Etiology and Outcomes of Hepatocellular Carcinoma in an Ethnically Diverse Population: The Multiethnic Cohort
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. HCC Identification and Tumor Characteristics
2.3. Statistical Analysis
3. Results
3.1. Cohort Characteristics by Race/Ethnicity
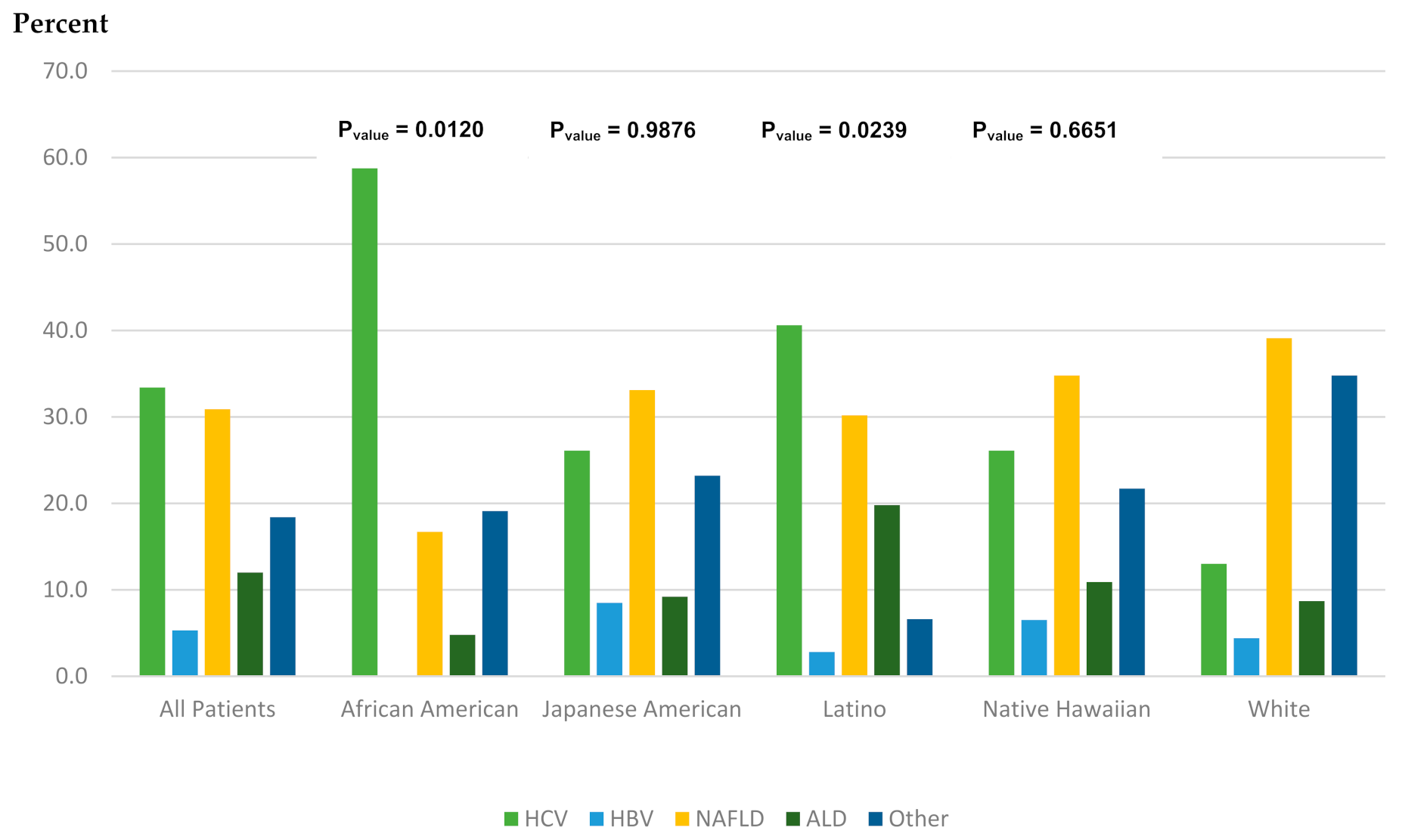
3.2. HCC Characteristics and Underlying Etiology by Race/Ethnicity
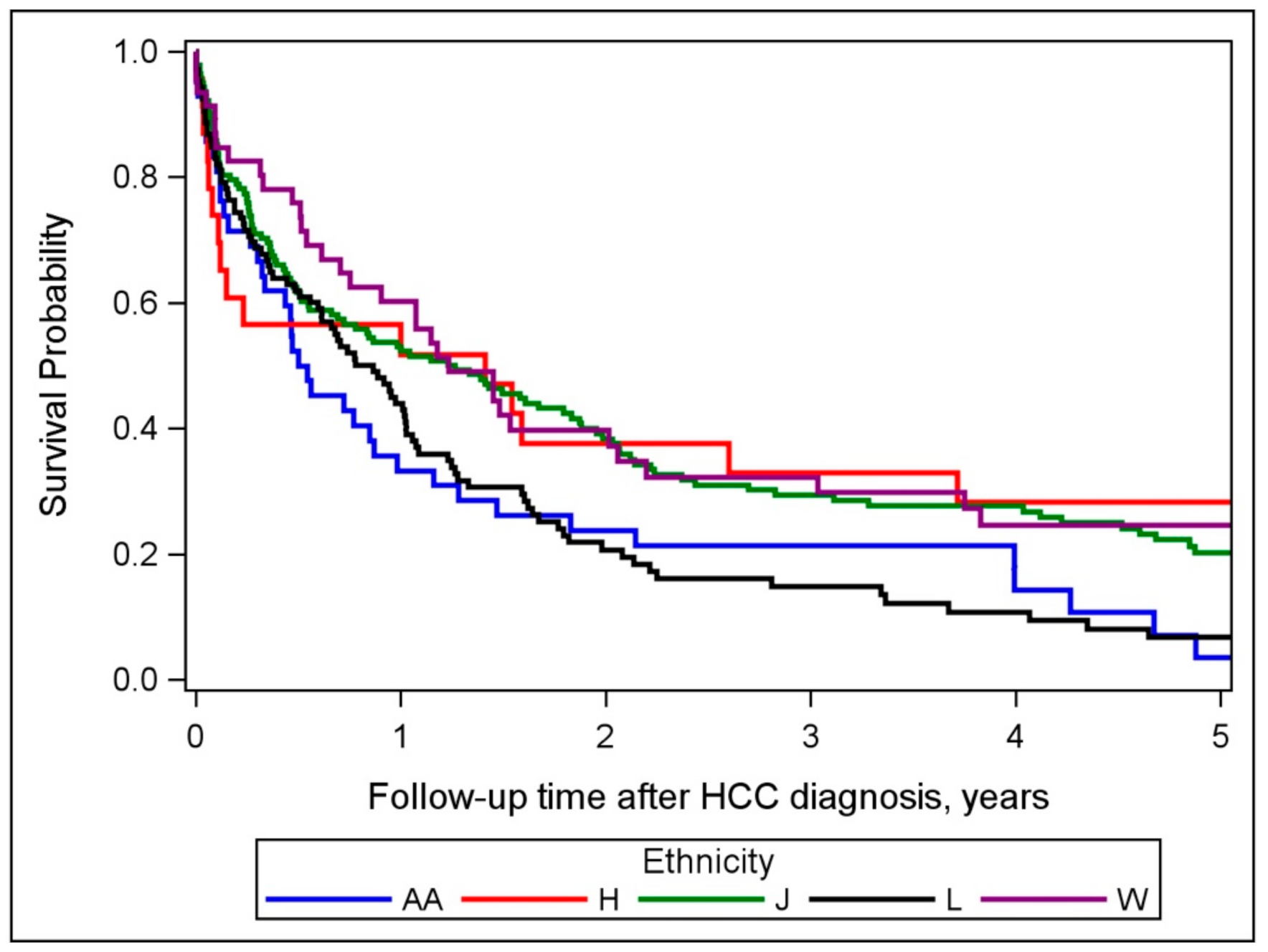
3.3. Relationship between Race/Ethnicity, Risk Factor, and Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akinyemiju, T.; Abera, S.; Ahmed, M.; Alam, N.; Alemayohu, M.A.; Allen, C.; Al-Raddadi, R.; Alvis-Guzman, N.; Amoako, Y.; Global Burden of Disease Liver Cancer Collaboration; et al. The Burden of Primary Liver Cancer and Underlying Etiologies From 1990 to 2015 at the Global, Regional, and National Level: Results From the Global Burden of Disease Study 2015. JAMA Oncol. 2017, 3, 1683–1691. [Google Scholar] [CrossRef] [PubMed]
- Hashim, D.; Boffetta, P.; La Vecchia, C.; Rota, M.; Bertuccio, P.; Malvezzi, M.; Negri, E. The global decrease in cancer mortality: Trends and disparities. Ann. Oncol. 2016, 27, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Pham, C.; Fong, T.L.; Zhang, J.; Liu, L. Striking Racial/Ethnic Disparities in Liver Cancer Incidence Rates and Temporal Trends in California, 1988–2012. J. Natl. Cancer Inst. 2018, 110, 1259–1269. [Google Scholar] [CrossRef] [PubMed]
- Ryerson, A.B.; Eheman, C.R.; Altekruse, S.F.; Ward, J.W.; Jemal, A.; Sherman, R.L.; Henley, S.J.; Holtzman, D.; Lake, A.; Noone, A.M.; et al. Annual Report to the Nation on the Status of Cancer, 1975–2012, featuring the increasing incidence of liver cancer. Cancer 2016, 122, 1312–1337. [Google Scholar] [CrossRef] [PubMed]
- Tapper, E.B.; Parikh, N.D. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: Observational study. BMJ 2018, 362, k2817. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.L.; Kwong, S.L.; Bowlus, C.L.; Nguyen, T.T.; Maxwell, A.E.; Bastani, R.; Chak, E.W.; Chen, M.S., Jr. Racial/ethnic disparities in hepatocellular carcinoma treatment and survival in California, 1988-2012. World J. Gastroenterol. 2016, 22, 8584–8595. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Liu, J.B.; So, S.K.; Han, S.S.; Wang, S.S.; Hertz, A.; Shariff-Marco, S.; Lin Gomez, S.; Rosenberg, P.S.; Nguyen, M.H.; et al. Disparities in hepatocellular carcinoma incidence by race/ethnicity and geographic area in California: Implications for prevention. Cancer 2018, 124, 3551–3559. [Google Scholar] [CrossRef] [PubMed]
