The Pre-Treatment C-Reactive Protein Represents a Prognostic Factor in Patients with Oral and Oropharyngeal Cancer Treated with Radiotherapy
Abstract
1. Introduction
2. Results
2.1. Analysis at Baseline
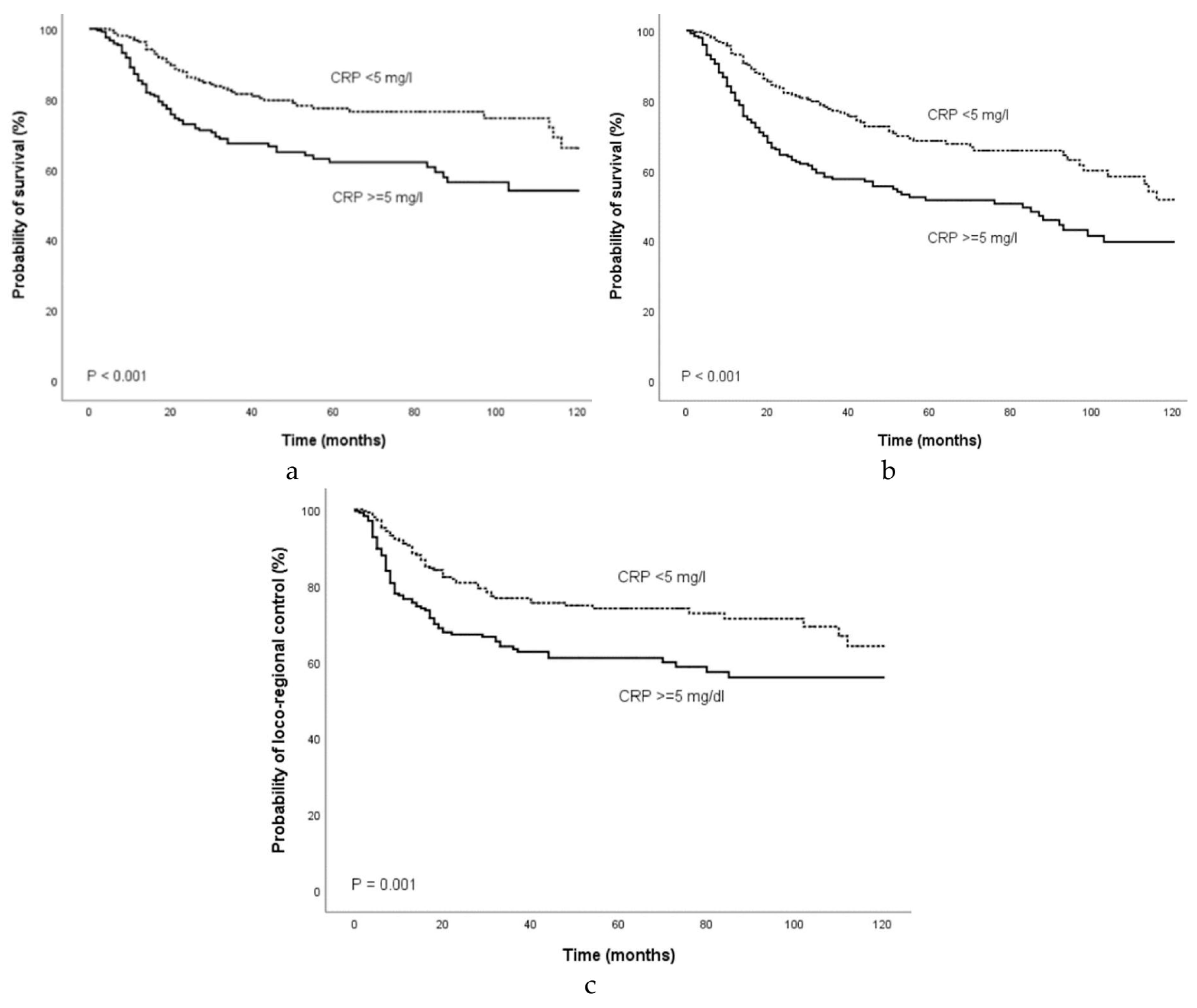
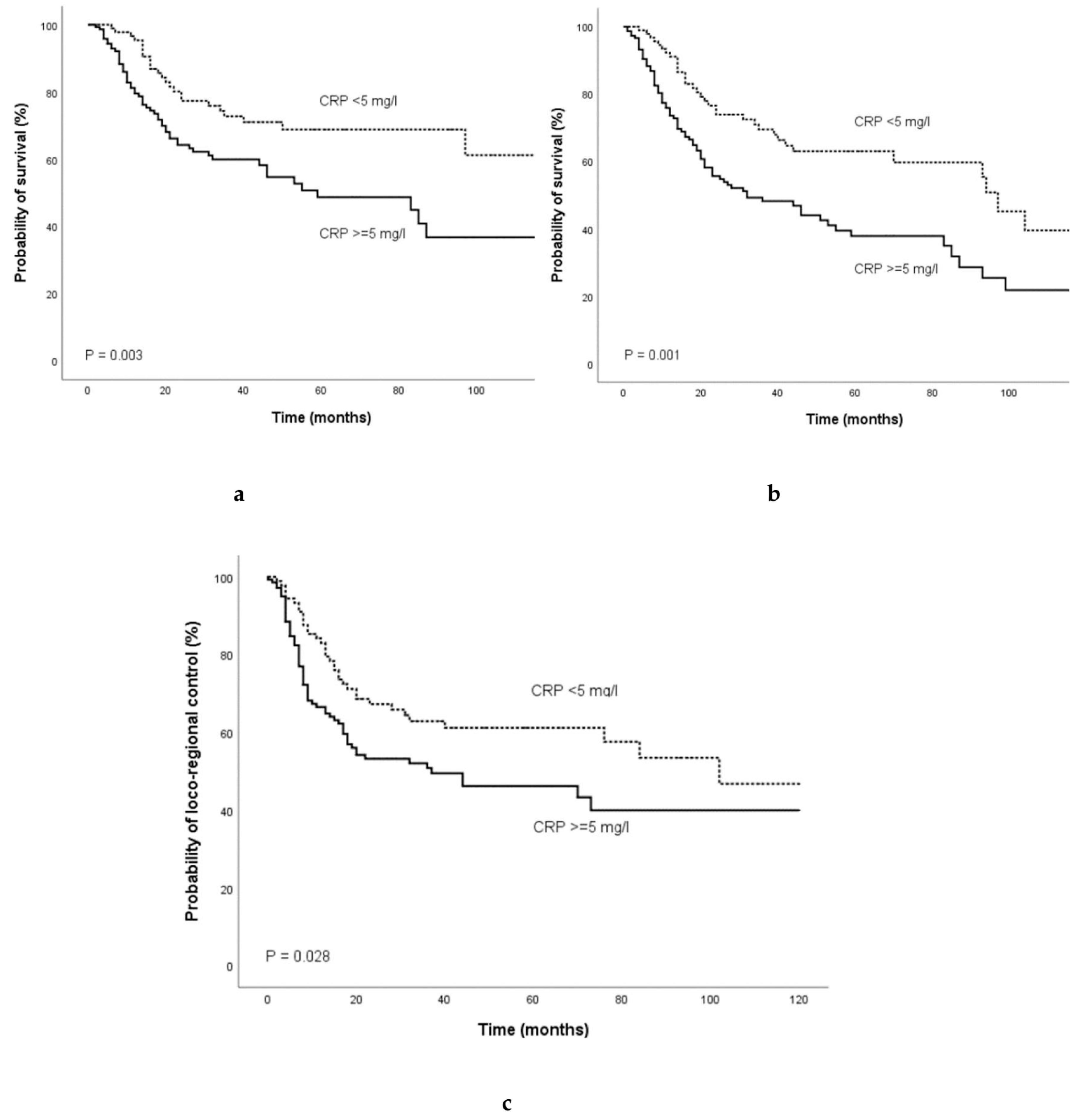
2.2. Analysis of Outcome
2.3. Predictors of Outcome
2.4. Prognostic Role of the CRP Depending on Initial Treatment
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Argiris, A.; Karamouzis, M.V.; Raben, D.; Ferris, R.L. Head and neck cancer. Lancet 2008, 371, 1695–1709. [Google Scholar] [CrossRef]
- Pignon, J.P.; le Maitre, A.; Maillard, E.; Bourhis, J.; Group, M.-N.C. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): An update on 93 randomised trials and 17,346 patients. Radiother. Oncol. 2009, 92, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Misawa, K.; Mima, M.; Satoshi, Y.; Misawa, Y.; Imai, A.; Mochizuki, D.; Nakagawa, T.; Kurokawa, T.; Oguro, M.; Ishikawa, R.; et al. Neuropeptide receptor genes GHSR and NMUR1 are candidate epigenetic biomarkers and predictors for surgically treated patients with oropharyngeal cancer. Sci. Rep. 2020, 10, e1007. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Wu, Y.; Feng, M.; Xue, X.; Fan, Y. A novel sevenmiRNA prognostic model to predict overall survival in head and neck squamous cell carcinoma patients. Mol. Med. Rep. 2019, 20, 4340–4348. [Google Scholar] [PubMed]
- Balkwill, F.; Mantovani, A. Inflammation and cancer: Back to Virchow? Lancet 2001, 357, 539–545. [Google Scholar] [CrossRef]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Choe, J.W.; Kim, H.K.; Sung, J. High-sensitivity C-reactive protein and cancer. J. Epidemiol. 2011, 21, 161–816. [Google Scholar] [CrossRef] [PubMed]
- Groblewska, M.; Mroczko, B.; Wereszczynska-Siemiatkowska, U.; Kedra, B.; Lukaszewicz, M.; Baniukiewicz, A.; Szmitkowski, M. Serum interleukin 6 (IL-6) and C-reactive protein (CRP) levels in colorectal adenoma and cancer patients. Clin. Chem. Lab. Med. 2008, 46, 1423–1428. [Google Scholar] [CrossRef]
- Roxburgh, C.S.; McMillan, D.C. The role of the in situ local inflammatory response in predicting recurrence and survival in patients with primary operable colorectal cancer. Cancer Treat. Rev. 2012, 38, 451–466. [Google Scholar] [CrossRef]
- Marnell, L.; Mold, C.; Du Clos, T.W. C-reactive protein: Ligands, receptors and role in inflammation. Clin. Immunol. 2005, 117, 104–111. [Google Scholar] [CrossRef]
