‘I Didn’t Even Recognise Myself’: Survivors’ Experiences of Altered Appearance and Body Image Distress during and after Treatment for Head and Neck Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Procedure
2.4. Data Analysis
2.5. Rigour
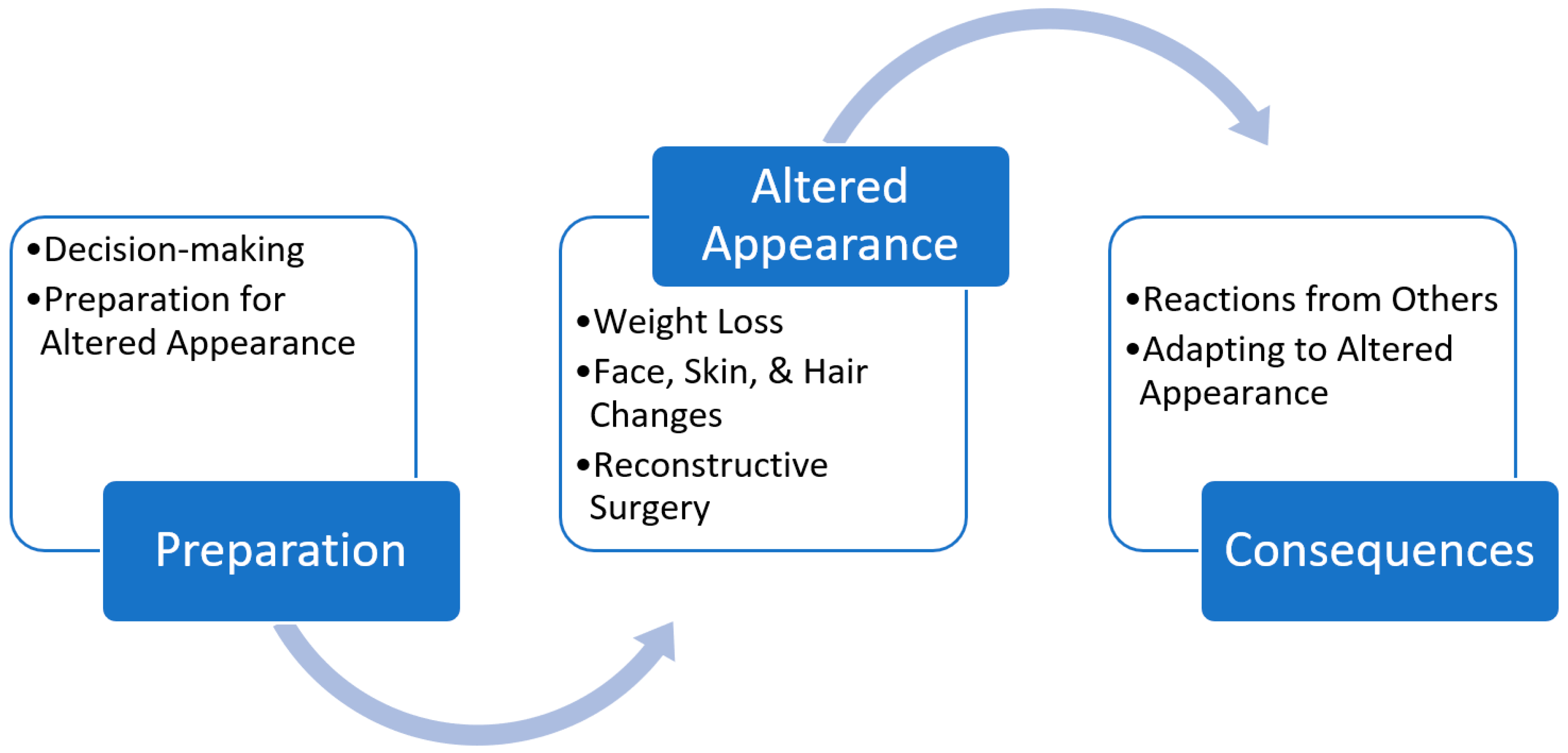
3. Results
3.1. Preparation
3.1.1. Decision-making
3.1.2. Preparation for Altered Appearance
‘I heard they were cutting out every part of the upper part of my mouth and they would replace that with parts of my leg, and it was beyond my understanding that they could do that inside my mouth. I felt so confronted and I was starting to shake, and I was getting pins and needles, so my husband just took me for a little walk up the corridor and back, and I had some water. I was dealing with the visceral shock of my mouth being invaded.’PID13
‘There was no preparation, they just said about the treatment and of course I wasn’t expecting it to be as uncomfortable as it was the first time.’
