Promising Therapy in Lung Cancer: Spotlight on Aurora Kinases
Abstract
Simple Summary
Abstract
1. Background
2. Cellular Localization and Functions of Aurora Kinases
3. Pre-Clinical Studies on Aurora Kinases
3.1. Overexpression of AURKA and AURKB Correlates with Unfavorable Therapeutic Response in Lung Cancer
3.2. Impact of AURKA and AURKB in Chemo- and Radiotherapy in Lung Cancer
3.3. Inhibition of AURKA and AURKB Suppresses Their Pro-Tumorigenic Actions in Lung Cancer
4. Aurora Kinase Inhibitors in Clinical Studies
5. Conclusions and Perspectives
Funding
Acknowledgments
Conflicts of Interest
References
- Bertran-Alamillo, J.; Cattan, V.; Schoumacher, M.; Codony-Servat, J.; Giménez-Capitán, A.; Cantero, F.; Burbridge, M.; Rodríguez, S.; Teixidó, C.; Roman, R.; et al. AURKB as a target in non-small cell lung cancer with acquired resistance to anti-EGFR therapy. Nat. Commun. 2019, 10, 1–14. [Google Scholar] [CrossRef]
- Mascaux, C.; Tomasini, P.; Greillier, L.; Barlesi, F. Personalised medicine for nonsmall cell lung cancer. Eur. Respir. Rev. 2017, 26. [Google Scholar] [CrossRef]
- Zappa, C.; Mousa, S.A. Non-small cell lung cancer: Current treatment and future advances. Transl. Lung Cancer Res. 2016, 5, 288–300. [Google Scholar] [CrossRef]
- Neal, R.D.; Sun, F.; Emery, J.D.; Callister, M.E. Lung cancer. BMJ 2019, 365. [Google Scholar] [CrossRef]
- Ohe, Y. Chemoradiotherapy for lung cancer: Current status and perspectives. Int. J. Clin. Oncol. 2004, 9, 435–443. [Google Scholar] [CrossRef]
- Zhang, C.; Leighl, N.B.; Wu, Y.-L.; Zhong, W.-Z. Emerging therapies for non-small cell lung cancer. J. Hematol. Oncol. 2019, 12, 45. [Google Scholar] [CrossRef]
- Hirsch, F.R.; Scagliotti, G.V.; Mulshine, J.L.; Kwon, R.; Curran, W.J.; Wu, Y.-L.; Paz-Ares, L. Lung cancer: Current therapies and new targeted treatments. Lancet 2017, 389, 299–311. [Google Scholar] [CrossRef]
- Ramalingam, S.; Belani, C. Systemic Chemotherapy for Advanced Non-Small Cell Lung Cancer: Recent Advances and Future Directions. Oncologist 2008, 13, 5–13. [Google Scholar] [CrossRef]
- Gridelli, C.; de Marinis, F.; Cappuzzo, F.; Maio, M.D.; Hirsch, F.R.; Mok, T.; Morgillo, F.; Rosell, R.; Spigel, D.R.; Yang, J.C.-H.; et al. Treatment of Advanced Non–Small-Cell Lung Cancer With Epidermal Growth Factor Receptor (EGFR) Mutation or ALK Gene Rearrangement: Results of an International Expert Panel Meeting of the Italian Association of Thoracic Oncology. Clin. Lung Cancer 2014, 15, 173–181. [Google Scholar] [CrossRef]
- Remon, J.; Passiglia, F.; Ahn, M.-J.; Barlesi, F.; Forde, P.M.; Garon, E.B.; Gettinger, S.; Goldberg, S.B.; Herbst, R.S.; Horn, L.; et al. Immune Checkpoint Inhibitors in Thoracic Malignancies: Review of the Existing Evidence by an IASLC Expert Panel and Recommendations. J. Thorac. Oncol. 2020, 15, 914–947. [Google Scholar] [CrossRef]
- Yuan, M.; Huang, L.-L.; Chen, J.-H.; Wu, J.; Xu, Q. The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal. Transduct. Target. Ther. 2019, 4, 1–14. [Google Scholar] [CrossRef]
- Dar, A.A.; Goff, L.W.; Majid, S.; Berlin, J.; El-Rifai, W. Aurora Kinase Inhibitors-Rising Stars in Cancer Therapeutics? Mol. Cancer Ther. 2010, 9, 268–278. [Google Scholar] [CrossRef]
- D’Assoro, A.B.; Haddad, T.; Galanis, E. Aurora-A Kinase as a Promising Therapeutic Target in Cancer. Front. Oncol. 2016, 5. [Google Scholar] [CrossRef]
- Lo Iacono, M.; Monica, V.; Saviozzi, S.; Ceppi, P.; Bracco, E.; Papotti, M.; Scagliotti, G.V. Aurora Kinase A expression is associated with lung cancer histological-subtypes and with tumor de-differentiation. J. Transl. Med. 2011, 9, 100. [Google Scholar] [CrossRef][Green Version]
- Katayama, H.; Sen, S. Aurora kinase inhibitors as anticancer molecules. Biochim. Biophys. Acta BBA Gene Regul. Mech. 2010, 1799, 829–839. [Google Scholar] [CrossRef]