- Heikkila, K.; Ebrahim, S.; Lawlor, D.A. A systematic review of the association between circulating concentrations of C reactive protein and cancer. J. Epidemiol. Community Health 2007, 61, 824–833. [Google Scholar] [CrossRef] [PubMed]
- Hefler, L.A.; Concin, N.; Hofstetter, G.; Marth, C.; Mustea, A.; Sehouli, J.; Zeillinger, R.; Leipold, H.; Lass, H.; Grimm, C.; et al. Serum C-reactive protein as independent prognostic variable in patients with ovarian cancer. Clin. Cancer Res. 2008, 14, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Thurner, E.M.; Krenn-Pilko, S.; Langsenlehner, U.; Stojakovic, T.; Pichler, M.; Gerger, A.; Kapp, K.S.; Langsenlehner, T. The elevated C-reactive protein level is associated with poor prognosis in prostate cancer patients treated with radiotherapy. Eur. J. Cancer 2015, 51, 610–619. [Google Scholar] [CrossRef] [PubMed]
- Polterauer, S.; Grimm, C.; Tempfer, C.; Sliutz, G.; Speiser, P.; Reinthaller, A.; Hefler, L.A. C-reactive protein is a prognostic parameter in patients with cervical cancer. Gynecol. Oncol. 2007, 107, 114–117. [Google Scholar] [CrossRef]
- Hashimoto, K.; Ikeda, Y.; Korenaga, D.; Tanoue, K.; Hamatake, M.; Kawasaki, K.; Yamaoka, T.; Iwatani, Y.; Akazawa, K.; Takenaka, K. The impact of preoperative serum C-reactive protein on the prognosis of patients with hepatocellular carcinoma. Cancer 2005, 103, 1856–1864. [Google Scholar] [CrossRef]
- Crozier, J.E.; McKee, R.F.; McArdle, C.S.; Angerson, W.J.; Anderson, J.H.; Horgan, P.G.; McMillan, D.C. Preoperative but not postoperative systemic inflammatory response correlates with survival in colorectal cancer. Br. J. Surg. 2007, 94, 1028–1032. [Google Scholar] [CrossRef]
- Katano, A.; Takahashi, W.; Yamashita, H.; Yamamoto, K.; Ando, M.; Yoshida, M.; Saito, Y.; Abe, O.; Nakagawa, K. The impact of elevated C-reactive protein level on the prognosis for oro-hypopharynx cancer patients treated with radiotherapy. Sci. Rep. 2017, 7, e17805. [Google Scholar] [CrossRef]
- Graupp, M.; Schaffer, K.; Wolf, A.; Vasicek, S.; Weiland, T.; Pondorfer, P.; Holzmeister, C.; Moser, U.; Thurnher, D. C-reactive protein is an independent prognostic marker in patients with tongue carcinoma - A retrospective study. Clin. Otolaryngol. 2018, 43, 1050–1056. [Google Scholar] [CrossRef]