‘They told me I would lose my teeth, but he did say they were going to save the eye. This eye was not able to be saved though as complications arose.’PID17
‘I Googled some things that they just said that I was going to have done and you’d only have to look at one picture and you just freak and turn it off.’PID16
‘I had to meet the prosthodontist for him to take extremely careful views of what my smile looked like at the time-so in other words, get the look of what (participant’s name) is before we do this to her.’PID13
‘I had no idea whatever about what I was going to look like… and I felt vulnerable in anticipation of that.’PID13
3.2. Altered Appearance
‘I didn’t even recognise myself. I didn’t even know who I was. I looked in the mirror and I didn’t even see myself. That’s how different I was.’ PID20, while others avoided or delayed looking at the results of surgery, ‘it took me about two weeks to actually have a look at where my nose was.’PID7
‘I often said to them, “Look, I understand there’s people that you could be operating on who’ve got critical cancer and this is really all cosmetic,” but I was offered the world and then suddenly it all filters back down to zero.’PID17
3.2.1. Weight Loss
‘I’ve got dry mouth, I’ve got thick saliva, I‘ve got occasional pain in my throat similar to after the tonsillectomy-type pain, feels like scabs are there… I lost maybe 10 kg in a week.’PID11
‘They kept giving me injections for nausea… but I couldn’t eat; I didn’t want to eat’.PID16
‘I think (it) is ironic because all my life I’ve been told to lose weight–but there’s this huge focus on keeping your weight up, because if you don’t there are all sorts of things that can go wrong like your mask won’t fit properly and the treatment won’t work as well.’PID10
‘I’ve gone from 120 kilos to 79 kilos. I look like a skin and bone man…my face was so withdrawn, I was like a skeleton…I have to sit down in the shower now and I’m looking at my legs going, “Jesus Christ, there’s nothing there.”.’PID20
‘I’m only a small build so I looked like something out of a concentration camp.’PID16
‘When I went to treatment I was 60 kilos and when I finished my treatment, I was 38 kilos.’PID8
‘I might have lost two or three kilos during treatment, but the big weight loss was when the mucositis comes in and your membranes are all so sore, you can’t swallow, you can’t eat, you can’t sleep. I lost 20 kgs.’PID3
3.2.2. Face, Skin, and Hair Changes
‘It was like somebody taking a blowtorch and just burnt…all my neck and my face.’PID17
‘Pretty uncomfortable really. I couldn’t go visiting. I went to my daughter’s on Tuesday. I was there about half an hour, and I had to come home. I just couldn’t talk; I was tired. And I wanted to take my shirt off.’
‘I’ve lost my eyebrows, but they’re starting to come back. My eyelashes, I’ve lost them, but my facial hair now comes back a lot darker.’PID7
‘I looked like I had 10 chins and he (doctor) said, “That’s just where everything’s been attacked and nuked. It’ll gradually go down.”‘PID18
‘Particularly the last couple of weeks, was quite horrible because it was that cooked and a lot of temperature and a lot of blistering on the neck.’
‘I got this pretty much straight after the radiation; it started deteriorating my jaw. (It took) five years all up before the jaw actually broke...the jawbone just got so infected and broke and my face was out like a balloon.’PID16
3.2.3. Reconstructive Surgery
‘The fact that the skin that’s where my teeth are now, is from my leg, means I get hair there sometimes.’