- Liu, N.; Wang, Y.A.; Sun, Y.; Ecsedy, J.; Sun, J.; Li, X.; Wang, P. Inhibition of Aurora A enhances radiosensitivity in selected lung cancer cell lines. Respir. Res. 2019, 20, 230. [Google Scholar] [CrossRef]
- Zhang, M.-Y.; Liu, X.-X.; Li, H.; Li, R.; Liu, X.; Qu, Y.-Q. Elevated mRNA Levels of AURKA, CDC20 and TPX2 are associated with poor prognosis of smoking related lung adenocarcinoma using bioinformatics analysis. Int. J. Med. Sci. 2018, 15, 1676–1685. [Google Scholar] [CrossRef]
- Al-Khafaji, A.S.K.; Marcus, M.W.; Davies, M.P.A.; Risk, J.M.; Shaw, R.J.; Field, J.K.; Liloglou, T. AURKA mRNA expression is an independent predictor of poor prognosis in patients with non-small cell lung cancer. Oncol. Lett. 2017, 13, 4463–4468. [Google Scholar] [CrossRef]
- Schneider, M.A.; Christopoulos, P.; Muley, T.; Warth, A.; Klingmueller, U.; Thomas, M.; Herth, F.J.F.; Dienemann, H.; Mueller, N.S.; Theis, F.; et al. AURKA, DLGAP5, TPX2, KIF11 and CKAP5: Five specific mitosis-associated genes correlate with poor prognosis for non-small cell lung cancer patients. Int. J. Oncol. 2017, 50, 365–372. [Google Scholar] [CrossRef]
- Li, X.; Liu, N.; Ren, P.; Cao, Q.; Wang, P.; Zhao, L.; Lu, B.; Wang, P. Prognostic value of combined expression of Aurora A, p53 and p21 WAF1 in patients after curative resection of non-small cell lung cancer. Zhonghua Zhong Liu Za Zhi 2015, 37, 512–516. [Google Scholar]
- Xu, J.; Yue, C.; Zhou, W.; Qian, Y.; Zhang, Y.; Wang, S.; Liu, A.; Liu, Q. Aurora-A contributes to cisplatin resistance and lymphatic metastasis in non-small cell lung cancer and predicts poor prognosis. J. Transl. Med. 2014, 12, 200. [Google Scholar] [CrossRef]
- Takeshita, M.; Koga, T.; Takayama, K.; Ijichi, K.; Yano, T.; Maehara, Y.; Nakanishi, Y.; Sueishi, K. Aurora-B overexpression is correlated with aneuploidy and poor prognosis in non-small cell lung cancer. Lung Cancer Amst. Neth. 2013, 80, 85–90. [Google Scholar] [CrossRef]
- Hayama, S.; Daigo, Y.; Yamabuki, T.; Hirata, D.; Kato, T.; Miyamoto, M.; Ito, T.; Tsuchiya, E.; Kondo, S.; Nakamura, Y. Phosphorylation and activation of cell division cycle associated 8 by aurora kinase B plays a significant role in human lung carcinogenesis. Cancer Res. 2007, 67, 4113–4122. [Google Scholar] [CrossRef]
- Vischioni, B.; Oudejans, J.J.; Vos, W.; Rodriguez, J.A.; Giaccone, G. Frequent overexpression of aurora B kinase, a novel drug target, in non-small cell lung carcinoma patients. Mol. Cancer Ther. 2006, 5, 2905–2913. [Google Scholar] [CrossRef]
- Shah, K.N.; Bhatt, R.; Rotow, J.; Rohrberg, J.; Olivas, V.; Wang, V.E.; Hemmati, G.; Martins, M.M.; Maynard, A.; Kuhn, J.; et al. Aurora kinase A drives the evolution of resistance to third-generation EGFR inhibitors in lung cancer. Nat. Med. 2019, 25, 111–118. [Google Scholar] [CrossRef]
- Wu, C.C.; Yu, C.-T.R.; Chang, G.-C.; Lai, J.-M.; Hsu, S.-L. Aurora-A promotes gefitinib resistance via a NF-κB signaling pathway in p53 knockdown lung cancer cells. Biochem. Biophys. Res. Commun. 2011, 405, 168–172. [Google Scholar] [CrossRef]
- Orth, M.; Unger, K.; Schoetz, U.; Belka, C.; Lauber, K. Taxane-mediated radiosensitization derives from chromosomal missegregation on tripolar mitotic spindles orchestrated by AURKA and TPX2. Oncogene 2018, 37, 52–62. [Google Scholar] [CrossRef]
- Lapenna, S.; Giordano, A. Cell cycle kinases as therapeutic targets for cancer. Nat. Rev. Drug Discov. 2009, 8, 547–566. [Google Scholar] [CrossRef]
- Tang, A.; Gao, K.; Chu, L.; Zhang, R.; Yang, J.; Zheng, J. Aurora kinases: Novel therapy targets in cancers. Oncotarget 2017, 8, 23937–23954. [Google Scholar] [CrossRef]
- Li, S.; Deng, Z.; Fu, J.; Xu, C.; Xin, G.; Wu, Z.; Luo, J.; Wang, G.; Zhang, S.; Zhang, B.; et al. Spatial Compartmentalization Specializes the Function of Aurora A and Aurora B. J. Biol. Chem. 2015, 290, 17546–17558. [Google Scholar] [CrossRef]