- Tai, S.F.; Chien, H.T.; Young, C.K.; Tsao, C.K.; de Pablo, A.; Fan, K.H.; Liao, C.T.; Wang, H.M.; Kang, C.J.; Chang, J.T.; et al. Roles of preoperative C-reactive protein are more relevant in buccal cancer than other subsites. World J. Surg. Oncol. 2017, 15, e47. [Google Scholar] [CrossRef]
- Khandavilli, S.D.; Ceallaigh, P.O.; Lloyd, C.J.; Whitaker, R. Serum C-reactive protein as a prognostic indicator in patients with oral squamous cell carcinoma. Oral Oncol. 2009, 45, 912–914. [Google Scholar] [CrossRef]
- Jaiswal, M.; LaRusso, N.F.; Burgart, L.J.; Gores, G.J. Inflammatory cytokines induce DNA damage and inhibit DNA repair in cholangiocarcinoma cells by a nitric oxide-dependent mechanism. Cancer Res. 2000, 60, 184–190. [Google Scholar] [PubMed]
- Kuper, H.; Adami, H.O.; Trichopoulos, D. Infections as a major preventable cause of human cancer. J. Intern. Med. 2000, 248, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Wahl, L.M.; Kleinman, H.K. Tumor-associated macrophages as targets for cancer therapy. J. Natl. Cancer Inst. 1998, 90, 1583–1584. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Allavena, P.; Sica, A.; Balkwill, F. Cancer-related inflammation. Nature 2008, 454, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, inflammation, and cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef] [PubMed]
- Achyut, B.R.; Bader, D.A.; Robles, A.I.; Wangsa, D.; Harris, C.C.; Ried, T.; Yang, L. Inflammation-mediated genetic and epigenetic alterations drive cancer development in the neighboring epithelium upon stromal abrogation of TGF-beta signaling. PLoS Genet. 2013, 9, e1003251. [Google Scholar] [CrossRef] [PubMed]
- Dewhirst, M.W.; Cao, Y.; Moeller, B. Cycling hypoxia and free radicals regulate angiogenesis and radiotherapy response. Nat. Rev. Cancer 2008, 8, 425–437. [Google Scholar] [CrossRef]
- Barsoum, I.B.; Smallwood, C.A.; Siemens, D.R.; Graham, C.H. A mechanism of hypoxia-mediated escape from adaptive immunity in cancer cells. Cancer Res. 2014, 74, 665–674. [Google Scholar] [CrossRef]
- Yang, J.; Wezeman, M.; Zhang, X.; Lin, P.; Wang, M.; Qian, J.; Wan, B.; Kwak, L.W.; Yu, L.; Yi, Q. Human C-reactive protein binds activating Fcgamma receptors and protects myeloma tumor cells from apoptosis. Cancer Cell 2007, 12, 252–265. [Google Scholar] [CrossRef]
- Nozoe, T.; Korenaga, D.; Futatsugi, M.; Saeki, H.; Maehara, Y.; Sugimachi, K. Immunohistochemical expression of C-reactive protein in squamous cell carcinoma of the esophagus-significance as a tumor marker. Cancer Lett. 2003, 192, 89–95. [Google Scholar] [CrossRef]
