Effect of Serum SPARC Levels on Survival in Patients with Digestive Tract Cancer: A Post Hoc Analysis of the AMATERASU Randomized Clinical Trial
Abstract
1. Introduction
2. Results
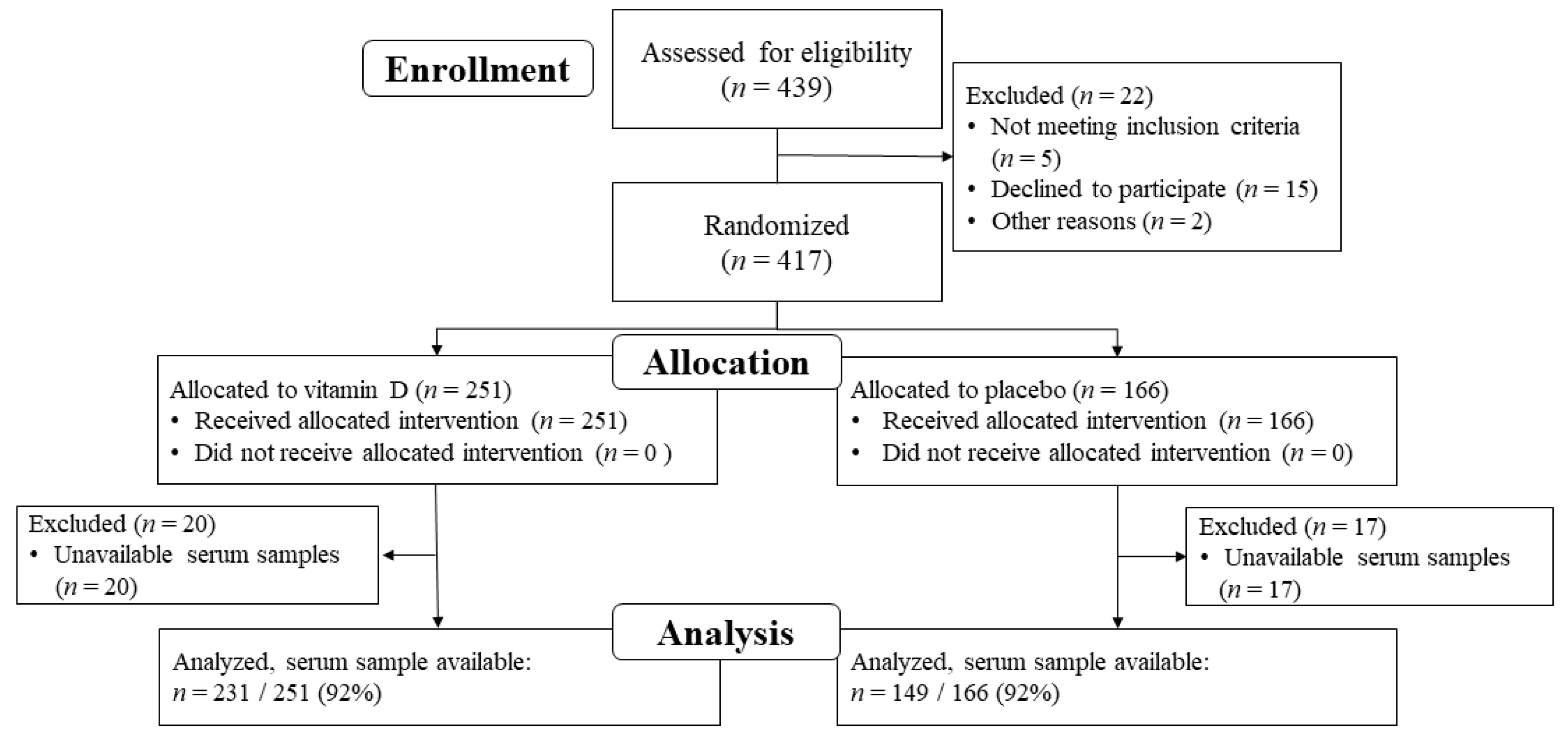
2.1. Study Population
2.2. Serum SPARC Level Assessment and Effect of Vitamin D Supplementation
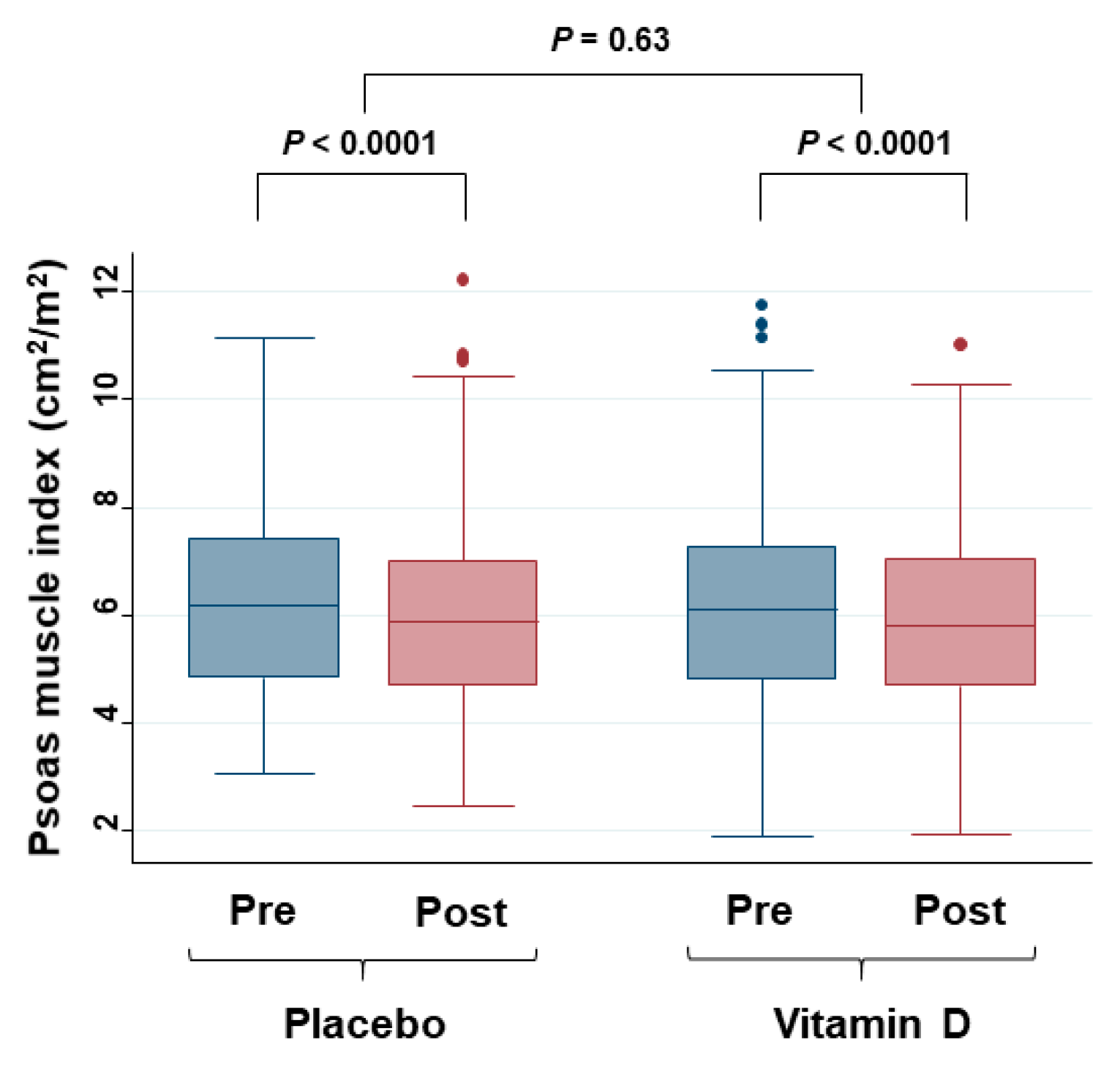
2.3. Skeletal Muscle and Sarcopenia Assessment and Effect of Vitamin D Supplementation
2.4. Patient Demographics
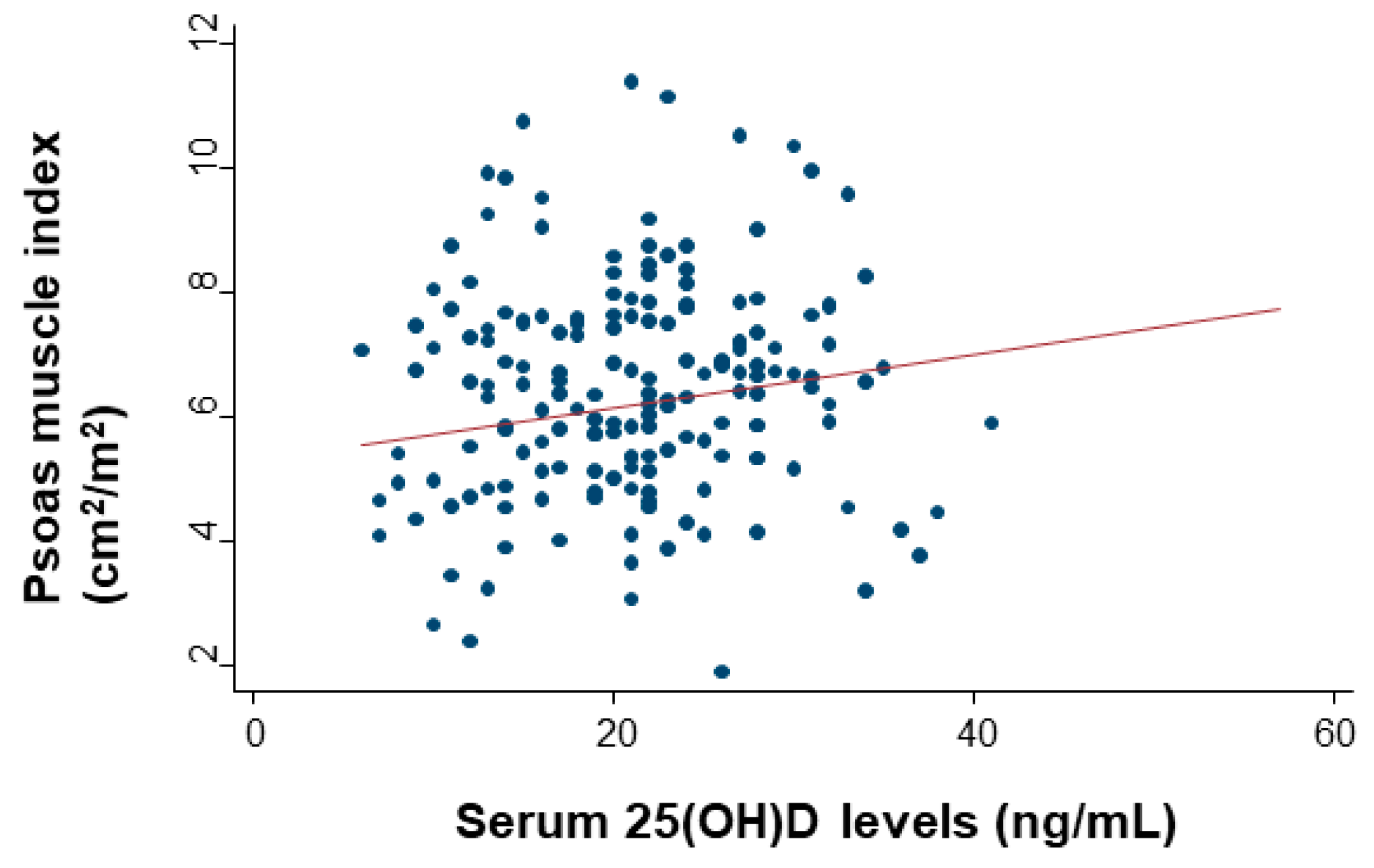
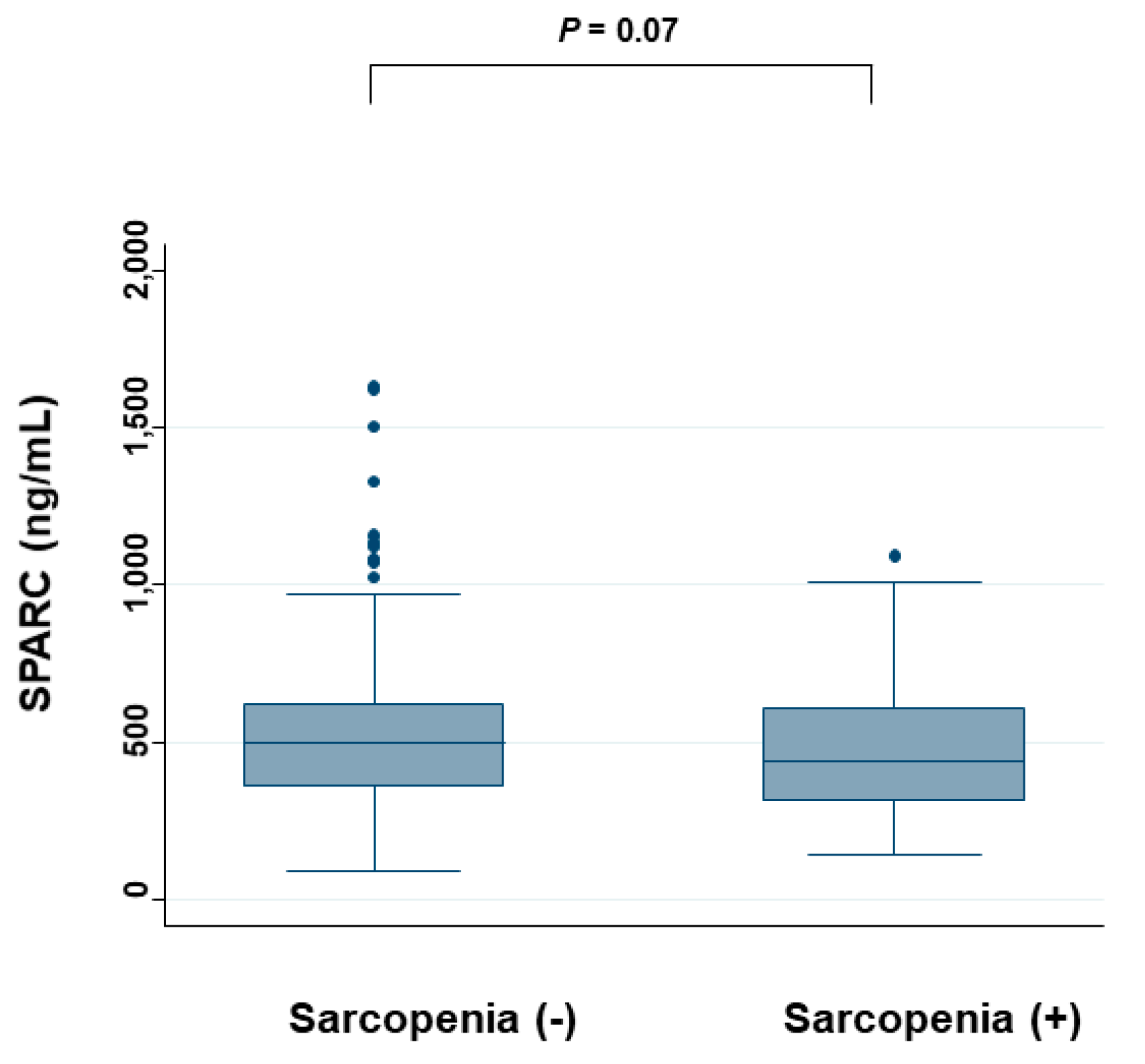
2.5. Relationship Between Serum SPARC Levels and Sarcopenia
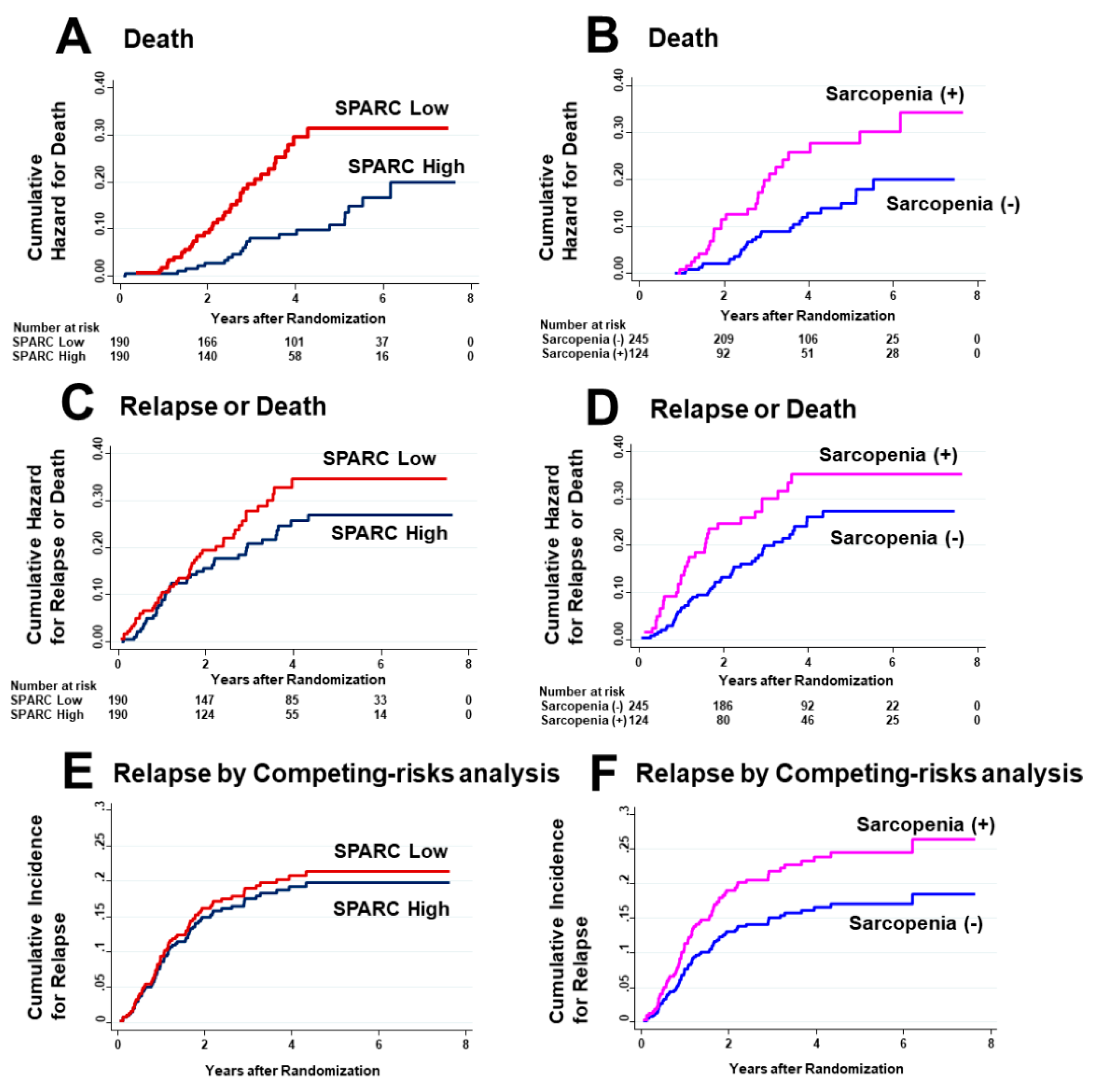
2.6. Effects of Serum SPARC Levels and Sarcopenia on Survival
3. Discussion
4. Materials and Methods
4.1. Trial Design Overview
4.2. Study Population
4.3. Outcome Measures
4.4. Measurement of Serum SPARC Levels
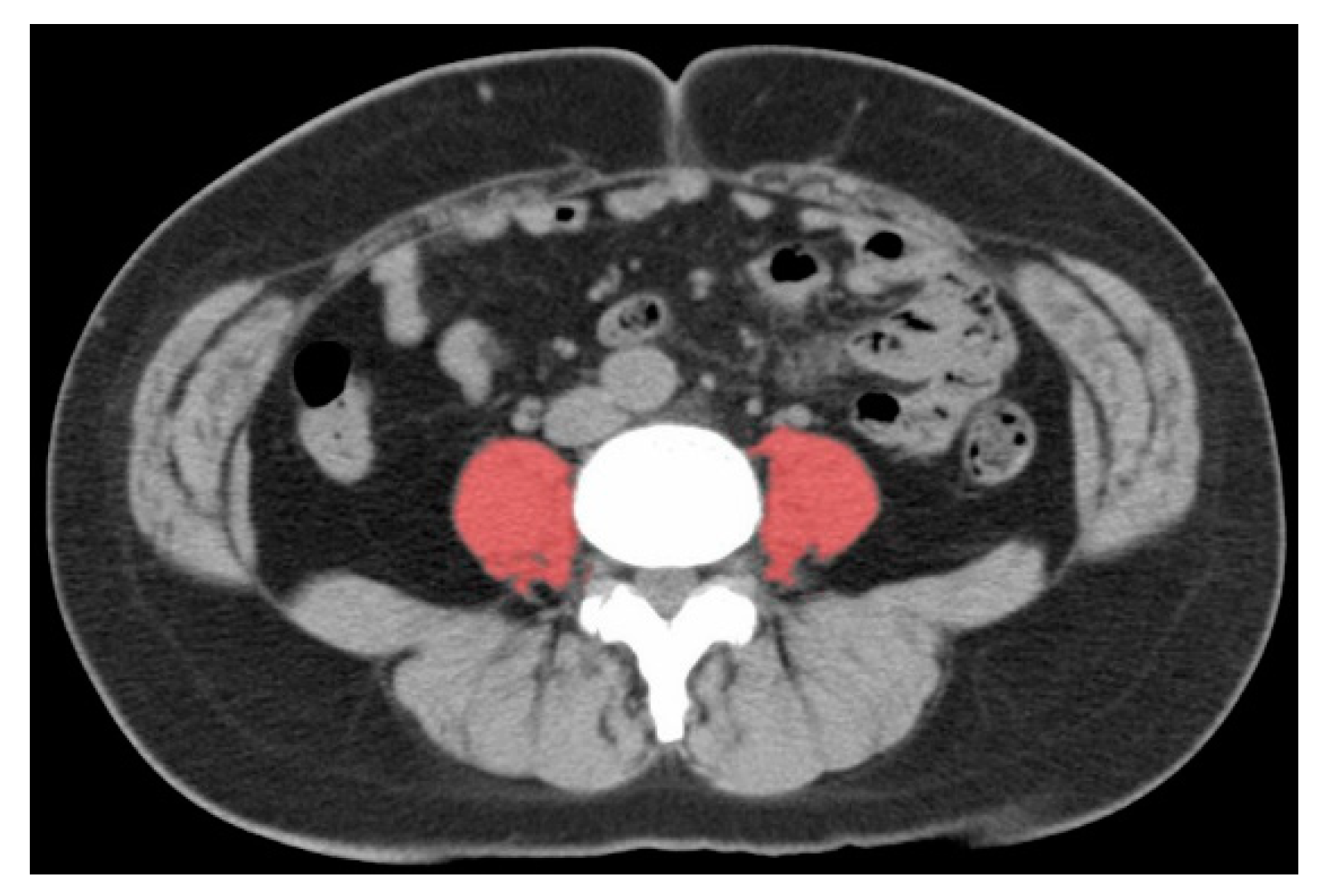
4.5. Skeletal Muscle Assessment
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Li, Y.; Gu, M.; Jing, F.; Cai, S.; Bao, C.; Wang, J.; Jin, M.; Chen, K. Association between physical activity and all cancer mortality: Dose-response meta-analysis of cohort studies. Int. J. Cancer 2016, 138, 818–832. [Google Scholar] [CrossRef] [PubMed]
- Shachar, S.S.; Williams, G.R.; Muss, H.B.; Nishijima, T.F. Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review. Eur. J. Cancer 2016, 57, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Lucia, A.; Ramírez, M. Muscling In on Cancer. N. Engl. J. Med. 2016, 375, 892–894. [Google Scholar] [CrossRef] [PubMed]