- Ke, Y.W.; Dou, Z.; Zhang, J.; Yao, X.B. Function and regulation of Aurora/Ipl1p kinase family in cell division. Cell Res. 2003, 13, 69–81. [Google Scholar] [CrossRef]
- Giet, R.; Prigent, C. Aurora/Ipl1p-related kinases, a new oncogenic family of mitotic serine-threonine kinases. J. Cell Sci. 1999, 112 Pt 21, 3591–3601. [Google Scholar]
- Quartuccio, S.M.; Schindler, K. Functions of Aurora kinase C in meiosis and cancer. Front. Cell Dev. Biol. 2015, 3. [Google Scholar] [CrossRef]
- Hirota, T.; Kunitoku, N.; Sasayama, T.; Marumoto, T.; Zhang, D.; Nitta, M.; Hatakeyama, K.; Saya, H. Aurora-A and an Interacting Activator, the LIM Protein Ajuba, Are Required for Mitotic Commitment in Human Cells. Cell 2003, 114, 585–598. [Google Scholar] [CrossRef]
- Eyers, P.A.; Erikson, E.; Chen, L.G.; Maller, J.L. A novel mechanism for activation of the protein kinase Aurora A. Curr. Biol. CB 2003, 13, 691–697. [Google Scholar] [CrossRef]
- Baldini, E.; Tuccilli, C.; Sorrenti, S.; Mascagni, D.; Arcieri, S.; Filippini, A.; Ulisse, S. Aurora Kinases: New Molecular Targets for the Therapy of Aggressive Thyroid Cancers. Anti Cancer Drugs Nat. Synth. Cell 2016. [Google Scholar] [CrossRef]
- Bishop, J.D.; Schumacher, J.M. Phosphorylation of the Carboxyl Terminus of Inner Centromere Protein (INCENP) by the Aurora B Kinase Stimulates Aurora B Kinase Activity. J. Biol. Chem. 2002, 277, 27577–27580. [Google Scholar] [CrossRef]
- Carmena, M.; Earnshaw, W.C. The cellular geography of Aurora kinases. Nat. Rev. Mol. Cell Biol. 2003, 4, 842–854. [Google Scholar] [CrossRef]
- Willems, E.; Dedobbeleer, M.; Digregorio, M.; Lombard, A.; Lumapat, P.N.; Rogister, B. The functional diversity of Aurora kinases: A comprehensive review. Cell Div. 2018, 13. [Google Scholar] [CrossRef]
- Abdul Azeez, K.R.; Chatterjee, S.; Yu, C.; Golub, T.R.; Sobott, F.; Elkins, J.M. Structural mechanism of synergistic activation of Aurora kinase B/C by phosphorylated INCENP. Nat. Commun. 2019, 10, 1–11. [Google Scholar] [CrossRef]
- Fernández-Miranda, G.; Trakala, M.; Martín, J.; Escobar, B.; González, A.; Ghyselinck, N.B.; Ortega, S.; Cañamero, M.; Castro, I.P.d.; Malumbres, M. Genetic disruption of aurora B uncovers an essential role for aurora C during early mammalian development. Development 2011, 138, 2661–2672. [Google Scholar] [CrossRef]
- Yu, J.; Zhou, J.; Xu, F.; Bai, W.; Zhang, W. High expression of Aurora-B is correlated with poor prognosis and drug resistance in non-small cell lung cancer. Int. J. Biol. Markers 2018, 33, 215–221. [Google Scholar] [CrossRef]
- Wang, W.; Yang, S.; Lin, J.; Zeng, Z.; Liu, D.; Liu, H. Expression of Aurora-B in non-small cell lung cancer and its clinical significance. Nan Fang Yi Ke Da Xue Xue Bao 2009, 29, 1853–1856. [Google Scholar]
- Smith, S.L.; Bowers, N.L.; Betticher, D.C.; Gautschi, O.; Ratschiller, D.; Hoban, P.R.; Booton, R.; Santibáñez-Koref, M.F.; Heighway, J. Overexpression of aurora B kinase (AURKB) in primary non-small cell lung carcinoma is frequent, generally driven from one allele, and correlates with the level of genetic instability. Br. J. Cancer 2005, 93, 719–729. [Google Scholar] [CrossRef]
- Al-Khafaji, A.S.; Davies, M.P.; Risk, J.M.; Marcus, M.W.; Koffa, M.; Gosney, J.R.; Shaw, R.J.; Field, J.K.; Liloglou, T. Aurora B expression modulates paclitaxel response in non-small cell lung cancer. Br. J. Cancer 2017, 116, 592–599. [Google Scholar] [CrossRef]
- Bibby, A.C.; Tsim, S.; Kanellakis, N.; Ball, H.; Talbot, D.C.; Blyth, K.G.; Maskell, N.A.; Psallidas, I. Malignant pleural mesothelioma: An update on investigation, diagnosis and treatment. Eur. Respir. Rev. 2016, 25, 472–486. [Google Scholar] [CrossRef]