- Setiawan, V.W.; Hernandez, B.Y.; Lu, S.C.; Stram, D.O.; Wilkens, L.R.; Le Marchand, L.; Henderson, B.E. Diabetes and racial/ethnic differences in hepatocellular carcinoma risk: The multiethnic cohort. J. Natl. Cancer Inst. 2014, 106. [Google Scholar] [CrossRef] [PubMed]
- Kolonel, L.N.; Henderson, B.E.; Hankin, J.H.; Nomura, A.M.; Wilkens, L.R.; Pike, M.C.; Stram, D.O.; Monroe, K.R.; Earle, M.E.; Nagamine, F.S. A multiethnic cohort in Hawaii and Los Angeles: Baseline characteristics. Am. J. Epidemiol. 2000, 151, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Artinyan, A.; Mailey, B.; Sanchez-Luege, N.; Khalili, J.; Sun, C.L.; Bhatia, S.; Wagman, L.D.; Nissen, N.; Colquhoun, S.D.; Kim, J. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer 2010, 116, 1367–1377. [Google Scholar] [CrossRef]
- Mathur, A.K.; Osborne, N.H.; Lynch, R.J.; Ghaferi, A.A.; Dimick, J.B.; Sonnenday, C.J. Racial/ethnic disparities in access to care and survival for patients with early-stage hepatocellular carcinoma. Arch. Surg. 2010, 145, 1158–1163. [Google Scholar] [CrossRef]
- Rich, N.E.; Hester, C.; Odewole, M.; Murphy, C.C.; Parikh, N.D.; Marrero, J.A.; Yopp, A.C.; Singal, A.G. Racial and Ethnic Differences in Presentation and Outcomes of Hepatocellular Carcinoma. Clin. Gastroenterol. Hepatol. 2019, 17, 551–559. [Google Scholar] [CrossRef]
- Jones, P.D.; Diaz, C.; Wang, D.; Gonzalez-Diaz, J.; Martin, P.; Kobetz, E. The Impact of Race on Survival After Hepatocellular Carcinoma in a Diverse American Population. Dig. Dis. Sci. 2018, 63, 515–528. [Google Scholar] [CrossRef]
- Younossi, Z.; Stepanova, M.; Ong, J.P.; Jacobson, I.M.; Bugianesi, E.; Duseja, A.; Eguchi, Y.; Wong, V.W.; Negro, F.; Yilmaz, Y.; et al. Nonalcoholic Steatohepatitis Is the Fastest Growing Cause of Hepatocellular Carcinoma in Liver Transplant Candidates. Clin. Gastroenterol. Hepatol. 2019, 17, 748–755 e743. [Google Scholar] [CrossRef]
