Comparison of Minimally Invasive versus Open Pancreatoduodenectomy for Pancreatic Ductal Adenocarcinoma: A Propensity Score Matching Analysis
Abstract
1. Introduction
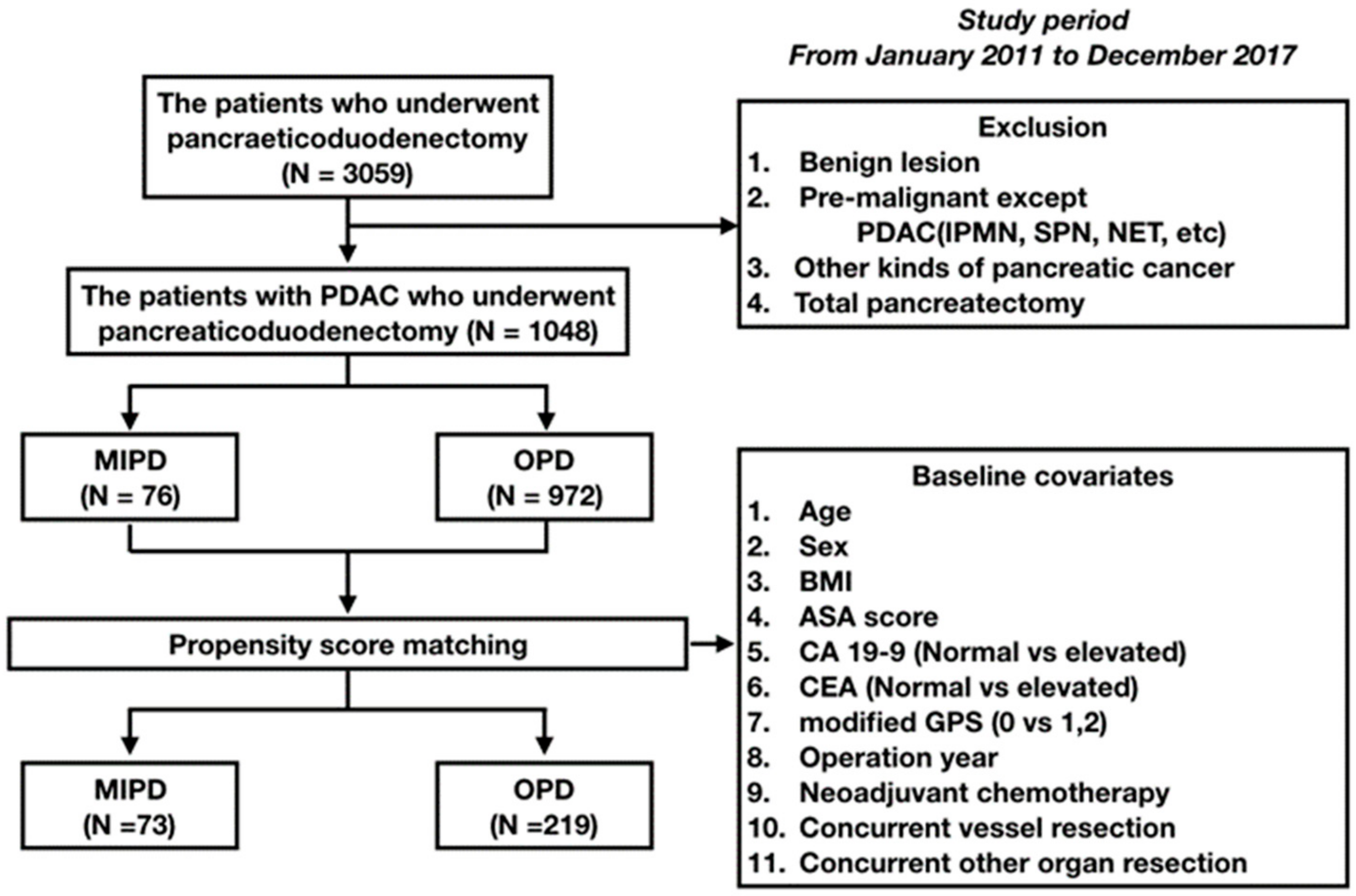
2. Materials and Methods
2.1. Patients and Post-Surgical Monitoring
2.2. Surgical Indications for MIPD in Patients with PDAC
2.3. Surgical Technique
2.3.1. Laparoscopic Pancreatoduodenectomy
2.3.2. Robotic Pancreatoduodenectomy
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics Prior to PSM
3.2. Comparison of Perioperative and Oncological Outcomes in the MIPD and OPD Groups Prior to PSM
3.3. Comparative Analysis of Perioperative and Oncologic Outcomes in the MIPD and OPD Groups After PSM
3.4. Multivariable Model of Prognostic Factors for OS and DFS After PSM
3.5. Comparative Analysis of Oncologic Outcomes Between Resectable MIPD and OPD Groups after PSM for Pathologic Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, K.; Pan, Y.; Cai, J.-Q.; Xu, X.-W.; Wu, D.; Mou, Y.-P. Totally laparoscopic gastrectomy for gastric cancer: A systematic review and meta-analysis of outcomes compared with open surgery. World J. Gastroenterol. 2014, 20, 15867–15878. [Google Scholar] [CrossRef] [PubMed]
- Haverkamp, L.; Brenkman, H.J.F.; Seesing, M.F.; Gisbertz, S.S.; Henegouwen, M.I.V.B.; Luyer, M.D.; Nieuwenhuijzen, G.; Wijnhoven, B.P.L.; Van Lanschot, J.; De Steur, W.O.; et al. Laparoscopic versus open gastrectomy for gastric cancer, a multicenter prospectively randomized controlled trial (LOGICA-trial). BMC Cancer 2015, 15, 556. [Google Scholar] [CrossRef] [PubMed]
- Peters, J.H.; Ellison, E.C.; Innes, J.T.; Liss, J.L.; Nichols, K.E.; Lomano, J.M.; Roby, S.R.; Front, M.E.; Carey, L.C. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann. Surg. 1991, 213, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Ma, R.; Yang, S.; Lin, S.; He, S.; Cai, X. Perioperative outcomes of laparoscopic versus open splenectomy for nontraumatic diseases: A meta-analysis. Chin. Med. J. 2014, 127, 2504–2510. [Google Scholar] [PubMed]
- Wu, P.C.; Langerman, A.; Ryan, C.W.; Hart, J.; Swiger, S.; Posner, M.C.; Santaniello, J.; Esposito, T.J.; A Luchette, F.; Atkian, D.K.; et al. Surgical treatment of gastrointestinal stromal tumors in the imatinib (STI-571) era. Surgery 2003, 134, 656–805. [Google Scholar] [CrossRef]
- Yang, X.; Zhong, M.-E.; Xiao, Y.; Zhang, G.-N.; Xu, L.; Lu, J.; Lin, G.-L.; Qiu, H.; Wu, B. Laparoscopic vs open resection of pT4 colon cancer: A propensity score analysis of 94 patients. Color. Dis. 2018. [Google Scholar] [CrossRef] [PubMed]
- Vennix, S.; Pelzers, L.; Bouvy, N.; Beets, G.L.; Pierie, J.-P.; Wiggers, T.; Breukink, S.O. Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst. Rev. 2014, CD005200. [Google Scholar] [CrossRef]
- Liu, G.; Ma, Y.; Wang, S.; Han, X.; Gao, D. Laparoscopic Versus Open Radical Nephrectomy for Renal Cell Carcinoma: A Systematic Review and Meta-Analysis. Transl. Oncol. 2017, 10, 501–510. [Google Scholar] [CrossRef]
- Guo, P.; Xu, W.; Li, H.; Ren, T.; Ni, S.; Ren, M. Laparoscopic Nephrectomy versus Open Nephrectomy for Patients with Autosomal Dominant Polycystic Kidney Disease: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0129317. [Google Scholar] [CrossRef]
- Raoof, M.; Ituarte, P.H.G.; Woo, Y.; Warner, S.G.; Singh, G.; Fong, Y.; Melstrom, L. Propensity score-matched comparison of oncological outcomes between laparoscopic and open distal pancreatic resection. BJS 2018, 105, 578–586. [Google Scholar] [CrossRef]
