The Impact of the Timing of Health-Related Quality of Life Assessments on the Actual Results in Glioma Patients: A Randomized Prospective Study
Abstract
1. Introduction
2. Results
2.1. Patient Population
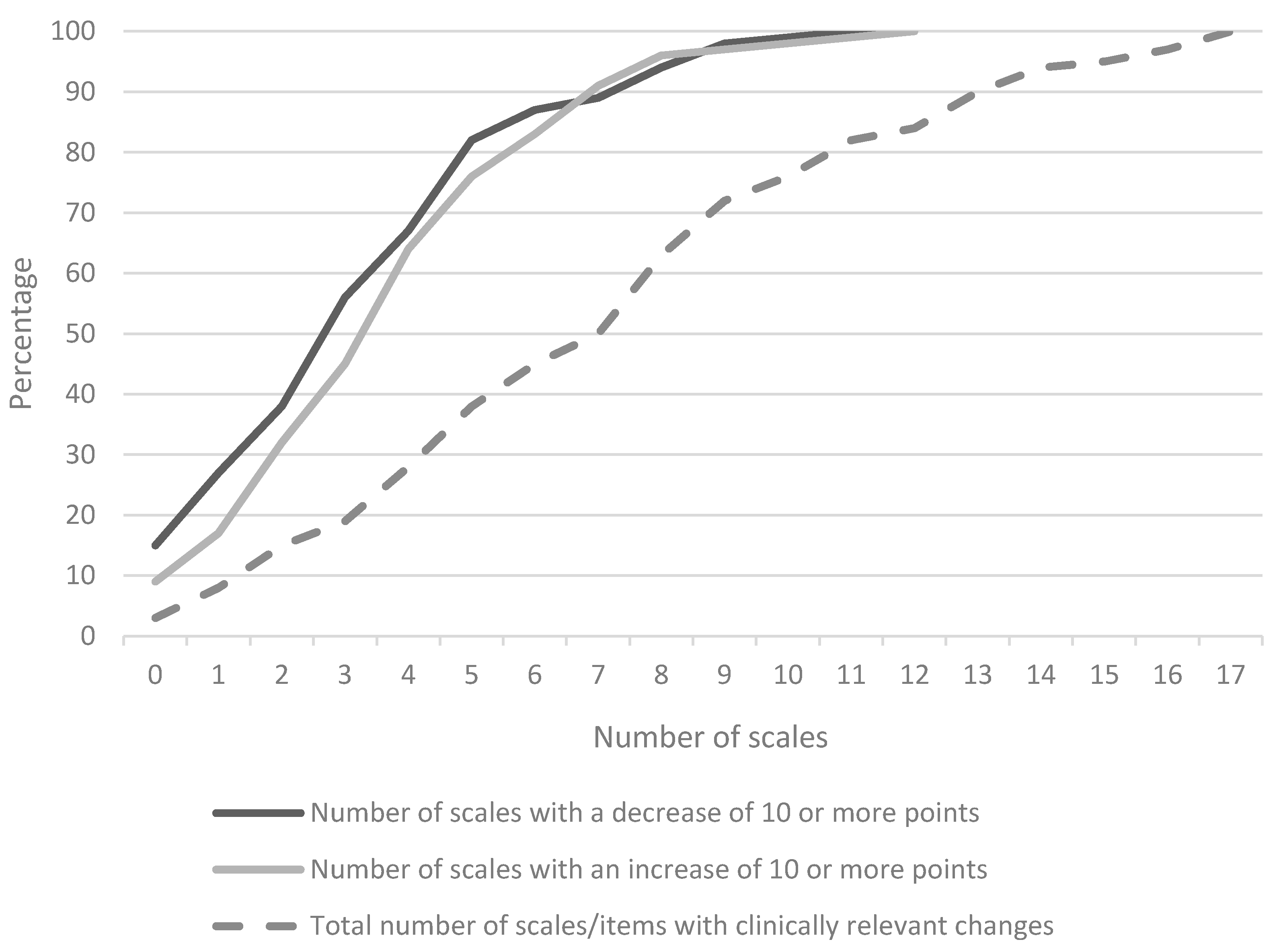
2.2. HRQoL Scores
2.3. Impact of Anxiety and Depression
3. Discussion
4. Materials and Methods
4.1. Study Design and Patients
4.2. Tools
4.3. Randomization and Timing of Assessments
4.4. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ricard, D.; Idbaih, A.; Ducray, F.; Lahutte, M.; Hoang-Xuan, K.; Delattre, J.Y. Primary brain tumours in adults. Lancet 2012, 379, 1984–1996. [Google Scholar] [CrossRef]
- Catt, S.; Chalmers, A.; Fallowfield, L. Psychosocial and supportive-care needs in high-grade glioma. Lancet Oncol. 2008, 9, 884–891. [Google Scholar] [CrossRef]
- Oberndorfer, S.; Lindeck-Pozza, E.; Lahrmann, H.; Struhal, W.; Hitzenberger, P.; Grisold, W. The end-of-life hospital setting in patients with glioblastoma. J. PalliatMed. 2008, 11, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Pace, A.; Di Lorenzo, C.; Guariglia, L.; Jandolo, B.; Carapella, C.M.; Pompili, A. End of life issues in brain tumor patients. J. Neurooncol. 2009, 91, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Sizoo, E.M.; Braam, L.; Postma, T.J.; Pasman, H.R.; Heimans, J.J.; Klein, M.; Reijneveld, J.C.; Taphoorn, M.J.B. Symptoms and problems in the end-of-life phase of high-grade glioma patients. Neuro. Oncol. 2010, 12, 1162–1166. [Google Scholar] [CrossRef] [PubMed]
- Taphoorn, M.J.; Klein, M. Cognitive deficits in adult patients with brain tumours. Lancet Neurol. 2004, 3, 159–168. [Google Scholar] [CrossRef]
- Aaronson, N.K. Quality of life: What is it? How should it be measured? Oncology (Williston Park) 1988, 2, 69–76. [Google Scholar]
- Heimans, J.J.; Taphoorn, M.J. Impact of brain tumour treatment on quality of life. J. Neurol. 2002, 249, 955–960. [Google Scholar] [CrossRef]
- Armstrong, T.S.; Gilbert, M.R. Patient reported endpoints for measuring clinical benefit in (high grade glioma) primary brain tumor patients. Curr. Treat. Options Oncol. 2014, 15, 519–528. [Google Scholar] [CrossRef]
- Efficace, F.; Taphoorn, M. Methodological issues in designing and reporting health-related quality of life in cancer clinical trials: The challenge of brain cancer studies. J. Neuro-oncol. 2012, 108, 221–226. [Google Scholar] [CrossRef]
- Weitzner, M.A.; Meyers, C.A.; Gelke, C.K.; Byrne, K.S.; Cella, D.F.; Levin, V.A. The Functional Assessment of Cancer Therapy (FACT) scale. Development of a brain subscale and revalidation of the general version (FACT-G) in patients with primary brain tumors. Cancer 1995, 75, 1151–1161. [Google Scholar] [CrossRef]