- Nicolini, F.; Bocchini, M.; Bronte, G.; Delmonte, A.; Guidoboni, M.; Crinò, L.; Mazza, M. Malignant Pleural Mesothelioma: State-of-the-Art on Current Therapies and Promises for the Future. Front. Oncol. 2020, 9. [Google Scholar] [CrossRef]
- Crispi, S.; Fagliarone, C.; Biroccio, A.; D’Angelo, C.; Galati, R.; Sacchi, A.; Vincenzi, B.; Baldi, A.; Verdina, A. Antiproliferative effect of Aurora kinase targeting in mesothelioma. Lung Cancer 2010, 70, 271–279. [Google Scholar] [CrossRef]
- López-Ríos, F.; Chuai, S.; Flores, R.; Shimizu, S.; Ohno, T.; Wakahara, K.; Illei, P.B.; Hussain, S.; Krug, L.; Zakowski, M.F.; et al. Global gene expression profiling of pleural mesotheliomas: Overexpression of aurora kinases and P16/CDKN2A deletion as prognostic factors and critical evaluation of microarray-based prognostic prediction. Cancer Res. 2006, 66, 2970–2979. [Google Scholar] [CrossRef]
- Liu, J.-B.; Hu, L.; Yang, Z.; Sun, Y.U.; Hoffman, R.M.; Yi, Z. Aurora-A/NF-ĸB Signaling Is Associated With Radio-resistance in Human Lung Adenocarcinoma. Anticancer Res. 2019, 39, 5991–5998. [Google Scholar] [CrossRef]
- Linardopoulos, S. Aurora-A kinase regulates NF-kappaB activity: Lessons from combination studies. J. Buon Off. J. Balk. Union Oncol. 2007, 12 (Suppl. S1), S67–S70. [Google Scholar]
- Sun, C.; Chan, F.; Briassouli, P.; Linardopoulos, S. Aurora kinase inhibition downregulates NF-kappaB and sensitises tumour cells to chemotherapeutic agents. Biochem. Biophys. Res. Commun. 2007, 352, 220–225. [Google Scholar] [CrossRef]
- Min, Y.H.; Kim, W.; Kim, J.-E. The Aurora kinase A inhibitor TC-A2317 disrupts mitotic progression and inhibits cancer cell proliferation. Oncotarget 2016, 7, 84718–84735. [Google Scholar] [CrossRef]
- McLaughlin, J.; Markovtsov, V.; Li, H.; Wong, S.; Gelman, M.; Zhu, Y.; Franci, C.; Lang, D.W.; Pali, E.; Lasaga, J.; et al. Preclinical characterization of Aurora kinase inhibitor R763/AS703569 identified through an image-based phenotypic screen. J. Cancer Res. Clin. Oncol. 2010, 136, 99–113. [Google Scholar] [CrossRef]
- Biran, A.; Brownstein, M.; Haklai, R.; Kloog, Y. Downregulation of survivin and aurora A by histone deacetylase and RAS inhibitors: A new drug combination for cancer therapy. Int. J. Cancer 2011, 128, 691–701. [Google Scholar] [CrossRef]
- Ma, Z.-L.; Zhang, B.-J.; Wang, D.T.; Li, X.; Wei, J.-L.; Zhao, B.-T.; Jin, Y.; Li, Y.-L.; Jin, Y.-X. Tanshinones suppress AURKA through up-regulation of miR-32 expression in non-small cell lung cancer. Oncotarget 2015, 6, 20111–20120. [Google Scholar] [CrossRef]
- Yu, C.-T.R.; Hsia, J.-Y.; Hseih, Y.-C.; Su, L.-J.; Lee, T.-C.; Ku, C.-F.; Chen, K.-S.; Chen, J.-M.M.; Wei, T.-Y.W.; Lee, Y.-C.G.; et al. The novel protein suppressed in lung cancer down-regulated in lung cancer tissues retards cell proliferation and inhibits the oncokinase Aurora-A. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2011, 6, 988–997. [Google Scholar] [CrossRef]
- Sak, A.; Stuschke, M.; Groneberg, M.; Kübler, D.; Pöttgen, C.; Eberhardt, W.E.E. Inhibiting the aurora B kinase potently suppresses repopulation during fractionated irradiation of human lung cancer cell lines. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 492–499. [Google Scholar] [CrossRef]
- Betta, P.; Bensi, T.; Trincheri, N.F.; Arnolfo, E.; Libener, R.; Botta, M.; Piccolini, E.; Bottero, G.; Grosso, F.; Orecchia, S. Aurora B kinase and malignant mesothelioma. J. Clin. Oncol. 2010, 28, e21021. [Google Scholar] [CrossRef]
- Wilkinson, R.W.; Odedra, R.; Heaton, S.P.; Wedge, S.R.; Keen, N.J.; Crafter, C.; Foster, J.R.; Brady, M.C.; Bigley, A.; Brown, E.; et al. AZD1152, a selective inhibitor of Aurora B kinase, inhibits human tumor xenograft growth by inducing apoptosis. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2007, 13, 3682–3688. [Google Scholar] [CrossRef]
