J.B.; Yanovsky, M.J. Role for LSM genes in the regulation of circadian rhythms. Proc. Nat. Acad. Sci. USA 2014, 111, 15166. [Google Scholar] [CrossRef]
- Derksen, A.; Shih, H.-Y.; Forget, D.; Darbelli, L.; Tran, L.T.; Poitras, C.; Guerrero, K.; Tharun, S.; Alkuraya, F.S.; Kurdi, W.I.; et al. Variants in LSM7 impair LSM complexes assembly, neurodevelopment in zebrafish and may be associated with an ultra-rare neurological disease. Hum. Genet. Genom. Adv. 2021, 2, 100034. [Google Scholar] [CrossRef]
- Chandrashekar, D.S.; Bashel, B.; Balasubramanya, S.A.H.; Creighton, C.J.; Ponce-Rodriguez, I.; Chakravarthi, B.V.S.K.; Varambally, S. UALCAN: A portal for facilitating tumor subgroup gene expression and survival analyses. Neoplasia 2017, 19, 649–658. [Google Scholar] [CrossRef]
- Modhukur, V.; Iljasenko, T.; Metsalu, T.; Lokk, K.; Laisk-Podar, T.; Vilo, J. MethSurv: A web tool to perform multivariable survival analysis using DNA methylation data. Epigenomics 2018, 10, 277–288. [Google Scholar] [CrossRef]
- Curtis, C.; Shah, S.P.; Chin, S.F.; Turashvili, G.; Rueda, O.M.; Dunning, M.J.; Speed, D.; Lynch, A.G.; Samarajiwa, S.; Yuan, Y.; et al. The genomic and transcriptomic architecture of 2000 breast tumours reveals novel subgroups. Nature 2012, 486, 346–352. [Google Scholar] [CrossRef]
- Koboldt, D.C.; Fulton, R.S.; McLellan, M.D.; Schmidt, H.; Kalicki-Veizer, J.; McMichael, J.F.; Fulton, L.L.; Dooling, D.J.; Ding, L.; Mardis, E.R.; et al. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef]
- Gao, J.; Aksoy, B.A.; Dogrusoz, U.; Dresdner, G.; Gross, B.; Sumer, S.O.; Sun, Y.; Jacobsen, A.; Sinha, R.; Larsson, E. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Sig. 2013, 6, pl1. [Google Scholar] [CrossRef]
- Network, C.G.A. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61. [Google Scholar] [CrossRef]
- Hagerling, C.; Gonzalez, H.; Salari, K.; Wang, C.-Y.; Lin, C.; Robles, I.; van Gogh, M.; Dejmek, A.; Jirström, K.; Werb, Z. Immune effector monocyte–neutrophil cooperation induced by the primary tumor prevents metastatic progression of breast cancer. Proc. Nat. Acad. Sci. USA 2019, 116, 21704–21714. [Google Scholar] [CrossRef]
- Wang, C.-Y.; Chiao, C.-C.; Phan, N.N.; Li, C.-Y.; Sun, Z.-D.; Jiang, J.-Z.; Hung, J.-H.; Chen, Y.-L.; Yen, M.-C.; Weng, T.-Y. Gene signatures and potential therapeutic targets of amino acid metabolism in estrogen receptor-positive breast cancer. Am. J. Cancer Res. 2020, 10, 95. [Google Scholar]
- Gbenedio, O.M.; Bonnans, C.; Grun, D.; Wang, C.-Y.; Hatch, A.J.; Mahoney, M.R.; Barras, D.; Matli, M.; Miao, Y.; Garcia, K.C. RasGRP1 is a potential biomarker for stratifying anti-EGFR therapy response in colorectal cancer. JCI Insight 2019, 4, e127552. [Google Scholar] [CrossRef]
- Sun, Z.; Wang, C.-Y.; Lawson, D.A.; Kwek, S.; Velozo, H.G.; Owyong, M.; Lai, M.-D.; Fong, L.; Wilson, M.; Su, H. Single-cell RNA sequencing reveals gene expression signatures of breast cancer-associated endothelial cells. Oncotarget 2018, 9, 10945. [Google Scholar] [CrossRef]
