Performance of Comprehensive Complication Index and Clavien-Dindo Complication Scoring System in Liver Surgery for Hepatocellular Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Material and Methods
2.1. Study Overview and Population
2.2. Variables and Definitions
2.3. Endpoints
2.4. Statistical Analysis
3. Results
3.1. Descriptive Findings
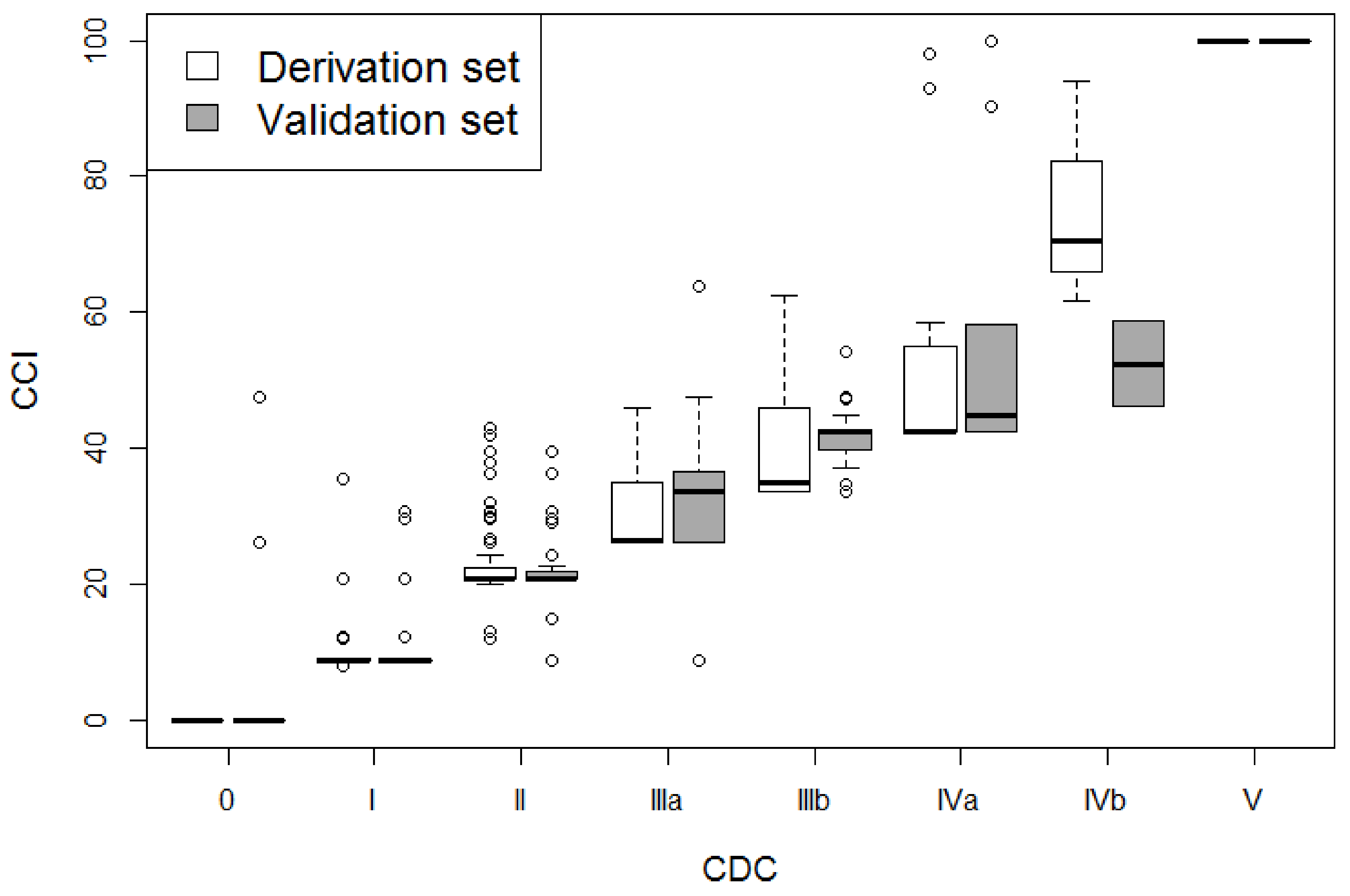
3.2. Association of CCI and CDC with Postoperative LOS and e-LOS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- El-Serag, H.B. Hepatocellular carcinoma. N. Engl. J. Med. 2011, 365, 1118–1127. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. European Organisation for Research and Treatment of Cancer EASL–EORTC Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2012, 56, 908–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mavros, M.N.; de Jong, M.; Dogeas, E.; Hyder, O.; Pawlik, T.M. Impact of complications on long-term survival after resection of colorectal liver metastases. Br. J. Surg. 2013, 100, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Mayo, S.C.; Heckman, J.E.; Shore, A.D.; Nathan, H.; Parikh, A.A.; Bridges, J.F.P.; Anders, R.A.; Anaya, D.A.; Becker, N.S.; Pawlik, T.M. Shifting trends in liver-directed management of patients with colorectal liver metastasis: A population-based analysis. Surgery 2011, 150, 204–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mezhir, J. Failure to rescue as a source of variation in hospital mortality after hepatic surgery. Br. J. Surg. 2014, 101, 836–846. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Slankamenac, K.; Graf, R.; Barkun, J.; Puhan, M.A.; Clavien, P.-A. The comprehensive complication index: A novel continuous scale to measure surgical morbidity. Ann. Surg. 2013, 258, 1–7. [Google Scholar] [CrossRef] [Green Version]
- De la Plaza Llamas, R.; Ramia Ángel, J.M.; Bellón, J.M.; Peralta, V.A.; Amador, C.G.; López Marcano, A.J.; Medina Velasco, A.A.; Sierra, B.G.; Vázquez, A.M. Clinical Validation of the Comprehensive Complication Index as a Measure of Postoperative Morbidity at a Surgical Department. Ann. Surg. 2018, 268, 838–844. [Google Scholar] [CrossRef]
- Staiger, R.D.; Cimino, M.; Javed, A.; Biondo, S.; Fondevila, C.; Périnel, J.; Aragão, A.C.; Torzilli, G.; Wolfgang, C.; Adham, M.; et al. The Comprehensive Complication Index (CCI®) is a Novel Cost Assessment Tool for Surgical Procedures. Ann. Surg. 2018, 268, 784–791. [Google Scholar] [CrossRef] [Green Version]