- Kim, K.W.; Mutter, R.W.; Willey, C.D.; Subhawong, T.K.; Shinohara, E.T.; Albert, J.M.; Ling, G.; Cao, C.; Gi, Y.J.; Lu, B. Inhibition of survivin and aurora B kinase sensitizes mesothelioma cells by enhancing mitotic arrests. Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 1519–1525. [Google Scholar] [CrossRef]
- Clémenson, C.; Chargari, C.; Liu, W.; Mondini, M.; Ferté, C.; Burbridge, M.F.; Cattan, V.; Jacquet-Bescond, A.; Deutsch, E. The MET/AXL/FGFR Inhibitor S49076 Impairs Aurora B Activity and Improves the Antitumor Efficacy of Radiotherapy. Mol. Cancer Ther. 2017, 16, 2107–2119. [Google Scholar] [CrossRef]
- Xingyu, Z.; Peijie, M.; Dan, P.; Youg, W.; Daojun, W.; Xinzheng, C.; Xijun, Z.; Yangrong, S. Quercetin suppresses lung cancer growth by targeting Aurora B kinase. Cancer Med. 2016, 5, 3156–3165. [Google Scholar] [CrossRef]
- Xie, H.; Lee, M.-H.; Zhu, F.; Reddy, K.; Peng, C.; Li, Y.; Lim, D.Y.; Kim, D.J.; Li, X.; Kang, S.; et al. Identification of an Aurora kinase inhibitor specific for the Aurora B isoform. Cancer Res. 2013, 73, 716–724. [Google Scholar] [CrossRef]
- Li, X.; Li, H.; Li, S.; Zhu, F.; Kim, D.J.; Xie, H.; Li, Y.; Nadas, J.; Oi, N.; Zykova, T.A.; et al. Ceftriaxone, an FDA-approved cephalosporin antibiotic, suppresses lung cancer growth by targeting Aurora B. Carcinogenesis 2012, 33, 2548–2557. [Google Scholar] [CrossRef]
- Doello, S.; Liang, Z.; Cho, I.K.; Kim, J.B.; Li, Q.X. Cytotoxic Effects of 24-Methylenecyloartanyl Ferulate on A549 Nonsmall Cell Lung Cancer Cells through MYBBP1A Up-Regulation and AKT and Aurora B Kinase Inhibition. J. Agric. Food Chem. 2018, 66, 3726–3733. [Google Scholar] [CrossRef]
- Dos Santos, E.O.; Carneiro-Lobo, T.C.; Aoki, M.N.; Levantini, E.; Bassères, D.S. Aurora kinase targeting in lung cancer reduces KRAS-induced transformation. Mol. Cancer 2016, 15, 12. [Google Scholar] [CrossRef]
- Woo, J.K.; Kang, J.-H.; Shin, D.; Park, S.-H.; Kang, K.; Nho, C.W.; Seong, J.K.; Lee, S.-J.; Oh, S.H. Daurinol Enhances the Efficacy of Radiotherapy in Lung Cancer via Suppression of Aurora Kinase A/B Expression. Mol. Cancer Ther. 2015, 14, 1693–1704. [Google Scholar] [CrossRef]
- Hardwicke, M.A.; Oleykowski, C.A.; Plant, R.; Wang, J.; Liao, Q.; Moss, K.; Newlander, K.; Adams, J.L.; Dhanak, D.; Yang, J.; et al. GSK1070916, a potent Aurora B/C kinase inhibitor with broad antitumor activity in tissue culture cells and human tumor xenograft models. Mol. Cancer Ther. 2009, 8, 1808–1817. [Google Scholar] [CrossRef]
- Huang, M.; Feng, X.; Su, D.; Wang, G.; Wang, C.; Tang, M.; Paulucci-Holthauzen, A.; Hart, T.; Chen, J. Genome-wide CRISPR screen uncovers a synergistic effect of combining Haspin and Aurora kinase B inhibition. Oncogene 2020. [Google Scholar] [CrossRef]
- Melichar, B.; Adenis, A.; Lockhart, A.C.; Bennouna, J.; Dees, E.C.; Kayaleh, O.; Obermannova, R.; DeMichele, A.; Zatloukal, P.; Zhang, B.; et al. Safety and activity of alisertib, an investigational aurora kinase A inhibitor, in patients with breast cancer, small-cell lung cancer, non-small-cell lung cancer, head and neck squamous-cell carcinoma, and gastro-oesophageal adenocarcinoma: A five-arm phase 2 study. Lancet Oncol. 2015, 16, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Godwin, J.L.; Mehra, R.; Litwin, S.; Olszanski, A.J.; Bauman, J.R.; Borghaei, H. A phase I/II study of MLN-8237 (alisertib), an oral aurora kinase inhibitor, in combination with erlotinib in patients with recurrent or metastatic EGFR wild-type non-small cell lung cancer. J. Clin. Oncol. 2016, 34, e20588. [Google Scholar] [CrossRef]
- Owonikoko, T.K.; Niu, H.; Nackaerts, K.; Csoszi, T.; Ostoros, G.; Mark, Z.; Baik, C.; Joy, A.A.; Chouaid, C.; Jaime, J.C.; et al. Randomized Phase II Study of Paclitaxel plus Alisertib versus Paclitaxel plus Placebo as Second-Line Therapy for SCLC: Primary and Correlative Biomarker Analyses. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2020, 15, 274–287. [Google Scholar] [CrossRef] [PubMed]