- Wang, C.-Y.; Li, C.-Y.; Hsu, H.-P.; Cho, C.-Y.; Yen, M.-C.; Weng, T.-Y.; Chen, W.-C.; Hung, Y.-H.; Lee, K.-T.; Hung, J.-H. PSMB5 plays a dual role in cancer development and immunosuppression. Am. J. Cancer Res. 2017, 7, 2103. [Google Scholar] [PubMed]
- Chen, P.S.; Hsu, H.P.; Phan, N.N.; Yen, M.C.; Chen, F.W.; Liu, Y.W.; Lin, F.P.; Feng, S.Y.; Cheng, T.L.; Yeh, P.H.; et al. CCDC167 as a potential therapeutic target and regulator of cell cycle-related networks in breast cancer. Aging 2021, 12. [Google Scholar] [CrossRef]
- Lawson, D.A.; Bhakta, N.R.; Kessenbrock, K.; Prummel, K.D.; Yu, Y.; Takai, K.; Zhou, A.; Eyob, H.; Balakrishnan, S.; Wang, C.-Y. Single-cell analysis reveals a stem-cell program in human metastatic breast cancer cells. Nature 2015, 526, 131–135. [Google Scholar] [CrossRef]
- Györffy, B.; Lanczky, A.; Eklund, A.C.; Denkert, C.; Budczies, J.; Li, Q.; Szallasi, Z. An online survival analysis tool to rapidly assess the effect of 22,277 genes on breast cancer prognosis using microarray data of 1809 patients. Breast. Cancer Res. Treat. 2010, 123, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Thul, P.J.; Lindskog, C. The human protein atlas: A spatial map of the human proteome. Protein Sci. 2018, 27, 233–244. [Google Scholar] [CrossRef]
- Li, T.; Fan, J.; Wang, B.; Traugh, N.; Chen, Q.; Liu, J.S.; Li, B.; Liu, X.S. TIMER: A Web server for comprehensive analysis of tumor-infiltrating immune cells. Cancer Res. 2017, 77, e108. [Google Scholar] [CrossRef]
- Kao, T.J.; Wu, C.C.; Phan, N.N.; Liu, Y.H.; Ta, H.D.K.; Anuraga, G.; Wu, Y.F.; Lee, K.H.; Chuang, J.Y.; Wang, C.Y. Prognoses and genomic analyses of proteasome 26S subunit, ATPase (PSMC) family genes in clinical breast cancer. Aging 2021, 13, 17970. [Google Scholar] [CrossRef]
- Choy, T.K.; Wang, C.Y.; Phan, N.N.; Khoa Ta, H.D.; Anuraga, G.; Liu, Y.H.; Wu, Y.F.; Lee, K.H.; Chuang, J.Y.; Kao, T.J. Identification of Dipeptidyl Peptidase (DPP) family genes in clinical breast cancer patients via an integrated bioinformatics approach. Diagnostics 2021, 11, 1204. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.H.; Yeh, I.J.; Phan, N.N.; Yen, M.C.; Hung, J.H.; Chiao, C.C.; Chen, C.F.; Sun, Z.; Hsu, H.P.; Wang, C.Y.; et al. Gene signatures and potential therapeutic targets of Middle East respiratory syndrome coronavirus (MERS-CoV)-infected human lung adenocarcinoma epithelial cells. J. Microbiol. Immunol. Infect. 2021. [Google Scholar] [CrossRef]
- Anuraga, G.; Tang, W.C.; Phan, N.N.; Ta, H.D.K.; Liu, Y.H.; Wu, Y.F.; Lee, K.H.; Wang, C.Y. Comprehensive Analysis of Prognostic and Genetic Signatures for General Transcription Factor III (GTF3) in clinical colorectal cancer patients using bioinformatics approaches. Curr. Issues Mol. Biol. 2021, 43, 2. [Google Scholar] [CrossRef]
- Khoa Ta, H.D.; Tang, W.C.; Phan, N.N.; Anuraga, G.; Hou, S.Y.; Chiao, C.C.; Liu, Y.H.; Wu, Y.F.; Lee, K.H.; Wang, C.Y. Analysis of LAGEs family gene signature and prognostic relevance in breast cancer. Diagnostics 2021, 11, 726. [Google Scholar] [CrossRef]
- Jin, B.; Li, Y.; Robertson, K.D. DNA methylation: Superior or subordinate in the epigenetic hierarchy? Genes Cancer 2011, 2, 607–617. [Google Scholar] [CrossRef]