- McGlynn, K.A.; Petrick, J.L.; London, W.T. Global epidemiology of hepatocellular carcinoma: An emphasis on demographic and regional variability. Clin. Liver Dis. 2015, 19, 223–238. [Google Scholar] [CrossRef]
- Pinheiro, P.S.; Medina, H.N.; Callahan, K.E.; Jones, P.D.; Brown, C.P.; Altekruse, S.F.; McGlynn, K.A.; Kobetz, E.N. The association between etiology of hepatocellular carcinoma and race-ethnicity in Florida. Liver Int. 2020, 40, 1201–1210. [Google Scholar] [CrossRef]
- Kowdley, K.V.; Wang, C.C.; Welch, S.; Roberts, H.; Brosgart, C.L. Prevalence of chronic hepatitis B among foreign-born persons living in the United States by country of origin. Hepatology 2012, 56, 422–433. [Google Scholar] [CrossRef]
- Yatsuhashi, H. Past, Present, and Future of Viral Hepatitis C in Japan. Euroasian J. Hepatogastroenterol. 2016, 6, 49–51. [Google Scholar] [CrossRef][Green Version]
- Hall, E.W.; Rosenberg, E.S.; Sullivan, P.S. Estimates of state-level chronic hepatitis C virus infection, stratified by race and sex, United States, 2010. BMC Infect. Dis. 2018, 18, 224. [Google Scholar] [CrossRef]
- Hester, D.; Golabi, P.; Paik, J.; Younossi, I.; Mishra, A.; Younossi, Z.M. Among Medicare Patients With Hepatocellular Carcinoma, Non-alcoholic Fatty Liver Disease is the Most Common Etiology and Cause of Mortality. J. Clin. Gastroenterol. 2019. [Google Scholar] [CrossRef]
- Chang, E.T.; Yang, J.; Alfaro-Velcamp, T.; So, S.K.; Glaser, S.L.; Gomez, S.L. Disparities in liver cancer incidence by nativity, acculturation, and socioeconomic status in California Hispanics and Asians. Cancer Epidemiol. Prev. Biomark. 2010, 19, 3106–3118. [Google Scholar] [CrossRef]
- Rich, N.E.; Oji, S.; Mufti, A.R.; Browning, J.D.; Parikh, N.D.; Odewole, M.; Mayo, H.; Singal, A.G. Racial and Ethnic Disparities in Nonalcoholic Fatty Liver Disease Prevalence, Severity, and Outcomes in the United States: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 198–210. [Google Scholar] [CrossRef]
- Setiawan, V.W.; Stram, D.O.; Porcel, J.; Lu, S.C.; Le Marchand, L.; Noureddin, M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: The multiethnic cohort. Hepatology 2016, 64, 1969–1977. [Google Scholar] [CrossRef]
