Radiation-Associated Angiosarcoma of the Breast and Chest Wall Treated with Thermography-Controlled, Contactless wIRA-Hyperthermia and Hypofractionated Re-Irradiation
Abstract
:Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Patient Groups
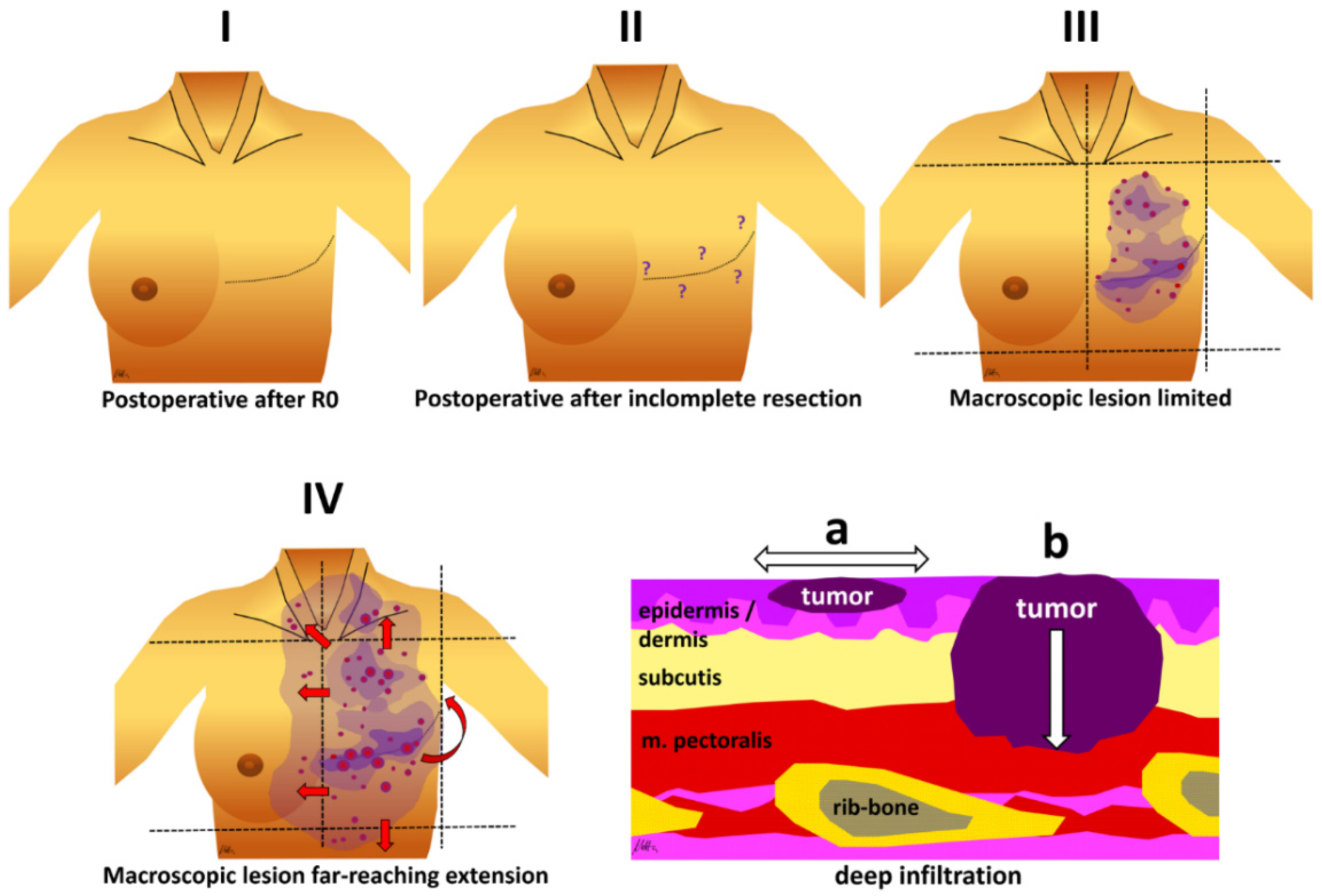
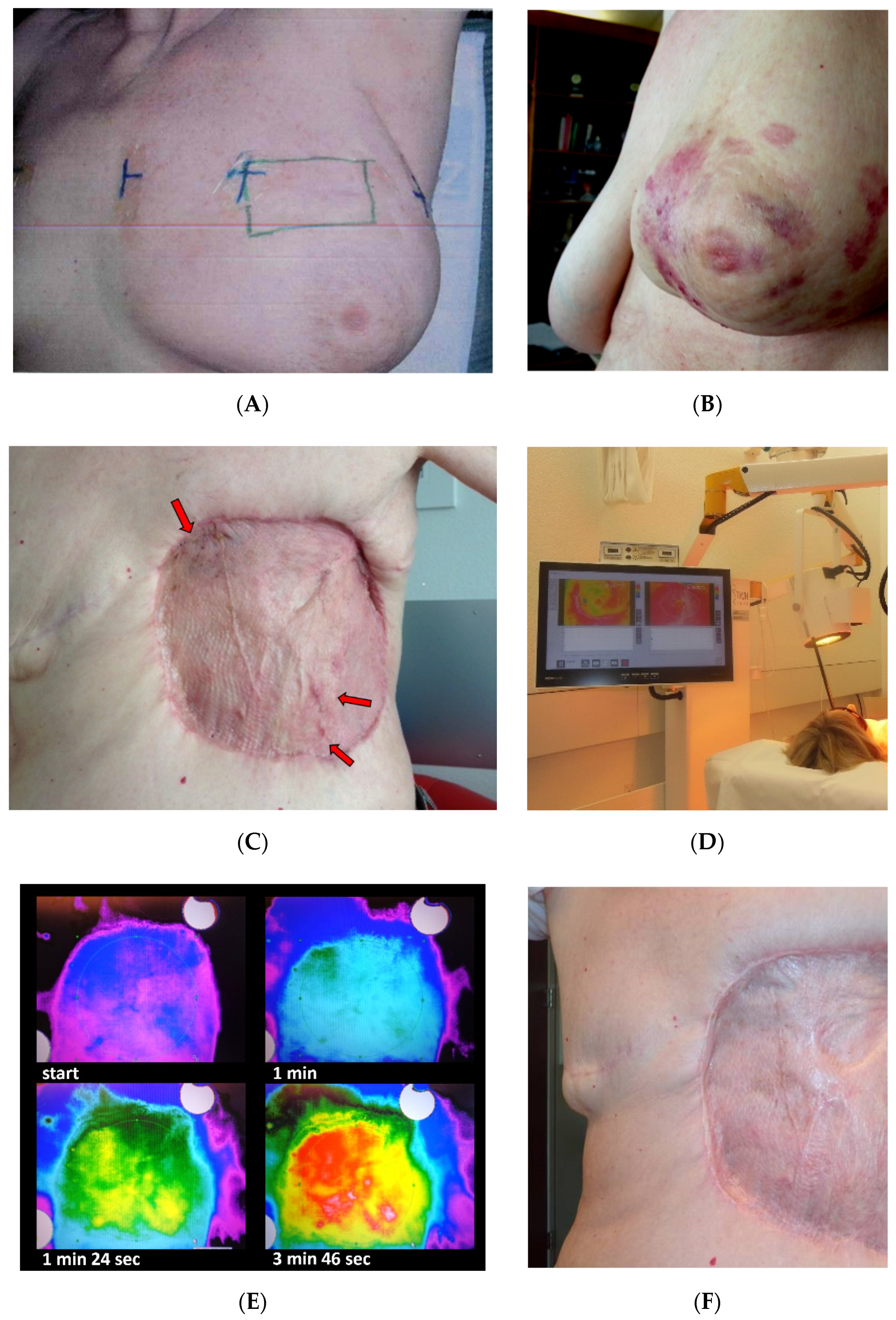
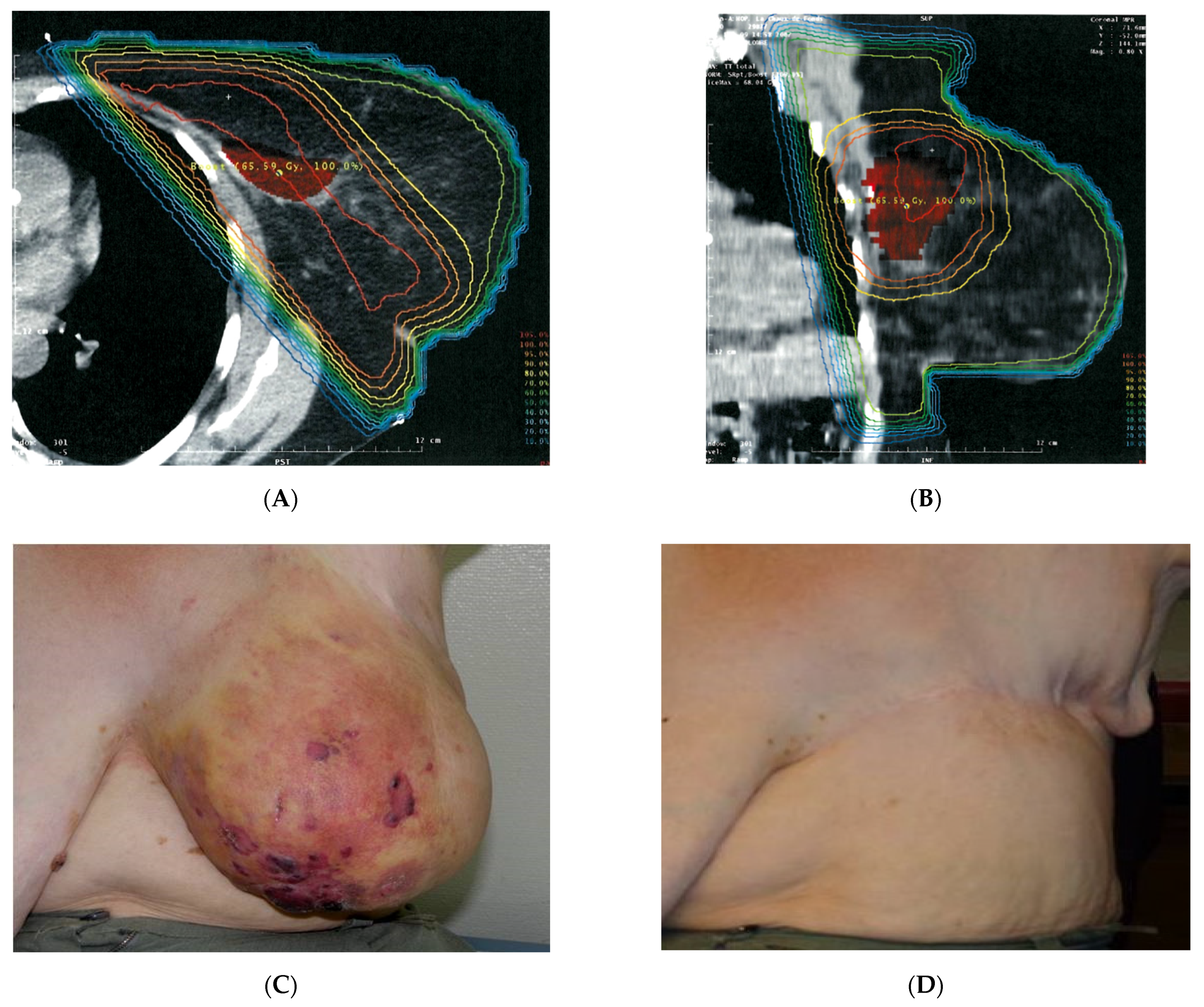
2.2. Treatment
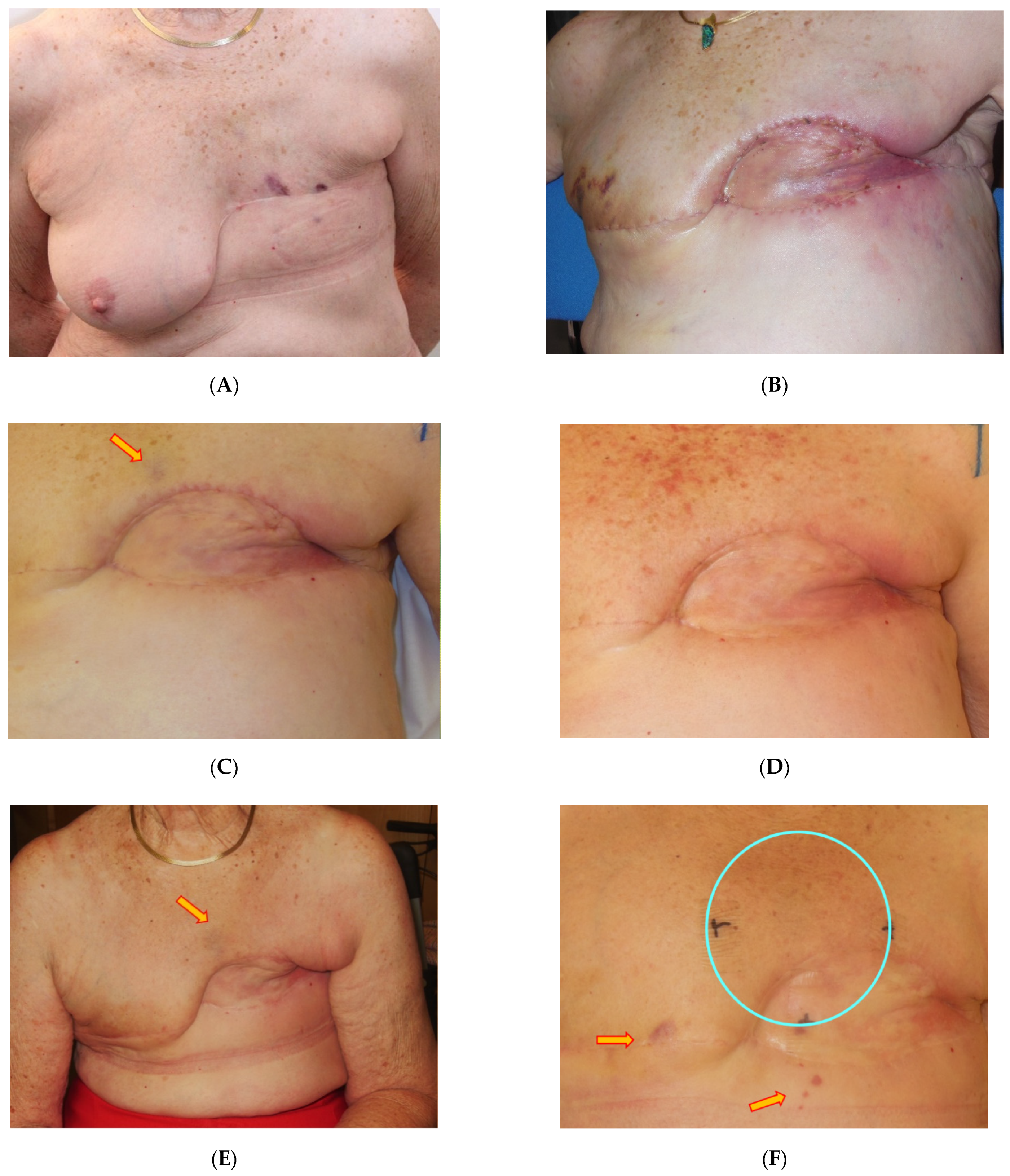
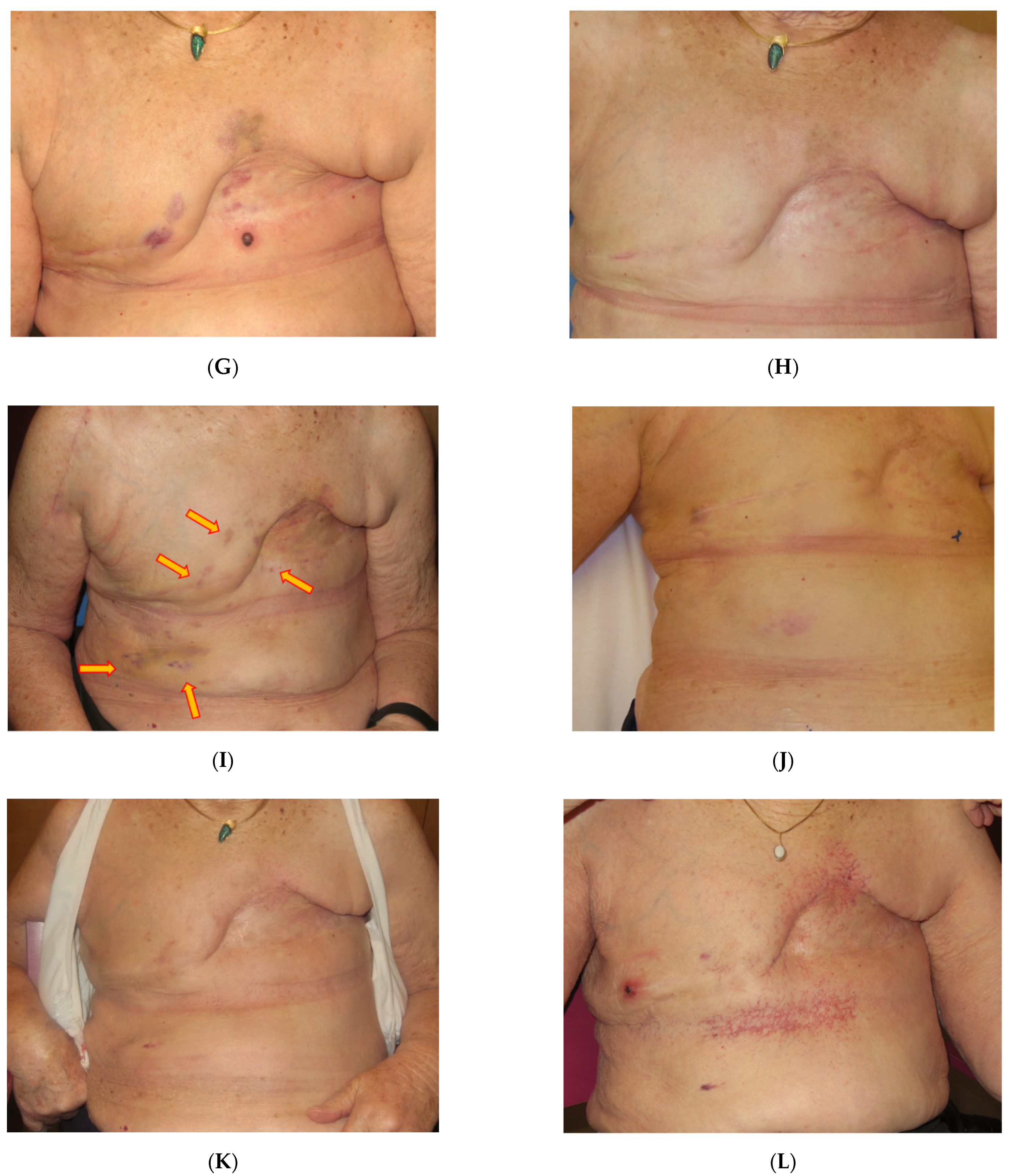
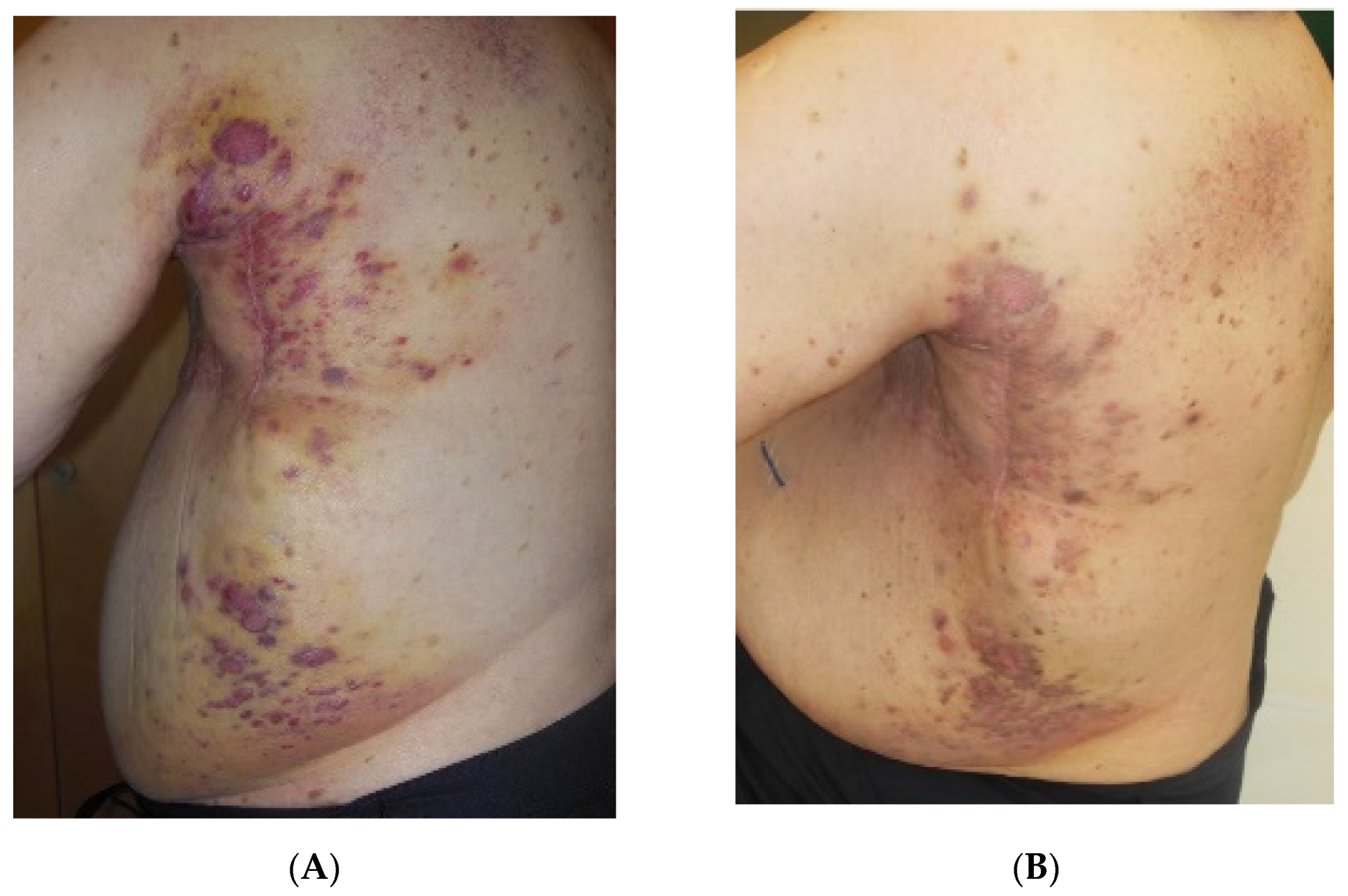
3. Results
3.1. Treatment Outcome
3.2. Toxicity
4. Discussion
5. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RAASB = radiation associated angiosarcoma of the breast |
| LRBC = locally recurrent breast cancer |
| RT = radiotherapy |
| re-RT = re-irradiation |
| HART = hypofractionated accelerated radiotherapy |
| wIRA = water filtered infrared-A |
| HT = hyperthermia |
| CT = chemotherapy |
| H = hormone therapy |
| S = surgery |
| OS = overall survival |
| LR = local recurrence |
| LRR = local recurrence rate |
| RFS = recurrence-free survival |
| FU = follow up |
| LFU = lost to follow-up |
| CR = complete remission |
| PR = partial remission |
| SD = stable disease |
| PD = progressive disease |
| LC = local control |
| NED = no evidence of disease |
| TA = telangiectases |
| AVL = atypical vascular lesions |
| Dx = diagnosis |
| TM = total mastectomy |