- Schöffski, P.; Besse, B.; Gauler, T.; Jonge, M.J.A.d.; Scambia, G.; Santoro, A.; Davite, C.; Jannuzzo, M.G.; Petroccione, A.; Delord, J.-P. Efficacy and safety of biweekly i.v. administrations of the Aurora kinase inhibitor danusertib hydrochloride in independent cohorts of patients with advanced or metastatic breast, ovarian, colorectal, pancreatic, small-cell and non-small-cell lung cancer: A multi-tumour, multi-institutional phase II study. Ann. Oncol. 2015, 26, 598–607. [Google Scholar] [CrossRef]
- Gauler, T.C.; Besse, B.; Novello, S.; Smit, E.F.; Plummer, E.R.; Delord, J.-P.; Nicodemo, M.; Santoro, A.; Barone, C.; Marchetti, P.; et al. Phase II study of danusertib (D) in advanced/metastatic non-small cell lung cancers (NSCLC). J. Clin. Oncol. 2013, 31, e19138. [Google Scholar] [CrossRef]
- Arkenau, H.-T.; Plummer, R.; Molife, L.R.; Olmos, D.; Yap, T.A.; Squires, M.; Lewis, S.; Lock, V.; Yule, M.; Lyons, J.; et al. A phase I dose escalation study of AT9283, a small molecule inhibitor of aurora kinases, in patients with advanced solid malignancies. Ann. Oncol. 2012, 23, 1307–1313. [Google Scholar] [CrossRef]
- Warner, S.L.; Munoz, R.M.; Stafford, P.; Koller, E.; Hurley, L.H.; Hoff, D.D.V.; Han, H. Comparing Aurora A and Aurora B as molecular targets for growth inhibition of pancreatic cancer cells. Mol. Cancer Ther. 2006, 5, 2450–2458. [Google Scholar] [CrossRef][Green Version]
 ) and AURKB (
) and AURKB ( ) are expressed and activated from the G2 through the M phase being involved in mitotic chromosomal segregation [13,14]. AURKA is mainly localized in the centrosomes in interphase and mitotic cells, and is important for centrosome maturation and separation, which in turn are necessary for mitotic entry and bipolar spindle formation. AURKB is generally located at the kinetochore of mitotic cells and to the midbody of cytokinetic cells, which regulate kinetochore-microtubule attachments that are critical for chromosome alignment and segregation as well as to regulate cytokinesis [31,32]. AURKB and AURKC are thought to have the same distribution pattern in mitotic cells [33], hence, AURKC is not included in the diagram.
) are expressed and activated from the G2 through the M phase being involved in mitotic chromosomal segregation [13,14]. AURKA is mainly localized in the centrosomes in interphase and mitotic cells, and is important for centrosome maturation and separation, which in turn are necessary for mitotic entry and bipolar spindle formation. AURKB is generally located at the kinetochore of mitotic cells and to the midbody of cytokinetic cells, which regulate kinetochore-microtubule attachments that are critical for chromosome alignment and segregation as well as to regulate cytokinesis [31,32]. AURKB and AURKC are thought to have the same distribution pattern in mitotic cells [33], hence, AURKC is not included in the diagram.
 ) and AURKB (
) and AURKB ( ) are expressed and activated from the G2 through the M phase being involved in mitotic chromosomal segregation [13,14]. AURKA is mainly localized in the centrosomes in interphase and mitotic cells, and is important for centrosome maturation and separation, which in turn are necessary for mitotic entry and bipolar spindle formation. AURKB is generally located at the kinetochore of mitotic cells and to the midbody of cytokinetic cells, which regulate kinetochore-microtubule attachments that are critical for chromosome alignment and segregation as well as to regulate cytokinesis [31,32]. AURKB and AURKC are thought to have the same distribution pattern in mitotic cells [33], hence, AURKC is not included in the diagram.