- Beste, L.A.; Leipertz, S.L.; Green, P.K.; Dominitz, J.A.; Ross, D.; Ioannou, G.N. Trends in Burden of Cirrhosis and Hepatocellular Carcinoma by Underlying Liver Disease in US Veterans, 2001–2013. Gastroenterology 2015, 149, 1471–1482. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Diehl, A.M.; Brunt, E.M.; Cusi, K.; Charlton, M.; Sanyal, A.J.; American Gastroenterological, A.; American Association for the Study of Liver, D.; et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012, 142, 1592–1609. [Google Scholar] [CrossRef]
- Li, W.Q.; Park, Y.; McGlynn, K.A.; Hollenbeck, A.R.; Taylor, P.R.; Goldstein, A.M.; Freedman, N.D. Index-based dietary patterns and risk of incident hepatocellular carcinoma and mortality from chronic liver disease in a prospective study. Hepatology 2014, 60, 588–597. [Google Scholar] [CrossRef]
- Bogumil, D.; Park, S.Y.; Le Marchand, L.; Haiman, C.A.; Wilkens, L.R.; Boushey, C.J.; Setiawan, V.W. High-Quality Diets Are Associated With Reduced Risk of Hepatocellular Carcinoma and Chronic Liver Disease: The Multiethnic Cohort. Hepatol. Commun. 2019, 3, 437–447. [Google Scholar] [CrossRef]
- Setiawan, V.W.; Stram, D.O.; Porcel, J.; Chari, S.T.; Maskarinec, G.; Le Marchand, L.; Wilkens, L.R.; Haiman, C.A.; Pandol, S.J.; Monroe, K.R. Pancreatic Cancer Following Incident Diabetes in African Americans and Latinos: The Multiethnic Cohort. J. Natl. Cancer Inst. 2019, 111, 27–33. [Google Scholar] [CrossRef]
- Ha, J.; Yan, M.; Aguilar, M.; Bhuket, T.; Tana, M.M.; Liu, B.; Gish, R.G.; Wong, R.J. Race/ethnicity-specific disparities in cancer incidence, burden of disease, and overall survival among patients with hepatocellular carcinoma in the United States. Cancer 2016, 122, 2512–2523. [Google Scholar] [CrossRef]
- Brar, G.; Greten, T.F.; Graubard, B.I.; McNeel, T.S.; Petrick, J.L.; McGlynn, K.A.; Altekruse, S.F. Hepatocellular Carcinoma Survival by Etiology: A SEER-Medicare Database Analysis. Hepatol. Commun. 2020, 4, 1541–1551. [Google Scholar] [CrossRef]
- Desai, A.; Sandhu, S.; Lai, J.P.; Sandhu, D.S. Hepatocellular carcinoma in non-cirrhotic liver: A comprehensive review. World J. Hepatol. 2019, 11, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; Jemal, A. Socioeconomic and Racial/Ethnic Disparities in Cancer Mortality, Incidence, and Survival in the United States, 1950–2014: Over Six Decades of Changing Patterns and Widening Inequalities. J. Environ. Public Health 2017, 2017, 2819372. [Google Scholar] [CrossRef] [PubMed]