- Lindenmann, J.; Fink-Neuboeck, N.; Koesslbacher, M.; Pichler, M.; Stojakovic, T.; Roller, R.E.; Maier, A.; Anegg, U.; Smolle, J.; Smolle-Juettner, F.M. The influence of elevated levels of C-reactive protein and hypoalbuminemia on survival in patients with advanced inoperable esophageal cancer undergoing palliative treatment. J. Surg. Oncol. 2014, 110, 645–650. [Google Scholar] [CrossRef]
- Peter, F.; Wittekindt, C.; Finkensieper, M.; Kiehntopf, M.; Guntinas-Lichius, O. Prognostic impact of pretherapeutic laboratory values in head and neck cancer patients. J. Cancer Res. Clin. Oncol. 2013, 139, 171–178. [Google Scholar] [CrossRef]
- Grimm, M.; Rieth, J.; Hoefert, S.; Krimmel, M.; Rieth, S.; Teriete, P.; Kluba, S.; Biegner, T.; Munz, A.; Reinert, S. Standardized pretreatment inflammatory laboratory markers and calculated ratios in patients with oral squamous cell carcinoma. Eur. Arch. Otorhinolaryngol. 2016, 273, 3371–3384. [Google Scholar] [CrossRef]
- Chen, I.H.; Liao, C.T.; Wang, H.M.; Huang, J.J.; Kang, C.J.; Huang, S.F. Using SCC antigen and CRP levels as prognostic biomarkers in recurrent oral cavity squamous cell carcinoma. PLoS ONE 2014, 9, e103265. [Google Scholar] [CrossRef]
- Huang, S.F.; Wei, F.C.; Liao, C.T.; Wang, H.M.; Lin, C.Y.; Lo, S.; Huang, J.J.; Chen, I.H.; Kang, C.J.; Chien, H.T.; et al. Risk stratification in oral cavity squamous cell carcinoma by preoperative CRP and SCC antigen levels. Ann. Surg. Oncol. 2012, 19, 3856–3864. [Google Scholar] [CrossRef]
- Chen, H.H.; Chen, I.H.; Liao, C.T.; Wei, F.C.; Lee, L.Y.; Huang, S.F. Preoperative circulating C-reactive protein levels predict pathological aggressiveness in oral squamous cell carcinoma: A retrospective clinical study. Clin. Otolaryngol. 2011, 36, 147–153. [Google Scholar] [CrossRef]
- Kuboki, A.; Kanaya, H.; Nakayama, T.; Konno, W.; Goto, K.; Nakajima, I.; Kashiwagi, T.; Hirabayashi, H.; Haruna, S.I. Prognostic value of C-reactive protein/albumin ratio for patients with hypopharyngeal and laryngeal cancer undergoing invasive surgery involving laryngectomy. Head Neck 2019, 41, 1342–1350. [Google Scholar] [CrossRef]
- Yu, S.T.; Zhou, Z.; Cai, Q.; Liang, F.; Han, P.; Chen, R.; Huang, X.M. Prognostic value of the C-reactive protein/albumin ratio in patients with laryngeal squamous cell carcinoma. Onco Targets Ther. 2017, 10, 879–884. [Google Scholar] [CrossRef]