- Wellner, U.F.; Lapshyn, H.; Bartsch, D.K.; Mintziras, I.; Hopt, U.T.; Wittel, U.; Kramling, H.J.; Preissinger-Heinzel, H.; Anthuber, M.; Geissler, B.; et al. Laparoscopic versus open distal pancreatectomy—A propensity score-matched analysis from the German StuDoQ|Pancreas registry. Int. J. Color. Dis. 2016, 32, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Croome, K.P.; Farnell, M.; Que, F.G.; Reid-Lombardo, K.; Truty, M.J.; Nagorney, D.M.; Kendrick, M.L. Total Laparoscopic Pancreaticoduodenectomy for Pancreatic Ductal Adenocarcinoma. Ann. Surg. 2014, 260, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Van Hilst, J.; De Rooij, T.; Klompmaker, S.; Rawashdeh, M.; Aleotti, F.; Al-Sarireh, B.; Alseidi, A.; Ateeb, Z.; Balzano, G.; Berrevoet, F.; et al. Minimally Invasive versus Open Distal Pancreatectomy for Ductal Adenocarcinoma (DIPLOMA). Ann. Surg. 2019, 269, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Stauffer, J.A.; Coppola, A.; Villacreses, D.; Mody, K.; Johnson, E.; Li, Z.; Asbun, H.J. Laparoscopic versus open pancreaticoduodenectomy for pancreatic adenocarcinoma: Long-term results at a single institution. Surg. Endosc. 2016, 31, 2233–2241. [Google Scholar] [CrossRef]
- McMillan, D.C. The systemic inflammation-based Glasgow Prognostic Score: A decade of experience in patients with cancer. Cancer Treat. Rev. 2013, 39, 534–540. [Google Scholar] [CrossRef]
- Schlitter, A.M.; Esposito, I. Definition of Microscopic Tumor Clearance (R0) in Pancreatic Cancer Resections. Cancers 2010, 2, 2001–2010. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Hackert, T.; Hinz, U.; Pausch, T.; Fesenbeck, I.; Strobel, O.; Schneider, L.; Fritz, S.; Büchler, M.W. Postoperative pancreatic fistula: We need to redefine grades B and C. Surgery 2016, 159, 872–877. [Google Scholar] [CrossRef]
- Wente, M.N.; Bassi, C.; Dervenis, C.; Fingerhut, A.; Gouma, D.J.; Izbicki, J.R.; Neoptolemos, J.P.; Padbury, R.T.; Sarr, M.G.; Traverso, L.W.; et al. Delayed gastric emptying (DGE) after pancreatic surgery: A suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007, 142, 761–768. [Google Scholar] [CrossRef]
- Wente, M.; Veit, J.A.; Bassi, C.; Dervenis, C.; Fingerhut, A.; Gouma, D.J.; Izbicki, J.; Neoptolemos, J.P.; Padbury, R.T.; Sarr, M.G.; et al. Postpancreatectomy hemorrhage (PPH)–An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007, 142, 20–25. [Google Scholar] [CrossRef]
- Song, K.B.; Kim, S.C.; Lee, W.; Hwang, D.W.; Lee, J.H.; Kwon, J.; Park, Y.; Lee, S.J.; Park, G. Laparoscopic pancreaticoduodenectomy for periampullary tumors: Lessons learned from 500 consecutive patients in a single center. Surg. Endosc. 2019, 34, 1343–1352. [Google Scholar] [CrossRef] [PubMed]
- Gagner, M.; Pomp, A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg. Endosc. 1994, 8, 408–410. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Liu, X.-L.; Pan, Y.; Maher, H.; Wang, X.-F. Expanding laparoscopic pancreaticoduodenectomy to pancreatic-head and periampullary malignancy: Major findings based on systematic review and meta-analysis. BMC Gastroenterol. 2018, 18, 102. [Google Scholar] [CrossRef] [PubMed]
- Torphy, R.J.; Friedman, C.; Halpern, A.; Chapman, B.C.; Ahrendt, S.S.; McCarter, M.M.; Edil, B.H.; Schulick, R.D.; Gleisner, A. Comparing Short-term and Oncologic Outcomes of Minimally Invasive Versus Open Pancreaticoduodenectomy Across Low and High Volume Centers. Ann. Surg. 2019, 270, 1147–1155. [Google Scholar] [CrossRef] [PubMed]