- Daniel, F.I.; Cherubini, K.; Yurgel, L.S.; de Figueiredo, M.A.; Salum, F.G. The role of epigenetic transcription repression and DNA methyltransferases in cancer. Cancer 2011, 117, 677–687. [Google Scholar] [CrossRef]
- Whiteside, T.L. The tumor microenvironment and its role in promoting tumor growth. Oncogene 2008, 27, 5904–5912. [Google Scholar] [CrossRef]
- Wang, M.; Zhao, J.; Zhang, L.; Wei, F.; Lian, Y.; Wu, Y.; Gong, Z.; Zhang, S.; Zhou, J.; Cao, K.; et al. Role of tumor microenvironment in tumorigenesis. J. Cancer 2017, 8, 761–773. [Google Scholar] [CrossRef]
- Ribeiro Franco, P.I.; Rodrigues, A.P.; de Menezes, L.B.; Pacheco Miguel, M. Tumor microenvironment components: Allies of cancer progression. Pathol. Res. Pract. 2020, 216, 152729. [Google Scholar] [CrossRef]
- Joyce, J.A. Therapeutic targeting of the tumor microenvironment. Cancer Cell 2005, 7, 513–520. [Google Scholar] [CrossRef]
- Bei, Y.; Cheng, N.; Chen, T.; Shu, Y.; Yang, Y.; Yang, N.; Zhou, X.; Liu, B.; Wei, J.; Liu, Q.; et al. CDK5 Inhibition Abrogates TNBC Stem-Cell Property and Enhances Anti-PD-1 Therapy. Adv. Sci. 2020, 7, 2001417. [Google Scholar] [CrossRef]
- Yu, J.M.; Sun, W.; Wang, Z.H.; Liang, X.; Hua, F.; Li, K.; Lv, X.X.; Zhang, X.W.; Liu, Y.Y.; Yu, J.J.; et al. TRIB3 supports breast cancer stemness by suppressing FOXO1 degradation and enhancing SOX2 transcription. Nat. Commun. 2019, 10, 5720. [Google Scholar] [CrossRef]
- Lahouel, K.; Younes, L.; Danilova, L.; Giardiello, F.M.; Hruban, R.H.; Groopman, J.; Kinzler, K.W.; Vogelstein, B.; Geman, D.; Tomasetti, C. Revisiting the tumorigenesis timeline with a data-driven generative model. Proc. Natl. Acad. Sci. USA 2020, 117, 857–864. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Female Breast Cancer; National Institutes of Health, National Cancer Institute: Bethseda, MD, USA, 2018. [Google Scholar]
- Barrett, T.; Wilhite, S.E.; Ledoux, P.; Evangelista, C.; Kim, I.F.; Tomashevsky, M.; Marshall, K.A.; Phillippy, K.H.; Sherman, P.M.; Holko, M.; et al. NCBI GEO: Archive for functional genomics data sets—Update. Nucleic Acids Res. 2013, 41, D991–D995. [Google Scholar] [CrossRef]
- Lin, J.C.; Liu, T.P.; Yang, P.M. CDKN2A-inactivated pancreatic ductal adenocarcinoma exhibits therapeutic sensitivity to paclitaxel: A bioinformatics study. J. Clin. Med. 2020, 9, 4019. [Google Scholar] [CrossRef]
- Lin, T.Y.; Wang, P.W.; Huang, C.H.; Yang, P.M.; Pan, T.L. Characterizing the relapse potential in different luminal subtypes of breast cancers with functional proteomics. Int. J. Mol. Sci. 2020, 21, 6077. [Google Scholar] [CrossRef]
- Liu, L.W.; Hsieh, Y.Y.; Yang, P.M. Bioinformatics Data Mining Repurposes the JAK2 (Janus Kinase 2) Inhibitor fedratinib for treating pancreatic ductal adenocarcinoma by reversing the KRAS (Kirsten Rat Sarcoma 2 Viral Oncogene Homolog)-driven gene signature. J. Pers. Med. 2020, 10, 130. [Google Scholar] [CrossRef]
- Yang, P.M.; Hsieh, Y.Y.; Du, J.L.; Yen, S.C.; Hung, C.F. Sequential interferon β-cisplatin treatment enhances the surface exposure of calreticulin in cancer cells via an interferon regulatory factor 1-dependent manner. Biomolecules 2020, 10, 643. [Google Scholar] [CrossRef]