| Cobalt-60 = radiation unit using 60Co sources |
References
- Laé, M.; Lebel, A.; Hamel-Viard, F.; Asselain, B.; Trassard, M.; Sastre, X.; Kirova, Y.M. Can c-myc amplification reliably dis-criminate postradiation from primary angiosarcoma of the breast? Cancer Radiother. 2015, 19, 168–174. [Google Scholar] [CrossRef]
- Mito, J.K.; Mitra, D.; Barysauskas, C.M.; Marino-Enriquez, A.; Morgan, E.A.; Fletcher, C.D.M.; Raut, C.P.; Baldini, E.H.; Doyle, L.A. A comparison of outcomes and prognostic features for radiation-associated angiosarcoma of the breast and other radia-tion-associated sarcomas. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Bonito, F.J.P.; de Almeida Cerejeira, D.; Dahlstedt-Ferreira, C.; Coelho, H.O.; Rosas, R. Radiation-induced angiosarcoma of the breast: A review. Breast J. 2019, 26, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Rombouts, A.J.M.; Huising, J.; Hugen, N.; Siesling, S.; Poortmans, P.M.; Nagtegaal, I.D.; de Wilt, J.H.W. Assessment of radiotherapy-associated angiosarcoma after breast cancer treatment in a Dutch population-based study. JAMA Oncol. 2019, 5, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Salminen, S.H.; Wiklund, T.; Sampo, M.M.; Tarkkanen, M.; Pulliainen, L.; Böhling, T.O.; Tukiainen, E.; Hukkinen, K.; Blomqvist, C.P. Treatment and prognosis of radiation-associated breast angiosarcoma in a nationwide population. Ann. Surg. Oncol. 2019, 27, 1002–1010. [Google Scholar] [CrossRef] [Green Version]