- Delitto, D.; Luckhurst, C.M.; Black, B.S.; Beck, J.L.; George, T.J.; Sarosi, G.A.; Thomas, R.M.; Trevino, J.G.; Behrns, K.E.; Hughes, S.J. Oncologic and Perioperative Outcomes Following Selective Application of Laparoscopic Pancreaticoduodenectomy for Periampullary Malignancies. J. Gastrointest. Surg. 2016, 20, 1343–1349. [Google Scholar] [CrossRef]
- Adam, M.A.; Choudhury, K.; Dinan, M.A.; Reed, S.D.; Scheri, R.P.; Blazer, D.; Roman, S.A.; Sosa, J.A. Minimally Invasive Versus Open Pancreaticoduodenectomy for Cancer. Ann. Surg. 2015, 262, 1–377. [Google Scholar] [CrossRef]
- Zhao, Z.; Yin, Z.; Hang, Z.; Ji, G.; Feng, Q.; Zhao, Q. A systemic review and an updated meta-analysis: Minimally invasive vs open pancreaticoduodenectomy. Sci. Rep. 2017, 7, 2220. [Google Scholar] [CrossRef]
- Van Hilst, J.; De Rooij, T.; Bosscha, K.; Brinkman, D.J.; Van Dieren, S.; Dijkgraaf, M.G.; Gerhards, M.F.; De Hingh, I.H.; Karsten, T.M.; Lips, D.J.; et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): A multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol. Hepatol. 2019, 4, 199–207. [Google Scholar] [CrossRef]
- Song, K.B.; Kim, S.C.; Hwang, D.W.; Lee, J.H.; Lee, D.J.; Lee, J.W.; Park, K.; Lee, Y.J. Matched Case-Control Analysis Comparing Laparoscopic and Open Pylorus-preserving Pancreaticoduodenectomy in Patients With Periampullary Tumors. Ann. Surg. 2015, 262, 146–155. [Google Scholar] [CrossRef]
- Kuesters, S.; Chikhladze, S.; Makowiec, F.; Sick, O.; Fichtner-Feigl, S.; Hopt, U.T.; Wittel, U.A.; Chikhladzen, S. Oncological outcome of laparoscopically assisted pancreatoduodenectomy for ductal adenocarcinoma in a retrospective cohort study. Int. J. Surg. 2018, 55, 162–166. [Google Scholar] [CrossRef]
- Palanivelu, C.; Senthilnathan, P.; Sabnis, S.C.; Babu, N.S.; Gurumurthy, S.S.; Vijai, N.A.; Nalankilli, V.P.; Raj, P.P.; Parthasarathy, R.; Rajapandian, S. Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. BJS 2017, 104, 1443–1450. [Google Scholar] [CrossRef]
- Poves, I.; Burdio, F.; Morató, O.; Iglesias, M.; Radosevic, A.; Ilzarbe, L.; Visa, L.; Grande, L. Comparison of Perioperative Outcomes Between Laparoscopic and Open Approach for Pancreatoduodenectomy. Ann. Surg. 2018, 268, 731–739. [Google Scholar] [CrossRef]
- Hiki, N.; Shimizu, N.; Yamaguchi, H.; Imamura, K.; Kami, K.; Kubota, K.; Kaminishi, M. Manipulation of the small intestine as a cause of the increased inflammatory response after open compared with laparoscopic surgery. BJS 2006, 93, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Qin, H.; Luo, Q.; He, X.; Lan, P.; Lian, L. Laparoscopic Colorectal Resection in Octogenarian Patients. Med. 2015, 94, e1765. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Mao, Z.; Jin, J.; Deng, Y.; Zheng, M.; Yu, B. The Safety of CO2 Pneumoperitoneum for Elderly Patients During Laparoscopic Colorectal Surgery. Surg. Laparosc. Endosc. Percutaneous Tech. 2010, 20, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Veldkamp, R.; Kuhry, E.; Hop, W.C.J.; Jeekel, J.; Kazemier, G.; Bonjer, H.J.; Haglind, E.; Påhlman, L.; Cuesta, M.A.; Msika, S.; et al. Laparoscopic surgery versus open surgery for colon cancer: Short-term outcomes of a randomised trial. Lancet Oncol. 2005, 6, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Lacy, A.; García-Valdecasas, J.C.; Delgado, S.; Castells, A.; Taurá, P.; Piqué, J.M.; Visa, J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: A randomised trial. Lancet 2002, 359, 2224–2229. [Google Scholar] [CrossRef]