‘(they used) my stomach muscles. That was quite a good palate, it really hung tight actually and then they put a bit of scapula with a bit of bone in, in the muscle…they thought they’d be able to screw teeth into that possibly… that failed after a week so then they went in and put some muscle out of my thigh in there and luckily that took okay.’
‘That’s about a two hour operation, but unfortunately, because it’s not life-threatening, I have to go on the waiting list.’PID7
‘They took the jaw from there down to here somewhere and then they took the tibia bone out of my leg and put it in there and then they put a chain, like a bicycle chain-type thing around there for it to heal, but they also had to cut this side of my neck as well to bring all the blood vessels and nerve endings and everything over to this side because radiation had actually killed everything on this side of the face.‘
‘I find it really hard at the moment walking because where they took the bone out of the leg that seems to be more of a problem than the neck and they said that would happen, where they take skin and bone and things is normally the last to heal.’PID16
3.3. Consequences
‘People say they don’t notice it, but I do and I hate it more than anything’.PID8
3.3.1. Reactions from Others
‘I haven’t got good self-esteem. To go out, I’m very conscious of people watching me, looking at me. Before you used to look [at] somebody and you’d make eye contact with somebody, that’s fine, but now it’s eye contact then their contact goes to your face, your neck, and I’m quite aware of it.’PID16
‘Bad enough people stare at me already because I look like some kind of anorexic walking around…I said, “I’ve just had radiation and chemo for cancer. I actually can’t eat anything.’PID8
‘For a whole year in this house I never went out… It all started with a family dinner. When I walked in one of the men said, “Oh my God, (name), you’re so skinny. You really need to put on some weight.” And that started something for me….I was devastated.’PID6
‘I’d have people walk up talking to like me and (partner), family friends walk up and start talking, they were talking to her, and they were sort of looking at me and looking away. They didn’t even know who I was. And then (partner) would go, “Aren’t you going to say hello to (participant’s name)?” and they were like, “Oh.” Nobody knew what to say to me.’PID20
‘I didn’t see what I looked like, but nobody recognised me–my face was out here and it was green and (daughter) wouldn’t believe (partner) when she said, “That’s your dad there.” “No, that’s not Dad.” And my mother-in-law came. She took one look and went outside and burst out crying.’PID17
‘You can understand these people that–you’ve got a married couple whatever and then she’ll just go or he’ll go because– it’s a nightmare for them… sometimes my wife would come to the hospital and I’d see her change colour; she’d just go white and have to go outside.’
‘I went out a couple of times, but I felt uncomfortable because people were really staring at you because it was white, it stood out.’
‘I said, “That’s really good, but it’s too new.” So I went back and said “Can you do some more colouring into it and put a bit other stuff in,” which he did.’
‘They’d pick up the phone and ring you, but they don’t actually come and see you.’
3.3.2. Adapting to Altered Appearance
‘Intellectually and I think in my heart now I see that it would be ridiculous. I’ve already had three 12 h-plus operations on this side of my face and, it’s not like I’m 25.’
‘A lot of people, friends, even women friends, have said, “You’re still the same person. It doesn’t matter what you look like.”’
‘I think people probably see me differently. They thought I was a tough cookie before, but they probably look at me and say that I’m quite a strong person… People look at me differently so I feel a bit different, although there is that negative thing of how they feel about me, my weight and how I look, but they also know that I have definitely done it tough and I’m okay still.’