- Taffurelli, M.; Pellegrini, A.; Meattini, I.; Orzalesi, L.; Tinterri, C.; Roncella, M.; Terribile, D.; Caruso, F.; Tazzioli, G.; Pollini, G.; et al. Secondary breast angiosarcoma: A multicentre retrospective survey by the national Italian association of Breast Surgeons (ANISC). Breast 2019, 45, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Depla, A.L.; Scharloo-Karels, C.H.; de Jong, M.A.A.; Oldenborg, S.; Kolff, M.W.; Oei, S.B.; van Coevorden, F.; van Rhoon, G.C.; Baartman, E.A.; Scholten, R.J.; et al. Treatment and prognostic factors of radiation-associated angio-sarcoma (RAASB) after primary breast cancer: A systematic review. Eur. J. Cancer 2014, 50, 1779–1788. [Google Scholar] [CrossRef]
- Dogan, A.; Kern, P.; Schultheis, B.; Häusler, G.; Rezniczek, G.A.; Tempfer, C.B. Radiogenic angiosarcoma of the breast: Case report and systematic review of the literature. BMC Cancer 2018, 18, 463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdou, Y.; Elkhanany, A.; Attwood, K.; Ji, W.; Takabe, K.; Opyrchal, M. Primary and secondary breast angiosarcoma: Single center report and a meta-analysis. Breast Cancer Res. Treat. 2019, 178, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Gutkin, P.M.; Ganjoo, K.N.; Lohman, M.; von Eyben, R.; Charville, G.W.; Nazerali, R.S.; Dirbas, F.M.; Horst, K.C. Angiosar-coma of the breast: Management and outcomes. Am. J. Clin. Oncol. 2020, 43, 820–825. [Google Scholar] [CrossRef] [PubMed]