- Armstrong, T.S.; Mendoza, T.; Gning, I.; Coco, C.; Cohen, M.Z.; Eriksen, L.; Hsu, M.A.; Gilbert, M.R.; Cleeland, C. Validation of the M.D. Anderson Symptom Inventory Brain Tumor Module (MDASI-BT). J. Neurooncol. 2006, 80, 27–35. [Google Scholar] [CrossRef]
- Taphoorn, M.J.; Claassens, L.; Aaronson, N.K.; Coens, C.; Mauer, M.; Osoba, D.; Stupp, R.; Mirimanoff, R.O.; van den Bent, M.J.; Bottomley, A. An international validation study of the EORTC brain cancer module (EORTC QLQ-BN20) for assessing health-related quality of life and symptoms in brain cancer patients. Eur. J. Cancer 2010, 46, 1033–1040. [Google Scholar] [CrossRef]
- Osoba, D. Rationale for the timing of health-related quality-of-life (HQL) assessments in oncological palliative therapy. Cancer Treat. Rev. 1996, 22, 69–73. [Google Scholar] [CrossRef]
- Calvert, M.; Kyte, D.; Duffy, H.; Gheorghe, A.; Mercieca-Bebber, R.; Ives, J.; Draper, H.; Brundage, M.; Blazeby, J.; King, M. Patient-reported outcome (PRO) assessment in clinical trials: A systematic review of guidance for trial protocol writers. PLoS ONE 2014, 9, e110216. [Google Scholar] [CrossRef]
- Calvert, M.; Kyte, D.; Mercieca-Bebber, R.; Slade, A.; Chan, A.W.; King, M.T.; Hunn, A.; Bottomley, A.; Regnault, A.; Chen, A.-W.; et al. Guidelines for Inclusion of Patient-Reported Outcomes in Clinical Trial Protocols: The SPIRIT-PRO Extension. JAMA 2018, 319, 483–494. [Google Scholar] [CrossRef]
- Taphoorn, M.J.; van den Bent, M.J.; Mauer, M.E.; Coens, C.; Delattre, J.Y.; Brandes, A.A.; Sillevis Smitt, P.A.E.; Bernsen, H.J.J.A.; Frénay, M.; Tijssen, C.C.; et al. Health-related quality of life in patients treated for anaplastic oligodendroglioma with adjuvant chemotherapy: Results of a European Organisation for Research and Treatment of Cancer randomized clinical trial. J. Clin. Oncol. 2007, 25, 5723–5730. [Google Scholar] [CrossRef]
- Taphoorn, M.J.; Stupp, R.; Coens, C.; Osoba, D.; Kortmann, R.; van den Bent, M.J.; Mason, W.; Mirimanoff, R.O.; Baumert, B.G.; Eisenhauer, E.; et al. Health-related quality of life in patients with glioblastoma: A randomised controlled trial. Lancet Oncol. 2005, 6, 937–944. [Google Scholar] [CrossRef]
- Ediebah, D.E.; Coens, C.; Maringwa, J.T.; Quinten, C.; Zikos, E.; Ringash, J.; King, M.; Gotay, C.; Flechtner, H.-H.; Schmucker von Koch, J.; et al. Effect of completion-time windows in the analysis of health-related quality of life outcomes in cancer patients. Ann. Oncol. 2013, 24, 231–237. [Google Scholar] [CrossRef]