- Ray, S.; Mehta, N.N.; Mangla, V.; Lalwani, S.; Mehrotra, S.; Chugh, P.; Yadav, A.; Nundy, S. A Comparison between the Comprehensive Complication Index and the Clavien-Dindo Grading as a Measure of Postoperative Outcome in Patients Undergoing Gastrointestinal Surgery-A Prospective Study. J. Surg. Res. 2019, 244, 417–424. [Google Scholar] [CrossRef]
- Veličković, J.; Feng, C.; Palibrk, I.; Veličković, D.; Jovanović, B.; Bumbaširević, V. The Assessment of Complications After Major Abdominal Surgery: A Comparison of Two Scales. J. Surg. Res. 2020, 247, 397–405. [Google Scholar] [CrossRef]
- Park, J.H.; Kim, D.J.; Kim, M.H.; Park, J.K.; Choi, S.H.; Lee, S. Validation of comprehensive complication index in the general surgery department of a small-volume hospital: A prospective observational study. Asian J. Surg. 2019, 42, 1009–1016. [Google Scholar] [CrossRef]
- De la Plaza Llamas, R.; Ramia, J.M. Postoperative complications in gastrointestinal surgery: A “hidden” basic quality indicator. World J. Gastroenterol. 2019, 25, 2833–2838. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strasberg, S.M.; Belghiti, J.; Clavien, P.A.; Gadzijev, E.; Garden, J.O.; Lau, W.Y.; Makuuchi, M.; Strong, R.W. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB 2000, 2, 333–339. [Google Scholar] [CrossRef]
- Famularo, S.; Di Sandro, S.; Giani, A.; Lauterio, A.; Sandini, M.; De Carlis, R.; Buscemi, V.; Romano, F.; Gianotti, L.; De Carlis, L. Long-term oncologic results of anatomic vs. parenchyma-sparing resection for hepatocellular carcinoma. A propensity score-matching analysis. Eur. J. Surg. Oncol. 2018, 44, 1580–1587. [Google Scholar] [CrossRef] [PubMed]
- Torzilli, G.; Viganò, L.; Giuliante, F.; Pinna, A.D. Liver surgery in Italy: Criteria to identify the hospital units and the tertiary referral centers entitled to perform it. Updates Surg. 2016, 68, 135–142. [Google Scholar] [CrossRef] [PubMed]
- De La Plaza Llamas, R.; Hidalgo Vega, Á.; Latorre Fragua, R.A.; López Marcano, A.J.; Medina Velasco, A.A.; Díaz Candelas, D.A.; García Gil, J.M.; Ramia Ángel, J.M. The Cost Of Postoperative Complications And Economic Validation Of The Comprehensive Complication Index: Prospective Study. Ann. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Slankamenac, K.; Nederlof, N.; Pessaux, P.; de Jonge, J.; Wijnhoven, B.P.L.; Breitenstein, S.; Oberkofler, C.E.; Graf, R.; Puhan, M.A.; Clavien, P.-A. The comprehensive complication index: A novel and more sensitive endpoint for assessing outcome and reducing sample size in randomized controlled trials. Ann. Surg. 2014, 260, 757–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricci, C.; Ingaldi, C.; Grego, D.G.; Alberici, L.; De Raffele, E.; Pagano, N.; Mosconi, C.; Di Marco, M.; Palloni, A.; Brandi, G.; et al. The use of comprehensive complication Index® in pancreatic surgery: A comparison with the Clavien-Dindo system in a high-volume center. HPB 2020. [Google Scholar] [CrossRef]