- Li, G.Z.; Fairweather, M.; Wang, J.; Orgill, D.P.; Bertagnolli, M.M.; Raut, C.P. Cutaneous radiation-associated breast angio-sarcoma: Radicality of surgery impacts survival. Ann. Surg. 2017, 265, 814–820. [Google Scholar] [CrossRef]
- Salminen, S.; Sampo, M.M.; Böhling, T.O.; Tuomikoski, L.; Tarkkanen, M.; Blomqvist, C. Radiation-associated sarcoma after breast cancer in a nationwide population: Increasing risk of angiosarcoma. Cancer Med. 2018, 7, 4825–4835. [Google Scholar] [CrossRef]
- Yin, M.; Wang, W.; Drabick, J.J.; Harold, H.A. Prognosis and treatment of non-metastatic primary and secondary breast an-giosarcoma: A comparative study. BMC Cancer 2017, 17, 295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seinen, J.M.; Styring, E.; Verstappen, V.; von Steyern, F.V.; Rydholm, A.; Suurmeijer, A.J.H.; Hoekstra, H.J. Radiation-associated angiosarcoma after breast cancer: High recurrence rate and poor survival despite surgical treatment with R0 resection. Ann. Surg. Oncol. 2012, 19, 2700–2706. [Google Scholar] [CrossRef] [Green Version]
- Amajoud, Z.; Vertongen, A.S.; Weytens, R.; Hauspy, J. Radiation induced angiosarcoma of the breast: Case series and review of the literature. Facts Views Vis. Obgyn. 2018, 10, 215–220. [Google Scholar]