- Hakamies-Blomqvist, L.; Luoma, M.L.; Sjostrom, J.; Pluzanska, A.; Sjodin, M.; Mouridsen, H.; Ostenstad, B.; Mjaaland, I.; Ottoson, S.; Bergh, J.; et al. Timing of quality of life (QoL) assessments as a source of error in oncological trials. J. Adv. Nurs. 2001, 35, 709–716. [Google Scholar] [CrossRef]
- Coomans, M.; Taphoorn, M.; Aaronson, N.; Baumert, B.; van den Bent, M.; Bottomley, A.; Brandes, A.; Chinot, O.; Coens, C.; Gorlia, T.; et al. Measuring Change in Health-Related Quality of Life: The Added Value of Analysis on the Individual Patient Level in Glioma Patients in Clinical Decision Making. Neuro Oncol. 2019, 21 (Suppl. 6), vi197–vi198. [Google Scholar] [CrossRef]
- Osoba, D.; Aaronson, N.K.; Muller, M.; Sneeuw, K.; Hsu, M.A.; Yung, W.K.; Brada, M.; Newlands, E. The development and psychometric validation of a brain cancer quality-of-life questionnaire for use in combination with general cancer-specific questionnaires. Qual. Life Res. 1996, 5, 139–150. [Google Scholar] [CrossRef]
- Bauml, J.M.; Troxel, A.; Epperson, C.N.; Cohen, R.B.; Schmitz, K.; Stricker, C.; Shulman, L.N.; Bradbury, A.; Mao, J.J.; Langer, C.J. Scan-associated distress in lung cancer: Quantifying the impact of “scanxiety”. Lung Cancer 2016, 100, 110–113. [Google Scholar] [CrossRef]
- Aaronson, N.K. Quality of life assessment in clinical trials: Methodologic issues. Control Clin. Trials 1989, 10 (Suppl. 4), 195s–208s. [Google Scholar] [CrossRef]
- Giesinger, J.M.; Loth, F.L.C.; Aaronson, N.K.; Arraras, J.I.; Caocci, G.; Efficace, F.; Groenvold, M.; van Leeuwen, M.; Petersen, M.A.; Ramage, J.; et al. Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research. J. Clin. Epidemiol. 2020, 118, 1–8. [Google Scholar] [CrossRef]
- Musoro, J.Z.; Bottomley, A.; Coens, C.; Eggermont, A.M.; King, M.T.; Cocks, K.; Sprangers, M.A.; Groenccold, M.; Velikova, G.; Flechtner, H.-H.; et al. Interpreting European Organisation for Research and Treatment for Cancer Quality of life Questionnaire core 30 scores as minimally importantly different for patients with malignant melanoma. Eur. J. Cancer 2018, 104, 169–181. [Google Scholar] [CrossRef]
- Musoro, J.Z.; Coens, C.; Fiteni, F.; Katarzyna, P.; Cardoso, F.; Russell, N.S.; King, M.T.; Cocks, K.; Sprangers, M.A.; Groenvold, M.; et al. Minimally Important Differences for Interpreting EORTC QLQ-C30 Scores in Patients with Advanced Breast Cancer. JNCI. Cancer Spect. 2019, 3, 15–20. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Cocks, K.; King, M.T.; Velikova, G.; Fayers, P.M.; Brown, J.M. Quality, interpretation and presentation of European Organisation for Research and Treatment of Cancer quality of life questionnaire core 30 data in randomised controlled trials. Eur. J. Cancer 2008, 44, 1793–1798. [Google Scholar] [CrossRef]