- Halbert, C.H.; Weathers, B.; Delmoor, E.; Mahler, B.; Coyne, J.; Thompson, H.S.; Have, T.T.; Vaughn, D.; Malkowicz, S.B.; Lee, D. Racial differences in medical mistrust among men diagnosed with prostate cancer. Cancer 2009, 115, 2553–2561. [Google Scholar] [CrossRef] [PubMed]
- Penner, L.A.; Dovidio, J.F.; Gonzalez, R.; Albrecht, T.L.; Chapman, R.; Foster, T.; Harper, F.W.; Hagiwara, N.; Hamel, L.M.; Shields, A.F.; et al. The Effects of Oncologist Implicit Racial Bias in Racially Discordant Oncology Interactions. J. Clin. Oncol 2016, 34, 2874–2880. [Google Scholar] [CrossRef]
- Lin, Y.J.; Lin, C.N.; Sedghi, T.; Hsu, S.H.; Gross, C.P.; Wang, J.D.; Wang, S.Y. Treatment patterns and survival in hepatocellular carcinoma in the United States and Taiwan. PLoS ONE 2020, 15, e0240542. [Google Scholar] [CrossRef]
| Characteristics | All Patients (N = 359) | African American (N = 42) | Japanese American (N = 142) | Latino (N = 106) | White (N = 46) | Native Hawaiian (N = 23) |
|---|---|---|---|---|---|---|
| Mean age at enrollment (SD), years | 61.5 ± 7.43 | 64.1 ± 7.65 | 62.5 ± 7.75 | 60.2 ± 5.94 | 59.6 ± 7.91 | 60.7 ± 8.61 |
| Sex (%) | ||||||
| Male | 235 (65.5) | 27 (64.3) | 71 (62.0) | 88 (67.0) | 32 (69.6) | 17 (73.9) |
| Female | 124 (34.5) | 15 (35.7) | 54 (38.0) | 35 (33.0) | 14 (30.4) | 6 (26.1) |
| BMI category (%) | ||||||
| <25.0 kg/m2 | 106 (29.5) | 12 (28.6) | 57 (40.1) | 19 (17.9) | 12 (26.1) | 17 (26.1) |
| 25.0–30.0 kg/m2 | 155 (43.2) | 19 (45.2) | 58 (40.9) | 51 (48.1) | 17 (37.0) | 10 (43.5) |
| ≥30.0 kg/m2 | 95 (26.5) | 9 (21.4) | 26 (18.3) | 36 (34.0) | 17 (37.0) | 7 (30.4) |
| Unknown | 3 (0.8) | 2 (4.8) | 1 (0.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Smoking status (%) | ||||||
| Never smoker | 96 (26.7) | 8 (19.1) | 38 (26.8) | 35 (33.0) | 12 (26.1) | 3 (13.0) |
| Ever smoker | 255 (71.1) | 34 (80.9) | 104 (73.2) | 66 (62.3) | 33 (71.7) | 18 (78.3) |
| Unknown | 8 (2.2) | 0 (0.0) | 0 (0.0) | 5 (4.7) | 1 (2.2) | 2 (8.7) |
| Education (%) | ||||||
| High school graduate or less | 170 (47.4) | 20 (47.6) | 58 (40.9) | 72 (67.9) | 10 (21.7) | 10 (43.5) |
| Some college/technical school | 112 (31.2) | 15 (35.7) | 47 (33.1) | 21 (19.8) | 20 (43.5) | 9 (39.1) |