‘When I go to my local tavern, people ask me what’s happened? I told the bar staff when I had the plastic on and they were, “Bloody hell, you’re brave coming out like that.” I said, “Well, what do you want me to do?” You can’t sit in the house.’PID7
4. Discussion
4.1. Limitations
4.2. Practice Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Callahan, C. Facial Disfigurement and Sense of Self in Head and Neck Cancer. Soc. Work. Health Care 2005, 40, 73–87. [Google Scholar] [CrossRef]
- Lebel, S.; Devins, G.M. Stigma in cancer patients whose behavior may have contributed to their disease. Futur. Oncol. 2008, 4, 717–733. [Google Scholar] [CrossRef]
- A Neilson, K.; Pollard, A.C.; Boonzaier, A.M.; Corry, J.; Castle, D.J.; Mead, K.R.; Gray, M.C.L.; I Smith, D.; Trauer, T.; Couper, J.W. Psychological distress (depression and anxiety) in people with head and neck cancers. Med. J. Aust. 2010, 193, S48–S51. [Google Scholar] [CrossRef] [PubMed]
- Ichikura, K.; Yamashita, A.; Sugimoto, T.; Kishimoto, S.; Matsushima, E. Persistence of psychological distress and correlated factors among patients with head and neck cancer. Palliat. Support. Care 2015, 14, 42–51. [Google Scholar] [CrossRef]
- Lang, H.; France, E.; Williams, B.; Humphris, G.; Wells, M. The psychological experience of living with head and neck cancer: A systematic review and meta-synthesis. Psychooncology 2013, 22, 2648–2663. [Google Scholar] [CrossRef]
- Furr, L.A.; Wiggins, O.; Cunningham, M.; Vasilic, D.; Brown, C.S.; Banis, J.C.; Maldonado, C.; Perez-Abadia, G.; Barker, J.H. Psychosocial Implications of Disfigurement and the Future of Human Face Transplantation. Plast. Reconstr. Surg. 2007, 120, 559–565. [Google Scholar] [CrossRef]
- Graboyes, E.M.; Maurer, S.; Park, Y.; Bs, C.H.M.; McElligott, J.T.; Day, T.A.; Hornig, J.D.; Sterba, K.R. Evaluation of a novel telemedicine-based intervention to manage body image disturbance in head and neck cancer survivors. Psychooncology 2020, 29, 1988–1994. [Google Scholar] [CrossRef]
- Garzaro, M.; Airoldi, M.; Raimondo, L.; Pecorari, G.; Giordano, C.; Caldera, P.; Varetto, A.; Zanon, C.; Torta, R. Long-term quality of life and psychological response after flap reconstructive surgery and radiotherapy in head and neck cancer patients. J. Clin. Oncol. 2008, 26, 20553. [Google Scholar] [CrossRef]
- Fingeret, M.; Teo, I.; Kagan, S. Facing Disfigurement: Understanding Body Image Adaptation Following Surgical Treatment for Head and Neck Cancer. Psychooncology 2014, 23, 15. [Google Scholar]
- Badr, H.; Herbert, K.; Reckson, B.; Rainey, H.; Sallam, A.; Gupta, V. Unmet needs and relationship challenges of head and neck cancer patients and their spouses. J. Psychosoc. Oncol. 2016, 34, 336–346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lebel, S.; Castonguay, M.; Mackness, G.; Irish, J.; Bezjak, A.; Devins, G.M. The psychosocial impact of stigma in people with head and neck or lung cancer. Psychooncology 2011, 22, 140–152. [Google Scholar] [CrossRef] [PubMed]
- Threader, J.; McCormack, L. Cancer-related trauma, stigma and growth: The ‘lived’ experience of head and neck cancer. Eur. J. Cancer Care 2016, 25, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Wali, I.M.; Regmi, K. People living with facial disfigurement after having had noma disease: A systematic review of the literature. J. Health Psychol. 2017, 22, 1243–1255. [Google Scholar] [CrossRef] [PubMed]