- Famularo, S.; Di Sandro, S.; Giani, A.; Angrisani, M.; Lauterio, A.; Romano, F.; Gianotti, L.; De Carlis, L. The impact of age and ageing on hepatocarcinoma surgery: Short- and long-term outcomes in a multicentre propensity-matched cohort. Liver Int. 2019, 39, 894–904. [Google Scholar] [CrossRef] [PubMed]
- Kusano, T.; Sasaki, A.; Kai, S.; Endo, Y.; Iwaki, K.; Shibata, K.; Ohta, M.; Kitano, S. Predictors and prognostic significance of operative complications in patients with hepatocellular carcinoma who underwent hepatic resection. Eur. J. Surg. Oncol. 2009, 35, 1179–1185. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Zhang, J.; Lu, J.-H.; Yang, G.-S.; Wu, M.-C.; Yu, W.-F. Risk factors influencing postoperative outcomes of major hepatic resection of hepatocellular carcinoma for patients with underlying liver diseases. World J. Surg. 2011, 35, 2073–2082. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.-H.; Suh, Y.-S.; Huh, Y.-J.; Son, Y.-G.; Park, J.-H.; Yang, J.-Y.; Kong, S.-H.; Ahn, H.S.; Lee, H.-J.; Slankamenac, K.; et al. The comprehensive complication index (CCI) is a more sensitive complication index than the conventional Clavien–Dindo classification in radical gastric cancer surgery. Gastric Cancer 2018, 21, 171–181. [Google Scholar] [CrossRef]
- Zhu, F.; Feng, D.; Zhang, T.; Gu, L.; Zhu, W.; Guo, Z.; Li, Y.; Gong, J.; Li, N.; Li, J. Toward a More Sensitive Endpoint for Assessing Postoperative Complications in Patients with Inflammatory Bowel Disease: A Comparison Between Comprehensive Complication Index (CCI) and Clavien-Dindo Classification (CDC). J. Gastrointest. Surg. 2018, 22, 1593–1602. [Google Scholar] [CrossRef]
- Vetterlein, M.W.; Klemm, J.; Gild, P.; Bradtke, M.; Soave, A.; Dahlem, R.; Fisch, M.; Rink, M. Improving Estimates of Perioperative Morbidity After Radical Cystectomy Using the European Association of Urology Quality Criteria for Standardized Reporting and Introducing the Comprehensive Complication Index. Eur. Urol. 2020, 77, 55–65. [Google Scholar] [CrossRef]
- Slaman, A.E.; Lagarde, S.M.; Gisbertz, S.S.; van Berge Henegouwen, M.I. A Quantified Scoring System for Postoperative Complication Severity Compared to the Clavien-Dindo Classification. Dig. Surg. 2015, 32, 361–366. [Google Scholar] [CrossRef] [Green Version]