- Ghanemi, A.; Melouane, A.; Yoshioka, M.; St-Amand, J. Secreted protein acidic and rich in cysteine and bioenergetics: Extracellular matrix, adipocytes remodeling and skeletal muscle metabolism. Int. J. Biochem. Cell Biol. 2019, 117. [Google Scholar] [CrossRef] [PubMed]
- Aoi, W.; Naito, Y.; Takagi, T.; Tanimura, Y.; Takanami, Y.; Kawai, Y.; Sakuma, K.; Hang, L.P.; Mizushima, K.; Hirai, Y.; et al. A novel myokine, secreted protein acidic and rich in cysteine (SPARC), suppresses colon tumorigenesis via regular exercise. Gut 2013, 62, 882–889. [Google Scholar] [CrossRef]
- Remelli, F.; Vitali, A.; Zurlo, A.; Volpato, S. Vitamin D Deficiency and Sarcopenia in Older Persons. Nutrients 2019, 11, 2861. [Google Scholar] [CrossRef]
- Urashima, M.; Ohdaira, H.; Akutsu, T.; Okada, S.; Yoshida, M.; Kitajima, M.; Suzuki, Y. Effect of Vitamin D Supplementation on Relapse-Free Survival Among Patients With Digestive Tract Cancers. JAMA 2019, 321, 1361. [Google Scholar] [CrossRef]
- Yonaga, H.; Okada, S.; Akutsu, T.; Ohdaira, H.; Suzuki, Y.; Urashima, M. Effect Modification of Vitamin D Supplementation by Histopathological Characteristics on Survival of Patients with Digestive Tract Cancer: Post Hoc Analysis of the AMATERASU Randomized Clinical Trial. Nutrients 2019, 11, 2547. [Google Scholar] [CrossRef]