- Yang, P.M.; Lin, L.S.; Liu, T.P. Sorafenib inhibits Ribonucleotide Reductase Regulatory Subunit M2 (RRM2) in hepatocellular carcinoma cells. Biomolecules 2020, 10, 117. [Google Scholar] [CrossRef]
- Kumar, A.; Swain, C.A.; Shevde, L.A. Informing the new developments and future of cancer immunotherapy: Future of cancer immunotherapy. Cancer Metastasis Rev. 2021. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.A.; Ngamcherdtrakul, W.; Luoh, S.W.; Yantasee, W. Prognostic and therapeutic role of tumor-infiltrating lymphocyte subtypes in breast cancer. Cancer Metastasis Rev. 2021. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Liu, S.; Leung, S.; Gru, A.A.; Tao, Y.; Hoog, J.; Ho, J.; Davies, S.R.; Allred, D.C.; Salavaggione, A.L.; et al. An mRNA gene expression-based signature to identify FGFR1-amplified estrogen receptor-positive breast tumors. J. Mol. Diagn. 2017, 19, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Young, J.H.; Peyton, M.; Seok Kim, H.; McMillan, E.; Minna, J.D.; White, M.A.; Marcotte, E.M. Computational discovery of pathway-level genetic vulnerabilities in non-small-cell lung cancer. Bioinformatics 2016, 32, 1373–1379. [Google Scholar] [CrossRef]
- Rosen, J.; He, M.; Umbricht, C.; Alexander, H.R.; Dackiw, A.P.; Zeiger, M.A.; Libutti, S.K. A six-gene model for differentiating benign from malignant thyroid tumors on the basis of gene expression. Surgery 2005, 138, 1050–1056. [Google Scholar] [CrossRef]
- Kontomanolis, E.N.; Koutras, A.; Syllaios, A.; Schizas, D.; Mastoraki, A.; Garmpis, N.; Diakosavvas, M.; Angelou, K.; Tsatsaris, G.; Pagkalos, A.; et al. Role of oncogenes and tumor-suppressor genes in carcinogenesis: A review. Anticancer Res. 2020, 40, 6009. [Google Scholar] [CrossRef]
- Yang, Z.Q.; Streicher, K.L.; Ray, M.E.; Abrams, J.; Ethier, S.P. Multiple interacting oncogenes on the 8p11–p12 amplicon in human breast cancer. Cancer Res. 2006, 66, 11632–11643. [Google Scholar] [CrossRef]
- Yang, Z.Q.; Liu, G.; Bollig-Fischer, A.; Giroux, C.N.; Ethier, S.P. Transforming properties of 8p11–12 amplified genes in human breast cancer. Cancer Res. 2010, 70, 8487–8497. [Google Scholar] [CrossRef]
- Little, E.C.; Camp, E.R.; Wang, C.; Watson, P.M.; Watson, D.K.; Cole, D.J. The CaSm (LSm1) oncogene promotes transformation, chemoresistance and metastasis of pancreatic cancer cells. Oncogenesis 2016, 5, e182. [Google Scholar] [CrossRef]
- Pan, Y.; Liu, H.; Wang, Y.; Kang, X.; Liu, Z.; Owzar, K.; Han, Y.; Su, L.; Wei, Y.; Hung, R.J.; et al. Associations between genetic variants in mRNA splicing-related genes and risk of lung cancer: A pathway-based analysis from published GWASs. Sci. Rep. 2017, 7, 44634. [Google Scholar] [CrossRef]
- Lyng, H.; Brøvig, R.S.; Svendsrud, D.H.; Holm, R.; Kaalhus, O.; Knutstad, K.; Oksefjell, H.; Sundfør, K.; Kristensen, G.B.; Stokke, T. Gene expressions and copy numbers associated with metastatic phenotypes of uterine cervical cancer. BMC Genom. 2006, 7, 268. [Google Scholar] [CrossRef]