- Kalisvaart, M.; de Haan, J.E.; Polak, W.G.; Metselaar, H.J.; Wijnhoven, B.P.L.; IJzermans, J.N.M.; de Jonge, J. Comparison of Postoperative Outcomes Between Donation after Circulatory Death and Donation After Brain Death Liver Transplantation Using the Comprehensive Complication Index. Ann. Surg. 2017, 266, 772–778. [Google Scholar] [CrossRef]
- Tu, R.-H.; Lin, J.-X.; Li, P.; Xie, J.-W.; Wang, J.-B.; Lu, J.; Chen, Q.-Y.; Cao, L.-L.; Lin, M.; Zheng, C.-H.; et al. Comprehensive Complication Index Predicts Cancer-Specific Survival of Patients with Postoperative Complications after Curative Resection of Gastric Cancer. Gastroenterol. Res. Pract. 2018, 4396018. [Google Scholar] [CrossRef] [Green Version]
- Dumitra, T.C.; Trepanier, M.; Fiore, J.F., Jr.; Kaneva, P.; Carli, F.; Fried, G.M.; Feldman, L.S.; Lee, L. The relationship of two postoperative complication grading schemas with postoperative quality of life after elective colorectal surgery. Surgery 2019, 166, 663–669. [Google Scholar] [CrossRef]
- Cloyd, J.M.; Mizuno, T.; Kawaguchi, Y.; Lillemoe, H.A.; Karagkounis, G.; Omichi, K.; Chun, Y.S.; Conrad, C.; Tzeng, C.-W.D.; Odisio, B.C.; et al. Comprehensive Complication Index Validates Improved Outcomes Over Time Despite Increased Complexity in 3707 Consecutive Hepatectomies. Ann. Surg. 2020, 271, 724–731. [Google Scholar] [CrossRef] [PubMed]


| Variables | Derivation Set (N = 1345) | Validation Set (N = 1324) | ||
|---|---|---|---|---|
| Median [IQR] or n (%) | Missing (%) | Median [IQR] or n (%) | Missing (%) | |
| Age | 70.0 [63.0, 75.0] | 1.2 | 69.8 [62.4, 75.1] | 0.7 |
| Females | 328 (24.4) | 0 | 271 (20.5) | 0 |
| American Society of Anesthesiologists score | 2.7 | 4.7 | ||
| 1 | 16 (1.2) | 50 (4.0) | ||
| 2 | 682 (52.1) | 550 (43.6) | ||
| ≥3 | 611 (46.7) | 662 (52.5) | ||
| Cirrhosis | 927 (70.5) | 2.3 | 741 (56.1) | 0.2 |
| Child-Pugh Grade | 3.9 | 0 | ||
| A | 1175 (90.9) | 1294 (97.1) | ||
| B | 118 (9.1) | 30 (2.3) | ||
| Surgery duration, min | 230 [170, 290] | 2.3 | 270 [200, 370] | 3.8 |
| Blood transfusion during surgery | 118 (9.1) | 3.3 | 181 (14.5) | 6.0 |
| Laparoscopy | 568 (42.2) | 0 | 268 (21.4) | 5.5 |
| Clavien-Dindo grading | 0 | 0 | ||
| 0 | 894 (66.5) | 789 (59.6) | ||
| I | 101 (7.5) | 155 (11.7) | ||
| II | 255 (19.0) | 236 (17.8) | ||
| IIIa | 40 (3.0) | 71 (5.4) | ||
| IIIb | 17 (1.3) | 31 (2.3) | ||
| IVa | 20 (1.5) | 18 (1.4) | ||
| IVb | 4 (0.3) | 4 (0.3) | ||
| V | 14 (1.0) | 20 (1.5) | ||
| Comprehensive Complication Index CCI > 0 | 20.9 [20.9, 26.6] | 0 | 20.9 [8.7, 29.6] | 0 |
| Length of hospitalization, days | 7.0 [5.0, 9.0] | 0 | 9.0 [7.0, 12.0] | 0 |
| HBV | 276 (21.4) | 4.0 | 213 (16.2) | 0.5 |
| HCV | 714 (55.3) | 4.1 | 544 (41.3) | 0.4 |
| Bilirubin, mg/dL | 0.90 [0.63, 1.23] | 1.8 | 0.80 [0.60, 1.01] | 1.4 |