- Ferris, R.L. Immunology and Immunotherapy of Head and Neck Cancer. J. Clin. Oncol. 2015, 33, 3293–3304. [Google Scholar] [CrossRef]
- Yang, L.; Huang, Y.; Zhou, L.; Dai, Y.; Hu, G. High pretreatment neutrophil-to-lymphocyte ratio as a predictor of poor survival prognosis in head and neck squamous cell carcinoma: Systematic review and meta-analysis. Head Neck 2019, 41, 1525–1535. [Google Scholar] [CrossRef]
- Kruse, A.L.; Luebbers, H.T.; Gratz, K.W. C-reactive protein levels: A prognostic marker for patients with head and neck cancer? Head Neck Oncol. 2010, 2, e21. [Google Scholar] [CrossRef]
- Selzer, E.; Grah, A.; Heiduschka, G.; Kornek, G.; Thurnher, D. Primary radiotherapy or postoperative radiotherapy in patients with head and neck cancer: Comparative analysis of inflammation-based prognostic scoring systems. Strahlenther. Onkol. 2015, 191, 486–494. [Google Scholar] [CrossRef]
- Rodriguez-Ruiz, M.E.; Vanpouille-Box, C.; Melero, I.; Formenti, S.C.; Demaria, S. Immunological Mechanisms Responsible for Radiation-Induced Abscopal Effect. Trends Immunol. 2018, 39, 644–655. [Google Scholar] [CrossRef]
- Formenti, S.C.; Demaria, S. Systemic effects of local radiotherapy. Lancet Oncol. 2009, 10, 718–726. [Google Scholar] [CrossRef]
- Galluzzi, L.; Maiuri, M.C.; Vitale, I.; Zischka, H.; Castedo, M.; Zitvogel, L.; Kroemer, G. Cell death modalities: Classification and pathophysiological implications. Cell Death Differ. 2007, 14, 1237–1243. [Google Scholar] [CrossRef]
- Nesslinger, N.J.; Sahota, R.A.; Stone, B.; Johnson, K.; Chima, N.; King, C.; Rasmussen, D.; Bishop, D.; Rennie, P.S.; Gleave, M.; et al. Standard treatments induce antigen-specific immune responses in prostate cancer. Clin. Cancer Res. 2007, 13, 1493–1502. [Google Scholar] [CrossRef]
- Baron, J.A.; Cole, B.F.; Sandler, R.S.; Haile, R.W.; Ahnen, D.; Bresalier, R.; McKeown-Eyssen, G.; Summers, R.W.; Rothstein, R.; Burke, C.A.; et al. A randomized trial of aspirin to prevent colorectal adenomas. N. Engl. J. Med. 2003, 348, 891–899. [Google Scholar] [CrossRef]
- Benamouzig, R.; Deyra, J.; Martin, A.; Girard, B.; Jullian, E.; Piednoir, B.; Couturier, D.; Coste, T.; Little, J.; Chaussade, S. Daily soluble aspirin and prevention of colorectal adenoma recurrence: One-year results of the APACC trial. Gastroenterology 2003, 125, 328–336. [Google Scholar] [CrossRef]
- Kashfi, K. Anti-inflammatory agents as cancer therapeutics. Adv. Pharmacol. 2009, 57, 31–89. [Google Scholar]