- Yaron, G.; Meershoek, A.; Widdershoven, G.; Brekel, M.V.D.; Slatman, J. Facing a Disruptive Face: Embodiment in the Everyday Experiences of “Disfigured” Individuals. Hum. Stud. 2017, 40, 285–307. [Google Scholar] [CrossRef] [Green Version]
- Clarke, C.; Mccorry, N.K.; Dempster, M. The Role of Identity in Adjustment among Survivors of Oesophageal Cancer. J. Health Psychol. 2011, 16, 99–108. [Google Scholar] [CrossRef] [Green Version]
- Dropkin, M.J. Anxiety, Problem-Focused Coping Strategies, Disfigurement/Dysfunction and Postoperative Coping Behaviors Associated with Head and Neck Cancer. Ph.D. Thesis, New York University, Ann Arbor, MI, USA, 1994. [Google Scholar]
- Rhoten, B.A. Body image disturbance in adults treated for cancer—A concept analysis. J. Adv. Nurs. 2016, 72, 1001–1011. [Google Scholar] [CrossRef]
- Price, B. Altered body image: Managing social encounters. Int. J. Palliat. Nurs. 2000, 6, 179–185. [Google Scholar] [CrossRef]
- Newell, R. Psychological difficulties amongst plastic surgery ex-patients following surgery tothe face: A survey. Br. J. Plast. Surg. 2000, 53, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Relic, A.; Mazemda, P.; Arens, C.; Koller, M.; Glanz, H. Investigating quality of life and coping resources after laryngectomy. Eur. Arch. Oto-Rhino-Laryngol. 2001, 258, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Rennie, C.; Stoddart, K.M.; Hubbard, G. A new normal: Reconciling change in appearance and function for men with head and neck cancer. Cancer Nurs. Pract. 2018, 17, 20–28. [Google Scholar] [CrossRef]
- Norman, A.; Moss, T.P. Psychosocial interventions for adults with visible differences: A systematic review. PeerJ 2015, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Semple, C.; Dunwoody, L.; Sullivan, K.; Kernohan, W.; Kernohan, G. Patients with head and neck cancer prefer individualized cognitive behavioural therapy. Eur. J. Cancer Care 2006, 15, 220–227. [Google Scholar] [CrossRef]
- Semple, C.J.; Sullivan, K.; Dunwoody, L.; Kernohan, W.G. Psychosocial Interventions for Patients with Head and Neck Cancer. Cancer Nurs. 2004, 27, 434–441. [Google Scholar] [CrossRef]
- Allison, P.; Edgar, L.; Nicolau, B.; Archer, J.; Black, M.; Hier, M. Results of a feasibility study for a psycho-educational intervention in head and neck cancer. Psychooncology 2004, 13, 482–485. [Google Scholar] [CrossRef] [PubMed]
- Luckett, T.; Britton, B.; Clover, K.; Rankin, N.M. Evidence for interventions to improve psychological outcomes in people with head and neck cancer: A systematic review of the literature. Support. Care Cancer 2011, 19, 871–881. [Google Scholar] [CrossRef]
- Malik, N.H.; Maganti, M.; McQuestion, M.; Tjong, M.C.; Keilty, D.; Monteiro, E.; Huang, S.H.; Jang, R.W.-J.; Gomes, A.; Pun, J.; et al. Pre-treatment psychoeducational intervention and outcomes in head and neck cancer patients undergoing radiotherapy. Support. Care Cancer 2021, 29, 1643–1652. [Google Scholar] [CrossRef]
- Rifkin, W.; David, J.A.; Plana, N.M.; Kantar, R.S.; Diaz-Siso, J.R.; Gelb, B.; Ceradini, D.J.; Rodriguez, E.D. Achievements and Challenges in Facial Transplantation. Ann. Surg. 2018, 268, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Gibson, C.; O’Connor, M.; White, R.; Baxi, S.; Halkett, G. Burnout or Fade Away; experiences of health professionals caring for patients with head and neck cancer. Eur. J. Oncol. Nurs. 2021, 50, 101881. [Google Scholar] [CrossRef]
- Given, L.M. SAGE Encyclopedia of Qualitative Research Methods; Sage Publications: London, UK, 2008; p. 868. [Google Scholar]
- Clarke, V.; Braun, V. Thematic analysis. J. Posit. Psychol. 2017, 12, 297–298. [Google Scholar] [CrossRef]