- Akutsu, T.; Okada, S.; Hirooka, S.; Ikegami, M.; Ohdaira, H.; Suzuki, Y.; Urashima, M. Effect of Vitamin D on Relapse-Free Survival in a Subgroup of Patients with p53 Protein-Positive Digestive Tract Cancer: A Post Hoc Analysis of the AMATERASU Trial. Cancer Epidemiol. Biomarkers Prev. 2020, 29, 406–413. [Google Scholar] [CrossRef]
- Urashima, M.; Okuyama, M.; Akutsu, T.; Ohdaira, H.; Kaji, M.; Suzuki, Y. Effect of vitamin D supplementation on survival of digestive tract cancer patients with low bioavailable 25-hydroxyvitamin d levels: A post hoc analysis of the AMATERASU randomized clinical trial. Cancers (Basel) 2020, 12, 347. [Google Scholar] [CrossRef]
- Lear, S.A.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R.; et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
- Wen, C.P.; Wai, J.P.M.; Tsai, M.K.; Yang, Y.C.; Cheng, T.Y.D.; Lee, M.C.; Chan, H.T.; Tsao, C.K.; Tsai, S.P.; Wu, X. Minimum amount of physical activity for reduced mortality and extended life expectancy: A prospective cohort study. Lancet 2011, 378, 1244–1253. [Google Scholar] [CrossRef]
- Swain, C.T.V.; Nguyen, N.H.; Eagles, T.; Vallance, J.K.; Boyle, T.; Lahart, I.M.; Lynch, B.M. Postdiagnosis sedentary behavior and health outcomes in cancer survivors: A systematic review and meta-analysis. Cancer 2019, 126. [Google Scholar] [CrossRef] [PubMed]
- Wagatsuma, A.; Sakuma, K. Vitamin D signaling in myogenesis: Potential for treatment of sarcopenia. Biomed. Res. Int. 2014, 2014. [Google Scholar] [CrossRef]