- Zhang, Z.; Chen, F.; Shang, L. Advances in antitumor effects of NSAIDs. Cancer Manag. Res. 2018, 10, 4631–4640. [Google Scholar] [CrossRef]
| Criterion | Value |
|---|---|
| Number of patients | 503 |
| Sex | |
| Male | 378 (75.1%) |
| Female | 125 (24.9%) |
| Age; median (mean ± SD) | 58.00 (59.2 ± 10.7) |
| BMI; median (mean ± SD) | 24.03 (24.52 ± 4.39) |
| Smoking status | |
| Former * or never | 183 (36.4%) |
| Current | 313 (62.2%) |
| Alcohol abuse | |
| Former * or never | 292 (58.1%) |
| Current | 197 (39.2%) |
| Tumor site | |
| Oral cavity | 195 (38.8%) |
| Oropharynx | 308(61.2%) |
| Tumor grade | |
| G 1/2 | 249 (49.5%) |
| G 3/4 | 249 (49.5%) |
| Tumor stage | |
| T 1/2 | 201 (40.0%) |
| T 3/4 | 292 (58.1%) |
| Nodal involvement | |
| Yes | 401 (79.7%) |
| No | 96 (19.1%) |
| Surgery | |
| Yes | 261 (51.9%) |
| No | 242 (48.1%) |
| Induction chemotherapy | |
| Yes | 77 (15.3%) |
| No | 426 (84.7%) |
| Concomitant chemotherapy | |
| Yes | 303 (60.2%) |
| No | 199 (39.6%) |
| NLR, median (mean ± SD) | 3.15 (3.79 ± 2.66) |
| PLR, median (mean ± SD) | 155.8 (178.1 ± 99.42) |
| CRP, median (mean ± SD) | 5.0 (15.08 ± 31.84) |
| Criterion | Cancer–Specific Survival | Overall Survival | Loco-Regional Control | |||
|---|---|---|---|---|---|---|
| HR (95% CI) * | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Sex | ||||||
| Male | 1 | 1 | 1 | |||
| Female | 1.15 (0.78–1.70) | 0.469 | 0.93 (0.67–1.30) | 0.681 | 1.09 (0.76–1.57) | 0.636 |
| Age (continuous) | 1.01 (0.99–1.02) | 0.412 | 1.01 (0.996–1.02) | 0.191 | 1.01 (0.99–1.02) | 0.508 |
| BMI (continuous) | 0.93 (0.89–0.98) | 0.003 | 0.92 (0.88–0.96) | <0.001 | 0.94 (0.90–0.98) | 0.003 |
| Smoking status | ||||||
| Former/never | 1 | 1 | 1 | |||
| Current | 1.54 (1.05–2.25) | 0.028 | 1.62 (1.18–2.24) | 0.003 | 1.55 (1.08–2.21) | 0.016 |
| Alcohol abuse | ||||||
| Former/never | 1 | 1 | 1 | |||
| Current | 1.83 (1.29–2.59) | 0.001 | 2.04 (1.52–2.73) | <0.001 | 1.65 (1.19–2.29) | 0.003 |
| Tumor site | ||||||
| Oropharynx | 1 | 1 | 1 | |||
| Oral cavity | 1.82 (1.29–2.58) | 0.001 | 1.29 (0.96–1.72) | 0.092 | 1.90 (1.37–2.63) | <0.001 |
| Tumor grade | ||||||
| G 1/2 | 1 | 1 | 1 | |||
| G 3/4 | 1.04 (0.74–1.48) | 0.807 | 0.98 (0.73–1.31) | 0.889 | 0.89 (0.65–1.24) | 0.502 |
| Tumor stage | ||||||
| T 1/2 | 1 | 1 | 1 | |||
| T 3/4 | 2.24 (1.52–3.31) | <0.001 | 1.96 (1.43–2.68) | <0.001 | 2.80 (1.91–4.12) | <0.001 |