- Peng, L.; Zhou, Z.; Cao, Z.; Wu, W.; Xiao, W.; Cao, J. Long-Term Oncological Outcomes in Laparoscopic Versus Open Pancreaticoduodenectomy for Pancreatic Cancer: A Systematic Review and Meta-Analysis. J. Laparoendosc. Adv. Surg. Tech. 2019, 29, 759–769. [Google Scholar] [CrossRef]
- Bin Jung, Y.; Kang, J.; Park, E.J.; Baik, S.H.; Lee, K.Y. Time to Initiation of Adjuvant Chemotherapy in Colon Cancer: Comparison of Open, Laparoscopic, and Robotic Surgery. J. Laparoendosc. Adv. Surg. Tech. 2016, 26, 799–805. [Google Scholar] [CrossRef]
- Chun, K.H.; Bae, B.-N.; An, H.; Jeong, H.; Cho, H.; Gwak, G.; Yang, K.H.; Kim, K.H.; Kim, H.J.; Kim, Y.D. Comparison of Compliance of Adjuvant Chemotherapy between Laparoscopic and Open Surgery in Patients With Colon Cancer. Ann. Coloproctol. 2014, 30, 274–279. [Google Scholar] [CrossRef]
- Malietzis, G.; Mughal, A.; Currie, A.C.; Anyamene, N.; Kennedy, R.H.; Athanasiou, T.; Jenkins, J.T. Factors Implicated for Delay of Adjuvant Chemotherapy in Colorectal Cancer: A Meta-analysis of Observational Studies. Ann. Surg. Oncol. 2015, 22, 3793–3802. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, J.S.; Jain, S.; Bentrem, D.J.; Sekeris, E.G.; Maggard-Gibbons, M.A.; Hines, O.J.; Reber, H.A.; Ko, C.Y. Accuracy of Staging Node-Negative Pancreas Cancer. Arch. Surg. 2007, 142, 767. [Google Scholar] [CrossRef]
- Tol, J.A.; Gouma, D.J.; Bassi, C.; Dervenis, C.; Montorsi, M.; Adham, M.; Andren-Sandberg, A.; Asbun, H.J.; Bockhorn, M.; Büchler, M.W.; et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: A consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 2014, 156, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.-Y.; Kang, M.; Heo, J.; Choi, S.H.; Choi, D.W.; Park, S.-J.; Han, S.-S.; Yoon, D.S.; Yu, H.C.; Kang, K.J.; et al. A Prospective Randomized Controlled Study Comparing Outcomes of Standard Resection and Extended Resection, Including Dissection of the Nerve Plexus and Various Lymph Nodes, in Patients With Pancreatic Head Cancer. Ann. Surg. 2014, 259, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Lahat, G.; Lubezky, N.; Gerstenhaber, F.; Nizri, E.; Gysi, M.; Rozenek, M.; Goichman, Y.; Nachmany, I.; Nakache, R.; Wolf, I.; et al. Number of evaluated lymph nodes and positive lymph nodes, lymph node ratio, and log odds evaluation in early-stage pancreatic ductal adenocarcinoma: Numerology or valid indicators of patient outcome? World J. Surg. Oncol. 2016, 14, 254. [Google Scholar] [CrossRef]
- Dokmak, S.; Ftériche, F.S.; Aussilhou, B.; Bensafta, Y.; Levy, P.; Ruszniewski, P.; Belghiti, J.; Sauvanet, A. Laparoscopic Pancreaticoduodenectomy Should Not Be Routine for Resection of Periampullary Tumors. J. Am. Coll. Surg. 2015, 220, 831–838. [Google Scholar] [CrossRef]
- Chen, K.; Zhou, Y.; Jin, W.; Zhu, Q.; Lu, C.; Niu, N.; Wang, Y.; Mou, Y.; Chen, Z. Laparoscopic pancreaticoduodenectomy versus open pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: Oncologic outcomes and long-term survival. Surg. Endosc. 2019, 34, 1948–1958. [Google Scholar] [CrossRef]




| Variables | MIPD (n = 76) | OPD (n = 972) | P-Value | |
|---|---|---|---|---|
| Mean age, years (±SD) | 62.2 (±10.4) | 61.9 (±9.8) | 0.836 | |