| Albumin, g/dL | 3.80 [3.50, 4.21] | 3.4 | 4.00 [3.80, 4.30] | 2.7 |
| Platelets, 10^3/mm3 | 169.0 [117.0, 230.0] | 1.8 | 170.0 [123.0, 223.8] | 0.5 |
| International Normalized Ratio | 1.12 [1.03, 1.29] | 1.9 | 1.08 [1.02, 1.15] | 1.3 |
| Number of nodules | 0.1 | 3.9 | ||
| 1 | 1068 (79.5) | 973 (76.4) | ||
| 2 | 202 (15.0) | 186 (14.6) | ||
| 3 | 56 (4.2) | 71 (5.6) | ||
| 4 | 12 (0.9) | 25 (2.0) | ||
| 5 | 5 (0.4) | 5 (0.4) | ||
| ≥6 | 1 (0.1) | 13 (1.0) | ||
| Size of bigger nodule, cm | 4.0 [2.9, 6.0] | 0.4 | 4.0 [2.5, 6.3] | 1.9 |
| Major surgery | 293 (21.8) | 0.3 | 263 (20.1) | 1.1 |
| Surgical procedure | 0.5 | 0.2 | ||
| Parenchyma-sparing resection | 400 (29.9) | 579 (43.8) | ||
| Segmentecnomy | 437 (32.6) | 325 (24.6) | ||
| Right hepatectomy | 129 (9.6) | 115 (8.7) | ||
| Left hepatectomy | 106 (7.9) | 81 (6.1) | ||
| Right posterior sectionectomy | 32 (2.4) | 19 (1.4) | ||
| Right anterior sectionectomy | 58 (4.3) | 32 (2.4) | ||
| Left lateral sectionectomy | 85 (6.3) | 52 (3.9) | ||
| Right trisectionectomy | 13 (1.0) | 14 (1.1) | ||
| Left trisectionectomy | 6 (0.4) | 1 (0.1) | ||
| Other | 72 (5.4) | 104 (7.9) | ||
| Number of complications | 0 | 0 | ||
| 0 | 894 (66.5) | 787 (59.4) | ||
| 1 | 260 (19.3) | 363 (27.4) | ||
| ≥2 | 191 (14.2) | 174 (13.1) | ||
| Center volume | 0 | 0 | ||
| Low | 108 (8.0) | 113 (8.5) | ||
| Medium | 608 (45.2) | 180 (13.6) | ||
| High | 629 (46.8) | 1031 (77.9) | ||
| Sample | Model | Derivation Set | Validation Set | |||
|---|---|---|---|---|---|---|
| Mean Change (95% CI) | R2 | RMSE | R2 | RMSE | ||
| Overall sample Derivation set n = 1331. Validation set n = 1304. | CCI, per 10 unit increase Univariate model | 0.290 (0.273;0.307) | 45% | 0.41 | 36% | 0.49 |
| Clavien-Dindo, per category increase Univariate model | 0.312 (0.292;0.332) | 41% | 0.43 | 34% | 0.49 | |
| CCI, per 10 unit increase Multivariate model | 0.267 (0.251;0.282) | 57% | 0.37 | 44% | 0.50 | |
| Clavien-Dindo, per category increase Multivariate model | 0.291 (0.273;0.309) | 54% | 0.38 | 43% | 0.51 | |
| Subgroup of patients with at least two complications Derivation set n = 177. Validation set n = 154. | CCI, per 10 unit increase Univariate model | 0.240 (0.197;0.283) | 41% | 0.47 | 15% | 0.59 |
| Clavien-Dindo, per category increase Univariate model | 0.254 (0.186;0.323) | 24% | 0.54 | 12% | 0.59 | |
| CCI, per 10 unit increase Multivariate model | 0.219 (0.176;0.262) | 47% | 0.45 | 23% | 0.59 | |
| Clavien-Dindo, per category increase Multivariate model | 0.223 (0.157;0.289) | 32% | 0.52 | 21% | 0.63 | |
| Sample | Model | Derivation Set | Validation Set | |