- Van Blarigan, E.L.; Fuchs, C.S.; Niedzwiecki, D.; Zhang, S.; Saltz, L.B.; Mayer, R.J.; Mowat, R.B.; Whittom, R.; Hantel, A.; Benson, A.; et al. Association of Survival With Adherence to the American Cancer Society Nutrition and Physical Activity Guidelines for Cancer Survivors After Colon Cancer Diagnosis. JAMA Oncol. 2018, 4, 783. [Google Scholar] [CrossRef]
- Skender, S.; Böhm, J.; Schrotz-King, P.; Chang-Claude, J.; Siegel, E.M.; Steindorf, K.; Owen, R.W.; Ose, J.; Hoffmeister, M.; Brenner, H.; et al. Plasma 25-Hydroxyvitamin D3 Levels in Colorectal Cancer Patients and Associations with Physical Activity. Nutr. Cancer 2017, 69, 229–237. [Google Scholar] [CrossRef]
- Morales-Oyarvide, V.; Meyerhardt, J.A.; Ng, K. Vitamin D and Physical Activity in Patients With Colorectal Cancer: Epidemiological Evidence and Therapeutic Implications. Cancer J. 2016, 22, 223–231. [Google Scholar] [CrossRef]
- Kang, D.W.; Lee, J.; Suh, S.H.; Ligibel, J.; Courneya, K.S.; Jeon, J.Y. Effects of exercise on insulin, IGF axis, adipocytokines, and inflammatory markers in breast cancer survivors: A systematic review and meta-analysis. Cancer Epidemiol. Biomarkers Prev. 2017, 26, 355–365. [Google Scholar] [CrossRef]
- Haydon, A.M.M.; MacInnis, R.J.; English, D.R.; Morris, H.; Giles, G.G. Physical activity, insulin-like growth factor 1, insulin-like growth factor binding protein 3, and survival from colorectal cancer. Gut 2006, 55, 689–694. [Google Scholar] [CrossRef]