| Sex, n (%) | Female | 34 (44.7) | 362 (37.2) | 0.153 |
| Male | 42 (55.3) | 610 (62.8) | ||
| Mean BMI, kg/m2 (±SD) | 22.7 (±2.8) | 22.8 (±2.94) | 0.832 | |
| ASA score, n (%) | I | 8 (10.5) | 59 (6.1) | 0.059 |
| II | 60 (78.9) | 858 (88.3) | ||
| III | 8 (10.5) | 55 (5.7) | ||
| CA19-9, n (%) | Normal | 34 (44.7) | 311 (32.0) | 0.017 |
| Increased | 38 (50.0) | 639 (65.7) | ||
| NA | 4 (5.3) | 22 (2.3) | ||
| CEA, n (%) | Normal | 53 (69.7) | 747 (76.9) | > 0.999 |
| Increased | 13 (17.1) | 178 (18.3) | ||
| NA | 10 (13.2) | 47 (4.8) | ||
| Preoperative biliary drainage, n (%) | Yes | 36 (47.4) | 603 (62.0) | 0.016 |
| No | 40 (52.6) | 369 (38.0) | ||
| mGPS, n (%) | 0 | 56 (73.7) | 700 (72.0) | 0.459 |
| 1–2 | 17 (22.4) | 164 (16.9) | ||
| NA | 3 (3.9) | 108 (11.1) | ||
| Neoadjuvant, n (%) | Yes | 6 (7.9) | 90 (9.3) | 0.849 |
| No | 70 (92.1) | 882 (90.7) | ||
| Concurrent vessel resection, n (%) | Vein | 11 (14.5) | 303 (31.2) | < 0.001 |
| Artery | 1 (1.3) | 35 (3.6) | ||
| Artery and vein | 0 (0) | 21 (2.2) | ||
| No | 64 (84.2) | 613 (63.1) | ||
| Concurrent resection of another organ, n (%) | Yes | 0 (0) | 29 (3.0) | 0.244 |
| No | 76 (100) | 943 (97.0) | ||
| Year of surgery, n (%) | < 2015 | 10 (13.2) | 520 (53.5) | < 0.001 |
| ≥ 2015 | 66 (86.8) | 452 (46.5) |
| Variables | MIPD (n = 76) | OPD (n = 972) | p-Value | |
|---|---|---|---|---|
| Mean operation time, minutes (±SD) | 392 (±96) | 368 (±99) | 0.043 | |
| Overall complications, n (%) | 23 (30.3) | 349 (35.9) | 0.322 | |
| In-hospital complications grade +, n (%) | No | 54 (71.1) | 659 (67.8) | 0.832 |
| Grade I–II | 18 (23.7) | 275 (28.3) | ||
| Grade III–V | 4 (5.3) | 38 (3.9) | ||
| Late complications grade +, n (%) | No | 69 (90.8) | 925 (95.2) | 0.021 |
| Grade I–II | 1 (1.3) | 26 (2.7) | ||
| Grade III–V | 6 (7.9) | 21 (2.2) | ||
| POPF ++, n (%) + | No or | 75 (98.7) | 931 (95.8) | 0.176 |
| biochemical leakage | ||||
| Grade B or C | 1 (1.3) | 41 (4.2) | ||
| Delayed gastric emptying B or C, n (%) * | Yes | 2 (2.6) | 30 (3.1) | >0.999 |
| No | 74 (97.4) | 942 (96.9) | ||
| Post-pancreatectomy hemorrhage grade B or C, n (%) ** | Yes | 2 (2.6) | 11 (1.1) | 0.242 |
| No | 74 (97.4) | 961 (98.9) | ||
| Biliary stricture during follow-up periods, n, (%) | Yes | 4 (5.3) | 7 (0.7) | 0.006 |
| No | 72 (94.7) | 965 (99.3) | ||
| Reoperation, n, (%) | Yes | 2 (2.6) | 18 (1.9) | 0.651 |
| No | 74 (97.4) | 954 (98.1) | ||
| 90 day mortality, n (%) | Yes | 0 (0) | 7 (0.7) | 0.589 |
| No | 76 (100) | 967 (99.3) | ||
| Hospital stay after operation, days (±SD) | Mean | 12.2 (±5.5) | 15.0 (±8.6) | <0.001 |
| Adjuvant | No | 15 (19.7) | 310 (31.9) | 0.001 |
| CTx | 44 (57.9) | 499 (51.3) | ||
| CCRTx | 14 (18.4) | 162 (16.7) | ||
| RTx | 3 (3.9) | 1 (0.1) | ||
| Adjuvant regimen | Fluorpyrimidine | 17 (22.4) | 303 (31.2) | 0.113 |
| Gemcitabine based | 41 (53.9) | 270 (27.8) | ||
| FOLFIRINOX | 0 (0.0) | 11 (1.1) | ||
| NA | 18 (23.7) | 388 (39.9) | ||
| Interval between surgery and adjuvant treatment, days (±SD) | Mean | 47.0 (±16.2) | 47.4 (±17.6) | 0.860 |
| Variables | MIPD (n = 76) | OPD (n = 972) | p-Value | |
|---|---|---|---|---|
| Mean pathologic tumor size, cm (±SD) | 2.7 (±0.8) | 3.1 (±1.0) | 0.019 | |
| T stage (AJCC 8th), n (%) | T1 | 17 (22.4) | 137 (14.1) | 0.011 |
| T2 | 55 (72.4) | 706 (72.6) | ||
| T3 | 4 (5.3) | 122 (12.6) | ||
| T4 | 0 (0) | 7 (0.7) | ||