- Strauss, A.L. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory/Anselm Strauss, Juliet Corbin, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Lincoln, Y.S. Naturalistic Inquiry; Lincoln, Y.S., Guba, E.G., Eds.; Sage Publications: Beverly Hills, CA, USA, 1985. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rinkel, R.; Leeuw, I.M.V.-D.; Doornaert, P.; Buter, J.; De Bree, R.; Langendijk, J.A.; Aaronson, N.K.; Leemans, C.R. Prevalence of swallowing and speech problems in daily life after chemoradiation for head and neck cancer based on cut-off scores of the patient-reported outcome measures SWAL-QOL and SHI. Eur. Arch. Oto-Rhino-Laryngol. 2015, 273, 1849–1855. [Google Scholar] [CrossRef]
- Glassey, R.; Hardcastle, S.J.; O’Connor, M.; Ives, A.; Investigators, K.; Saunders, C. Perceived influence of psychological consultation on psychological well-being, body image, and intimacy following bilateral prophylactic mastectomy: A qualitative analysis. Psychooncology 2018, 27, 633–639. [Google Scholar] [CrossRef]
- Ozsoy, S.; Beşirli, A.; Unal, D.; Abdulrezzak, U.; Orhan, O. The association between depression, weight loss and leptin/ghrelin levels in male patients with head and neck cancer undergoing radiotherapy. Gen. Hosp. Psychiatry 2015, 37, 31–35. [Google Scholar] [CrossRef]
- Rhondali, W.; Chisholm, G.B.; Daneshmand, M.; Allo, J.; Kang, D.-H.; Filbet, M.; Hui, D.; Fingeret, M.C.; Bruera, E. Association Between Body Image Dissatisfaction and Weight Loss Among Patients With Advanced Cancer and Their Caregivers: A Preliminary Report. J. Pain Symptom Manag. 2013, 45, 1039–1049. [Google Scholar] [CrossRef]
- Fingeret, M.C.; Nipomnick, S.; Guindani, M.; Baumann, N.; Hanasono, M.; Crosby, M. Body image screening for cancer patients undergoing reconstructive surgery. Psychooncology 2014, 23, 898–905. [Google Scholar] [CrossRef] [Green Version]
- Brodsky, L. Identity change as a consequence of oral surgery. Aesthetic Plast. Surg. 1978, 2, 303–310. [Google Scholar] [CrossRef]
- Furness, P.J. Exploring supportive care needs and experiences of facial surgery patients. Br. J. Nurs. 2005, 14, 641–645. [Google Scholar] [CrossRef]
- Newell, R.J. Altered body image: A fear-avoidance model of psycho-social difficulties following disfigurement. J. Adv. Nurs. 1999, 30, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Fingeret, M.C.; Teo, I.; Goettsch, K. Body Image: A Critical Psychosocial Issue for Patients with Head and Neck Cancer. Curr. Oncol. Rep. 2014, 17, 422. [Google Scholar] [CrossRef] [PubMed]
- McCormick, M. Facing disfigurement. Nurs. N. Z. 1995, 1, 13–15. [Google Scholar] [PubMed]
- Clarke, A. Psychosocial aspects of facial disfigurement: Problems, management and the role of a lay-led organization. Psychol. Health Med. 1999, 4, 127–142. [Google Scholar] [CrossRef]
- Chen, S.-C.; Huang, B.-S.; Lin, C.-Y.; Fan, K.-H.; Chang, J.T.-C.; Wu, S.-C.; Lai, Y.-H. Psychosocial effects of a skin camouflage program in female survivors with head and neck cancer: A randomized controlled trial. Psychooncology 2016, 26, 1376–1383. [Google Scholar] [CrossRef]
- Freysteinson, W.M. Demystifying the mirror taboo: A neurocognitive model of viewing self in the mirror. Nurs. Inq. 2020, 27, e12351. [Google Scholar] [CrossRef]
- Porges, S.W. The polyvagal perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef] [PubMed]
- Wood, S.; I Bisson, J. Experience of incorporating a mental health service into patient care after operations for cancers of the head and neck. Br. J. Oral Maxillofac. Surg. 2004, 42, 149–154. [Google Scholar] [CrossRef]