- Matsubara, D.; Arita, T.; Nakanishi, M.; Kuriu, Y.; Murayama, Y.; Kudou, M.; Konishi, H.; Komatsu, S.; Shiozaki, A.; Otsuji, E. The impact of postoperative inflammation on recurrence in patients with colorectal cancer. Int. J. Clin. Oncol. 2019, 25, 602–613. [Google Scholar] [CrossRef]
- Mitsiopoulos, N.; Baumgartner, R.N.; Heymsfield, S.B.; Lyons, W.; Gallagher, D.; Ross, R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J. Appl. Physiol. 1998, 85, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Hamaguchi, Y.; Kaido, T.; Okumura, S.; Kobayashi, A.; Hammad, A.; Tamai, Y.; Inagaki, N.; Uemoto, S. Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition 2016, 32, 1200–1205. [Google Scholar] [CrossRef] [PubMed]
- Fine, J.P.; Gray, R.J. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J. Am. Stat. Assoc. 1999, 94, 496–509. [Google Scholar] [CrossRef]
| Characteristics | Total (n = 380) | SPARC Low (n = 190) | SPARC High (n = 190) |
|---|---|---|---|
| Baseline SPARC level | |||
| ng/mL, median (IQR) | 478 (351–611) | 351 (275–409) | 611 (538–720) |
| Intervention | |||
| Vitamin D supplementation, no. (%) | 231 (61) | 120 (63) | 111 (58) |
| Baseline 25(OH)D levels | |||
| ng/mL, median (IQR) | 21 (16–27) | 21 (16–28) | 21 (16–27) |
| Subgroup of 25(OH)D, no. (%) | |||
| < 20 ng/mL | 153 (41) | 77 (41) | 76 (40) |
| 20–40 ng/mL | 219 (58) | 108 (58) | 111 (59) |