- Alves, I.; Marques, J.C. Radiation-induced angiosarcoma of the breast: A retrospective analysis of 15 years’ experience at an oncology center. Radiol. Bras. 2018, 51, 281–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torres, K.E.; Ravi, V.; Kin, K.; Yi, M.; Guadagnolo, B.A.; May, C.D.; Arun, B.K.; Hunt, K.K.; Lam, R.; Lahat, G.; et al. Long-term outcomes in patients with radiation-associated angio-sarcomas of the breast following surgery and radiotherapy for breast cancer. Ann. Surg. Oncol. 2013, 20, 1267–1274. [Google Scholar] [CrossRef] [Green Version]
- Nestle-Krämling, C.; Bölke, E.; Budach, W.; Peiper, M.; Niederacher, D.; Janni, W.; Eisenberger, C.F.; Knoefel, W.T.; Scherer, A.; Baldus, S.E.; et al. Hämangiosarkom nach brusterhaltender Therapie beim Mammakarzinom: Vier Fallbeispiele mit molekulargenetischer Diagnostik und Literaturübersicht [Hemangiosarcoma after breast-conserving therapy of breast cancer: Report of four cases with molecular genetic diagnosis and literature review]. Strahlenther. Onkol. 2011, 187, 656–664. (In German) [Google Scholar] [CrossRef]
- Cugh, R.; Sabel, M.S.; Feng, M.; Maki, R.; Hayes, D.F.; Chagpar, A.; DeLaney, T.F. Breast Sarcoma: Treatment. Available online: https://www.uptodate.com/contents/breast-sarcoma-treatment/print (accessed on 1 May 2021).