| Variable | All (n = 100) | Group 1 (Before Consultation) n = 49 | Group 2 (After Consultation) n = 51 | p-Value |
|---|---|---|---|---|
| Age, years; mean (SD) | 56 (12) | 56 (12) | 55 (13) | 0.855 |
| Sex; n (%) male | 58 (58%) | 26 (53%) | 32 (63%) | 0.418 |
| Time since diagnosis (months) (median, range) | 26 (6–298) | 34 (6–298) | 23 (7–256) | 0.274 |
| Time between HRQoL assessments (days) (mean, SD) | 7 (5) | 6 (4) | 7 (6) | 0.152 |
| Tumor type; n (%) | 0.447 | |||
| Non-glioblastoma | 57 (57%) | 30 (61%) | 29 (57%) | |
| Glioblastoma | 43 (43%) | 19 (39%) | 22 (43%) | |
| KPS; median (range) | 90 (60–100) | 80 (60–100) | 90 (60–100) | 0.076 |
| Radiological response on MRI; n (%) | 0.494 | |||
| Minor response | 3 (3%) | 1 (2%) | 2 (4%) | |
| Stable disease | 87 (87%) | 42 (86%) | 45 (88%) | |
| Progressive disease | 9 (9%) | 6 (12%) | 3 (6%) | |
| Pseudoprogression | 1 (1%) | 1 (2%) | ||
| Hemisphere; n (%) | 0.34 | |||
| Left hemisphere | 47 (47%) | 23 (47%) | 24 (47%) | |
| Right hemisphere | 51 (51%) | 24 (49%) | 27 (53%) | |
| Both hemispheres | 2 (2%) | 2 (4%) | ||
| Prior antitumor treatment (multiple options possible); n (%) (maximum n = 99) | 0.788 | |||
| Biopsy | 14 (14%) | 6 (13%) | 8 (16%) | |
| Resection | 85 (86%) | 42 (88%) | 43 (84%) | |
| Chemotherapy | 74 (75%) | 38 (78%) | 36 (71%) | |
| Radiotherapy | 91 (92%) | 44 (90%) | 47 (92%) | |
| Current antitumor treatment; n (%) | 0.871 | |||
| No active treatment | 48 (48%) | 23 (47%) | 25 (49%) | |
| Chemotherapy | 46 (46%) | 23 (47%) | 23 (45%) | |
| Other | 6 (6%) | 3 (6%) | 3 (6%) | |
| Marital status; n (%) | 0.31 | |||
| Without partner | 19 (19%) | 7 (14%) | 12 (12%) | |
| With partner | 81 (81%) | 42 (86%) | 39 (76%) | |
| Dexamethasone; n (%) | 0.521 | |||
| Yes | 10 (10%) | 6 (12%) | 4 (8%) | |
| No | 90 (90%) | 43 (88% | 47 (92%) | |
| Antiepileptic drug; n (%) | 0.227 | |||
| Yes | 56 (56%) | 24 (49%) | 32 (63%) | |
| No | 44 (44%) | 25 (51%) | 19 (37%) | |
| Level of education; n (%) | 0.83 | |||
| Lower | 31 (31%) | 16 (33%) | 15 (29%) | |
| Higher | 69 (69%) | 33 (67%) | 36 (71%) |
| Scale | Mean Change Scores (95% CI of the Difference) of the Total Group (n = 100) | Unpaired t-test Mean Change Scores | Mean (SD) Change (t0 to t1) in HRQoL Group 1 | Mean (SD) Change (t0 to t1) in HRQoL Group 2 | p-value for Change (t0 to t1) between Group 1 and 2 | Number of Patients in the Total Group (n = 100) with a Change Score of <10 or >10 Points, n (%) |