| > 40 ng/mL | 5 (1) | 3 (1) | 2 (1) |
| Female, no. (%) | 125 (33) | 61 (32) | 64 (33) |
| Age (y), mean (SD) | 66 ± 11 | 68 ± 11 | 64 ± 10 |
| Physical condition | |||
| Height (cm), median (IQR) | 161 (154–167) | 161 (154–167) | 162 (155–168) |
| Weight (kg), median (IQR) | 56 (49–63) | 55 (48–61) | 58 (51–65) |
| BMI (kg/m2), median (IQR) | 22 (20–24) | 21 (19–23) | 22 (20–24) |
| Waist circumference (cm), median (IQR) | 81 (75–86) | 80 (74–85) | 82 (76–88) |
| Systolic blood pressure (mmHg), median (IQR) | 126 (115–136) | 126 (116–135) | 126 (115–136) |
| Diastolic blood pressure (mmHg), median (IQR) | 73 (67–81) | 72 (66–80) | 75 (68–82) |
| Comorbid conditions, no. (%) | |||
| Hypertension | 143 (38) | 71 (37) | 72 (38) |
| Diabetes mellitus | 61 (16) | 30 (16) | 31 (16) |
| Endocrine disease | 41 (11) | 19 (10) | 22 (12) |
| Cardiovascular disease | 28 (7) | 15 (8) | 13 (7) |
| Chronic kidney disease | 4 (1) | 4 (2) | 0 (0) |
| Asthma | 3 (1) | 1 (1) | 2 (1) |
| Orthopedic disease | 2 (1) | 1 (1) | 1 (1) |
| History of other cancers | 15 (4) | 12 (6) | 3 (2) |
| Site of cancer, no. (%) | |||
| Esophageal cancer | 37 (10) | 27 (14) | 10 (5) |
| Gastric cancer | 167 (44) | 84 (44) | 83 (44) |
| Small bowel cancer | 2 (1) | 1 (1) | 1 (1) |
| Colorectal cancer | 174 (46) | 78 (41) | 96 (51) |
| Clinical stage, no. (%) | |||
| Stage I | 169 (44) | 81 (43) | 88 (46) |
| Stage II | 100 (26) | 54 (28) | 46 (24) |