| N stage (AJCC 8th), n (%) | N0 | 30 (39.5) | 373 (38.4) | 0.330 |
| N1 | 37 (48.7) | 411 (42.3) | ||
| N2 | 9 (11.8) | 188 (19.3) | ||
| Staging (AJCC 8th), + n (%) | IA | 11 (14.5) | 85 (8.7) | 0.330 |
| IB | 16 (21.1) | 257 (26.4) | ||
| IIA | 3 (3.9) | 31 (3.2) | ||
| IIB | 36 (47.4) | 395 (40.6) | ||
| III | 9 (11.8) | 182 (18.7) | ||
| IV | 1 (1.3) | 22 (2.3) | ||
| Differentiation | WD | 6 (7.9) | 113 (11.6) | 0.798 |
| MD | 59 (77.6) | 721 (74.2) | ||
| PD | 7 (9.2) | 106 (10.9) | ||
| NA | 4 (5.3) | 32 (3.3) | ||
| Lymphovascular invasion, n (%) | Yes | 50 (65.8) | 608 (62.6) | 0.574 |
| No | 26 (34.2) | 364 (37.4) | ||
| Perineural invasion, n (%) | Yes | 53 (69.7) | 852 (87.7) | <0.001 |
| No | 23 (30.3) | 120 (12.3) | ||
| Mean number of harvested lymph nodes, n (±SD) | 18.6 (±9.9) | 22.1 (±10.6) | 0.006 | |
| Mean number of positive lymph nodes, n (±SD) | 1.5 (±1.9) | 2.0 (±2.8) | 0.041 | |
| Mean positive lymph node ratio, %, (±SD) | 9.8 (±15.1) | 9.8 (±13.4) | 0.976 | |
| Resection margin ++, n (%) | R0 | 57 (75.0) | 696 (71.6) | 0.526 |
| R1 | 19 (25.0) | 276 (28.4) |
| Variables | MIPD (n = 73) | OPD (n = 219) | SMD | |
|---|---|---|---|---|
| Mean age, years | 62.4 | 63.3 | 0.091 | |
| Sex, n (%) | Female | 32 (43.8) | 105 (47.9) | 0.083 |
| Male | 41 (56.2) | 114 (52.1) | ||
| Mean BMI, kg/m2 | 22.79 | 22.85 | 0.021 | |
| ASA score, n (%) | I | 7 (9.6) | 23 (10.5) | 0.054 |
| II | 59 (80.8) | 178 (81.3) | ||
| III | 7 (9.6) | 18 (8.2) | ||
| CA19-9, n (%) | Normal | 33 (45.2) | 102 (46.6) | 0.010 |
| Increased | 36 (49.3) | 109 (49.8) | ||
| NA | 4 (5.5) | 8 (3.7) | ||
| CEA, n (%) | Normal | 50 (68.5) | 166 (75.8) | 0.040 |
| Increased | 13 (17.8) | 39 (17.8) | ||
| NA | 10 (13.7) | 14 (6.4) | ||
| Preoperative biliary drainage, n (%) | Yes | 35 (47.9) | 109 (49.8) | 0.037 |
| No | 38 (52.1) | 110 (50.2) | ||
| mGPS, n (%) | 0 | 55 (75.3) | 165 (75.3) | 0.009 |
| 1–2 | 15 (20.5) | 44 (20.1) | ||
| NA | 3 (4.1) | 10 (4.6) | ||
| Neoadjuvant, n (%) | Yes | 6 (8.2) | 15 (6.8) | 0.052 |
| No | 67 (91.8) | 204 (93.2) | ||
| Concurrent vessel resection, n (%) | Yes | 12 (16.4) | 39 (17.8) | 0.036 |
| No | 61 (83.6) | 180 (82.2) | ||
| Concurrent resection of another organ, n (%) | Yes | 0 (0) | 0 (0) | <0.001 |
| No | 73 (100) | 219 (100) | ||
| Year of surgery, n (%) | <2015 | 10 (13.7) | 31 (14.2) | 0.013 |
| ≥2015 | 63 (86.3) | 188 (85.8) |
| Variables | MIPD (n = 73) | OPD (n = 219) | p-Value # | |
|---|---|---|---|---|
| Mean operation time, minutes | 392 | 327 | <0.001 | |
| Overall complications, n, (%) | 23 (31.5) | 91 (41.6) | 0.128 | |
| In-hospital complications grade +, n (%) | No | 51 (69.9) | 142 (64.8) | 0.781 |
| Grade I–II | 18 (23.7) | 68 (31.1) | ||
| Grade III–V | 4 (5.3) | 9 (4.1) | ||
| Late complications grade +, n (%) | No | 66 (90.4) | 202 (92.2) | 0.202 |
| Grade I–II | 1 (1.4) | 10 (4.6) | ||
| Grade III–V | 6 (8.2) | 7 (3.2) | ||
| POPF ++, n (%) | No or Biochemical leakage | 72 (98.6) | 214 (97.7) | 0.640 |
| Grade B–C | 1 (1.4) | |||
| Delayed gastric emptying B or C, n (%) * | Yes | 2 (2.7) | 6 (2.7) | >0.999 |
| Post-pancreatectomy hemorrhage grade B or C, n (%) ** | Yes | 2 (2.7) | 1 (0.5) | 0.140 |
| Biliary stricture during follow-up periods, n, (%) | Yes | 4 (5.5) | 4 (1.8) | 0.110 |
| Reoperation, n (%) | Yes | 2 (2.7) | 4 (1.8) | 0.630 |
| Mean hospital stay after surgery, days | 12.4 | 14.2 | 0.040 | |