- Tan, M.S.; Chang, S.W.; Cheah, P.L.; Yap, H.J. Integrative machine learning analysis of multiple gene expression profiles in cervical cancer. PeerJ. 2018, 6, e5285. [Google Scholar] [CrossRef]
- Xie, N.; Yao, Y.; Wan, L.; Zhu, T.; Liu, L.; Yuan, J. Next-generation sequencing reveals lymph node metastasis associated genetic markers in colorectal cancer. Exp. Ther. Med. 2017, 14, 338–343. [Google Scholar] [CrossRef][Green Version]
- Gandini, R.; Dossena, S.; Vezzoli, V.; Tamplenizza, M.; Salvioni, E.; Ritter, M.; Paulmichl, M.; Furst, J. LSm4 associates with the plasma membrane and acts as a co-factor in cell volume regulation. Cell Physiol. Biochem. 2008, 22, 579–590. [Google Scholar] [CrossRef]
- Xue, R.; Hua, L.; Xu, W.; Gao, Y.; Pang, Y.; Hao, J. Derivation and validation of the potential core genes in pancreatic cancer for tumor-stroma crosstalk. Biomed. Res. Int. 2018, 2018, 4283673. [Google Scholar] [CrossRef]
- Long, Y.; Weng, W.H.; Li, F.; Yuan, X.; Li, Z. The effect of RNA binding protein Lsm4 on the proliferation and migration of esophageal carcinoma cell line EC109. Tumor 2014, 34, 204–210. [Google Scholar] [CrossRef]
- Hou, W.; Zhang, Y. Circ_0025033 promotes the progression of ovarian cancer by activating the expression of LSM4 via targeting miR-184. Pathol. Res. Pract. 2021, 217, 153275. [Google Scholar] [CrossRef]
- Yin, J.; Lin, C.; Jiang, M.; Tang, X.; Xie, D.; Chen, J.; Ke, R. CENPL, ISG20L2, LSM4, MRPL3 are four novel hub genes and may serve as diagnostic and prognostic markers in breast cancer. Sci. Rep. 2021, 11, 15610. [Google Scholar] [CrossRef]
- Wang, L.; Wrobel, J.A.; Xie, L.; Li, D.; Zurlo, G.; Shen, H.; Yang, P.; Wang, Z.; Peng, Y.; Gunawardena, H.P.; et al. Novel RNA-affinity proteogenomics dissects tumor heterogeneity for revealing personalized markers in precision prognosis of cancer. Cell Chem. Biol. 2018, 25, 619–633. [Google Scholar] [CrossRef]
- Kamikubo, Y. Genetic compensation of RUNX family transcription factors in leukemia. Cancer Sci. 2018, 109, 2358–2363. [Google Scholar] [CrossRef]
- Carelle-Calmels, N.; Saugier-Veber, P.; Girard-Lemaire, F.; Rudolf, G.; Doray, B.; Guérin, E.; Kuhn, P.; Arrivé, M.; Gilch, C.; Schmitt, E.; et al. Genetic compensation in a human genomic disorder. N. Engl. J. Med. 2009, 360, 1211–1216. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, I.P.M.; Novelli, M.R.; Bodmer, W.F. The mutation rate and cancer. Proc. Nat. Acad. Sci. USA 1996, 93, 14800. [Google Scholar] [CrossRef] [PubMed]
- Van Aelst, L.; D’Souza-Schorey, C. Rho GTPases and signaling networks. Genes Dev. 1997, 11, 2295–2322. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, C.; Su, B.; Song, Q.; Zhang, Y.; Luo, Y.; Li, Q.; Tan, W.; Ma, D.; Wang, L. Recombinant human PDCD5 protein enhances chemosensitivity of breast cancer in vitro and in vivo. Biochem. Cell Biol. 2013, 91, 526–531. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, L.Q.; Yang, C.C.; Li, J.; Tian, X.Y.; Li, D.N.; Cui, J.; Cai, J.P. The high expression of NUDT5 indicates poor prognosis of breast cancer by modulating AKT/Cyclin D signaling. PLoS ONE 2021, 16, e0245876. [Google Scholar] [CrossRef]