) are expressed and activated from the G2 through the M phase being involved in mitotic chromosomal segregation [13,14]. AURKA is mainly localized in the centrosomes in interphase and mitotic cells, and is important for centrosome maturation and separation, which in turn are necessary for mitotic entry and bipolar spindle formation. AURKB is generally located at the kinetochore of mitotic cells and to the midbody of cytokinetic cells, which regulate kinetochore-microtubule attachments that are critical for chromosome alignment and segregation as well as to regulate cytokinesis [31,32]. AURKB and AURKC are thought to have the same distribution pattern in mitotic cells [33], hence, AURKC is not included in the diagram.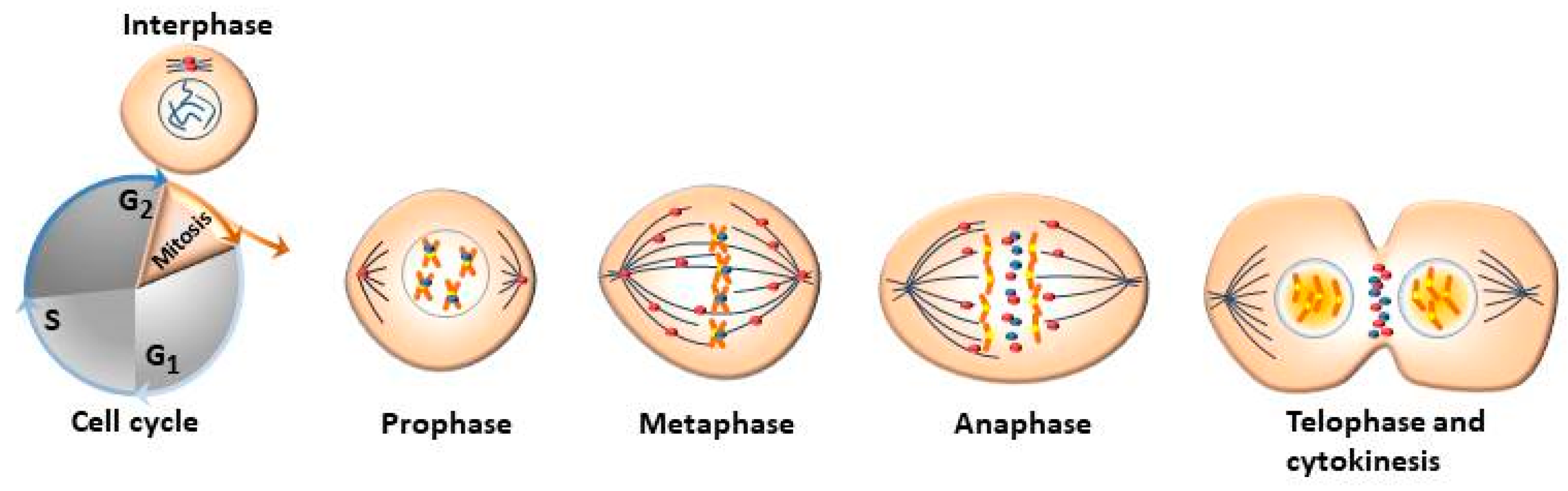
| Aurora Kinase | Prognostic/Oncogenic Effect | Experimental Specimen; Method | Reference |
|---|---|---|---|
| AURKA | Correlates with decreased OS | NSCLC tumor samples; IHC | [16] |
| AURKA | Potential biomarker for predicting poor prognosis in smoking-related LC | Cancer Genome Atlas data base; bioinformatic-based analysis | [17] |
| AURKA | Independent predictor of poor prognosis | NSCLC tumor and adjacent normal lung tissues; PCR | [18] |
| AURKA | Correlates with poor survival | NSCLC tumor and corresponding normal lung tissues; IHC | [19] |
| AURKA | Correlates with shorter OS | NSCLC tissues; IHC | [20] |
| AURKA | Correlates with poor OS and progression-free interval; contributes to reduced drug response | NSCLC tissues; IHC | [21] |
| AURKA | No correlation with patient survival | NSCLC tumor and corresponding normal lung tissues; IHC and RT-PCR | [14] |
| AURKA | Potential pro-oncogenic role in MPM | MPM tissues; qPCR analysis | [48] |
| AURKB | Correlates with reduced OS and disease-free interval; impairs response to cisplatin and paclitaxel | NSCLC tumor biopsies; RT-PCR | [42] |
| AURKB | No correlation with OS | Frozen NSCLC tissues; qPCR | [45] |
| AURKB | Correlates with poor prognosis | NSCLC tissues; IHC Same as above NSCLC tumor and adjacent lung tissues; IHC | [22] [23] [24] |
| AURKB | Correlates with lymph node metastasis and poor tumor differentiation grade | NSCLC tissues; IHC NSCLC tumor and adjacent lung tissues; IHC | [43] [24] |
| AURKA and AURKB | Potential pro-oncogenic role in MPM | MPM tissues and cell lines; transcript analysis | [48] |
| AURKA and AURKB | High expression levels in aggressive MPM | MPM tissues; microarray analysis | [49] |
| Aurora Kinase | Effect on Chemo-and/or Radiotherapy | Experimental Sample; Method | Reference |
|---|---|---|---|
| AURKA | Resistance to EGFR inhibitors; triggers disease recurrence | EGFR-mutant lung adenocarcinoma cells; in vitro/in vivo analysis | [25] |
| AURKA | Overexpression confers resistance to radiotherapy in docetaxel-resistant, SPC-A1/DTX lung adenocarcinoma cells | SPC-A1 lung cancer cells; in vitro analysis | [50] |
| AURKA | AURKA/TPX2 overexpression associates with paclitaxel-mediated radiosensitization; improves OS | Cancer genome atlas lung adenocarcinoma cohort; in vitro analysis | [27] |
| AURKA | Resistance to gefitinib-induced apoptosis | A549 lung cancer cells: in vitro analysis | [26] |
| AURKA | Resistance to cytotoxic agents such as adriamycin and VP-16 (etoposide) | A549 lung cancer cells; in vitro analysis | [51,52] |
| AURKB | Resistance to EGFR inhibitors | NSCLC tumor samples; in vitro analysis | [1] |
| AURKB | Low levels confer resistance to paclitaxel | NSCLC cell lines; in vitro analysis | [45] |
| Inhibitor | Therapeutic Effect | Reference |
|---|---|---|
| 24-mCAF (major component of rice bran oil) | Inhibition of cell proliferation and activation of apoptosis in A549 lung cancer cells | [66] |
| S49076 (MET/AXL/FGFR inhibitor) | Inhibition of AURKB confers improved radiotherapy in MET-dependent and MET–independent lung cancer cell lines | [62] |