- Smith, T.L.; Morris, C.G.; Mendenhall, N.P. Angiosarcoma after breast-conserving therapy: Long-term disease control and late effects with hyperfractionated accelerated re-irradiation (HART). Acta Oncol. 2013, 53, 235–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Jong, M.; Oldenborg, S.; Oei, S.; Griesdoorn, V.; Kolff, M.; Koning, C.; van Tienhoven, G. Reirradiation and hyperthermia for radiation-associated sarcoma. Cancer 2011, 47, S667–S668. [Google Scholar] [CrossRef]
- Linthorst, M.; van Geel, A.; Baartman, E.; Oei, S.; Ghidey, W.; van Rhoon, G.; van Der Zee, J. Effect of a combined surgery, re-irradiation and hyperthermia therapy on local control rate in radio-induced angiosarcoma of the chest wall. Strahlenther. Onkol. 2013, 189, 387–393. [Google Scholar] [CrossRef]
- Thews, O.; Li, Y.; Kelleher, D.K.; Chance, B.; Vaupel, P. Microcirculatory functions, tissue oxygenation, microregional redox status and ATP distribution in tumors upon localized infrared-A-hyperthermia at 42 °C. Adv. Exp. Med. Biol. 2003, 530, 237–247. [Google Scholar] [CrossRef]
- Thomsen, A.R.; Saalmann, M.R.; Kollefrath, M.; Grosu, A.L.; Nicolay, N.H.; Scholber, J.; Notter, M.; Vaupel, P. Oxygenation status in human skin, subcutis and superficial tumor lesions upon thermography-controlled wIRA-hyperthermia: Implications for thermoradiation of superficial tumors. Strahlenther. Onkol. 2021, 197 (Suppl. 1). [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, B.; Chen, S.; Wang, Y. Near-infrared light irradiation induced mild hyperthermia enhances glutathione de-pletion and DNA interstrand cross-link formation for efficient chemotherapy. ACS Nano 2020, 14, 14831–14845. [Google Scholar] [CrossRef]
- Oei, A.; Kok, H.; Oei, S.; Horsman, M.; Stalpers, L.; Franken, N.; Crezee, J. Molecular and biological rationale of hyperthermia as radio- and chemosensitizer. Adv. Drug Deliv. Rev. 2020, 163, 84–97. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.T.; Mace, T.; Repasky, E.A. Hypoxia-driven immunosuppression: A new reason to use thermal therapy in the treatment of cancer? Int. J. Hyperth. 2010, 26, 232–246. [Google Scholar] [CrossRef]
- Notter, M.; Piazena, H.; Vaupel, P. Hypofractionated re-irradiation of large-sized recurrent breast cancer with thermography-controlled, contact-free water-filtered infrared-A hyperthermia: A retrospective study of 73 patients. Int. J. Hyperth. 2017, 33, 227–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Notter, M.; Thomsen, A.R.; Nitsche, M.; Hermann, R.M.; Wolff, H.; Habl, G.; Münch, K.; Grosu, A.L.; Vaupel, P. Combined wIRA-hyperthermia and hypofractionated re-irradiation in the treatment of locally recurrent breast cancer: Evaluation of thera-peutic outcome based on a novel size classification. Cancers 2020, 12, 606. [Google Scholar] [CrossRef] [Green Version]
- Vaupel, P.; Piazena, H.; Müller, W.; Notter, M. Biophysical and photobiological basics of water-filtered infrared-A hyperthermia of superficial tumors. Int. J. Hyperth. 2018, 35, 26–36. [Google Scholar] [CrossRef] [Green Version]
- Stutz, E.; Puric, E.; Datta, N.; Bodis, S.; Notter, M. Strahlenassoziiertes Angiosarkom der Brust: Was können wir aus Fallberichten lernen? Info Onkol. Hämatol. 2017, 5, 4. (In German) [Google Scholar]
- Feinberg, L.; Srinivasan, A.; Singh, J.K.; Parry, M.; Stevenson, J.; Jeys, L.; Grimer, R.; Peart, F.; Warner, R.; Ford, S.; et al. Impact of specialist management on survival from radiation-associated angiosarcoma of the breast. Br. J. Surg. 2018, 105, 401–409. [Google Scholar] [CrossRef]
- Lehnhardt, M.; Bohm, J.; Hirsch, T.; Behr, B.; Daigeler, A.; Harati, K. Strahlen-induzierte Angiosarkome der Brust [Radiation-induced angiosarcoma of the breast]. Handchir. Mikrochir. Plast. Chir. 2017, 49, 103–110. (In German) [Google Scholar] [CrossRef]
- Wiebringhaus, P.; Gröger, A.; Menke, H. Das sekundäre Angiosarkom der Brust nach brusterhaltender Therapie [Secondary angiosarcoma of the breast after breast-conserving therapy]. Handchir. Mikrochir. Plast. Chir. 2015, 47, 134–138. (In German) [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Wang, J.; He, C.; Fang, M. Angiosarcoma: A review of diagnosis and current treatment. Am. J. Cancer Res. 2019, 9, 2303–2313. [Google Scholar] [PubMed]