- Van Genderen, C.; Harkness, T.A.A.; Arnason, T.G. The role of anaphase promoting complex activation, inhibition and substrates in cancer development and progression. Aging 2020, 12, 15818–15855. [Google Scholar] [CrossRef]
- Chan, S.; Sridhar, P.; Kirchner, R.; Lock, Y.J.; Herbert, Z.; Buonamici, S.; Smith, P.; Lieberman, J.; Petrocca, F. Basal-A Triple-Negative Breast Cancer Cells Selectively Rely on RNA Splicing for Survival. Mol. Cancer Ther. 2017, 16, 2849. [Google Scholar] [CrossRef]
- Tay, R.E.; Richardson, E.K.; Toh, H.C. Revisiting the role of CD4+ T cells in cancer immunotherapy—New insights into old paradigms. Cancer Gene Ther. 2021, 28, 5–17. [Google Scholar] [CrossRef]
- Chan, M.-Y.; Lee, B.-J.; Chang, P.-S.; Hsiao, H.-Y.; Hsu, L.-P.; Chang, C.-H.; Lin, P.-T. The risks of ubiquinone and β-carotene deficiency and metabolic disorders in patients with oral cancer. BMC Cancer 2020, 20, 310. [Google Scholar] [CrossRef]
- Zhao, L.; Yang, X.; Feng, C.; Wang, Y.; Wang, Q.; Pei, J.; Wu, J.; Li, S.; Zhang, H.; Cao, X. Triple-negative breast cancer cells respond to T cells severely at the alternative splicing layer. Electr. J. Biotechnol. 2021, 50, 59–67. [Google Scholar] [CrossRef]
- Jaillon, S.; Ponzetta, A.; Di Mitri, D.; Santoni, A.; Bonecchi, R.; Mantovani, A. Neutrophil diversity and plasticity in tumour progression and therapy. Nat. Rev. Cancer 2020, 20, 485–503. [Google Scholar] [CrossRef]
- Wu, L.; Saxena, S.; Awaji, M.; Singh, R.K. Tumor-associated neutrophils in cancer: Going pro. Cancers 2019, 11, 564. [Google Scholar] [CrossRef]
- Olson, M.F.; Sahai, E. The actin cytoskeleton in cancer cell motility. Clin. Exp. Metastasis 2008, 26, 273. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Condeelis, J. Regulation of the actin cytoskeleton in cancer cell migration and invasion. Biochim. Biophys. Acta (BBA) Mol. Cell Res. 2007, 1773, 642–652. [Google Scholar] [CrossRef]
- Ostuni, R.; Kratochvill, F.; Murray, P.J.; Natoli, G. Macrophages and cancer: From mechanisms to therapeutic implications. Trends Immunol. 2015, 36, 229–239. [Google Scholar] [CrossRef]
- Duan, Z.; Luo, Y. Targeting macrophages in cancer immunotherapy. Sign. Transduct. Target. Ther. 2021, 6, 127. [Google Scholar] [CrossRef]
- Nielsen, S.R.; Schmid, M.C. Macrophages as key drivers of cancer progression and metastasis. Mediat. Inflamm. 2017, 2017, 9624760. [Google Scholar] [CrossRef]
- Binnewies, M.; Roberts, E.W.; Kersten, K.; Chan, V.; Fearon, D.F.; Merad, M.; Coussens, L.M.; Gabrilovich, D.I.; Ostrand-Rosenberg, S.; Hedrick, C.C.; et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 2018, 24, 541–550. [Google Scholar] [CrossRef]
- Burugu, S.; Asleh-Aburaya, K.; Nielsen, T.O. Immune infiltrates in the breast cancer microenvironment: Detection, characterization and clinical implication. Breast Cancer 2017, 24, 3–15. [Google Scholar] [CrossRef]
- Cohen, I.J.; Blasberg, R. Impact of the tumor microenvironment on tumor-infiltrating lymphocytes: Focus on breast cancer. Breast Cancer 2017, 11, 1178223417731565. [Google Scholar] [CrossRef]