| TC-A2317 (AURKA inhibitor) | Reduction in cell proliferation in lung cancer cells; induction of cell type-dependent apoptosis and autophagy | [53] |
| Quercetin | Direct binding to AURKB inhibits its pro-tumorigenic actions in lung cancer cells and lung cancer xenografts | [63] |
| AKII (dual AURKA and AURKB inhibitor) | Repression of cell growth, viability and induction of apoptosis in a KRAS-dependent manner in A549 and H358 lung cancer cells | [67] |
| Tanschinone (traditional herbal medicine) | Inhibition of lung cancer cells in vitro by suppression of AURKA | [56] |
| HOI-07 | Attenuation of cancer cell-anchorage-independent growth and inhibition of lung cancer xenografts through suppression of AURKB and histone H3 Ser10 phosphorylation | [64] |
| Ceftriaxone (cephalosporin antibiotic) | Off-target effect on AURKB; decreases anchorage-dependent growth of lung cancer cells; growth reduction in lung cancer xenografts | [65] |
| AZD 1152-HQPA (inhibitor of AURKB) concomitant to radiotherapy | Prevents repopulation of NSCLC cells during radiotherapy | [58] |
| Valproic acid and FTS (RAS inhibitor) | Reduction in A549 cell proliferation; block expression of survivin and AURKA | [55] |
| SLAN (KIAA0256) | Repression of AURKA kinase activity and expression levels; inhibition of cell proliferation of lung cancer cells | [57] |
| R763/AS703569 | Exerts anti-proliferative activity via inhibition of Aurora kinases and FMS-related tyrosine kinases; growth inhibition of lung tumor xenografts | [54] |
| AZD 1152 | Selective inhibition of AURKB; growth inhibition of lung tumor xenografts | [60] |
| ZM447439 (AURKB inhibitor) and survivin antisense oligonucleotide | Sensitization of mesothelioma cells to radiotherapy | [61] |
| AZD 1152-HQPA | Reduction in cell viability; induction of cell apoptosis in mesothelioma cell lines | [59] |
| ZM447439 | Inhibition of AURKA and AURKB; suppression of cell growth of mesothelioma cells via reduction in histone H3 phosphorylation | [48] |
| Daurinol (topoisomerase inhibitor) | In combination with radiation decreases growth of lung cancer xenografts through inhibition of AURKA and AURKB | [68] |
| GSK 1070916 (AURKB and AURKC inhibitor) | Dose-dependent inhibition of histone H3 phosphorylation causing failure in cell division and polyploidy leading to apoptosis: tumor growth suppression in murine model | [69] |
| Inhibitor | Therapeutic Effect/Clinical Trial | Reference |
|---|---|---|
| Alisertib (MLN8238), AURKA inhibitor | Antitumor effect in advanced SCLC/phase II study | [71] |
| Combined alisertib and erlotinib, EGFR inhibitor | Synergistic antitumor effect in wild- type EGFR NSCLC/phase I/II study | [72] |
| Combined alisertib and paclitaxel | Modest efficacy signal as second-line therapy in relapsed or refractory SCLC/phase II study | [73] |
| Danusertib (PHA-739358), pan-Aurora kinase inhibitor | Marginal antitumor action after failure of prior systematic therapies in NSCLC and squamous NSCLC/phase II study | [74] |
| Danusertib | Insufficient efficacy as monotherapy in advanced/metastatic NCSLC/phase II study | [75] |
| AT9283, AURKA and AURKB inhibitor | No objective tumor response; stable RECIST disease of ≥6 months/phase I study | [76] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galetta, D.; Cortes-Dericks, L. Promising Therapy in Lung Cancer: Spotlight on Aurora Kinases. Cancers 2020, 12, 3371. https://doi.org/10.3390/cancers12113371
Galetta D, Cortes-Dericks L. Promising Therapy in Lung Cancer: Spotlight on Aurora Kinases. Cancers. 2020; 12(11):3371. https://doi.org/10.3390/cancers12113371
Chicago/Turabian StyleGaletta, Domenico, and Lourdes Cortes-Dericks. 2020. "Promising Therapy in Lung Cancer: Spotlight on Aurora Kinases" Cancers 12, no. 11: 3371. https://doi.org/10.3390/cancers12113371
APA StyleGaletta, D., & Cortes-Dericks, L. (2020). Promising Therapy in Lung Cancer: Spotlight on Aurora Kinases. Cancers, 12(11), 3371. https://doi.org/10.3390/cancers12113371