|---|---|---|---|---|---|---|
| QLQc30: Global health status | 2.0 (−3.4–7.5) | 0.464 | −2.3 (14.8) | −4.4 (12.7) | 0.840 | 14 (27.5%) |
| QLQc30: Physical functioning | −0.4 (−3.9–3.0) | 0.798 | −1.4 (9.7) | −0.9 (7.5) | 0.968 | 8 (15.7%) |
| QLQc30: Role functioning | −1.2 (−9.8–7.4) | 0.783 | −5.4 (21.6) | −4.2 (21.6) | 0.414 | 22 (43.1%) |
| QLQc30: Emotional functioning | −2.0 (−8.0–4.0) | 0.504 | −1.5 (15.9) | 0.5 (14.2) | 0.563 | 11 (21.6%) |
| QLQc30: Cognitive functioning | 0.6 (−7.7–8.8) | 0.893 | −2.3 (19.2) | −2.9 (22.0) | 0.667 | 29 (56.9%) |
| QLQc30: Social functioning | −1.6 (−9.2–6.1) | 0.684 | −6.8 (20.9) | −5.2 (17.5) | 0.903 | 22 (43.1%) |
| QLQc30: Fatigue | 3.1 (−2.6–8.8) | 0.281 | 7.5 (15.1) | 4.4 (13.7) | 0.348 | 28 (54.9%) |
| QLQc30: Nausea and vomiting | −0.3 (−3.8–3.3) | 0.884 | 1.7 (7.8) | 2.0 (9.8) | 0.938 | 7 (13.7%) |
| QLQc30: Pain | −1.4 (−8.1–5.4) | 0.693 | −1.0 (18.1) | 0.3 (15.8) | 0.531 | 19 (37.7%) |
| QLQc30: Dyspnea | 0.8 (−6.1–7.6) | 0.827 | 2.7 (17.8) | 2.0 (16.9) | 0.880 | 10 (19.6%) |
| QLQc30: Insomnia | 0.7 (−6.7–8.1) | 0.845 | 2.0 (19.7) | 1.3 (17.6) | 0.681 | 14 (27.5%) |
| QLQc30: Appetite loss | 1.5 (−5.8–8.8) | 0.681 | 5.4 (19.7) | 3.9 (17.2) | 0.782 | 11 (21.6%) |
| QLQc30: Constipation | 5.4 (−2.3–13.1) | 0.165 | 4.8 (22.6) | −0.65 (15.6) | 0.292 | 11 (21.6%) |
| QLQc30: Diarrhea | −1.4 (−7.4–4.7) | 0.655 | −1.4 (15.1) | 0 (15.1) | 0.386 | 7 (14%) |
| QLQc30: Financial difficulties | 4.1 (−3.7–11.8) | 0.301 | 3.4 (17.0) | −0.65 (21.6) | 0.363 | 10 (19.6%) |
| QLQBN20: Future uncertainty | 1.1 (−3.7–5.8) | 0.655 | 3.9 (10.9) | 2.8 (12.9) | 0.387 | 18 (36%) |
| QLQBN20: Visual deficits | 3.5 (−0.4–7.4) | 0.076 | 2.4 (8.3) | −1.1 (10.8) | 0.142 | 19 (39%) |
| QLQBN20: Motor dysfunction | 0 (−5.4–5.3) | 0.992 | −1.4 (14.6) | −1.3 (12.0) | 0.754 | 25 (50%) |
| QLQBN20: Communication deficit | 1.6 (−4.7–8.0) | 0.615 | 2.9 (12.8) | 1.3 (18.5) | 0.411 | 20 (40%) |
| QLQBN20: Headache | 0.7 (−7.6–9.1) | 0.862 | 3.4 (23.8) | 2.7 (17.6) | 0.834 | 11 (22%) |
| QLQBN20: Seizures | −5.4 (−11.6–9) | 0.090 | −2.0 (12.6) | 3.3 (18.1) | 0.153 | 4 (8%) |
| QLQBN20: Drowsiness | −1.3 (−10–7.4) | 0.768 | 2.0 (24.9) | 3.3 (18.1) | 0.864 | 15 (30%) |
| QLQBN20: Hair loss | 0.7 (−6.6–7.9) | 0.859 | −0.7 (17.3) | −1.3 (19.0) | 0.600 | 7 (14%) |
| QLQBN20: Itchy skin | 0 (−6.6–6.6) | 0.997 | 0.7 (18.6) | 0.7 (14.2) | 0.802 | 6 (12%) |
| QLQBN20: Weakness of legs | 3.3 (−3.1–9.8) | 0.304 | 0.7 (18.6) | −2.7 (13.2) | 0.241 | 8 (16%) |