| Adjuvant treatment | Yes | 59 (80.8) | 128 (59.8) | 0.002 |
| Adjuvant regimen | Fluoropyrimidine | 16 (21.9) | 47 (21.5) | 0.191 |
| Gemcitabine based | 40 (54.8) | 74 (33.8) | ||
| or FOLFIRINOX | ||||
| NA | 17 (23.3) | 98 (44.7) | ||
| Mean interval between surgery and adjuvant treatment (±SD) | 47.3 (±16.1) | 46.6(±15.8) | 0.740 |
| Variables | MIPD (n = 73) | OPD (n = 219) | p-Value * | |
|---|---|---|---|---|
| Mean pathologic tumor size, cm | 2.75 | 2.84 | 0.49 | |
| T stage (AJCC 8th), n (%) | T1 | 15 (20.5) | 37 (16.9) | 0.415 |
| T2 | 54 (74.0) | 166 (75.8) | ||
| T3 | 4 (5.5) | 16 (7.3) | ||
| T4 | 0 (0.0) | 0 (0.0) | ||
| N stage (AJCC 8th), n (%) | N0 | 29 (39.7) | 103 (47.0) | 0.573 |
| N1 | 35 (47.9) | 76 (34.7) | ||
| N2 | 9 (12.3) | 40 (18.3) | ||
| Staging (AJCC 8th) +, n (%) | IA | 10 (13.7) | 28 (12.8) | 0.444 |
| IB | 16 (21.9) | 70 (32.0) | ||
| IIA | 3 (4.1) | 6 (2.7) | ||
| IIB | 34 (46.6) | 74 (33.8) | ||
| III | 9 (12.3) | 36 (16.4) | ||
| IV | 1 (1.4) | 5 (2.3) | ||
| Differentiation | WD | 6 (8.2) | 28 (12.8) | 0.286 |
| MD | 58 (79.5) | 168 (76.7) | ||
| PD | 6 (8.2) | 16 (7.3) | ||
| NA | 3 (4.1) | 7 (3.2) | ||
| Lymphovascular invasion, n (%) | Yes | 48 (65.8) | 127 (58.0) | 0.243 |
| No | 25 (34.2) | 92 (42.0) | ||
| Perineural invasion, n (%) | Yes | 51 (69.9) | 179 (81.7) | 0.042 |
| No | 22 (30.1) | 40 (18.3) | ||
| Mean number of harvested lymph nodes, n | 18.9 | 21.3 | 0.073 | |
| Mean number of positive lymph nodes, n | 1.52 | 1.94 | 0.82 | |
| Mean positive lymph node ratio, % | 9.52 | 9.17 | 0.86 | |
| Resection margin ++, n (%) | R0 | 56 (76.7) | 164 (74.9) | 0.76 |
| R1 | 17 (23.3) | 55 (25.1) |
| Variables | HR | 95% CI | p-Value | |
|---|---|---|---|---|
| Type of surgery | OPD | Ref | - | 0.24 |
| MIPD | 0.786 | 0.525–1.175 | ||
| Size | 1.092 | 0.847–1.409 | 0.496 | |
| T stage (AJCC 8th) | T1 | Ref | - | 0.452 |
| T2 | 1.397 | 0.776–2.514 | 0.265 | |
| T3 | 1.881 | 0.662–5.341 | 0.236 | |
| N stage (AJCC 8th) | N0 | Ref | - | 0.125 |
| N1 | 1.501 | 0.972–2.317 | 0.067 | |
| N2 | 1.958 | 0.980–3.913 | 0.057 | |
| M stage (AJCC 8th) | M1 | 1.229 | 0.682–2.214 | 0.493 |
| Differentiation | WD | Ref | - | <0.001 |
| MD | 1.826 | 1.085–3.074 | ||
| PD | 4.962 | 2.664–9.245 | ||
| Lymphovascular invasion | No | Ref | - | 0.122 |
| Yes | 1.411 | 0.912–2.184 | ||
| Perineural invasion | No | Ref | - | 0.026 |
| Yes | 1.833 | 1.074–3.128 | ||
| Number of harvested lymph nodes | 1 | 0.978–1.022 | 0.991 | |
| Number of positive lymph nodes | 1.046 | 0.924–1.183 | 0.478 | |
| Positive lymph node ratio | 0.994 | 0.966–1.022 | 0.657 | |
| Resection margin | R0 | Ref | - | 0.001 |
| R1 | 1.793 | 1.268–2.536 | ||
| Variables | HR | 95% CI | p-Value | |
|---|---|---|---|---|
| Type of surgery | OPD | Ref | - | 0.206 |
| MIPD | 0.776 | 0.523–1.150 | ||
| Size | 1.194 | 0.957–1.489 | 0.116 | |
| T stage (AJCC 8th) | T1 | Ref | - | 0.909 |
| T2 | 0.921 | 0.557–1.523 | 0.748 | |
| T3 | 0.793 | 0.281–2.242 | 0.662 | |
| N stage (AJCC 8th) | N0 | Ref | - | 0.075 |
| N1 | 1.674 | 1.061–2.641 | 0.027 | |
| N2 | 1.901 | 0.706–5.116 | 0.204 | |
| M stage (AJCC 8th) | M1 | 1.209 | 0.420–3.482 | 0.725 |
| Differentiation | WD | Ref | - | <0.001 |
| MD | 1.357 | 0.911–2.023 | 0.133 | |
| PD | 3.293 | 1.838–5.899 | <0.001 | |
| Lymphovascular invasion | No | Ref | - | 0.21 |
| Yes | 1.299 | 0.863–1.954 | ||
| Perineural invasion | No | Ref | - | 0.067 |