- Feber, T.; Cost, S.; Hoole, J.; Davis, R. Definitely not for the squeamish: Head and neck cancer is a relatively rare disease that most nursing teams never come across, therefore it requires a high level of specialist knowledge, says Tricia Feber and colleagues. Cancer Nurs. Pract. 2006, 12, 12. [Google Scholar] [CrossRef]
- Bennett, J.A.; Cameron, L.D.; Whitehead, L.C.; Porter, D. Differences between Older and Younger Cancer Survivors in Seeking Cancer Information and Using Complementary/Alternative Medicine. J. Gen. Intern. Med. 2009, 24, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Halkett, G.K.; Golding, R.M.; Langbecker, D.; White, R.; Jackson, M.; Kernutt, E.; O’Connor, M. From the carer’s mouth: A phenomenological exploration of carer experiences with head and neck cancer patients. Psychooncology 2020, 29, 1695–1703. [Google Scholar] [CrossRef]
- Hopwood, P.; Fletcher, I.; Lee, A.; Al Ghazal, S. A body image scale for use with cancer patients. Eur. J. Cancer 2001, 37, 189–197. [Google Scholar] [CrossRef]
- Carr, T.; Moss, T.; Harris, D. The DAS24: A short form of the Derriford Appearance Scale DAS59 to measure individual responses to living with problems of appearance. Br. J. Health Psychol. 2005, 10, 285–298. [Google Scholar] [CrossRef]
- Sundaram, C.S.; Dhillon, H.M.; Butow, P.N.; Sundaresan, P.; Rutherford, C. A systematic review of body image measures for people diagnosed with head and neck cancer (HNC). Support. Care Cancer 2019, 27, 3657–3666. [Google Scholar] [CrossRef] [PubMed]
| Age | Min 34, Max 79 | Mean 64 years | SD 10.75 |
| Gender | Males 15 | Females 6 | Other 0 |
| Time since diagnosis | Min 60 days, Max 1827 days | Mean 646 days or ~21.5 months | SD 713.00 |
| Diagnosis | HPV (P16+) | Non-HPV | Unknown |
| 47% 10/21 | 33% 7/21 | 19% 4/21 | |
| Treatment Received | Surgery | Radiation therapy | Chemotherapy |
| 43% 13/21 | 95% 20/21 | 76% 16/21 | |
| Race | Caucasian | Aboriginal | Other |
| 95% 20/21 | 5% 1/21 | 0 | |
| Education Level | Less than school grad | School Grad | Beyond Year 12 qualification |
| 33% 7/21 | 24% 6/21 | 38% 8/21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gibson, C.; O’Connor, M.; White, R.; Jackson, M.; Baxi, S.; Halkett, G.K.B. ‘I Didn’t Even Recognise Myself’: Survivors’ Experiences of Altered Appearance and Body Image Distress during and after Treatment for Head and Neck Cancer. Cancers 2021, 13, 3893. https://doi.org/10.3390/cancers13153893
Gibson C, O’Connor M, White R, Jackson M, Baxi S, Halkett GKB. ‘I Didn’t Even Recognise Myself’: Survivors’ Experiences of Altered Appearance and Body Image Distress during and after Treatment for Head and Neck Cancer. Cancers. 2021; 13(15):3893. https://doi.org/10.3390/cancers13153893
Chicago/Turabian StyleGibson, Chandrika, Moira O’Connor, Rohen White, Melanie Jackson, Siddhartha Baxi, and Georgia K. B. Halkett. 2021. "‘I Didn’t Even Recognise Myself’: Survivors’ Experiences of Altered Appearance and Body Image Distress during and after Treatment for Head and Neck Cancer" Cancers 13, no. 15: 3893. https://doi.org/10.3390/cancers13153893
APA StyleGibson, C., O’Connor, M., White, R., Jackson, M., Baxi, S., & Halkett, G. K. B. (2021). ‘I Didn’t Even Recognise Myself’: Survivors’ Experiences of Altered Appearance and Body Image Distress during and after Treatment for Head and Neck Cancer. Cancers, 13(15), 3893. https://doi.org/10.3390/cancers13153893