| College graduate | 35 (9.8) | 5 (11.9) | 15 (10.6) | 5 (4.7) | 8 (17.4) | 2 (8.7) |
| Graduate/professional school | 34 (9.5) | 2 (4.8) | 21 (14.8) | 3 (2.8) | 7 (15.2) | 1 (4.4) |
| Unknown | 8 (2.2) | 0 (0.0) | 1 (0.7) | 5 (4.7) | 1 (2.2) | 1 (4.4) |
| Alcohol Intake (%) | ||||||
| 0 | 176 (49.0) | 19 (45.2) | 82 (57.8) | 49 (46.2) | 18 (39.1) | 8 (34.8) |
| <12 g/day | 83 (23.1) | 11 (26.2) | 30 (21.1) | 28 (26.4) | 12 (26.1) | 2 (8.7) |
| ≥12 g/day | 84 (23.4) | 11 (26.2) | 24 (16.9) | 23 (21.7) | 14 (30.4) | 12 (52.2) |
| Missing | 16 (4.5) | 1 (2.4) | 6 (4.2) | 6 (5.7) | 2 (4.4) | 1 (4.4) |
| Diabetes mellitus (%) | 223 (62.1) | 21 (50.0) | 89 (62.7) | 79 (74.5) | 22 (47.8) | 12 (52.2) |
| Healthy Eating Index 2010 | ||||||
| Median (range) | 64.5 (32.1–93.7) | 66.5 (32.1–85.6) | 64.6 (34.6–86.8) | 62.8 (45.0–92.3) | 69.5 (41.0–93.7) | 67.8 (51.0–78.8) |
| Characteristics | All Patients (N = 359) | African American (N = 42) | Japanese American (N = 142) | Latino (N = 106) | White (N = 46) | Native Hawaiian (N = 23) |
|---|---|---|---|---|---|---|
| Mean age at diagnosis (SD), years | 75.1 ± 7.16 | 76.7 ± 8.26 | 76.2 ± 7.40 | 74.0 ± 5.86 | 72.9 ± 7.27 | 74.7 ± 7.47 |
| Median follow-up time *, months | 10.6 | 6.4 | 12.4 | 8.8 | 14.7 | 12.2 |
| Stage at diagnosis (%) | ||||||
| Localized | 169 (47.1) | 18 (40.5) | 72 (50.7) | 51 (48.1) | 21 (45.7) | 8 (34.8) |
| Regional | 87 (24.2) | 11 (26.2) | 37 (26.1) | 24 (22.6) | 10 (21.7) | 5 (21.7) |
| Distant | 57 (15.9) | 7 (16.7) | 22 (15.5) | 15 (14.2) | 8 (17.4) | 5 (21.7) |
| Unknown | 46 (12.8) | 7 (16.7) | 11 (7.8) | 16 (15.1) | 7 (15.2) | 5 (21.7) |
| p-value ** | 0.7605 | 0.9495 | 0.4677 | 0.9645 | Reference | 0.7741 |
| Underlying Etiology | ||||||
| HCV | 120 (33.4) | 25 (59.5) | 37 (26.1) | 43 (40.6) | 12 (26.1) | 3 (13.0) |
| HBV | 19 (5.3) | 0 (0.0) | 12 (8.5) | 3 (2.8) | 3 (6.5) | 1 (4.4) |
| NAFLD | 111 (30.9) | 7 (16.7) | 47 (33.1) | 32 (30.2) | 16 (34.8) | 7 (39.1) |
| ALD | 43 (12.0) | 2 (4.8) | 13 (9.2) | 21 (19.8) | 5 (10.9) | 2 (8.7) |
| Other | 66 (18.4) | 8 (19.1) | 33 (23.2) | 7 (6.6) | 10 (21.7) | 8 (34.8) |
| p-value ** | <0.0001 | 0.0120 | 0.9876 | 0.0239 | Reference | 0.6651 |
| Treatment (%) | ||||||
| None | 119 (33.2) | 21 (50.0) | 37 (26.1) | 48 (45.3) | 7 (15.2) | 6 (26.1) |