| Yes | 1.487 | 0.973–2.272 | ||
| Number of harvested lymph nodes | 1.002 | 0.984–1.020 | 0.853 | |
| Number of positive lymph nodes | 1.044 | 0.860–1.267 | 0.661 | |
| Positive lymph node ratio | 0.994 | 0.972–1.016 | 0.595 | |
| Resection margin | R0 | Ref | - | 0.211 |
| R1 | 1.255 | 0.879–1.793 | ||
| Variables | MIPD (n = 66) | OPD (n = 132) | SMD | |
|---|---|---|---|---|
| Mean age, years | 62.1 | 62.5 | 0.035 | |
| Sex, n (%) | Female | 29 (43.9) | 57 (43.2) | 0.015 |
| Mean BMI, kg/m2 | 22.91 | 22.83 | 0.028 | |
| ASA score, n (%) | I | 5 (7.6) | 10 (7.6) | 0.027 |
| II | 55 (83.3) | 111 (84.1) | ||
| III | 6 (9.1) | 11 (8.3) | ||
| CA19-9, n (%) | Increased | 33 (50.0) | 67 (50.1) | 0.018 |
| CEA, n (%) | Increased | 12 (18.2) | 25 (18.9) | 0.043 |
| Preoperative biliary drainage, n (%) | Yes | 33 (50.0) | 60 (45.5) | 0.091 |
| mGPS, n (%) | 1–2 | 12 (18.2) | 28 (21.2) | 0.087 |
| Neoadjuvant, n (%) | Yes | 6 (9.1) | 10 (7.6) | 0.055 |
| Concurrent vessel resection, n (%) | Yes | 12 (18.2) | 25 (18.9) | 0.019 |
| Concurrent resection of another organ, n (%) | Yes | 0 (0) | 0 (0) | <0.001 |
| Year of surgery, n (%) | ≥2015 | 57 (86.4) | 111 (84.1) | 0.064 |
| Mean pathologic tumor size, cm | Mean | 2.78 | 2.77 | 0.01 |
| Staging (AJCC 8th)+, n (%) | IA | 9 (13.6) | 20 (15.2) | 0.15 |
| IB | 16 (24.2) | 30 (22.7) | ||
| IIA | 3 (4.5) | 5 (3.8) | ||
| IIB | 28 (42.4) | 61 (46.2) | ||
| III | 9 (13.6) | 13 (9.8) | ||
| IV | 1 (1.5) | 3 (2.3) | ||
| Differentiation | WD | 6 (9.1) | 15 (11.4) | 0.158 |
| MD | 54 (81.8) | 101 (76.5) | ||
| PD | 3 (4.5) | 10 (7.6) | ||
| NA | 3 (4.5) | 6 (4.5) | ||
| Lymphovascular invasion, n (%) | Yes | 41 (62.1) | 83 (62.9) | 0.016 |
| Perineural invasion, n (%) | Yes | 49 (74.2) | 93 (70.5) | 0.085 |
| Mean number of harvested lymph nodes, n | 19.4 | 20 | 0.066 | |
| Mean number of positive lymph nodes, n | 1.53 | 1.55 | 0.007 | |
| Mean positive lymph node ratio, % | 8.29 | 8.46 | 0.016 | |
| Resection margin++, n (%) | R1 | 16 (24.2) | 35 (26.5) | 0.052 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, J.; Song, K.B.; Park, S.Y.; Shin, D.; Hong, S.; Park, Y.; Lee, W.; Lee, J.H.; Hwang, D.W.; Kim, S.C. Comparison of Minimally Invasive versus Open Pancreatoduodenectomy for Pancreatic Ductal Adenocarcinoma: A Propensity Score Matching Analysis. Cancers 2020, 12, 982. https://doi.org/10.3390/cancers12040982
Kwon J, Song KB, Park SY, Shin D, Hong S, Park Y, Lee W, Lee JH, Hwang DW, Kim SC. Comparison of Minimally Invasive versus Open Pancreatoduodenectomy for Pancreatic Ductal Adenocarcinoma: A Propensity Score Matching Analysis. Cancers. 2020; 12(4):982. https://doi.org/10.3390/cancers12040982
Chicago/Turabian StyleKwon, Jaewoo, Ki Byung Song, Seo Young Park, Dakyum Shin, Sarang Hong, Yejong Park, Woohyung Lee, Jae Hoon Lee, Dae Wook Hwang, and Song Cheol Kim. 2020. "Comparison of Minimally Invasive versus Open Pancreatoduodenectomy for Pancreatic Ductal Adenocarcinoma: A Propensity Score Matching Analysis" Cancers 12, no. 4: 982. https://doi.org/10.3390/cancers12040982
APA StyleKwon, J., Song, K. B., Park, S. Y., Shin, D., Hong, S., Park, Y., Lee, W., Lee, J. H., Hwang, D. W., & Kim, S. C. (2020). Comparison of Minimally Invasive versus Open Pancreatoduodenectomy for Pancreatic Ductal Adenocarcinoma: A Propensity Score Matching Analysis. Cancers, 12(4), 982. https://doi.org/10.3390/cancers12040982