| Stage III | 111 (29) | 55 (29) | 56 (29) |
| Pathological subtype, no. (%) | |||
| Adenocarcinoma | 340 (89) | 160 (84) | 180 (95) |
| Squamous cell carcinoma | 35 (9) | 26 (14) | 9 (5) |
| Others | 5 (1) | 4 (2) | 1 (1) |
| Adjuvant chemotherapy, no. (%) | 133 (35) | 70 (36) | 63 (33) |
| Baseline serum levels, median (IQR) | |||
| Calcium (mg/dL) | 9.3 (9.0–9.6) | 9.2 (8.9–9.5) | 9.4 (9.0–9.6) |
| ALP (IU/L) | 228 (187–265) | 222 (187–262) | 234 (187–270) |
| Intact PTH (pg/mL) | 40 (32–53) | 43 (33–55) | 38 (31–50) |
| Total cholesterol (mg/dL) | 186 (161–209) | 181 (160–202) | 191 (168–212) |
| High-density cholesterol (mg/dL) | 50 (41–60) | 51 (40–59) | 49 (40–60) |
| Triglycerides (mg/dL) | 101 (73–140) | 97 (70–136) | 106 (77–145) |
| Blood glucose (mg/dL) | 103 (94–117) | 101 (92–121) | 104 (96–115) |
| HbA1c (%) | 5.6 (5.2–5.9) | 5.6 (5.2–5.9) | 5.6 (5.3–5.9) |
| BUN (mg/dL) | 14 (11–16) | 14 (11–17) | 13 (11–16) |
| Creatinine (mg/dL) | 0.8 (0.6–0.9) | 0.8 (0.6–0.9) | 0.8 (0.6–0.9) |
| Analysis Type | Death | p Value | Relapse or Death | p Value | Relapse | p Value |
|---|---|---|---|---|---|---|
| SPARC low vs. high, HR (95% CI) | ||||||
| Univariate analysis | 2.37 (1.38–4.04) | 0.002 | 1.30 (0.85–1.98) | 0.22 | 1.10 (0.69–1.74) | 0.70 |
| Multivariate analysis | 2.25 (1.25–4.05) | 0.007 | 1.20 (0.76–1.89) | 0.43 | 0.92 (0.57–1.51) | 0.75 |
| Sarcopenia presence vs. absence, HR (95% CI) | ||||||