- Hasan, S.; Metzger, A.; Wegner, R.; Verma, V.; Hilton, C.; Julian, T.; Trombetta, M. Management trends and outcomes of breast angiosarcoma: Is breast conservation feasible? Breast J. 2019, 25, 1230–1234. [Google Scholar] [CrossRef]
- Donovan, E.K.; Corbett, T.; Vansantvoort, J.; Kak, I.; Popvic, S.; Heller, B. Radical chest wall resection and hyperfractionated accelerated radiotherapy for radiation-associated angiosarcoma of the breast: A safe and effective treatment strategy. Breast J. 2017, 24, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Molitoris, J.K.; Chhabra, A.; Snider, J.W.; Harvilla, N.; Okonkwo, N.; Nichols, E.M.; Vujaskovic, Z.; Ioffe, O.B.; Kesmodel, S.B.; Feigenberg, S.J. Intensification of treatment for angiosarcoma of the breast with accelerated hyperfractionated radiation, hyperthermia, and surgical resection. Cureus 2017, 9, e1406. [Google Scholar] [CrossRef] [Green Version]
- Giotopoulos, G.; Symonds, R.P.; Foweraker, K.; Griffin, M.; Peat, I.; Osman, A.; Plumb, M. The late radiotherapy normal tissue injury phenotypes of telangiectasia, fibrosis and atrophy in breast cancer patients have distinct genotype-dependent causes. Br. J. Cancer 2007, 96, 1001–1007. [Google Scholar] [CrossRef]
- Fodor, J.; Orosz, Z.; Szabó, E.; Sulyok, Z.; Polgár, C.; Zaka, Z.; Major, T. Angiosarcoma after conservation treatment for breast carcinoma: Our experience and a review of the literature. J. Am. Acad. Dermatol. 2006, 54, 499–504. [Google Scholar] [CrossRef]
- Brenn, T.; Fletcher, C.D.M. Radiation-associated cutaneous atypical vascular lesions and angiosarcoma: Clinicopathologic ana-lysis of 42 cases. Am. J. Surg. Pathol. 2005, 29, 983–996. [Google Scholar] [CrossRef]
- Brenn, T.; Fletcher, C.D.M. Postradiation vascular proliferations: An increasing problem. Histopathology 2006, 48, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Ashack, K.A.; Kuritza, V.; Visconti, M.J.; Ashack, L. Dermatologic sequelae associated with radiation therapy. Am. J. Clin. Dermatol. 2020, 21, 541–555. [Google Scholar] [CrossRef] [PubMed]
- Watt, T.C.; Inskip, P.D.; Stratton, K.; Smith, S.A.; Kry, S.; Sigurdson, A.J.; Stovall, M.; Leisenring, W.; Robison, L.L.; Mertens, A.C. Radiation-related risk of basal cell carcinoma: A report from the Childhood Cancer Survivor Study. J. Natl. Cancer Inst. 2012, 104, 1240–1250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banks, J.; George, J.; Potter, S.; Gardiner, M.D.; Ives, C.; Shaaban, A.M.; Singh, J.; Sherriff, J.; Hallissey, M.T.; Horgan, K.; et al. Breast Angiosarcoma Surveillance Study: UK national audit of management and outcomes of angiosarcoma of the breast and chest wall. Br. J. Surg. 2021, 108, 388–394. [Google Scholar] [CrossRef]
| Patient No. 1 | Patient No. 2 | Patient No. 3 | Patient No. 4 | Patient No. 5 | Patient No. 6 | Patient No. 7 | Patient No. 8 | Patient No. 9 | Patient No. 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age at Dx | 68 | 59 | 73 | 75 | 59 | 62 | 71 | 73 | 69 | 72 |
| BC-Stage | T1N0M0 | T1N0M0 | T1N0M0 | T1N0M0 | T1N0M0 | T2N0M0 | T2N2aM0 | T1N0M0 | T2N0M0 | T1N0M0 |
| Grade | G2 | G2 | G1 | G2 | G2 | G2 | G2 | G2 | G2 | G3 |
| BC-Tx | BCS + RT + H | BCS + RT + H | BCS + RT + H | BCS + RT + H | BCS + RT + H | BCS + RT + H | BCS + RT + CT + H | BCS + RT + H | BCS + RT + H | BCS + RT + H |
| RT Breast (Gy) | 25 × 2 | 28 × 1.8 * | 25 × 2 | 25 × 2 | 21 × 1.8 ** + 6 × 2.2 | 25 × 2 | 28 × 1.8 | 25 × 2 | 28 × 1.8 | 25 × 2 |
| RT-Tech-nique | Photons 6/15 MV | Photons 6 MV | 60Co | Photons 6 MV | Photons 6 MV | Photons 6 MV | Photons 6 MV | Photons 6 MV | Photons 6 MV | Photons 6 MV |
| Boost (Gy) | 8 × 2 | Ø | 5 × 2 | 5 × 2 | 5 × 2.5 | 5 × 2 | 5 × 2 | 5 × 2.5 | 8 × 2 | 8 × 2 |
| Type of Boost | Photons 15 MV | Ø | e− 9 MeV | e− 9 MeV | Photons 6 MV | e− 9 MeV | e− 9MeV | e− 9 MeV | e− 12 MeV | e− 9 MeV |
| Patient No. 1 | Patient No. 2 | Patient No. 3 | Patient No. 4 | Patient No. 5 | Patient No. 6 | Patient No. 7 | Patient No. 8 | Patient No. 9 | Patient No. 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age at RAASB Dx | 73 | 63 | 80 | 80 | 71 | 68 | 78 | 80 | 74 | 86 |