| Nodal involvement | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 1.07 (0.68–1.70) | 0.774 | 1.02 (0.70–1.48) | 0.928 | 0.95 (0.63–1.43) | 0.787 |
| Surgery | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 0.39 (0.27–0.56) | <0.001 | 0.43 (0.32–0.58) | <0.001 | 0.29 (0.21–0.42) | <0.001 |
| Induction chemotherapy | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 1.52 (1.001–2.29) | 0.049 | 1.20 (0.83–1.73) | 0.341 | 1.61 (1.09–2.38) | 0.016 |
| Concomitant chemotherapy | ||||||
| No | ||||||
| Yes | 0.98 (0.68–1.40) | 0.898 | 1.05 (0.78–1.42) | 0.738 | 0.94 (0.68–1.31) | 0.721 |
| NLR (continuous) | 1.035 (0.975–1.098) | 0.257 | 1.047 (0.998–1.097) | 0.059 | 1.026 (0.969–1.086) | 0.38 |
| PLR (continuous) | 1.002 (1.000–1.003) | 0.038 | 1.001 (1.000–1.002) | 0.149 | 1.001 (1.000–1.003) | 0.186 |
| CRP (continuous) | 1.009 (1.005–1.013) | <0.001 | 1.008 (1.003–1.013) | 0.002 | 1.007 (1.003–1.012) | 0.002 |
| CRP | ||||||
| <5 | 1 | 1 | 1 | |||
| ≥5 | 1.95 (1.37–2.78) | <0.001 | 1.85 (1.38–2.47) | <0.001 | 1.73 (1.25–2.40) | 0.001 |
| Criterion * | Cancer-Specific Survival | Overall Survival | Loco-Regional Control | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| BMI (continuous) | 0.96 (0.92–1.01) | 0.134 | 0.93 (0.90–0.97) | 0.001 | 0.97 (0.93–1.01) | 0.181 |
| Smoking status | ||||||
| Former/never | 1 | 1 | 1 | |||
| Current | 1.08 (0.67–1.74) | 0.748 | 1.07 (0.72–1.59) | 0.723 | 1.15 (0.75–1.78) | 0.526 |
| Alcohol abuse | ||||||
| Former/never | 1 | 1 | 1 | |||
| Current | 1.55 (1.03–2.34) | 0.037 | 1.55 (1.10–2.20) | 0.012 | 1.52 (1.04–2.21) | 0.03 |
| Tumor site | ||||||
| Oropharynx | 1 | 1 | ||||
| Oral cavity | 1.99 (1.34-2.94) | 0.001 | - | - | 2.30 (1.59–3.32) | <0.001 |
| Tumor stage | ||||||
| T 1/2 | 1 | 1 | 1 | |||
| T 3/4 | 1.16 (0.70–1.91) | 0.565 | 1.02 (0.68–1.54) | 0.919 | 1.67 (1.04–2.68) | 0.035 |
| Surgery | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 0.39 (0.23–0.64) | <0.001 | 0.460 (0.31–0.69) | <0.001 | 0.34 (0.22–0.55) | <0.001 |
| Induction chemotherapy | ||||||
| No | 1 | 1 | ||||
| Yes | 1.08 (0.67–1.75) | 0.76 | - | - | 1.06 (0.68–1.65) | 0.804 |
| PLR (continuous) | 1.001 (0.999-1.003) | 0.239 | - | - | - | - |
| CRP | ||||||
| <5 | 1 | 1 | 1 | |||
| ≥5 | 1.60 (1.08–2.37) | 0.019 | 1.62 (1.17–2.24) | 0.004 | 1.51 (1.60–2.15) | 0.023 |