| Treated | 218 (60.7) | 20 (47.6) | 97 (68.3) | 54 (50.9) | 33 (71.7) | 14 (60.9) |
| Unknown | 22 (6.1) | 1 (2.4) | 8 (5.6) | 4 (3.8) | 6 (13.0) | 3 (13.0) |
| p-value ** | 0.0005 | 0.0009 | 0.1128 | 0.0007 | Reference | 0.5387 |
| Conditions (%) *** | ||||||
| Yes | 51 (14.2) | 28 (4.8) | 21 (14.8) | 25 (23.6) | 1 (2.2) | 2 (8.7) |
| p-value ** | 0.0021 | 0.6039 | 0.0207 | 0.0013 | Reference | 0.2559 |
| Cause of death (%) | ||||||
| All death (n) | 295 | 38 | 111 | 93 | 35 | 18 |
| HCC-related | 213 (72.2) | 28 (73.7) | 77 (69.4) | 68 (73.1) | 25 (71.4) | 15 (83.3) |
| Liver-related | 22 (7.5) | 2 (5.3) | 6 (5.4) | 12 (12.9) | 2 (5.7) | 0 (0.0) |
| Non-liver-related | 58 (19.7) | 8 (21.1) | 27 (24.3) | 12 (12.9) | 8 (22.9) | 3 (16.7) |
| Unknown | 2 (0.7) | 0 (0.0) | 1 (0.9) | 1 (1.1) | 0 (0.0) | 0 (0.0) |
| No. Deaths | Univariate HR (95% CI) a | p-Value | Multivariate HR (95% CI) b | p-Value | |
|---|---|---|---|---|---|
| Race/ethnicity | |||||
| White | 35 | 1.00 | <0.0001 | 1.00 | 0.0067 |
| African American | 38 | 1.73 (1.08–2.78) | 1.87 (1.06–3.28) | ||
| Japanese American | 111 | 0.96 (0.65–1.41) | 1.02 (0.66–1.57) | ||
| Latino | 93 | 1.92 (1.29–2.85) | 1.47 (0.91–2.38) | ||
| Native Hawaiian | 18 | 0.75 (0.42–1.34) | 0.65 (0.34–1.23) | ||
| Sex | |||||
| Female | 105 | 1.00 | 0.5638 | ||
| Male | 190 | 1.08 (0.84–1.37) | |||
| Underlying etiology | |||||
| HCV | 96 | 1.00 | 0.0007 | 1.00 | 0.0030 |
| HBV | 14 | 0.90 (0.51–1.60) | 2.00 (1.03–3.86) | ||
| NAFLD | 90 | 1.53 (1.13–2.08) | 2.02 (1.40–2.91) | ||
| ALD | 40 | 2.11 (1.44–3.09) | 1.73 (1.11–2.72) | ||
| Other | 55 | 1.20 (0.86–1.68) | 1.32 (0.88–1.99) | ||
| Stage at diagnosis | |||||
| Localized | 121 | 1.00 | <0.0001 | 1.00 | <0.0001 |
| Regional | 76 | 2.33 (1.74–3.12) | 2.16 (1.57–2.98) | ||
| Distant | 56 | 3.79 (2.74–5.25) | 3.06 (2.13–4.39) | ||
| Unknown | 42 | 4.76 (3.29–6.87) | 1.76 (1.11–2.78) | ||
| First course of treatment | |||||
| None | 113 | 1.00 | <0.0001 | 1.00 | <0.0001 |
| Treated | 162 | 0.17 (0.13–0.22) | 0.22 (0.16–0.30) | ||
| Unknown | 20 | 1.04 (0.62–1.77) | 1.06 (0.57–1.99) | ||
| Smoking status | |||||
| Never smoker | 75 | 1.00 | 0.0238 | 1.00 | 0.0021 |
| Ever smoker | 213 | 1.45 (1.11–1.90) | 1.72 (1.26–2.33) | ||
| Unknown | 7 | 1.44 (0.66–3.15) | 0.98 (0.38–2.51) | ||
| Education | |||||