| Latency BC-TTx to Dx of RAASB (y) | 5 | 4 | 7 | 4.5 | 12 | 6 | 7 | 6 | 7 | 14 |
| Initial RAASB Diameter (10 cm) | >10 | <10 | <10 | <10 | <10 | <10 | <10 | >10 | >10 | >10 |
| Grading | 3 | 3 | 2 | 3 | 3 | 2 | 3 | 3 | 3 | 3 |
| Skin Type | II | I | II | II | II | II | I | I | I | I |
| Hair | brown | red | brown | fair | brown | brown | fair | fair | fair | fair |
| Benign Skin Alterations | Verrucae seniles | Lentigo solaris | Ruby points | Ruby points | Lentigo solaris | Ruby points | Ruby points | Ruby points | Lentigo solaris | |
| RT-related Skin Alteration | Teleangi-ectases | Teleangi-ectases | Teleangi-ectases | Fibrosis lymph-edema | Fibrosis lymph-edema |
| Patient No. 1 | Patient No. 2 | Patient No. 3 | Patient No. 4 | Patient No. 5 | Patient No. 6 | Patient No. 7 | Patient No. 8 | Patient No. 9 | Patient No. 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Group | A | A | B | B | B | C | C | D | D | D |
| Surgery 1st RAASB | TM | TM | TM | TM | Resect | TM | TM | TM | TM | TM |
| R status 1st Surg | R2 | R0 | R0 | R0 | R0 | R0 | R0 | R0 | R0 | R0 |
| Latency to local recurrence | - | - | 8 months | 10 months | 52 months | 4 weeks | 3 weeks | 1st: 4 months 2nd: 2 months 3rd: 3 months | 3 months | 14 months |
| RAASB-recurrence: surgery | - | - | Resect. (mesh graft) | Resect. (mesh graft) | Mast. | Ø | Ø | 1st: resect 2nd: resect 3rd: inop. | Non-resectable | Non-resectable |
| R status 2nd surgery | - | - | R1 | R1 | R0 | - | - | 1st: R0 2nd: R1 | - | - |
| Chemotherapy | Ø | Ø | 2× | Ø | Ø | Ø | * | 7× | Ø | Ø |
| Tumor extension | II | I | II | II | I | IIIa | IIIa | IIIb | IVb | IIIa |
| HT/re-RT 1st course | 5 × 4 Gy 1×/w | 5 × 4 Gy 1×/w | 5 × 4 Gy 1×/w | 5 × 4 Gy 1×/w | 5 × 4 Gy 1×/w | 5 × 4 Gy 1×/w | 5 × 4 Gy 1×/w | 5 × 4 Gy 1×/w + 2 × 4 Gy | 5 × 4 Gy 1×/w | 25 × 2 Gy + 5 × 2 Gy |
| Response 1st course | - | - | - | - | - | CR | CR | PD | PR | CR |
| Repeated HT/re-RT | - | - | 1× | 3× | - | - | - | - | - | - |
| Response repeated HT/re-HT | - | - | CR | 3 × CR | - | - | - | - | - | - |
| Time to local progression (mts) | - | - | 6 | 3 | - | - | - | 0 (PD) | 1 | - |
| Survival (mts) | 67 | 37 | 20 | 45 | 10 | 16 | 1 | 1 | 7 | 18 |
| Status | LFU | Living, NED | Dead | Living, SD | Living, NED | Living, NED | Living, NED | Dead | Dead | Living, NED |
| Patient No. 1 | Patient No. 2 | Patient No. 3 | Patient No. 4 | Patient No. 5 | Patient No. 6 | Patient No. 7 | Patient No. 8 | Patient No. 9 | Patient No. 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Acute side effects | ||||||||||
| Erythema | G1 | G1 | G1 | - | G1 | G1 | G1 | - | - | G1 |
| Hyper-pigmentation | - | G1 | G1 | - | G1 | G1 | - | G1 | G1 | - |
| Chronic side effects | ||||||||||
| Induration | - | - | - | - | - | - | - | - | - | - |
| Hyper-pigmentation | - | - | - | G1 | - | - | - | - | - | G1 |
| New telangiectases | - | - | - | G1 * | - | - | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Notter, M.; Stutz, E.; Thomsen, A.R.; Vaupel, P. Radiation-Associated Angiosarcoma of the Breast and Chest Wall Treated with Thermography-Controlled, Contactless wIRA-Hyperthermia and Hypofractionated Re-Irradiation. Cancers 2021, 13, 3911. https://doi.org/10.3390/cancers13153911
Notter M, Stutz E, Thomsen AR, Vaupel P. Radiation-Associated Angiosarcoma of the Breast and Chest Wall Treated with Thermography-Controlled, Contactless wIRA-Hyperthermia and Hypofractionated Re-Irradiation. Cancers. 2021; 13(15):3911. https://doi.org/10.3390/cancers13153911
Chicago/Turabian StyleNotter, Markus, Emanuel Stutz, Andreas R. Thomsen, and Peter Vaupel. 2021. "Radiation-Associated Angiosarcoma of the Breast and Chest Wall Treated with Thermography-Controlled, Contactless wIRA-Hyperthermia and Hypofractionated Re-Irradiation" Cancers 13, no. 15: 3911. https://doi.org/10.3390/cancers13153911
APA StyleNotter, M., Stutz, E., Thomsen, A. R., & Vaupel, P. (2021). Radiation-Associated Angiosarcoma of the Breast and Chest Wall Treated with Thermography-Controlled, Contactless wIRA-Hyperthermia and Hypofractionated Re-Irradiation. Cancers, 13(15), 3911. https://doi.org/10.3390/cancers13153911