| Univariate analysis | 1.77 (1.05–2.99) | 0.03 | 1.42 (0.93–2.17) | 0.11 | 1.51 (0.95–2.40) | 0.08 |
| Multivariate analysis | 1.30 (0.72–2.35) | 0.38 | 1.06 (0.66–1.70) | 0.82 | 1.18 (0.69–2.00) | 0.55 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akutsu, T.; Ito, E.; Narita, M.; Ohdaira, H.; Suzuki, Y.; Urashima, M. Effect of Serum SPARC Levels on Survival in Patients with Digestive Tract Cancer: A Post Hoc Analysis of the AMATERASU Randomized Clinical Trial. Cancers 2020, 12, 1465. https://doi.org/10.3390/cancers12061465
Akutsu T, Ito E, Narita M, Ohdaira H, Suzuki Y, Urashima M. Effect of Serum SPARC Levels on Survival in Patients with Digestive Tract Cancer: A Post Hoc Analysis of the AMATERASU Randomized Clinical Trial. Cancers. 2020; 12(6):1465. https://doi.org/10.3390/cancers12061465
Chicago/Turabian StyleAkutsu, Taisuke, Eisaku Ito, Mitsuo Narita, Hironori Ohdaira, Yutaka Suzuki, and Mitsuyoshi Urashima. 2020. "Effect of Serum SPARC Levels on Survival in Patients with Digestive Tract Cancer: A Post Hoc Analysis of the AMATERASU Randomized Clinical Trial" Cancers 12, no. 6: 1465. https://doi.org/10.3390/cancers12061465
APA StyleAkutsu, T., Ito, E., Narita, M., Ohdaira, H., Suzuki, Y., & Urashima, M. (2020). Effect of Serum SPARC Levels on Survival in Patients with Digestive Tract Cancer: A Post Hoc Analysis of the AMATERASU Randomized Clinical Trial. Cancers, 12(6), 1465. https://doi.org/10.3390/cancers12061465