| High school graduate or less | 149 | 1.00 | 0.0072 | 1.00 | 0.1614 |
| Some college/technical school | 91 | 0.82 (0.63–1.07) | 0.72 (0.52–0.98) | ||
| College graduate | 26 | 0.90 (0.59–1.38) | 0.90 (0.55–1.47) | ||
| Graduate/professional school | 22 | 0.43 (0.27–0.68) | 0.63 (0.36–1.09) | ||
| Unknown | 7 | 1.04 (0.48–2.25) | 1.43 (0.51–3.99) | ||
| Alcohol intake | |||||
| 0 | 145 | 1.00 | 0.2200 | ||
| <12 g/day | 72 | 1.21 (0.91–1.62) | |||
| ≥12 g/day | 66 | 0.93 (0.69–1.25) | |||
| Unknown | 12 | 1.56 (0.85–2.87) | |||
| BMI category (kg/m2) | |||||
| <25.0 | 87 | 1.00 | <0.0001 | 1.00 | 0.0011 |
| 25.0–30.0 | 124 | 1.43 (1.08–1.89) | 0.98 (0.71–1.36) | ||
| ≥30.0 | 81 | 2.55 (1.86–3.49) | 1.89 (1.29–2.75) | ||
| Unknown | 3 | 1.69 (0.51–5.64) | 0.82 (0.22–3.04) | ||
| Diabetes mellitus | |||||
| No | 112 | 1.00 | 0.4653 | ||
| Yes | 183 | 1.09 (0.86–1.39) | |||
| Healthy Eating Index 2010 | 283 | 0.98 (0.97–0.995) | 0.0029 | 1.00 (0.99–1.02) | 0.5470 |
| Year of diagnosis | 295 | 1.04 (1.01–1.07) | 0.0056 | 0.98 (0.95–1.01) | 0.2508 |
| Conditions c | |||||
| No | 252 | 1.00 | 0.4104 | ||
| Yes | 43 | 1.15 (0.83–1.60) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barzi, A.; Zhou, K.; Wang, S.; Dodge, J.L.; El-Khoueiry, A.; Setiawan, V.W. Etiology and Outcomes of Hepatocellular Carcinoma in an Ethnically Diverse Population: The Multiethnic Cohort. Cancers 2021, 13, 3476. https://doi.org/10.3390/cancers13143476
Barzi A, Zhou K, Wang S, Dodge JL, El-Khoueiry A, Setiawan VW. Etiology and Outcomes of Hepatocellular Carcinoma in an Ethnically Diverse Population: The Multiethnic Cohort. Cancers. 2021; 13(14):3476. https://doi.org/10.3390/cancers13143476
Chicago/Turabian StyleBarzi, Afsaneh, Kali Zhou, Songren Wang, Jennifer L. Dodge, Anthony El-Khoueiry, and Veronica Wendy Setiawan. 2021. "Etiology and Outcomes of Hepatocellular Carcinoma in an Ethnically Diverse Population: The Multiethnic Cohort" Cancers 13, no. 14: 3476. https://doi.org/10.3390/cancers13143476
APA StyleBarzi, A., Zhou, K., Wang, S., Dodge, J. L., El-Khoueiry, A., & Setiawan, V. W. (2021). Etiology and Outcomes of Hepatocellular Carcinoma in an Ethnically Diverse Population: The Multiethnic Cohort. Cancers, 13(14), 3476. https://doi.org/10.3390/cancers13143476