- Luckheeram, R.V.; Zhou, R.; Verma, A.D.; Xia, B. CD4⁺T cells: Differentiation and functions. Clin. Dev. Immunol. 2012, 2012, 925135. [Google Scholar] [CrossRef]
- Ohue, Y.; Nishikawa, H. Regulatory T (Treg) cells in cancer: Can Treg cells be a new therapeutic target? Cancer Sci. 2019, 110, 2080–2089. [Google Scholar] [CrossRef] [PubMed]
- Stenström, J.; Hedenfalk, I.; Hagerling, C. Regulatory T lymphocyte infiltration in metastatic breast cancer—an independent prognostic factor that changes with tumor progression. Breast Cancer Res. 2021, 23, 27. [Google Scholar] [CrossRef]
- Verma, C.; Kaewkangsadan, V.; Eremin, J.M.; Cowley, G.P.; Ilyas, M.; El-Sheemy, M.A.; Eremin, O. Natural killer (NK) cell profiles in blood and tumour in women with large and locally advanced breast cancer (LLABC) and their contribution to a pathological complete response (PCR) in the tumour following neoadjuvant chemotherapy (NAC): Differential restoration of blood profiles by NAC and surgery. J. Transl. Med. 2015, 13, 180. [Google Scholar] [CrossRef] [PubMed]
- Oh, K.; Lee, O.Y.; Shon, S.Y.; Nam, O.; Ryu, P.M.; Seo, M.W.; Lee, D.S. A mutual activation loop between breast cancer cells and myeloid-derived suppressor cells facilitates spontaneous metastasis through IL-6 trans-signaling in a murine model. Breast Cancer Res. 2013, 15, R79. [Google Scholar] [CrossRef]
- Markowitz, J.; Wesolowski, R.; Papenfuss, T.; Brooks, T.R.; Carson, W.E., 3rd. Myeloid-derived suppressor cells in breast cancer. Breast Cancer Res. Treat. 2013, 140, 13–21. [Google Scholar] [CrossRef]
- Chen, N.; Feng, Q.; Deng, J.; Xiong, Y.; Deng, Y.J.; Wang, M.M.; Zhou, L.; Yu, Q.W.; Hu, J.P.; Deng, H. Hdc-expressing myeloid-derived suppressor cells promote basal-like transition and metastasis of breast cancer. Int. J. Clin. Exp. Pathol. 2020, 13, 1431–1443. [Google Scholar]
- Xing, S.; Wang, Y.; Hu, K.; Wang, F.; Sun, T.; Li, Q. WGCNA reveals key gene modules regulated by the combined treatment of colon cancer with PHY906 and CPT11. Biosci. Rep. 2020, 40, BSR20200935. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ta, H.D.K.; Wang, W.-J.; Phan, N.N.; An Ton, N.T.; Anuraga, G.; Ku, S.-C.; Wu, Y.-F.; Wang, C.-Y.; Lee, K.-H. Potential Therapeutic and Prognostic Values of LSM Family Genes in Breast Cancer. Cancers 2021, 13, 4902. https://doi.org/10.3390/cancers13194902
Ta HDK, Wang W-J, Phan NN, An Ton NT, Anuraga G, Ku S-C, Wu Y-F, Wang C-Y, Lee K-H. Potential Therapeutic and Prognostic Values of LSM Family Genes in Breast Cancer. Cancers. 2021; 13(19):4902. https://doi.org/10.3390/cancers13194902
Chicago/Turabian StyleTa, Hoang Dang Khoa, Wei-Jan Wang, Nam Nhut Phan, Nu Thuy An Ton, Gangga Anuraga, Su-Chi Ku, Yung-Fu Wu, Chih-Yang Wang, and Kuen-Haur Lee. 2021. "Potential Therapeutic and Prognostic Values of LSM Family Genes in Breast Cancer" Cancers 13, no. 19: 4902. https://doi.org/10.3390/cancers13194902
APA StyleTa, H. D. K., Wang, W.-J., Phan, N. N., An Ton, N. T., Anuraga, G., Ku, S.-C., Wu, Y.-F., Wang, C.-Y., & Lee, K.-H. (2021). Potential Therapeutic and Prognostic Values of LSM Family Genes in Breast Cancer. Cancers, 13(19), 4902. https://doi.org/10.3390/cancers13194902