| QLQBN20: Bladder control | 1.5 (−4.2–7.1) | 0.608 | 3.4 (15.7) | 2.0 (12.4) | 0.935 | 7 (14%) |
| HADS: Anxiety score | 0.1 (−7–9) | 0.893 | 0.2 (2.2) | 0.1 (1.5) | 0.792 | |
| HADS: Depression score | 0.8 (0–1.6) | 0.060 | 1.0 (2.4) | 0.3 (1.7) | 0.105 |
| Univariable Regression | Multivariable Regression | |||
|---|---|---|---|---|
| Variable | p-Value | OR, 95%CI | p-Value | OR, 95%CI |
| Current antitumor treatment | 0.028 | 4.636 (1.183–18.170) | ||
| No | 0.013 | Ref | ||
| Yes | 5.444 (1.431–20.716) | |||
| Age (years) | 0.36 | 1.020 (0.977–1.065) | ||
| Sex | ||||
| Male | 0.463 | Ref | ||
| Female | 1.542 (0.485–4.898) | |||
| Educational level | ||||
| Low | 0.694 | Ref | ||
| High | 0.781 (0.228–2.678) | |||
| Partner | ||||
| No | 0.547 | Ref | ||
| Yes | 0.615 (0.127–2.990) | |||
| KPS | 0.016 | 0.913 (0.848–0.983) | 0.035 | 0.920 (0.851–0.994) |
| Disease status | ||||
| Stable | 0.998 | Ref | ||
| Progressive | 1.333 (0.457–3.883) | |||
| AED use | ||||
| No | 0.432 | Ref | ||
| Yes | 1.556 (0.517–4.682) | |||
| Corticosteroid use | ||||
| No | 0.644 | Ref | ||
| Yes | 1.658 (0.194–14.136) | |||
| HADS anxiety change score | 0.93 | 0.987 (0.731–1.331) | ||
| HADS depression change score | 0.641 | 0.940 (0.727–1.217) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peeters, M.C.M.; Zwinkels, H.; Koekkoek, J.A.F.; Vos, M.J.; Dirven, L.; Taphoorn, M.J.B. The Impact of the Timing of Health-Related Quality of Life Assessments on the Actual Results in Glioma Patients: A Randomized Prospective Study. Cancers 2020, 12, 2172. https://doi.org/10.3390/cancers12082172
Peeters MCM, Zwinkels H, Koekkoek JAF, Vos MJ, Dirven L, Taphoorn MJB. The Impact of the Timing of Health-Related Quality of Life Assessments on the Actual Results in Glioma Patients: A Randomized Prospective Study. Cancers. 2020; 12(8):2172. https://doi.org/10.3390/cancers12082172
Chicago/Turabian StylePeeters, Marthe C.M., Hanneke Zwinkels, Johan A.F. Koekkoek, Maaike J. Vos, Linda Dirven, and Martin J.B. Taphoorn. 2020. "The Impact of the Timing of Health-Related Quality of Life Assessments on the Actual Results in Glioma Patients: A Randomized Prospective Study" Cancers 12, no. 8: 2172. https://doi.org/10.3390/cancers12082172
APA StylePeeters, M. C. M., Zwinkels, H., Koekkoek, J. A. F., Vos, M. J., Dirven, L., & Taphoorn, M. J. B. (2020). The Impact of the Timing of Health-Related Quality of Life Assessments on the Actual Results in Glioma Patients: A Randomized Prospective Study. Cancers, 12(8), 2172. https://doi.org/10.3390/cancers12082172