| Criterion * | Cancer-Specific Survival | Overall Survival | Loco-Regional Control | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | P-Value | HR (95% CI) | p-Value | |
| BMI (continuous) | 0.96 (0.90–1.01) | 0.135 | 0.94 (0.90–0.99) | 0.015 | 0.97 (0.92–1.02) | 0.233 |
| Smoking status | ||||||
| Former/never | 1 | 1 | 1 | |||
| Current | 1.18 (0.66–2.09) | 0.574 | 0.94 (0.59–1.51) | 0.806 | 1.34 (0.80–2.23) | 0.269 |
| Alcohol abuse | ||||||
| Former/never | 1 | 1 | 1 | |||
| Current | 1.80 (1.10–2.92) | 0.019 | 1.79 (1.17–2.74) | 0.007 | 1.80 (1.16–2.80) | 0.009 |
| Primary site | ||||||
| Oropharynx | 1 | 1 | ||||
| Oral cavity | 1.65 (1.02–2.67) | 0.041 | - | - | 1.73 (1.1–2.73) | 0.018 |
| Concomitant chemotherapy | ||||||
| No | 1 | 1 | ||||
| Yes | - | - | 0.55 (0.35–0.87) | 0.01 | 0.59 (0.36–0.97) | 0.037 |
| CRP | ||||||
| <5 | 1 | 1 | 1 | |||
| ≥5 | 1.77 (1.09–2.89) | 0.022 | 1.75 (1.15–2.67) | 0.009 | 1.55 (1.01–2.39) | 0.046 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knittelfelder, O.; Delago, D.; Jakse, G.; Lukasiak, K.; Thurner, E.-M.; Thurnher, D.; Pichler, M.; Renner, W.; Stranzl-Lawatsch, H.; Langsenlehner, T. The Pre-Treatment C-Reactive Protein Represents a Prognostic Factor in Patients with Oral and Oropharyngeal Cancer Treated with Radiotherapy. Cancers 2020, 12, 626. https://doi.org/10.3390/cancers12030626
Knittelfelder O, Delago D, Jakse G, Lukasiak K, Thurner E-M, Thurnher D, Pichler M, Renner W, Stranzl-Lawatsch H, Langsenlehner T. The Pre-Treatment C-Reactive Protein Represents a Prognostic Factor in Patients with Oral and Oropharyngeal Cancer Treated with Radiotherapy. Cancers. 2020; 12(3):626. https://doi.org/10.3390/cancers12030626
Chicago/Turabian StyleKnittelfelder, Olivia, Daniela Delago, Gabriele Jakse, Katarzyna Lukasiak, Eva-Maria Thurner, Dietmar Thurnher, Martin Pichler, Wilfried Renner, Heidi Stranzl-Lawatsch, and Tanja Langsenlehner. 2020. "The Pre-Treatment C-Reactive Protein Represents a Prognostic Factor in Patients with Oral and Oropharyngeal Cancer Treated with Radiotherapy" Cancers 12, no. 3: 626. https://doi.org/10.3390/cancers12030626
APA StyleKnittelfelder, O., Delago, D., Jakse, G., Lukasiak, K., Thurner, E.-M., Thurnher, D., Pichler, M., Renner, W., Stranzl-Lawatsch, H., & Langsenlehner, T. (2020). The Pre-Treatment C-Reactive Protein Represents a Prognostic Factor in Patients with Oral and Oropharyngeal Cancer Treated with Radiotherapy. Cancers, 12(3), 626. https://doi.org/10.3390/cancers12030626