|---|---|---|---|---|
| OR (95% CI) | AUC | AUC | ||
| Overall sample Derivation set n = 1331. Validation set n = 1304. | CCI, per 10 unit increase Univariate model | 5.826 (4.402;7.709) | 96.1% | 87.7% |
| Clavien-Dindo, per category increase Univariate model | 5.298 (4.067;6.902) | 94.0% | 86.9% | |
| CCI, per 10 unit increase Multivariate model | 5.590 (4.201;7.438) | 96.4% | 89.3% | |
| Clavien-Dindo, per category increase Multivariate model | 5.507 (4.152;7.304) | 96.2% | 89.0% | |
| Subgroup of patients with at least two complications Derivation set n = 177. Validation set n = 154. | CCI, per 10 unit increase Univariate model | 3.003 (2.085;4.327) | 83.0% | 67.1% |
| Clavien-Dindo, per category increase Univariate model | 2.638 (1.794;3.878) | 76.5% | 65.2% | |
| CCI, per 10 unit increase Multivariate model | 2.793 (1.896;4.115) | 85.0% | 67.3% | |
| Clavien-Dindo, per category increase Multivariate model | 2.439 (1.666;3.57) | 80.6% | 65.8% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giani, A.; Cipriani, F.; Famularo, S.; Donadon, M.; Bernasconi, D.P.; Ardito, F.; Fazio, F.; Nicolini, D.; Perri, P.; Giuffrida, M.; et al. Performance of Comprehensive Complication Index and Clavien-Dindo Complication Scoring System in Liver Surgery for Hepatocellular Carcinoma. Cancers 2020, 12, 3868. https://doi.org/10.3390/cancers12123868
Giani A, Cipriani F, Famularo S, Donadon M, Bernasconi DP, Ardito F, Fazio F, Nicolini D, Perri P, Giuffrida M, et al. Performance of Comprehensive Complication Index and Clavien-Dindo Complication Scoring System in Liver Surgery for Hepatocellular Carcinoma. Cancers. 2020; 12(12):3868. https://doi.org/10.3390/cancers12123868
Chicago/Turabian StyleGiani, Alessandro, Federica Cipriani, Simone Famularo, Matteo Donadon, Davide Paolo Bernasconi, Francesco Ardito, Federico Fazio, Daniele Nicolini, Pasquale Perri, Mario Giuffrida, and et al. 2020. "Performance of Comprehensive Complication Index and Clavien-Dindo Complication Scoring System in Liver Surgery for Hepatocellular Carcinoma" Cancers 12, no. 12: 3868. https://doi.org/10.3390/cancers12123868
APA StyleGiani, A., Cipriani, F., Famularo, S., Donadon, M., Bernasconi, D. P., Ardito, F., Fazio, F., Nicolini, D., Perri, P., Giuffrida, M., Pontarolo, N., Zanello, M., Lai, Q., Conci, S., Molfino, S., Germani, P., Pinotti, E., Romano, M., La Barba, G., ... Gianotti, L. (2020). Performance of Comprehensive Complication Index and Clavien-Dindo Complication Scoring System in Liver Surgery for Hepatocellular Carcinoma. Cancers, 12(12), 3868. https://doi.org/10.3390/cancers12123868













